Abstract
Left ventricular hypertrophy (LVH) is a major cardiac complication of hypertension. Weight-adjusted-waist index (WWI) is a new obesity index that has been found to be positively associated with cardiovascular disease mortality. We aimed to investigate the relationship between the WWI and LVH in Chinese hypertension adults. The study is a community-based cross-sectional study that included 4715 patients with hypertension and integrated clinical and echocardiographic data. LVH was diagnosed by transthoracic echocardiography in these patients based on a criterion of left ventricular mass index (LVMI) over 49.2 g/m2.7 in men and 46.7 g/m2.7 in women. The independent association between the WWI quartiles and LVH prevalence was analyzed by logistic regression models. The prevalence of LVH in the first quartile of WWI (Q1: <10.16), second (Q2: 10.16 ~ 10.67), the third (Q3: 10.68~11.19), and the highest quartile (Q4: ≥11.20) was 34.1%, 38.4%, 42.4%, 51.5%, respectively. Logistic regression analysis suggested that the WWI was independently correlated with LVH with adjustment of confounding factors, and increased across the quartile of WWI. Compared to the first quartile of WWI (Q1), the odds ratios (ORs) and their 95% confidence intervals (CIs) for LVH in the increasing quartiles (Q2–Q4) were 1.33(1.08-1.63), 1.50 (1.19–1.89) and 2.28(1.74–2.99), respectively. In stratified analyses, the relationship between WWI and LVH risk persisted. The WWI may be an independent determinant of LVH in Chinese hypertension adults.
Similar content being viewed by others
Introduction
Left ventricular hypertrophy (LVH) is a serious cardiac disease characterized by ventricular wall thickening, increased myocardial weight, and myocardial remodeling, which further leads to heart failure [1, 2]. LVH often occurs in hypertensive patients and is the most common complication of hypertension [3, 4]. LVH significantly increases the risk of coronary atherosclerotic heart disease, heart failure, stroke, and death in hypertensive patients [2, 5, 6]. Studies have shown that obesity increases the accumulation of fat in the heart and increases the risk of hypertensive LVH [7, 8]. Therefore, early improvement of obesity assessment and early identification and reversal of LVH in patients with obesity-related hypertension can significantly reduce the risk of cardiovascular events and death. [9, 10].
WWI is a new obesity index. Previous studies have shown that WWI is positively associated with fat mass and negatively associated with muscle mass [11]. The study of approximately 1 million Korean adults found that WWI was positively associated with cardiovascular mortality and was best at predicting the risk of cardiometabolic disease and death, which has been proposed to assess obesity [11, 12]. Studies have shown that obesity increases fat accumulation in the heart, which is often associated with LVH [7]. Traditionally, body mass index (BMI) and waist circumference (WC) have been used to identify obesity and related cardiometabolic diseases. However, recently, a large epidemiological study showed that WWI was the best predictor of cardiovascular mortality compared with BMI/WC [12]. Given that LVH is an independent risk factor for cardiovascular disease, the relationship between WWI and LVH in hypertensive population remains unclear. These findings suggest that epidemiological studies should further explore the association between WWI and LVH. We hypothesized that WWI could be used as an effective indicator for the early identification of LVH risk in hypertensive population. Therefore, we conducted a cross-sectional study to clarify the association between WWI and LVH and to assess whether it was influenced by other relevant factors. In addition, subgroup analyses were performed to test the robustness of our results.
Methods
Study population
Our study protocol and exclusion criteria were described in detail in previous studies [6, 13]. This study used a multi-stage cluster sampling method to conduct a cross-sectional survey of rural residents aged 40–75 years in Xinyang County, central China during 2004–2005. A total of 13,444 villagers (5270 males and 8174 females) completed the survey. A total of 5421 hypertensive patients were enrolled. Among them, 4805 patients completed the measurement of left ventricular weight. Ninety participants were excluded due to a lack of anthropometric data. Figure 1 shows the recruitment process of the study population. This study was approved by the ethics committees of Fuwai Hospital and local hospitals. The research process follows ethical standards. All study subjects provided written consent forms and all investigators received uniform training at the Chinese Academy of Medical Sciences (Beijing, China) before the start of the study.
Covariate measurements and definitions
Demographic data, past medical history, smoking, and alcohol consumption were recorded accurately. Smoking history refers to past or current regular smoking behavior. Drinking history refers to regular drinking behavior in the past or at present. All subjects underwent routine physical examinations, including height, weight, WC, hip circumference, and resting blood pressure (blood pressure measured by a trained professional with a standard mercury sphygmomanometer). Participants should rest for at least five minutes and refrain from caffeinated beverages or exercise before taking blood pressure measurements. Measurements were taken three times, at least 30 s apart, and averaged over three times. Use the same height–weight measuring machine and ruler. During the measurement, the subjects wore light-colored clothes, took off their shoes and hats, and stood at attention. The height and weight of the subjects were accurate to 0.1 cm and 0.1 kg, respectively. We measured the WC of the standing subjects with a piece of soft tape located between the lowest rib and the iliac crest (to the nearest 0.1 cm).
WWI was a new anthropometric index to assess adiposity by standardizing WC for weight and it was calculated with the following formula: WWI = WC (cm)/\(\sqrt {{{{{{{{\mathrm{weight}}}}}}}}{{{{{\rm{(kg)}}}}}}}\) [12]. BMI was calculated with the following formula: BMI = weight (kg)/height2 (m2). All patients were fasted for at least 12 h in the morning to collect blood from the antecubital vein. Quantitative analysis of fasting blood glucose (FPG), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), triglycerides (TG), electrolytes and renal functional indicators, etc. Hypertension was defined as diastolic blood pressure (DBP) of ≥90 mmHg, systolic blood pressure (SBP) of ≥140 mmHg, physician diagnosis, or current hypertension medication (defined by World Health Organization in 1999) [14].
Echocardiography measurements
A HP 5500 (Phillips Healthcare System, USA) or HDI 3000 (ATL, USA) color Doppler ultrasound diagnostic instrument was used to make M-mode, two-dimensional (2D) and color Doppler recordings from parasternal long-axis and short-axis Windows. 2D and color Doppler assessments were also performed from the apical window to produce 2, 3, and 4 chamber images. We also measured end-systolic diameter, end-diastolic diameter, interventricular septal thickness, and posterior left ventricular wall thickness. LV interior dimensions, interventricular septum, and posterior wall thickness were measured during three cardiac cycles, end-diastolic and systolic, as recommended by the American Society of Echocardiography [15]. Left ventricular mass (LVM) was calculated by using the following equation: 0.8 × 1.04[(IVS + LVEDD + PW)3 − LVEDD3] × 0.6. Interventricular septal thickness (IVS) is the interventricular septum, posterior wall thickness (PW) is the posterior wall, and left ventricular end-diastolic diameter (LVEDD) is left ventricular end-diastolic diameter. LVM was divided by height2.7 to obtain LVMI (LVMIh2.7). LVH was diagnosed with the criteria of LVM ≥ 49.2 gm−2.7 in males and 46.7 gm−2.7 in females [16]. Transthoracic echocardiography was performed by 2 echocardiographers trained in echocardiography at Fuwai Hospital, Chinese Academy of Medical Sciences [1].
Statistical analyses
SPSS 26.0 statistical software was used for data management and statistical analysis. According to the baseline WWI, the subjects were divided into four groups Q1(<10.16), Q2(10.16–10.67), Q3(10.68–11.19), and Q4(≥11.20), and the parameters of the four groups were compared. The Kolmogorov–Smirnoff test is used to check whether the data has a normal distribution. Data are reported as mean ± standard deviation for continuous variables and as percentages for categorical variables. The clinical variables and echocardiographic data of all subjects were grouped by WWI quartile, the continuous variables were analyzed by ANOVA, and the categorical variables were compared by chi-square test. Logistic regression analysis was used to calculate ORs and 95% CIs. The sequence model is established. Firstly, we refer to the previous high-quality literatures in related fields, summarize the confounding corrected by most literatures, and make the next adjustment as an alternative. Secondly, after we have determined the confounders that need to be adjusted and alternative, we can make the final confirmation of alternative confounders through the results of univariate analysis. Variables with statistical significance (P < 0.05) were included in subsequent models for analysis. However, because in univariate analysis, the differences between the results could not fully reflect the relationship between the alternative confounders and the study factors or outcomes. Because univariate analysis only makes a comparison between two variables, and ignores the influence of other effects. To reduce this effect, we can appropriately relax the P value threshold to 0.1, 0.2, or even 0.4, etc. In addition, although there is no significant difference in factor analysis, the real effect between them is likely to be underestimated, masked, or reinforced. Broadening the P value can include as many alternative confounders as possible. We adjusted these variables into the model according to the steps above. Model 1 is the unadjusted variable. In model 2, adjustments were made for age and sex. In addition to confounding factors analyzed in Model 2, pulse, BMI, WC, SBP, DBP FPG, alanine aminotransferase (ALT) and aspartate aminotransferase (AST), TC, TG, LDI-C, HDL-C, serum creatinine (SCr), serum uric acid (SUA), smoking, drinking, and coronary heart disease, diabetes, stroke history were adjusted in Model 3 on the basis of Model 2. In addition, the ORs and 95% CIs of LVH and WWI in each subgroup were obtained by stratified analysis according to sex, age and BMI. The differences were considered significant if a two-tailed P value is less than 0.05.
Results
Clinical characteristics of the study population
Table 1 shows the clinical and demographic characteristics of the study population by WWI categories: as compared with the lowest WWI category (<10.68 cm/√kg), the highest WWI category (≥11.25 cm/√kg) had higher age, female proportion, BMI, WC, SBP, DBP, FPG, ALT, TC, TG, LDL-C, SCr, SUA, but lower HDL-C. In terms of echocardiographic parameters, from Q1–Q4, IVST, RWT, and LVMI parameters increased significantly with increasing WWI (all P < 0.001). The prevalence of LVH was higher in patients in the highest quartile of WWI compared with patients in the lowest quartile of WWI. The prevalence of LVH was 34.1%, 38.4%, 42.2%, and 51.5%, respectively. As this study was conducted in a remote area of China in 2004, the local rural medical level was relatively backward at that time, and the awareness rate of hypertension, drug utilization rate, and control rate were low. Participants take a wide variety of antihypertensive drugs, most of which are proprietary Chinese medicines, and the proportion is low, less than 20%. The use of statins and antidiabetic drugs was also low, at less than 5.0% and 4.8%, respectively.
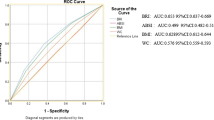
Association between WWI and LVH
Table 2 shows the association between WWI and the risk of LVH. As shown in Table 2, WWI was associated with an increased risk of LVH in univariate analysis (Model 1). After adjustment for age and sex (Model 2) and further adjustment for pulse rate, BMI, WC, SBP, DBP, FPG, ALT, AST, TC, TG, LDL-C, HDL-C, SCr, SUA, and smoking, drinking, coronary heart disease, diabetes, stroke history (model 3), WWI and LVH remained independently associated. Compared with the lowest WWI category Q1(<10.16 cm/√kg), a WWI of Q2(10.16–10.67)cm/√kg, Q3(10.68–11.19) cm/√kg increased the probability of LVH (OR 1.33, 95% CI 1.08–1.63) and 1.50 (1.19–1.89), as did the highest WWI category (≥11.20 cm/√kg) (OR 2.28, 95% CI 1.74–2.99). We further check the multicollinearity for WC and WWI. The results showed that there were free from excessive collinearity. In addition, we found that the prevalence of LVH increased with WWI quartiles in all models (P for trend < 0.001).
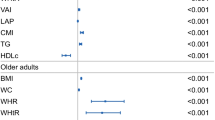
Subgroup analyses for association between WWI and LVH
The association between the highest WWI category (≥11.20 cm/√kg) and the risk of LVH was evaluated by the subgroups sex, age, and BMI, with the lowest WWI category (<10.16 cm/√kg) as the reference. After controlling for all covariates except for the stratified variable, the relationship between WWI and LVH remained in nearly every subgroup analysis, but was not significant at male (Fig. 2). In addition, we conducted an interaction analysis of the WWI quartile with each stratified factor and found no interaction between them.
Discussion
We conducted a cross-sectional study to analyze the association between WWI and LVH risk in hypertensive patients. The major finding is that the prevalence of LVH increased with WWI quartiles and that there was a significant correlation between WWI and LVH. This association was independent of sex, age, lifestyle, BMI, WC, and various cardiovascular and cerebrovascular risk factors. The stratified analysis also explored whether the relationship between WWI and LVH was influenced by gender. In fact, the relationship between WWI and LVH was more significant in female than in male. The underlying mechanism is currently unknown, but one possible explanation could be the effect of sex hormones, or it could be caused by differences in fat distribution between men and women. In addition, the proportion of males and females involved in the study is not balanced, with men far less than women, resulting in the limited statistical power of men in this study. The ASIAN-HF registry also showed gender differences. The study demonstrated that females with heart failure are more likely to have concentric left ventricular geometry than males [17]. A previous study showed found that lower estradiol levels and higher testosterone/estradiol ratios were associated with an increased risk of heart failure, which is more common in older women [18]. Decreased estradiol during menopause may affect vascular and cardiac remodeling processes, resulting in different heart failure phenotypes [19]. Our results provide new insights into the pathophysiology of LVH in men and women and provide new impetus for further research. Finally, we stratified study subjects by age and BMI, and the associations persisted.
LVH refers to cardiac enlargement characterized by cardiomyocyte hypertrophy and fibrous connective tissue hyperplasia. LVH is one of the most common heart damages associated with high blood pressure and can increase the risk of heart failure [3, 4]. However, so far, the pathogenesis of LVH is not fully understood, which may be related to age, sex, weight, race, genetic susceptibility, metabolic status (such as insulin resistance), hypertension, etc. It has been proposed that there is an inverse relationship between insulin sensitivity and LV wall thickness in subjects with essential hypertension [20, 21]. Leptin also increases the activity of extracellular matrix metalloproteinases, can induce interstitial fibrosis, and is involved in the inflammatory response during the development of LVH [22]. Disruption of the leptin signaling pathway within the heart causes LVH [23].
Obesity is a major public health problem worldwide [24]. The prevalence of obesity has increased dramatically worldwide over the last decades and nearly a third of the world’s population now classified as overweight or obese [25]. Obesity can increase the risk of diabetes, several cancers, and cardiovascular disease, and has also been found to be an independent risk factor for congestive heart failure [26,27,28]. Previous studies have shown that obesity is a risk factor for LVH and an early marker of myocardial damage in obese people [29,30,31,32]. In recent years, several studies have found that there is a positive correlation between obesity and left ventricular mass. According to the calculation method of left ventricular mass index, the incidence of LVH in obese patients ranged from 9.5% to 48.4% [33]. Obese patients are often accompanied by increased blood volume, decreased peripheral vascular resistance, and increased heart rate, which together lead to increased stroke volume, ultimately manifested as increased cardiac output and volume load. The increase in volume and pressure load will further increase the cardiomyocyte volume, change the cardiomyocyte volume, change the collagen matrix composition, and ultimately lead to LVH [34]. The mechanism of obesity-related LVH has not been fully elucidated, and it is believed that it is mainly caused by hemodynamic factors and neurohumoral factors [34, 35]. Different adipose tissues have different effects on the diseases. Visceral adipocytes have high lipolysis activity and anti-lipolysis effect of insulin, and can secrete inflammatory factors that act on blood vessels. With the increase of visceral fat, tumor necrosis factor-α, interleukin-6, C-reactive protein and other cytokines increased significantly, which can promote insulin secretion and induce pancreatic β-cell apoptosis. These factors may be involved in the process of LV remodeling hypertrophy, suggesting that visceral fat accumulation is associated with LVH.
WWI is a novel weight and waist-based obesity index with good predictive power for heart disease incidence and mortality in the Korean population [12]. Li et al. recently reported that WWI was significantly associated with an increased risk of hypertension in a rural Chinese cohort study [36]. A recent study showed that WWI is positively associated with fat mass and negatively associated with muscle mass in older adults [11]. A recent prospective study of our own showed that WWI was associated with all-cause mortality in elderly Chinese [37]. The current study verified the association between this index and LVH in Chinese adults with hypertension. The index is simple to operate, economical, and practical. It can be applied at all levels of medical and healthcare facilities, especially in areas that lack medical standards or require large-scale data research. Therefore, for people with high WWI, early assessment of target organ damage and initiation of treatment can reduce the risk of cardiovascular and cerebrovascular diseases and improve the prognosis.
Although our study recruited a large number of hypertensive patients and effectively reduced selection bias, it still had some limitations. Prospective follow-up and intervention studies were not performed in the cross-sectional study. High WWI is independently correlated with LVH, suggesting that obesity may lead to the occurrence and development of LVH. However, the causal relationship between WWI and LVH cannot be conclusively concluded. The proportion of male subjects in this study was relatively low (33.8%). Therefore, the effect of gender on the association between WWI and LVH needs to be further elucidated by expanding the proportion of male subjects.
Conclusion
In this study, WWI was independently associated with LVH, especially in females, suggesting that WWI can be used to identify patients at high risk for LVH in hypertensive populations.
Data availability
The research data used to support the finding of this study are available from the corresponding authors upon request.
References
Wang SX, Xue H, Zou YB, Sun K, Fu CY, Wang H, et al. Prevalence and risk factors for left ventricular hypertrophy and left ventricular geometric abnormality in the patients with hypertension among Han Chinese. Chin Med J. 2012;125:21–26.
Prisant LM. Hypertensive heart disease. J Clin Hypertens. 2005;7:231–8.
Maimaitiaili R, Teliewubai J, Zhao S, Tang J, Chi C, Zhang Y, et al. Relationship between vascular aging and left ventricular concentric geometry in community-dwelling elderly: the Northern Shanghai Study. Clin Interv Aging. 2020;15:853–63.
Yildiz M, Oktay AA, Stewart MH, Milani RV, Ventura HO, Lavie CJ. Left ventricular hypertrophy and hypertension. Prog Cardiovas Dis. 2020;63:10–21.
Palmieri V, Devereux RB, Hollywood J, Bella JN, Liu JE, Lee ET, et al. Association of pulse pressure with cardiovascular outcome is independent of left ventricular hypertrophy and systolic dysfunction: the Strong Heart Study. Am J Hypertens. 2006;19:601–7.
Wang S, Xue H, Zou Y, Sun K, Fu C, Wang H, et al. Left ventricular hypertrophy, abnormal ventricular geometry and relative wall thickness are associated with increased risk of stroke in hypertensive patients among the Han Chinese. Hypertens Res. 2014;37:870–4.
Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918.
Imahori Y, Mathiesen EB, Morgan KE, Frost C, Hughes AD, Hopstock LA, et al. The association between anthropometric measures of adiposity and the progression of carotid atherosclerosis. BMC Cardiovas Disord. 2020;20:138.
Gottdiener JS, Kop WJ. Body and heart: effects of weight gain and loss on left ventricular size and function. Circ Cardiovasc Imaging. 2017;10:e006084.
Pierdomenico SD, Cuccurullo F. Risk reduction after regression of echocardiographic left ventricular hypertrophy in hypertension: a meta-analysis. Am J Hypertens. 2010;23:876–81.
Kim NH, Park Y, Kim NH, Kim SG. Weight-adjusted waist index reflects fat and muscle mass in the opposite direction in older adults. Age Ageing. 2021;50:780–6.
Park Y, Kim NH, Kwon TY, Kim SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep. 2018;8:16753.
Cai S, Dong J, Cheng B, Zhang A, Sun J, Li M, et al. Relationship of a new anthropometric index with left ventricular hypertrophy in hypertensive patients among the Han Chinese. BMC Cardiovasc Disord. 2022;22:16.
Chalmers J, MacMahon S, Mancia G, Whitworth J, Beilin L, Hansson L, et al. 1999 World Health Organization-International Society of Hypertension Guidelines for the management of hypertension. Guidelines sub-committee of the World Health Organization. Clin Exp Hypertens. 1999;21:1009–60.
Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978;58:1072–83.
de Simone G, Devereux RB, Daniels SR, Koren MJ, Meyer RA, Laragh JH. Effect of growth on variability of left ventricular mass: assessment of allometric signals in adults and children and their capacity to predict cardiovascular risk. J Am Coll Cardiol. 1995;25:1056–62.
Chandramouli C, Teng TK, Tay WT, Yap J, MacDonald MR, Tromp J, et al. Impact of diabetes and sex in heart failure with reduced ejection fraction patients from the ASIAN-HF registry. Eur J Heart Fail. 2019;21:297–307.
Zhao D, Guallar E, Ouyang P, Subramanya V, Vaidya D, Ndumele CE, et al. Endogenous sex hormones and incident cardiovascular disease in post-menopausal women. J Am Coll Cardiol. 2018;71:2555–66.
Nagai M, Förster CY, Dote K, Shimokawa H. Sex hormones in heart failure revisited? Eur J Heart Fail. 2019;21:308–10.
Watanabe K, Sekiya M, Tsuruoka T, Funada J, Kameoka H. Effect of insulin resistance on left ventricular hypertrophy and dysfunction in essential hypertension. J Hypertens. 1999;17:1153–60.
Anan F, Yonemochi H, Masaki T, Takahashi N, Fukunaga N, Teshima Y, et al. High-density lipoprotein cholesterol and insulin resistance are independent and additive markers of left ventricular hypertrophy in essential hypertension. Hypertens Res. 2007;30:125–31.
Alpert MA, Karthikeyan K, Abdullah O, Ghadban R. Obesity and cardiac remodeling in adults: mechanisms and clinical implications. Prog Cardiovasc Dis. 2018;61:114–23.
Raju SV, Zheng M, Schuleri KH, Phan AC, Bedja D, Saraiva RM, et al. Activation of the cardiac ciliary neurotrophic factor receptor reverses left ventricular hypertrophy in leptin-deficient and leptin-resistant obesity. Proc Natl Acad Sci USA. 2006;103:4222–7.
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health effects of overweight and obesity in 195 countries over 25 Years. N Engl J Med. 2017;377:13–27.
Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10.
Singh GM, Danaei G, Farzadfar F, Stevens GA, Woodward M, Wormser D, et al. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: a pooled analysis. PLoS ONE. 2013;8:e65174.
Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. Body fatness and cancer-viewpoint of the IARC Working Group. N Engl J Med. 2016;375:794–8.
Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, et al. Obesity and the risk of heart failure. N Engl J Med. 2002;347:305–13.
Hammond IW, Devereux RB, Alderman MH, Laragh JH. Relation of blood pressure and body build to left ventricular mass in normotensive and hypertensive employed adults. J Am Coll Cardiol. 1988;12:996–1004.
Lauer MS, Anderson KM, Kannel WB, Levy D. The impact of obesity on left ventricular mass and geometry. The Framingham Heart Study. JAMA. 1991;266:231–6.
Alpert MA, Lambert CR, Terry BE, Cohen MV, Mukerji V, Massey CV, et al. Influence of left ventricular mass on left ventricular diastolic filling in normotensive morbid obesity. Am Heart J. 1995;130:1068–73.
Li X, Li S, Ulusoy E, Chen W, Srinivasan SR, Berenson GS. Childhood adiposity as a predictor of cardiac mass in adulthood: the Bogalusa Heart Study. Circulation. 2004;110:3488–92.
Booysen HL, Woodiwiss AJ, Sibiya MJ, Hodson B, Raymond A, Libhaber E, et al. Indexes of aortic pressure augmentation markedly underestimate the contribution of reflected waves toward variations in aortic pressure and left ventricular mass. Hypertension. 2015;65:540–6.
Lavie CJ, Arena R, Alpert MA, Milani RV, Ventura HO. Management of cardiovascular diseases in patients with obesity. Nat Rev Cardiol. 2018;15:45–56.
Schütten MT, Houben AJ, de Leeuw PW, Stehouwer CD. The link between adipose tissue renin-angiotensin-aldosterone system signaling and obesity-associated hypertension. Physiology. 2017;32:197–209.
Li Q, Qie R, Qin P, Zhang D, Guo C, Zhou Q, et al. Association of weight-adjusted-waist index with incident hypertension: The Rural Chinese Cohort Study. Nutr Metab Cardiovasc Dis. 2020;30:1732–41.
Cai S, Zhou L, Zhang Y, Cheng B, Zhang A, Sun J, et al. Association of the weight-adjusted-waist index with risk of all-cause mortality: a 10-year follow-up study. Front Nutr. 2022;9:894686.
Acknowledgements
We would like to thank the researchers and study participants for their contributions.
Funding
This work was supported by the National Key Research and Development Program of China (2020YFC2008900), the National Defense Science and Technology Innovation Special Zone Project (19-163-15-ZD-009-001-10), and the Key Projects of Logistics Scientific Research Project of Chinese PLA (19BJZ30), the Military Medical Youth Growth Project of PLA General Hospital (Funding No. QNC19005), which contributed to the data collection job.
Author information
Authors and Affiliations
Contributions
SW, XL, and SC designed the research. SC, TZ, YD, BC, and AZ, collected the data. SC, TZ, and YD wrote the paper. JS, ML, and QB help optimize the research and proofread the paper. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval and consent to participate
The study protocol was reviewed and approved by the ethical committees of the Fuwai Hospital and local hospitals. The research procedures followed the ethically normative criteria. Written informed consent to participate in the study was obtained from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cai, S., Zhu, T., Ding, Y. et al. The relationship between the weight-adjusted-waist index and left ventricular hypertrophy in Chinese hypertension adults. Hypertens Res 46, 253–260 (2023). https://doi.org/10.1038/s41440-022-01075-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-01075-z
- Springer Nature Singapore Pte Ltd.
Keywords
This article is cited by
-
Association of weight-adjusted waist index with all-cause mortality among non-Asian individuals: a national population-based cohort study
Nutrition Journal (2024)
-
The association between weight-adjusted waist circumference index and cardiovascular disease and mortality in patients with diabetes
Scientific Reports (2024)
-
Association between the weight-adjusted-waist index and circadian syndrome in findings from a nationwide study
Scientific Reports (2024)
-
Association of weight-adjusted waist index with cardiovascular disease and mortality among metabolic syndrome population
Scientific Reports (2024)
-
2023 update and perspectives
Hypertension Research (2024)