Abstract
Hypertension is the most important risk factor for cerebral small vessel disease (SVD). In this cross-sectional study, we tested the independent association of cerebral SVD burden with global cognitive function and each cognitive domain in patients with vascular risk factors. The Tokyo Women’s Medical University Cerebral Vessel Disease (TWMU CVD) registry is an ongoing prospective, observational registry in which patients with any evidence of CVD in magnetic resonance imaging (MRI) and at least one vascular risk factor were consecutively enrolled. For SVD-related findings, we evaluated white matter hyperintensity, lacunar infarction, cerebral microbleeds, enlarged perivascular space, and medial temporal atrophy. We used the total SVD score as the SVD burden. They underwent the Mini-mental State Examination (MMSE) and Japanese version of the Montreal Cognitive Assessment (MoCA-J) global cognitive tests, and each cognitive domain was evaluated. After excluding patients without MRI T2* images and those with MMSE score <24, we analyzed 648 patients. The total SVD score was significantly associated with MMSE and MoCA-J scores. After adjustment for age, sex, education, risk factors, and medial temporal atrophy, the association between the total SVD score and MoCA-J score remained significant. The total SVD score was independently associated with attention. In conclusion, the total SVD score, cerebral SVD burden, was independently association with global cognitive function and attention. A strategy to reduce SVD burden will have the potential to prevent cognitive decline.

A total of 648 patients with any evidence of cerebral small vessel disease (SVD) in MRI and at least one vascular risk factor underwent Mini-mental State Examination (MMSE) and Japanese version of the Montreal Cognitive Assessment (MoCA-J) global cognitive tests. The total SVD scores count the presence of each SVD-related findings (white matter hyperintensity, Lacunar infarction, cerebral microbleeds and enlarged perivascular space), ranging from 0 to 4, as the SVD burden. Total SVD scores were significantly associated with MoCA-J scores (r = −0.203, P < 0.001). After adjustment for age, sex, education, risk factors, and medial temporal atrophy, the association between the total SVD score and global cognitive scores remained significant.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Cerebral small vessel disease (SVD) has attracted much attention because several cohort studies have shown an association between cerebral SVD and incident stroke, as well as incident dementia [1,2,3,4]. Cerebral SVD is believed to be a key factor in explaining the relationship between vascular risk factors and dementia, especially Alzheimer’s disease (AD). Cross-sectional studies have shown that cerebral SVD is associated with cognitive function, especially executive function and processing speed [5]. Among risk factors, hypertension is the most important risk factor for SVD [6].
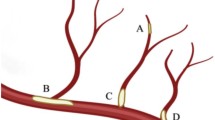
Features of cerebral SVD seen on neuroimaging include recent small subcortical infarcts, lacunar infarction (LI), white matte hyperintensity (WMH), cerebral microbleeds (CMB), enlarged perivascular space (EPVS), and brain atrophy [7]. Previous studies have shown a significant association between cognitive function and WMH [8, 9] and CMB [10]; however, the relationship between EPVS and cognitive function is unclear [11].
Recently, the total SVD score was proposed as a simple score representing WMH, LI, CMB and EPVS [12, 13]. The total SVD scores is related to vascular risk factors [13, 14], and are associated with global cognitive function [12, 15, 16]. The total SVD score can predict the risk of recurrent stroke [17, 18], cardiovascular event [19], incident dementia [18] and cognitive decline [20].
However, several key factors such as age, education, risk factors and brain atrophy other than cerebral SVD-related findings also showed a close association with dementia [21, 22], and cerebral SVD-related findings also showed a relationship with age, vascular risk factors, and brain atrophy [23].
It still remains unclear whether SVD burden is significantly associated with global cognitive function and each cognitive subdomain independent of medial temporal atrophy (MTA), a strong biomarker predictive of incident AD [22], and other confounding factors.
Methods
Participants
Data were derived from a prospective study, the Tokyo Women’s Medical University Cerebral Vessel Disease (TWMU CVD) Registry (Registration-URL: https://www.umin.ac.jp/ctr/index.htm; UMIN000026671), from October 2015 to July 2019. This study conformed to the ethical guidelines of the 1975 Declaration of Helsinki in line with the Ethical Guidelines for Epidemiological Research by the Japanese government and the Strengthening the Reporting of Observational Studies in Epidemiology guidelines. Written informed consent was obtained from all the participants. This study was approved by the institutional review board of Tokyo Women’s Medical University. The research protocol and inclusion criteria of the TWMU CVD registry have been previously described in detail [24, 25]. In brief, we consecutively included outpatients aged 40 years with any vascular risk factors or a history of cerebrovascular events who underwent brain magnetic resonance imaging (MRI) within 1 year and had any signs of cerebral vessel disease. The exclusion criteria for the registry were any kind of aphasia, evidence of dementia (clinical dementia rating ≥1), and dependence for activities of daily living and walking. We also excluded those who suffered vascular events including stroke within one month.
Cognitive examination
Patients underwent the Mini-Mental State Examination (MMSE) and the Japanese version of Montreal Cognitive Assessment (MoCA-J) [26] within 1 year of MRI examination. Among the items in the MMSE and MoCA-J, the scores of each cognitive domain; executive function (0–4), memory (0–8), orientation (0–10), language (0–13), visuospatial function (0-5) and attention and working memory (0–11) were extracted (Supplementary Table 1).
MRI assessment
Each participant underwent a brain MRI scan within 1 year of entry into the registry. The MRI assessment included WMH consisting of periventricular hyperintensity (PVH) and deep WMH (DWMH), LI, CMB, EPVS, total SVD score [14], and MTA [27]. WMH severity was visually rated using axial fluid attenuated inversion recovery (FLAIR) images. According to the Fazekas scale (0 = none; 1 = mild; 2 = moderate; 3 = severe) [28], PVH and DWMH were evaluated from 0 to 3; additionally, the total WMH score was assigned ranging from 0 to 6 with the sum of PVH and DWMH. Lesions in the basal ganglia, internal capsule, centrum semiovale, or brainstem with hypointensity on T1-weighted imaging, hyperintensity on T2-weighted imaging, and a hyperintense rim around the cavity on FLAIR were defined as LI with sizes ranging from 3 to 15 mm. CMB were defined as punctate or small patchy lesions <10 mm in diameter with obvious low intensity on T2-star weighted imaging. EPVS were defined as round, oval, or linear-shaped lesions with a smooth margin and signal intensity equal to that of cerebrospinal fluid on both T1 and T2-weighted images [29]. We counted the EPVS on the slide with the highest number in the basal ganglia. MTA was rated from 0 (absent) to 4 (severe) according to the previous guideline [27].
The total SVD score was assigned from 0 to 4 by incorporating all four MRI markers including WMH, LI, CMB, and EPVS [14]. A point was awarded for WMH if PVH Fazekas 3 (extending into the deep white matter) and /or DWMH Fazekas 2-3 (confluent or early confluent) was present. For LI, one point was awarded if ≥1 asymptomatic lesions was present. For CMB, one point was awarded if ≥1 any CMB was present in the cerebellum, brainstem, the basal ganglia, white matter, or cortico-subcortical junction. For EPVS, one point was awarded if more than 10 EPVS in the slice, including the basal ganglia, were present. All grades of cerebral SVD-related findings were rated by two trained board-certified neurologists (MH and KK) who were blinded to clinical details.
Statistical analysis
All analyses were performed using JMP 13 Pro. For baseline characteristics, the mean and standard deviation (SD) were used for continuous variables, and the frequency and percentage of the total population were used for categorical variables. The median and interquartile range were presented for ordinal and non-normally distributed variables. Relationships between the MMSE, MOCA-J, or each cognitive domain and continuous variables were examined using Pearson’s correlation analysis. For categorical variables, differences in MMSE and MoCA-J scores were examined using an unpaired t test. Subsequently, multiple linear regression analyses were performed to examine associations between the total SVD score and MMSE or MOCA-J scores by controlling for age, sex, education, risk factors and other MRI findings.
Results
Among the 1022 patients enrolled in the TWMU CVD registry, 64 refused to undergo cognitive examination, 234 did not undergo T2* imaging, and 76 had a MMSE score <24 (Supplementary Fig. 1). After exclusion of 374 patients, 648 patients who underwent MRI examination, including T2*, and both MMSE and MoCA-J examinations, were analyzed.
The baseline characteristics of study participants are summarized in Table 1. The median age was 71 years, 58.4% were men, and the median number of years of education was 16 years. Sixty-eight percent of the participants had hypertension, 29% had DM, and 48% had chronic kidney disease (CKD), and 53% had a history of cerebrovascular disease. The median total WMH score was 2. The presence of LI, CMB and EPVS > 10 in the basal ganglia slice were 47.2%, 35.0% and 9.1%, respectively. The median total SVD scores was 1. The distribution of MMSE and MoCA-J scores is shown in Supplementary Figure 2. MMSE was 28.9 ± 1.9 (mean ± SD), and MoCA-J was 23.6 ± 3.5. In the subdomain of cognitive function, the median score for orientation and visuospatial function reached the highest point.
The association between global cognitive function and confounding factors is presented in Supplementary Table 2. Both MMSE and MoCA-J scores were correlated with age and education. MMSE scores were lower in those with hypertension than in those without it, and the MoCA-J score was lower in men, and in those with DM and CKD than in women and in those without DM and CKD, respectively.
The correlation between global cognitive function and each MRI finding is shown in Figs. 1 and 2, respectively. The total WMH, PVH and DWMH Fazekas scores were significantly related to the MMSE and MoCA-J scores (Fig. 1). However, the correlation seems stronger with MoCA-J than with the MMSE score. Those with LI had lower MMSE and MoCA-J scores than those without LI (Supplementary Table 3). Those with CMB had lower MMSE scores than those without it, however, MoCA-J scores were similar between patients with and without CMB. Both MMSE and MoCA-J scores were similar between patients with and without EPVS > 10. Both MMSE and MoCA-J scores were significantly correlated with MTA. The correlation between the total SVD score and global cognitive function is shown in Fig. 3. There were several confounding factors related to cognitive function, as shown in Supplementary Table 2 therefore, we examined the association after controlling for these factors (Table 2). In model 1, the association between the total SVD score and global cognitive function remained significant. However, after controlling for age, sex, education and vascular risk factors (model 2), the association between the total SVD score and MMSE scores was not significant. After further controlling for MTA (model 3), the relationship between the total SVD score and MoCA-J remained significant. We analyzed the relationship between the total SVD score and each cognitive subdomain (Fig. 4). Univariate analysis revealed a significant correlation between the total SVD score and executive function, memory, language, and attention. After controlling for confounding factors, the association between the total SVD score and attention remained significant (Supplementary Table 4).
Correlation between global cognitive functions and white matter hyperintensity. Correlation between MMSE and total WMH (A), PVH (B) and DWMH (C). Correlation between MoCA-J and total WMH (D), PVH (E) and DWMH (F). MMSE Mini-Mental State Examination, MoCA-J the Japanese version of the Montreal Cognitive Assessment, WMH white matter hyperintensity, PVH periventricular hyperintensity, DWMH deep white matter hyperintensity
Discussion
This study clarified that the total SVD score was significantly associated with global cognitive function and its subdomains, attention, even after controlling for confounding factors and MTA.
Among SVD-related findings, WMH, LI and CMB were significantly associated with global cognitive function; however, the relationship between EPVS and cognitive function was not significant. These findings are consistent with previous finding [7,8,9,10,11]. This study is the first to show that the total SVD score was significantly associated with cognitive function independent of years of education, vascular risk factors, and MTA, strong predictor of incident AD dementia [22]. In terms of the cognitive subdomain, a significant association between attention and working memory and total SVD score was in line with previous finding [30]. Among SVD-related findings, LI and WMH were shown to be closely associated with executive function, attention and frontal assessment battery [8, 31, 32].
Previous studies have shown a close association between SVD-related findings and vascular risk factors [13, 14] and brain atrophy [23], and our study added an important aspect of the total SVD score on cognitive function. Further studies are needed to strengthen the predictive value of total SVD score for vascular events and incident dementia.
The close association between the total SVD score and cognitive function raises the question of whether therapeutic intervention for SVD-related findings reduces the risk of cognitive decline and incident dementia. However, five categories from 0 to 4 in the total SVD score would not be suitable as a surrogate index of intervention. Evaluation of each SVD-related finding as well as the total SVD burden would be important for follow-up studies because previous studies have shown that the progression of WMH is related to cognitive decline [33, 34].
This study had several limitations. First, because of the single-center setting, the findings need to be confirmed in other centers and ethnic populations. Second, although we examined the association between each cognitive domain and total SVD score, we extracted each component from the MMSE and MoCA-J. Therefore, the power of the battery for the measurement of each component is not sufficient for a thorough investigation. This would explain why the median score in several components, such as orientation and visuospatial function, had already reached the highest score. We might have overlooked subtle changes in these cognitive domains. Third, we employed a visual rating, not a quantitative evaluation for WMH. Although the WMH grading scale is practical in routine clinical practice, it is neither an objective nor a sensitive method. A volumetric measure is needed to evaluate the longitudinal changes or effects of WMH intervention.
Perspectives in Asia
Cerebral SVD is the main etiology in Asian stroke patients. Hypertension is the most important risk factor for both symptomatic and asymptomatic SVD. Our findings showed the close association between cerebral SVD-related findings and cognitive function. Although it remains unclear whether intensive blood pressure control is effective for prevention of SVD development, our findings suggest that anti-hypertensive treatment would have potential for prevention of dementia, especially in Asian people.
Conclusions
Cerebral SVD-related findings are associated with global cognitive function and its subdomain, attention, independent of confounding factors and MTA. Preventing the development of cerebral SVD-related findings by controlling vascular risk factors, especially hypertension, could potentially prevent cognitive impairment.
References
Vermeer SE, Longstreth WT Jr, Koudstaal PJ. Silent brain infarcts: a systematic review. Lancet Neurol. 2007;6:611–9.
Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ. 2010;341:c3666.
Akoudad S, Portegies MLP, Koudstaal PJ, Hofman A, van der Lugt A, Ikram MA, et al. Cerebral microbleeds are associated with an increased risk of stroke: the Rotterdam Study. Circulation. 2015;132:509–16.
Akoudad S, Wolters FJ, Viswanathan A, de Bruijn EF, van der Lugt A, Hofman A, et al. Association of cerebral microbleeds with cognitive decline and dementia. JAMA Neurol. 2016;73:934–43.
Hamilton OKL, Backhouse EV, Janssen E, Jochems ACC, Maher C, Ritakari TE, et al. Cognitive impairment in sporadic cerebral small vessel disease: a systematic review and meta-analysis. Alzheimers Dement. 2021;17:665–85.
Kitagawa K. Blood pressure management for secondary stroke prevention. Hypertens Res. 2022;45:936–43.
Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013;12:822–38.
Zamboni G, Griffanti L, Jenkinson M, Mazzucco S, Li L, Küker W, et al. White matter imaging correlates of early cognitive impairment detected by the montreal cognitive assessment after transient ischemic attack and minor stroke. Stroke. 2017;48:1539–47.
Hoshi T, Yamagami H, Furukado S, Miwa K, Tanaka M, Sakaguchi M, et al. Serum inflammatory proteins and frontal lobe dysfunction in patients with cardiovascular risk factors. Eur J Neurol. 2010;17:1134–40.
Yakushiji Y, Nishiyama M, Yakushiji S, Hirotsu T, Uchino A, Nakajima J, et al. Brain microbleeds and global cognitive function in adults without neurological disorder. Stroke. 2008;39:3323–8.
Hilal S, Tan CS, Adams HHH, Habes M, Mok V, Venketasubramanian N, et al. Enlarged perivascular spaces and cognition: a meta-analysis of 5 population-based studies. Neurology. 2018;91:e832–e842.
Huijts M, Duits A, van Oostenbrugge RJ, Kroon AA, de Leeuw PW, Staals J. Accumulation of MRI markers of cerebral small vessel disease is associated with decreased cognitive function. a study in first-ever lacunar stroke and hypertensive patients. Front Aging Neurosci. 2013;5:72.
Klarenbeek P, van Oostenbrugge RJ, Rouhl RP, Knottnerus IL, Staals J. Ambulatory blood pressure in patients with lacunar stroke: association with total MRI burden of cerebral small vessel disease. Stroke 2013;44:2995–9.
Staals J, Makin SD, Doubal FN, Dennis MS, Wardlaw JM. Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden. Neurology. 2014;83:1228–34.
Staals J, Booth T, Morris Z, Bastin ME, Gow AJ, Corley J, et al. Total MRI load of cerebral small vessel disease and cognitive ability in older people. Neurobiol Aging. 2015;36:2806–11.
Uiterwijk R, van Oostenbrugge RJ, Huijts M, De Leeuw PW, Kroon AA, Staals J. Total cerebral small vessel disease MRI score is associated with cognitive decline in executive function in patients with hypertension. Front Aging Neurosci. 2016;8:301.
Lau KK, Li L, Schulz U, Simoni M, Chan KH, Ho SL, et al. Total small vessel disease score and risk of recurrent stroke: Validation in 2 large cohorts. Neurology. 2017;88:2260–7.
Yilmaz P, Ikram MK, Niessen WJ, Ikram MA, Vernooij MW. Practical small vessel disease score relates to stroke, dementia, and death. Stroke. 2018;49:2857–65.
Suzuyama K, Yakushiji Y, Ogata A, Nishihara M, Eriguchi M, Kawaguchi A, et al. Total small vessel disease score and cerebro-cardiovascular events in healthy adults: the Kashima scan study. Int J Stroke. 2020;15:973–9.
Zhi N, Zhang L, Wang Y, Bai S, Geng J, Yu L, et al. Modified cerebral small vessel disease score is associated with vascular cognitive impairment after lacunar stroke. Aging. 2021;13:9510–21.
Serrano-Pozo A, Growdon JH. Is Alzheimer’s disease risk modifiable? J Alzheimers Dis. 2019;67:795–819.
Frisoni GB, Fox NC, Jack CR Jr, Scheltens P, Thompson PM. The clinical use of structural MRI in Alzheimer disease. Nat Rev Neurol. 2010;6:67–77.
Litak J, Mazurek M, Kulesza B, Szmygin P, Litak J, Kamieniak P, et al. Cerebral small vessel disease. Int J Mol Sci. 2020;21:9729.
Kubota M, Iijima M, Shirai Y, Toi S, Kitagawa K. Association between cerebral small vessel disease and central motor conduction time in patients with vascular risk. J Stroke Cerebrovasc Dis. 2019;28:2343–50.
Seki M, Yoshizawa H, Hosoya M, Kitagawa K. Neuropsychological profile of early cognitive impairment in cerebral small vessel disease. Cerebrovasc Dis. 2022;51:600–7.
Fujiwara Y, Suzuki H, Yasunaga M, Sugiyama M, Ijuin M, Sakuma N, et al. Brief screening tool for mild cognitive impairment in older Japanese: validation of the Japanese version of the Montreal Cognitive Assessment. Geriatr Gerontol Int. 2010;10:225–32.
Kim GH, Kim JE, Choi KG, Lim SM, Lee JM, Na DL, et al. T1-weighted axial visual rating scale for an assessment of medial temporal atrophy in Alzheimer’s disease. J Alzheimers Dis. 2014;41:169–78.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. Am J Roentgenol. 1987;149:351–6.
Doubal FN, MacLullich AMJ, Ferguson KJ, Dennis MS, Wardlaw JM. Enlarged perivascular spaces on MRI are a feature of cerebral small vessel disease. Stroke. 2010;41:450–4.
Vasquez BP, Zakzanis KK. The neuropsychological profile of vascular cognitive impairment not demented: a meta-analysis. J Neuropsychol. 2015;9:109–36.
Ishikawa H, Meguro K, Ishii H, Tanaka N, Yamaguchi S. Silent infarction or white matter hyperintensity and impaired attention task scores in a nondemented population: the Osaki-Tajiri Project. J Stroke Cerebrovasc Dis. 2012;21:275–82.
Carey CL, Kramer JH, Josephson SA, Mungas D, Reed BR, Schuff N, et al. Subcortical lacunes are associated with executive dysfunction in cognitively normal elderly. Stroke. 2008;39:397–402.
Hirao K, Yamashita F, Tsugawa A, Haime R, Fukasawa R, Sato T, et al. Association of white matter hyperintensity progression with cognitive decline in patients with amnestic mild cognitive impairment. J Alzheimers Dis. 2021;80:877–83.
Jiang J, Yao K, Huang X, Zhang Y, Shen F, Weng S. Longitudinal white matter hyperintensity changes and cognitive decline in patients with minor stroke. Aging Clin Exp Res. 2022;34:1047–54.
Funding
This work was supported in part by Research Funding of Longevity Sciences (28-15, 30-1) from the National Center for Geriatrics and Gerontology, the Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KK reports personal fees from Daiichi Sankyo, Kyowa Kirin and Kowa. Others have nothing to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hosoya, M., Toi, S., Seki, M. et al. Association between total cerebral small vessel disease score and cognitive function in patients with vascular risk factors. Hypertens Res 46, 1326–1334 (2023). https://doi.org/10.1038/s41440-023-01244-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01244-8
- Springer Nature Singapore Pte Ltd.
Keywords
This article is cited by
-
Small vessels cause big problems
Hypertension Research (2024)