Abstract
In Black populations excessive salt intake may exacerbate the genetic predisposition to hypertension and promote the early onset of cardiovascular disease. Ethnic differences in the interaction between sodium intake and the metabolome may play a part in hypertension and cardiovascular disease development. We determined (1) urinary amino acid and acylcarnitine profiles of young Black and White adults according to low, moderate, and high dietary salt intake, and (2) investigated the triad of salt intake, systolic blood pressure (SBP), and the associated metabolomics profile. This study included 447 White and 380 Black adults aged 20–30 years from the African-PREDICT study. Estimated salt intake was determined from 24-hour urinary sodium levels. Urinary amino acids and acylcarnitines were measured using liquid chromatography-tandem mass spectrometry. Black adults exhibited no significant differences in SBP, amino acids, or acylcarnitines across low (<5g/day), moderate (5–10g/day), and high (>10g/day) salt intake. White adults with a high salt intake had elevated SBP compared to those with low or moderate intakes (p < 0.001). Furthermore, gamma-aminobutyric acid (GABA) (q = 0.020), citrulline (q = 0.020), glutamic acid (q = 0.046), serine (q = 0.054) and proline (q = 0.054) were lowest in those with higher salt intake. Only in White and not Black adults did we observe inverse associations of clinic SBP with GABA (Adj. R2 = 0.34; Std. β = −0.133; p = 0.003), serine (Adj. R2 = 0.33; Std. β = −0.109; p = 0.014) and proline (Adj. R2 = 0.33; Std. β = −0.109; p = 0.014). High salt intake in White, but not in black adults, were related to metabolomic changes and may contribute to pathophysiological mechanisms associated with increased BP.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) can be ascribed to genetic, environmental, and behavioural risk factors [1, 2]. Elevated systolic blood pressure (SBP) and dietary habits are the two top-ranked modifiable risk factors contributing to the high burden of CVD [1]. An estimated 7.94 million CVD-related deaths and 188 million disability-adjusted life years have been attributed to dietary risk factors [1], with a high sodium intake being a primary culprit [3].
While dietary salt intake is regarded as a behavioural risk factor, its role in CVD development also encompasses genetic susceptibility whereby BP is elevated in response to increased salt intake, which is known as salt sensitivity [4]. Salt sensitivity is frequently observed in Black ethnic groups [4, 5], and has been attributed to genetic factors such as divergent renal sodium handling [4]. In Black individuals excessive salt intake exacerbates this genetic predisposition and promotes the early onset of hypertension and CVD [6].
Excessive salt intake further increases the risk of hypertension and CVD irrespective of ethnicity through mechanisms such as increased sympathetic activity, hormonal responses, oxidative stress, and the gut microbiome [7]. Coinciding metabolic changes related to these mechanisms may result in the up- or downregulation of various metabolites. Sodium reduction has been associated with increased short-chain fatty acid [8], acylcarnitine [9], and organic and amino acid levels [9,10,11]. The metabolomic changes were subsequently associated with improved endothelial function [10] and reduced blood pressure [8, 11].
Ethnic differences in the interaction between diet and the metabolome may play an integral part in the susceptibility, incidence, progression, and severity of hypertension and CVD development. This study (1) aimed to determine the amino acid and acylcarnitine profiles of Black and White populations in relation to dietary salt intake, and (2) investigated the triad of salt intake, SBP, and the associated metabolomics profile.
Methods
The African Prospective study on the Early Detection and Identification of Cardiovascular Disease and Hypertension (African-PREDICT) aims to identify lifestyle behaviours and known and novel biomarkers that may be implicated in the development of hypertension. The African-PREDICT study recruited 1202 participants from communities in and around the Potchefstroom area in the North-West Province of South Africa [12]. This study included 380 Black and 447 White participants with urinary amino acid, acylcarnitine as well as complete 24-hour urinary data (volume ≥300mL and 24-hour urinary creatinine for men: ≤6 and ≥30 mmol/day; and for women: ≤4 and ≥25 mmol/day) (Fig. 1). Inclusion criteria were 20–30 years of age, screening clinic BP <140/90 mmHg, no self-reported chronic diseases or treatment thereof, HIV uninfected, not pregnant or lactating. Despite the BP screening criteria for African-PREDICT 18 participants had clinic SBP ≥140 mmHg with normal DBP, 46 participants had clinic DBP ≥90 mmHg with normal SBP, and 20 participants had clinic BP ≥140/90 when clinic BP was taken on the day of other study measurements. While some participants from the African-PREDICT study have white coat or masked hypertension based on BP reading we did not focus on HT status in this study.
All participants gave written informed consent. The African-PREDICT study complies with the Declaration of Helsinki, was approved by the Health Research Ethics Committee of the North-West University (NWU-00001-12-A1) and is registered on ClinicalTrials.gov (NCT03292094).
Questionnaire data
Sex and ethnicity data were obtained from a General Health Questionnaire. Data on dietary protein intake was obtained by means of three 24-hour dietary recall interviews using a standardized dietary collection kit (example pictures, packages, measurement tools and food models) and the five-step multiple-pass approach. The data was coded according to the South African Medical Research Council Food Composition Tables and the Food Quantities Manual was used to convert household measures to grams. Nutrient and food analysis of the dietary data was conducted by the South African Medical Research Council at the Biostatistics Unit.
Anthropometric, and physical activity data
Researchers were trained to measure weight (kg) (SECA electronic scales, SECA, Birmingham, UK), height (m) (SECA stadiometer, SECA, Birmingham, UK) and waist circumference (anthropometric nonflexible tape measure, Holtain, Ltd, Crymych, UK). All three variables were measured in triplicate, and the mean height and weight used to calculate body mass index (BMI) using the standard weight (kg)/height (m2) formula. Participants wore a triaxial accelerometer for seven days, during which total energy expenditure (TEE) was measured as an estimate of participants’ physical activity (ActiHeart; CamNtech, Cambridge, UK) and was corrected for body mass.
Blood pressure measures
Appropriately sized brachial cuffs were fitted to participants. Clinic BP was measured in duplicate on the right and left arms, with the arm rested at heart level (Dinamap Procare 100 Vital Signs Monitor, GE Medical Systems, Milwaukee, USA). We reported clinic BP as the average of all four measurements.
Biochemical analyses
Participants fasted from 22:00 on the evening prior to the day of the study. Early morning spot urine samples were taken, and a registered nurse collected blood samples from the antebrachial vein using a sterile winged infusion set and syringes. Samples were immediately taken to the onsite laboratory for preparation and storage at −80 °C. Twenty-four-hour urine samples were collected according to the Pan American Health Organization/WHO protocol for population-level sodium determination in 24-hour urine samples [13]. After discarding the first passed urine, participants collected all urinary voids in a 5 L container. Urine was stored in a cool place until a researcher came to collect the 5L container from participants. Twenty-four-hour urinary volume was measured, whereafter samples were aliquoted into cryovials for storage also at −80 °C.
Total cholesterol, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglycerides, creatinine, and gamma-glutamyl transferase (GGT) were measured in serum and glucose in sodium fluoride plasma (Cobas Integra, 400plus, Roche, Basel Switzerland). Insulin was determined from serum using the Electrochemiluminescence method on the E411 (Roche, Basel Switzerland). Serum creatinine was used to determine the estimated glomerular filtration rate (eGFR) using the Chronic Kidney Disease Epidemiology equation (CKD-EPI) (without the race component) [14]. Twenty-four-hour urinary sodium and potassium were measured using ion-selective electrode potentiometry, and creatinine with the Creatinine Jaffé Gen.2 reagent (Cobas Integra, 400plus, Roche, Basel Switzerland). Completeness for 24-hour urine samples was based on urine volume (volume ≥300 mL) and 24-hour urinary creatinine (men: ≤6 and ≥30 mmol/day; women: ≤4 and ≥25 mmol/day) [15].
We have previously published detailed methodology on the metabolomic analyses done in the African-PREDICT study [16]. Amino acids and acylcarnitines were measured from spot urine samples using liquid chromatography-tandem mass spectrometry (LC-MS/MS) (Agilent 6410 LC-MS/MS system with 1200 series LC front-end). We applied a 50% CV filter to the data, and metabolites with more than 50% zero values were removed from the data matrix.
Statistical analyses
Statistical analyses were performed using SPSS version 27 (IBM, Armonk, New York, USA), and figures were created with GraphPad Prism version 8.4.3 (GraphPad software Inc., La Jolla, California, USA). Data for continuous variables that were not normally distributed were logarithmically transformed. Basic characteristics of Black and White adults were compared across low (<5 g/day), moderate (5–10 g/day), and high (>10 g/day) salt intake groups using Welch analysis of variance (ANOVA). The current recommendation of the World Health Organization is less than 5 g salt per day, with most adults consuming almost double [17]. Therefore, increasing increments of 5 grams salt was used to define groups. Data for animal protein intake remained skew despite logarithmic transformation, therefore we performed a nonparametric Kruskal-Wallis H test to compare animal protein intake across salt intake groups. To lower the false discovery rate of statistically significant metabolites as a result of performing multiple comparisons, we calculated the adjusted p values using the Benjamini–Hochberg procedure (reported as q values). We additionally performed Pearson correlations, and partial and linear regression analyses to demonstrate the relationship of estimated salt intake with clinic SBP and significant metabolites (identified using ANOVA). Age, WC, BMI, TEE, total cholesterol, HDL-C, LDL-C, triglycerides, glucose, insulin, eGFR, and GGT were considered as covariates for linear and stepwise multiple regression models. We ultimately included age, WC, TEE, triglycerides, glucose, eGFR, and GGT into backward stepwise multiple regression models based on the strongest bivariate correlations with SBP measures and metabolites. As a sensitivity analyses, we repeated ANOVA with participants stratified according to sex, and included sex as a covariate in linear regression models.
Results
Table 1 demonstrates the characteristics of Black and White adults across low to high salt intake. In Black adults, clinic BPs were similar across salt intake groups (p trend > 0.05). In White participants, the high salt intake group had a higher clinic SBP than those in the low or moderate intake groups (p trend < 0.001). Anthropometric measures (p trend < 0.001), total (p trend = 0.004) and animal protein intake (p trend = 0.020) increased with an increase in estimated salt intake in White adults only.
When we compared thirty-five amino acids and acylcarnitines across salt intake groups, we found no significant differences in metabolite levels in Black adults (all p values > 0.05). In White adults however, we demonstrated lower GABA (p = 0.001), citrulline (p = 0.001), glutamic acid (p = 0.004), serine (p = 0.006), proline (p = 0.008), aspartic acid (p = 0.023), arginine (p = 0.026), dimethylglycine (p = 0.037) and glycine (p = 0.049) with increased salt intake. After using the Benjamini–Hochberg procedure, GABA (q = 0.020), citrulline (q = 0.020) and glutamic acid (q = 0.046) remained significantly different between the salt intake groups (Table 2). Additionally, White adults in the high salt intake group had attenuated levels of proline (q = 0.042) and serine (q = 0.042) compared to those in the low intake group.
Relationship between estimated salt intake and metabolites
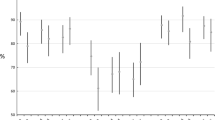
We subsequently performed Pearson (Fig. 2) and partial correlations to determine relationships between the identified metabolites and estimated salt intake in the Black and White groups. In Black adults, estimated salt intake correlated negatively with proline (r = −0.107; p = 0.037). In White adults we confirmed inverse relationships of estimated salt intake with GABA (r = −0.140; p = 0.004), citrulline (r = −0.134; p = 0.011), glutamic acid (r = −0.098; p = 0.038) and serine (r = −0.107; p = 0.024), and a borderline significant correlation with proline (r = 0.086; p = 0.069). The negative correlations of estimated salt intake with GABA and citrulline persisted after partial adjustment for either age, WC, TEE, or animal protein intake. The correlations of estimated salt intake with serine lost significance when adjusting for animal protein intake, and with glutamic acid when adjusting for TEE or animal protein intake. With partial adjustment for clinic SBP, all relationships between estimated salt intake and metabolites became non-significant (Supplementary Table 1).
Relationship between systolic blood pressure and estimated salt intake
With Pearson analysis we observed positive correlations between estimated salt intake and clinic SBP in Black (r = 0.101; p = 0.049) and White adults (r = 0.230; p < 0.001) (Fig. 2). In Black adults the relationship between estimated salt intake and SBP became non-significant after adjusting for age, WC, and TEE (Adj. R2 = 0.026; Std. β = 0.079; p = 0.18). In White adults, however, the positive relationship between estimated salt intake and clinic SBP remained robust after adjusting for age, WC, TEE, glucose, triglycerides, GGT, eGFR, and animal protein intake (Model 4) (Adj. R2 = 0.35; Std. β = 0.142; p = 0.001) (Fig. 3). The relationship between estimated salt intake and clinic SBP was also independent of GABA, citrulline, glutamic acid, serine and proline.
Multiple regression analyses with clinic SBP as the dependent variable and identified metabolites as well as estimated salt intake as the main independent variables. Model 1: adjusted for waist circumference and total energy expenditure. Model 2: adjusted for waist, circumference, total energy expenditure, glucose and triglycerides, λ-glutamyl transferase. Model 3: adjusted for waist, circumference, total energy expenditure, glucose, triglycerides, λ-glutamyl transferase and estimated glomerular filtration rate. Model 4: adjusted for waist, circumference, total energy expenditure, glucose and triglycerides, λ-glutamyl transferase, estimated glomerular filtration rate and animal protein intake
Relationship between systolic blood pressure and metabolites
In the following analyses we determined whether clinic SBP was related to metabolites that differed significantly across salt intake groups. Only in White, and not Black adults, did we observe significant negative correlations between SBP and amino acids (GABA, serine, and proline) after multivariable adjusted analyses (Fig. 3). In the White group only, inverse association of clinic SBP with GABA (Adj. R2 = 0.34; Std. β = −0.133; p = 0.003), serine (Adj. R2 = 0.33; Std. β = −0.109; p = 0.014) and proline (Adj. R2 = 0.33; Std. β = −0.109; p = 0.014) persisted with linear regression analyses after adjusting for age, WC, TEE, glucose, GGT, triglycerides, and eGFR, and a borderline significant association with glutamic acid (Adj. R2 = 0.33; Std. β = −0.083; p = 0.063). These negative associations were substantiated with backward stepwise multiple regression analyses for GABA (Adj. R2 = 0.35; Std. β = −0.135; p = 0.002), serine (Adj. R2 = 0.34; Std. β = −0.110; p = 0.011), proline (Adj. R2 = 0.34; Std. β = −0.111; p = 0.010) and glutamic acid (Adj. R2 = 0.34; Std. β = −0.085; p = 0.049). When NaCl or animal protein intake was added to linear regression models, the negative association of clinic SBP with GABA (Adj. R2 = 0.36; Std. β = −0.114; p = 0.012) (Adj. R2 = 0.35; Std. β = −0.120; p = 0.009), serine (Adj. R2 = 0.35; Std. β = −0.091; p = 0.038) (Adj. R2 = 0.34; Std. β = −0.092; p = 0.040) and proline (Adj. R2 = 0.35; Std. β = −0.096; p = 0.030) (Adj. R2 = 0.34; Std. β = −0.91; p = 0.047) remained robust.
Sensitivity analyses for sex
When stratified according to sex, we found that the reduction of metabolite levels with increased salt intake in the White group was particularly evident in women (Supplementary Table 2). Although dimethylglycine, serine, proline, glutamic acid, GABA and citrulline had a p trend <0.05 across increasing salt intake groups in White women, all q values were >0.05. Notably sex also had a significant confounding effect on the relationships observed between clinic SBP, estimated salt intake and metabolites (GABA, serine, and proline) (Fig. 3).
Discussion
In this study we investigated the triad of salt intake, clinic SBP and the associated metabolomics profile. We found that in White, but not Black adults, a high salt intake associated with a unique metabolomics profile consisting of lower levels of GABA, glutamic acid, serine, and proline (Fig. 4)––which in turn were related to elevated SBP. Furthermore, in White adults only, estimate salt intake associate positively with clinic SBP after multiple adjustments. Although the relationship between estimated salt intake and clinic SBP was independent of identified metabolites we still postulate that lower levels of these amino acids––related to increased salt intake––may play a contributing role in pathophysiological mechanisms whereby excessive salt intake increases SBP in White individuals.
Metabolomics profile of Black adults in relation to dietary salt intake
Despite Black ethnicity being associated with salt sensitivity we did not observe significant differences in clinic SBP, amino acids or acylcarnitines across low to high salt intake groups. Additionally, the observed correlations of estimated salt intake with clinic SBP, and GABA were non-significant after adjusting for WC and TEE expenditure, suggesting that the latter relationship are dependent on central adiposity and physical activity. Given that WC, BMI and TEE were similar across salt intake groups, it may explain the lack of a significant increase in SBP with higher salt intake. Using targeted metabolomics, this study only measured amino acids and acylcarnitines. The likelihood of salt intake influencing other metabolite classes such as organic compounds, phospholipids, sphingolipids, advanced glycation end-products and others––all linked to arterial stiffness [18]––cannot be disregarded. An untargeted metabolomics approach in future studies may help identify other metabolite classes affected by salt intake in Black ethnic groups. Arterial stiffness and early vascular aging are hallmark cardiovascular risk factors associated with Black ethnicity, and can precede marked BP changes [19, 20]. Our research group have previously demonstrated independent associations of arterial stiffness with β-alanine, 1-methyl-histidine, L-proline, threonic acid and malonic acid in Black but not White boys (6–8 years of age) [21]. Further investigations into possible relationships between amino acids, acylcarnitines and arterial stiffness are required.
Metabolomics profile of White adults in relation to dietary salt intake
Glutamic acid, serine and proline are glucogenic acids that can be converted to glucose via gluconeogenesis [22]––a metabolic pathway associated with reduced insulin sensitivity and type 2 diabetes mellitus (T2DM) [23]. Given the health status of this study cohort, it is an alluring prospect that the early changes in the glucogenic metabolites associated with a high salt intake, could reflect the initial stages of a harmful continuum ranging from increased gluconeogenesis to hyperinsulinemia, insulin resistance, hyperglycaemia, and ultimately the development of T2DM. Considering the higher BMI and WC with excessive salt intake in the White group, central obesity may play an important role. Although not the focus of this article, we did indeed find negative correlations between glucogenic metabolites (glutamic acid, serine, and proline) and glucose in our cohort (Supplementary Table 4). There is also some evidence that the role of gluconeogenesis in the aetiology of insulin resistance may be ethnic-specific [24]. Chung et al., showed that Black women had a 10% lower rate of gluconeogenesis despite similar age, BMI, and whole-body insulin sensitivity than their White counterparts. The authors suggest that while increased gluconeogenesis may be a hallmark of insulin resistance in Whites, it may not be the case for Black ethnic groups [24].
We also observed an increase in animal protein intake with a higher salt intake. This is in line with a positive correlation reported between animal protein intake and sodium from a recent study that evaluated the nutritional contents of 971 foods from the South African Food Composition Database [25]. While it is known that dietary protein intake affects endogenous metabolite levels, it was beyond the scope of this article. We did, however, find that animal protein intake influenced the relationship of salt intake with glutamic acid, serine, and proline. Still, the marked reduction in glutamic acid, serine, and proline with excessive salt intake, be it due to the high sodium content associated with animal protein intake or not, remains of interest.
Metabolite markers and blood pressure
GABA and glutamic acid
Glutamic acid (glutamate) and GABA are major excitatory and inhibitory neurotransmitters in the central nervous system that play a role in BP regulation [26]. In White adults, lower levels of sympathoinhibitory GABA, associated with a high salt intake, may increase clinic SBP by means of increased sympathetic activity. A recent review by Ngo et al., additionally highlighted not only the anti-hypertensive properties of GABA, but also the antioxidative, anti-inflammatory, anti-diabetic, hepatic––and reno-protective effects thereof [27].
Although a positive relationship between SBP and glutamic acid could be expected based on the notion that glutamic acid/glutamate promotes sympathetic outflow, we observed an inverse relationship with unadjusted analyses. Accordingly negative relationships between SBP and glutamic acid were also reported for findings from the INTERMAP study [28] and the Twins UK registry [29]. This relationship in our study, however, was significantly influenced by WC and physical activity. Stemler et al. suggested that the inverse association between SBP and glutamate may be attributed to glutamate being a substrate for arginine, a precursor of nitric oxide (NO) which promotes vasodilation. Glutamate itself, however, can also increase the bioavailability of NO by activating neuronal nitric oxide synthase (nNOS) [30]. The inhibition of nNOS in healthy men (24 ± 4 years) has been reported to increase mean arterial pressure and systemic vascular resistance [31]. Conversely, there is also evidence that nNOS activation by glutamate may promote oxidative stress and vasoconstriction [30].
Serine and proline
White adults from our study with a habitual daily salt intake >10g/day had significantly lower levels of serine and proline compared with those consuming <5g salt/day. The inverse relationships of serine and proline with SBP in White adults from this study again correspond with findings from the INTERMAP study mentioned earlier [28]. Higher levels of serine are also associated with a lower risk of developing hypertension [32, 33]. Elevated L-serine may play an antihypertensive role by promoting endothelium-dependent vasodilation. In vitro, L-serine was shown to exhibit antioxidative and cytoprotective properties by promoting nuclear factor erythroid 2 related factors or activity, heme-oxygenase-1 expression and NO production [34]. Lower serine levels, associated with increased salt intake, may therefore increase SBP by means of impaired endothelial vasodilation in White adults.
In contrast with our findings and that of the INTERMAP study, Teymoori et al., reported a greater risk of incident hypertension associated with increased proline intake [35]. Proline plays an important role in maintaining healthy collagen turnover and stability [36]. It is possible that alterations in proline metabolism may contribute to adverse collagen turnover which promotes arterial stiffness and concurrently increases BP.
Strengths and limitations
Our study cohort of apparently healthy Black and White adults (aged 20–30 years) is larger than previously reported studies that have focused on metabolomics profiling and salt intake [8,9,10,11]. Since this study only recruited participants from the North West Province of South Africa the results may not be reflective of the South-African population in its entirety. We made use of a targeted metabolomics approach to measure predetermined metabolite groups (amino acids and acylcarnitines). Future studies may use untargeted metabolomics to determine whether other metabolite groups such as organic acids, not included in our study, are affected by salt intake. While multiple 24-hour urine samples are recommended to determine individual salt intake, the use of a single 24-hour urine sample to determine habitual population salt intake is sufficient [37].
Conclusion
In White adults, early metabolomic changes related to salt intake may contribute to an increased risk of hypertension and concurrently early CVD development. Our results suggest that the manner in which excessive salt intake promotes elevated SBP in White compared to Black adults may be mediated by different pathophysiological mechanisms.
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76:2982–3021.
Said MA, Verweij N, van der Harst P. Associations of combined genetic and lifestyle risks with incident cardiovascular disease and diabetes in the UK Biobank Study. JAMA Cardiol. 2018;3:693–702.
Qiao J, Lin X, Wu Y, Huang X, Pan X, Xu J, et al. Global burden of non-communicable diseases attributable to dietary risks in 1990-2019. J Hum Nutr Dietetics. 2022;35:202–13.
Schutte AE Ethnicity and cardiovascular disease. Textbook of Vascular Medicine: Springer; 2019. pp. 287-959
Elijovich F, Weinberger MH, Anderson CA, Appel LJ, Bursztyn M, Cook NR, et al. Salt sensitivity of blood pressure: a scientific statement from the American Heart Association. Hypertension. 2016;68:e7–e46.
Schutte AE, Botha S, Fourie CMT, Gafane-Matemane LF, Kruger R, Lammertyn L, et al. Recent advances in understanding hypertension development in sub-Saharan Africa. J Hum Hypertens. 2017;31:491–500.
He FJ, Tan M, Ma Y, MacGregor GA. Salt reduction to prevent hypertension and cardiovascular disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75:632–47.
Chen L, He FJ, Dong Y, Huang Y, Wang C, Harshfield GA, et al. Modest sodium reduction increases circulating short-chain fatty acids in untreated hypertensives. Hypertension. 2020;76:73–9.
Derkach A, Sampson J, Joseph J, Playdon MC, Stolzenberg-Solomon RZ. Effects of dietary sodium on metabolites: the Dietary Approaches to Stop Hypertension (DASH)-Sodium Feeding Study. Am. Clin Nutr. 2017;106:1131–41.
Jablonski KL, Klawitter J, Chonchol M, Bassett CJ, Racine ML, Seals DR. Effect of dietary sodium restriction on human urinary metabolomic profiles. Clin J Am Soc Nephrol. 2015;10:1227–34.
Chen L, He FJ, Dong Y, Huang Y, Harshfield GA, Zhu H. Sodium reduction, metabolomic profiling, and cardiovascular disease risk in untreated black hypertensives. Hypertension. 2019;74:194–200.
Schutte AE, Gona PN, Delles C, Uys AS, Burger A, Mels CM, et al. The African Prospective study on the Early Detection and Identification of Cardiovascular disease and Hypertension (African-PREDICT): Design, recruitment and initial examination. Eur. J Prev Cardiol. 2019;26:458–70.
WHO/PAHO Regional Expert Group for Cardiovascular Disease Prevention through Population‐wide Dietary Salt Reduction. Protocol for population level sodium determination in 24‐hour urine samples. World Health Organization Geneva, Switzerland; 2010.
Stevens LA, Claybon MA, Schmid CH, Chen J, Horio M, Imai E, et al. Evaluation of the Chronic Kidney Disease Epidemiology Collaboration equation for estimating the glomerular filtration rate in multiple ethnicities. Kidney Int. 2011;79:555–62.
Stolarz-Skrzypek K, Kuznetsova T, Thijs L, Tikhonoff V, Seidlerová J, Richart T, et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011;305:1777–85.
Strauss-Kruger M, Kruger R, Jansen Van Vuren E, Jacobs A, Louw R, Mels C Identifying a metabolomics profile associated with masked hypertension in two independent cohorts: Data from the African-PREDICT and SABPA studies. Hypertension Research 2022; https://doi.org/10.1038/s41440-022-01010-2.
World Health Organization. Guideline: Sodium intake for adults and children. World Health Organization; 2012.
Paapstel K, Kals J. Metabolomics of arterial stiffness. Metabolites. 2022;1212:370 https://doi.org/10.3390/metabo12050370.
Breet Y, Huisman HW, Kruger R, Van Rooyen JM, Gafane-Matemane LF, Ware LJ, et al. Pulse pressure amplification and its relationship with age in young, apparently healthy black and white adults: the African-PREDICT study. 2017; 249:387-91.
Mokwatsi GG, Schutte AE, Kruger R. Ethnic differences regarding arterial stiffness of 6‐8‐year-old black and white boys. J Hypertens. 2017;35:960–67.
Erasmus D, Mels CM, Louw R, Lindeque JZ, Kruger RJP. Urinary metabolites and their link with premature arterial stiffness in black boys: the ASOS study. Pulse. 2018;6:144–53.
Rédei GP Glucogenic Amino Acids. In: Rédei GP, editor. Encyclopedia of genetics, genomics, proteomics and informatics. Dordrecht: Springer; 2008. p. 803.
Chung ST, Hsia DS, Chacko SK, Rodriguez LM, Haymond MW. Increased gluconeogenesis in youth with newly diagnosed type 2 diabetes. Diabetologia. 2015;58:596–603.
Chung ST, Courville AB, Onuzuruike AU, Galvan-De La Cruz M, Mabundo LS, DuBose CW, et al. Gluconeogenesis and risk for fasting hyperglycemia in Black and White women. JCI insight. 2018;3:e121495.
Balakrishna Y, Manda S, Mwambi H, van Graan A. Identifying nutrient patterns in south african foods to support national nutrition guidelines and policies. Nutrients. 2021;13:3194.
Carmichael CY, Wainford RD. Hypothalamic signaling mechanisms in hypertension. Curr Hypertens Rep. 2015;17:39.
Ngo D-H, Vo TS. An updated review on pharmaceutical properties of gamma-aminobutyric acid. Molecules. 2019;24:2678.
Stamler J, Brown IJ, Daviglus ML, Chan Q, Kesteloot H, Ueshima H, et al. Glutamic acid, the main dietary amino acid, and blood pressure: the INTERMAP Study (International Collaborative Study of Macronutrients, Micronutrients and Blood Pressure). Circulation. 2009;120:221–8.
Jennings A, MacGregor A, Welch A, Chowienczyk P, Spector T, Cassidy A. Amino acid intakes are inversely associated with arterial stiffness and central blood pressure in women. J Nutr. 2015;145:2130–8.
McGee MA, Abdel-Rahman AA. N-Methyl-D-Aspartate receptor signaling and function in cardiovascular tissues. J Cardiovasc Pharm. 2016;68:97–105.
Shabeeh H, Khan S, Jiang B, Brett S, Melikian N, Casadei B, et al. Blood pressure in healthy humans is regulated by neuronal NO synthase. Hypertension. 2017;69:970–6.
Dietrich S, Floegel A, Weikert C, Prehn C, Adamski J, Pischon T, et al. Identification of serum metabolites associated with incident hypertension in the European Prospective Investigation Into Cancer and Nutrition-Potsdam Study. Hypertension. 2016;68:471–7.
Louca P, Nogal A, Moskal A, Goulding NJ, Shipley MJ, Alkis T, et al. Cross-sectional blood metabolite markers of hypertension: a multicohort analysis of 44,306 individuals from the COnsortium of METabolomics Studies. Metabolites. 2022;12:601.
Maralani MN, Movahedian A, Javanmard Sh H. Antioxidant and cytoprotective effects of L-Serine on human endothelial cells. Res Pharm Sci. 2012;7:209–15.
Teymoori F, Asghari G, Farhadnejad H, Nazarzadeh M, Atifeh M, Mirmiran P, et al. Various proline food sources and blood pressure: substitution analysis. Int J Food Sci Nutr. 2019;71:1–9.
Karna E, Szoka L, Huynh TYL, Palka JA. Proline-dependent regulation of collagen metabolism. Cell Mol Life Sci. 2020;77:1911–8.
Charlton KE, Schutte AE, Wepener L, Corso B, Kowal P, Ware LJ. Correcting for intra-individual variability in sodium excretion in spot urine samples does not improve the ability to predict 24 h urinary sodium excretion. Nutrients. 2020;12:2026.
Acknowledgements
The authors are grateful to all individuals who voluntarily participated in the African-PREDICT study. The dedication of the support and research staff as well as students at the Hypertension Research and Training Clinic at the North-West University are also duly acknowledged.
Funding
The research funded in this manuscript is part of an ongoing larger research project financially supported by the South African Medical Research Council (SAMRC) with funds from National Treasury under its Economic Competitiveness and Support Package; the South African Research Chairs Initiative (SARChI) of the Department of Science and Technology and National Research Foundation (NRF) of South Africa (GUN 86895); SAMRC with funds received from the South African National Department of Health, GlaxoSmithKline R&D (Africa Non-Communicable Disease Open Lab grant), the UK Medical Research Council and with funds from the UK Government’s Newton Fund; and corporate social investment grants from Pfizer (South Africa), Boehringer-Ingelheim (South Africa), Novartis (South Africa), the Medi Clinic Hospital Group (South Africa) and in-kind contributions of Roche Diagnostics (South Africa). This work is based on the research supported in part by the NRF of South Africa (Grant Number: UID: 138499). Any opinion, findings, and conclusions or recommendations expressed in this material are those of the authors, and therefore, the NRF does not accept any liability in this regard.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
TvZ, MP, RK, LGM, GM, HM, AJ, RL and CM reported no COI. Honoraria (lecture fees): AES (Abbott, Servier); Research Funding: AES (Medical Research Future Fund, Australia). Scholarship or donation: MSK (Postdoctoral grant from the National Research Foundation, South Africa).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Strauss-Kruger, M., van Zyl, T., Pieters, M. et al. Urinary metabolomics, dietary salt intake and blood pressure: the African-PREDICT study. Hypertens Res 46, 175–186 (2023). https://doi.org/10.1038/s41440-022-01071-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-01071-3
- Springer Nature Singapore Pte Ltd.
Keywords
This article is cited by
-
Amino acid profiles associated with plant-rich protein diets may contribute to lower blood pressure
Hypertension Research (2024)
-
Hypertension in sub-Saharan Africa: the current profile, recent advances, gaps, and priorities
Journal of Human Hypertension (2024)






 ) and (B) White adults (
) and (B) White adults ( ) from the African-PREDICT study
) from the African-PREDICT study
