Abstract
Epidemiological information regarding the relationship between hypertension, dyslipidemia, and/or diabetes and hearing impairment (HI) has been controversial. The present cross-sectional study investigated this issue in Japan. The subjects were 371 men and 639 women aged 36‒84 years. Hypertension was defined as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or current use of antihypertensive medication. Dyslipidemia was defined as a serum low-density lipoprotein cholesterol concentration ≥140 mg/dL, high-density lipoprotein cholesterol concentration <40 mg/dL, triglyceride concentration ≥150 mg/dL, or current use of cholesterol-lowering medication. Diabetes was defined as a fasting plasma glucose level ≥126 mg/dL, hemoglobin A1c level ≥6.5%, or current use of diabetic medication. HI was defined as present when subjects did not respond to a pure-tone average of >25 dB HL in the better hearing ear. Adjustments were made for age, smoking, alcohol consumption, body mass index, household income, and education. The prevalence of HI was 31.5% in men and 20.8% in women. In men, hypertension, but not dyslipidemia or diabetes, was independently positively associated with HI: the adjusted prevalence ratio (PR) was 1.52 (95% CI: 1.07‒2.16). Having at least two cardiovascular risk factors among hypertension, dyslipidemia, and diabetes was independently positively related to HI: the adjusted PR was 1.82 (95% CI: 1.11‒2.99, P for trend = 0.02). Such positive associations were not found in women. Hypertension and having at least two cardiovascular risk factors may be positively associated with HI in men only.
Highlights
-
Question: Is there a relationship between hypertension, dyslipidemia, and/or diabetes and hearing impairment (HI)?
-
Findings: In the present cross-sectional study of 371 men and 639 women, hypertension was independently associated with an increased prevalence of HI in men only, and having at least two cardiovascular risk factors among hypertension, dyslipidemia, and diabetes mellitus was independently positively related to the prevalence of HI in men only.
-
Meanings: Hypertension and having at least two cardiovascular risk factors may be positively associated with HI in men only.
Similar content being viewed by others
Introduction
Approximately one-third of people aged 65 years and older are affected by significant hearing impairment (HI) [1]. Age-related HI is associated with various health issues, including accelerated cognitive decline, depression, poor balance, and falls, as well as social implications such as reduced communication and social isolation [2]. Prevention of age-related HI is an important element of public health, and accordingly, it is essential to identify risk and preventive factors for age-related HI.
Epidemiological evidence regarding the relationship between hypertension and/or dyslipidemia and HI has been limited; however, the results obtained from seven studies conducted in the US, Japan, or Korea were not consistent [3,4,5,6,7,8,9]. A meta-analysis in 2014 that included six studies showed a significant positive association between type 2 diabetes mellitus and HI [10]. Five recent prospective cohort studies performed in the US, Japan, and Korea examined this issue and yielded inconsistent results [6, 11,12,13,14]. The definitions of HI used in the abovementioned previous studies were also inconsistent [3,4,5,6,7,8,9,10,11,12,13,14].
The present cross-sectional study investigated the associations of hypertension, dyslipidemia, and diabetes with the prevalence of HI based on the WHO definition in a Japanese population using baseline data from the Aidai Cohort Study (AICOS) conducted in Yawatahama and Uchiko.
Material and methods
Study population
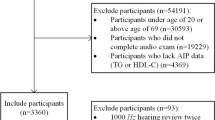
The baseline survey of the AICOS was conducted in 2015 in Yawatahama city, with a total population of nearly 36,000, and in 2016 in the town of Uchiko, with a total population of nearly 17,000, and it is still ongoing in other municipalities in Ehime Prefecture on Shikoku Island, which is located south of Japan’s main island. The current study used data obtained in Yawatahama and Uchiko. In Yawatahama in 2015 and Uchiko in 2016, 798 and 347 individuals participated in the baseline survey, respectively; i.e., 1145 participants aged 36‒84 years (419 men aged 36‒84 years and 726 women aged 37‒79 years) in 2015 and 2016 gave their written informed consent and completed a baseline questionnaire. A total of 118 participants with missing or incomplete data on the variables under study or the audiometric hearing assessment were excluded. In addition, 17 participants with an asymmetrical hearing threshold defined as a between-ear difference of pure-tone average (PTA) >20 dB hearing level (HL) were excluded to rule out subjects with otologic disease to the greatest extent possible. Ultimately, data on 371 men and 639 women were used for analysis. The ethics committee of the Ehime University Graduate School of Medicine approved the AICOS.
Measurements
A self-administered questionnaire elicited information on smoking habits; drinking habits; current use of antihypertensive, cholesterol-lowering, and diabetic medications; household income; and education. Blood pressure was measured twice with a cuff in the sitting position after a rest period of greater than 5 min; the value recorded in the second measurement was adopted for the present study. Hypertension was defined as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or current use of antihypertensive medication. Blood samples were collected from an antecubital vein after an overnight fast. Serum concentrations of low-density cholesterol, high-density lipoprotein (HDL) cholesterol and triglyceride, plasma glucose concentrations, and hemoglobin A1c levels were determined at an external laboratory (Shikoku Chuken, Matsuyama, Japan). Dyslipidemia was defined as a serum low-density lipoprotein cholesterol concentration ≥140 mg/dL, HDL cholesterol concentration <40 mg/dL, triglyceride concentration ≥150 mg/dL, or current use of cholesterol-lowering medication. Diabetes mellitus was defined as a fasting plasma glucose level ≥126 mg/dL, hemoglobin A1c level ≥6.5%, or current use of diabetic medication. Height and weight were measured with the subject in light clothes without shoes. Body mass index (BMI) was calculated by dividing body weight (kg) by the square of height (m).
Hearing assessment
The audiometric hearing assessment was made using air conduction threshold testing with a pure-tone audiometer (AA-75; Rion, Tokyo, Japan) calibrated according to Japanese Industrial Standards T 1201. Air conduction thresholds were obtained at octave frequencies from 0.125 to 8 kHz using a manual testing protocol. Testing was performed by a trained staff member using headphones. We used the audiometric definition of HI adopted by the World Health Organization, which identifies the speech-frequency PTA hearing thresholds at 0.5, 1, 2, and 4 kHz tones. HI was defined as present when the PTA was >25 dB HL in the better hearing ear.
Statistical analysis
Age, smoking status, alcohol consumption, BMI, household income, and educational level were selected a priori as potential confounding factors. Smoking was classified into three categories (never, former, and current), alcohol consumption into three categories (never, former, and current), household income into three categories (<3, 3‒5, and ≥5 million yen per year), educational level into three categories (low [junior high school], medium [high school], and high [junior college, vocational technical school, or university]), and the total number of three risk factors (hypertension, dyslipidemia, and diabetes mellitus) into three categories (0, 1, and ≥2). Age and BMI were adjusted for as continuous variables. Estimations of crude and adjusted prevalence ratios (PRs) and their 95% confidence intervals (CIs) of HI in relation to hypertension, dyslipidemia, and diabetes mellitus were made by means of Poisson regression with robust variance [15]. All computations were performed using the SAS software package version 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
The prevalence of HI was 31.5% in 371 men and 20.8% in 639 women. Compared with women, men were more likely to be former smokers and current drinkers and have a high BMI and high prevalence values of hypertension and diabetes mellitus (Table 1). There were no differences between sexes with regard to age, household income, educational level, or the prevalence of dyslipidemia.
Table 2 gives crude and adjusted PRs and 95% CIs for HI in relation to hypertension, dyslipidemia, and diabetes mellitus. Among 1010 men and women, hypertension, dyslipidemia, and diabetes mellitus were significantly positively related to the prevalence of HI. After adjustment for age, sex, smoking status, alcohol consumption, BMI, household income, and educational level, the positive relationships between hypertension, dyslipidemia, and diabetes mellitus and the prevalence of HI did not reach a significant level. In men, after adjustment for age, smoking status, alcohol consumption, BMI, household income, and educational level, hypertension was independently positively associated with the prevalence of HI: the adjusted PR was 1.52 (95% CI: 1.07‒2.16). No evident relationships were observed between dyslipidemia or diabetes mellitus and the prevalence of HI. In women, hypertension, dyslipidemia, and diabetes mellitus were significantly associated with a higher prevalence of HI in crude analysis; however, these associations completely disappeared after adjusting for confounding factors. There was no multiplicative interaction between hypertension and sex with respect to the prevalence of HI (P for interaction = 0.22).
In 1010 men and women, the positive association between having at least two cardiovascular risk factors and the prevalence of HI fell just short of the significance level in the multivariate model compared with having none of the three cardiovascular risk factors under study; however, the positive exposure–response relationship was statistically significant (P for trend = 0.045): the adjusted PR for having at least two cardiovascular risk factors was 1.35 (95% CI: 0.99‒1.85) (Table 3). In men, those with at least two cardiovascular risk factors had a significantly increased prevalence of HI in the multivariate model, showing a clear positive exposure–response relationship (P for trend = 0.02): the adjusted PR for having at least two cardiovascular risk factors was 1.82 (95% CI: 1.11‒2.99). In women, neither a significant positive linear trend nor a significant positive association with having at least two cardiovascular risk factors was found in the multivariate model. No multiplicative interaction was observed between having at least two cardiovascular risk factors and sex regarding HI (P for interaction = 0.18).
Discussion
In the present study, hypertension was independently associated with a higher prevalence of HI in men only, while we failed to find significant positive relationships between dyslipidemia or diabetes mellitus and HI regardless of sex. To our knowledge, this study is the first to report that having at least two cardiovascular risk factors among hypertension, dyslipidemia, and diabetes mellitus was independently positively related to the prevalence of HI in men only and that significant positive exposure–response relationships between the total number of cardiovascular risk factors and HI were found not only in 1010 men and women but also in 371 men.
The Nurses’ Health Study I found that a history of hypertension was independently associated with a modestly increased risk of self-reported hearing loss [5]. Hypertension was cross-sectionally associated with moderate HI, which was based on the inability to respond to 30 dB at 1 kHz and/or 40 dB at 4 kHz in 13,475 Japanese workers [3]. A US cross-sectional study using data from the National Health and Nutrition Examination Survey 1999–2004 showed an increased prevalence of HI, defined as a PTA of 25 dB or higher at 0.5, 1, 2, and 4 kHz, in either ear among people with hypertension [7]. These findings are in partial agreement with our results. Our results are also in partial agreement with previous findings showing a positive relationship between systolic or diastolic blood pressure and HI [9, 16, 17]. The Health Professionals Follow-up Study found no association between a history of hypertension and the risk of self-reported professionally diagnosed HI [6]. No relationship was observed between hypertension and HI, defined as a PTA of the thresholds at 0.5, 1, 2, and 4 kHz of >25 dB HL in the worse ear, in a cross-sectional study of 7434 Korean individuals aged 40 years and older [4] or in a cross-sectional study of 699 middle-aged Japanese men [8]. In a cross-sectional study of 2052 older US adults, hypertension was not related to HI (PTA of 0.5, 1, and 2 kHz of >25 dB HL) or high-frequency HI (PTA of 2, 4, and 8 kHz of >40 dB HL) in the worse ear [9]. These findings are in contrast to our results. In terms of our results regarding dyslipidemia, partial agreement was found with the results of the previously cited Japanese cross-sectional study showing no relationship between hypercholesterolemia and HI based on a PTA of the thresholds at 0.5, 1, 2, and 4 kHz of >25 dB HL in the worse ear [8]. The aforementioned Health Professionals Follow-up Study showed that hypercholesterolemia was associated with a significantly increased risk of self-reported professionally diagnosed HI, while no relationship was found between diabetes mellitus and the outcome [6]. These findings are inconsistent with our results regarding dyslipidemia but are in partial agreement with our results regarding diabetes mellitus. A cohort study of 202,975 Japanese showed that HbA1c ≥ 8.0% was not associated with low-frequency HI at a hearing threshold >30 dB at 1 kHz or high-frequency HI at a hearing threshold >40 dB at 4 kHz in the better ear compared with HbA1c 5.0‒5.4% [12]. Diabetes was not related to the risk of HI, defined as a failure to hear a 30 dB HL signal at 1 kHz and a 40 dB HL signal at 4 kHz in the better ear, while HbA1c levels were significantly positively associated with the risk of HI in a cohort study of 338 older Japanese individuals [14]. These findings are partially consistent with our results. The present results are in contrast to those of the abovementioned meta-analysis consisting of six studies conducted in Saudi Arabia, Iran, Turkey, Australia, Japan, and the US, which demonstrated that diabetes was significantly associated with a 1.91-fold increased risk of HI based on a PTA greater than or equal to 25 dB at selected frequencies in the worse ear [10]. The Nurses’ Health Studies I and II found that type 2 diabetes was associated with a modestly increased risk of self-reported moderate or worse HI [11]. In a cohort study of 253,301 Korean subjects, diabetes, but not prediabetes, was significantly positively associated with the risk of HI, defined as a PTA of thresholds at 0.5, 1.0, and 2.0 kHz of >25 dB in both the right and left ears [13].
The underlying mechanisms for the observed positive association between hypertension and HI are not clear. Hypertension might affect the cochlea via hypertensive microangiopathy of the vascular stria feeding the organ of Corti, resulting in a decrease in the cochlear oxygen partial pressure [18]. Cumulative oxidative stress can be enhanced by hypoxic situations resulting from the impaired homeostasis of cochlear blood supply and could induce damage to macromolecules such as mitochondrial DNA in the cochlea; the resulting accumulation of mitochondrial DNA mutations/deletions and decline in mitochondrial function over time could progressively induce apoptosis of the cochlear cells [19]. In addition, the increase in natriuretic hormone induced by hypertension may accelerate the development of hearing loss by inhibiting the potassium pump in the cochlear stria vascularis [18]. Hypertension may be related to high-frequency hearing loss, while dyslipidemia and diabetes may affect middle and low tones [18]. Having at least two cardiovascular risk factors among hypertension, dyslipidemia, and diabetes mellitus may enhance inner ear disturbance and increase the risk of HI.
The methodological strengths of the present study include the homogeneity of the test subjects in terms of their residential area and use of the World Health Organization definition of HI. Several weaknesses of the present study should be clarified. The cross-sectional nature of the present study does not permit the assessment of causality due to the uncertain temporality of the association.
Selection bias also has to be taken into account. The participation rate could not be calculated because the exact number of eligible subjects is not available; however, the participation rate must have been low. Our subjects were also probably not representative of the Japanese general population. In fact, the educational levels of our subjects were higher than those of the general population. According to a population census conducted in 2010 in Ehime Prefecture [20], the proportions of men aged 60‒69 years with low, medium, and high educational levels and an unknown educational level were 28.2%, 48.6%, 19.0%, and 4.2%, respectively. The corresponding figures among men aged 60‒69 years in the present study were 10.8%, 54.5%, 34.7%, and 0.0%, respectively. The proportions of women aged 60‒69 years in 2010 in Ehime Prefecture with low, medium, and high educational levels and an unknown educational level were 26.7%, 56.4%, 12.9%, and 4.0%, respectively. The corresponding figures among women aged 60‒69 years in the present study were 10.0%, 58.2%, 31.8%, and 0.0%, respectively. The present population therefore might have had a greater awareness of health issues than did the general population. According to data from the Hisayama Study, a population-based cohort study in the town of Hisayama adjoining a metropolis on Kyushu Island, the prevalence of hypertension (systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or current use of antihypertensive medication), dyslipidemia (serum total cholesterol level ≥220 mg/dL, HDL cholesterol level <40 mg/dL, triglyceride level ≥150 mg/dL, or current use of antihyperlipidemic medication), and diabetes (fasting plasma glucose level ≥126 mg/dL, 2-h postloading glucose level ≥200 mg/dL, or medical history of diabetes) was 49.4%, 46.4%, and 16.6%, respectively, in 524 males aged 40 years or older and 37.6%, 54.1%, and 6.6%, respectively, in 877 females aged 40 years or older [21]. The prevalence of hypertension, dyslipidemia, and diabetes in the current study was 56.6%, 51.8%, and 8.9%, respectively, in men and 37.4%, 57.4%, and 5.5%, respectively, in women. The prevalence values of the present study were unlikely to be distorted. In the present study, data on the observation of the tympanic membrane or ear canal, conductive hearing loss such as bilateral otitis media, and noise-related hearing loss were not available. The possibility of nondifferential outcome misclassification would introduce a bias toward the null. In the current study, although significant associations were detected, the borderline significant associations with hypertension and having at least two cardiovascular risk factors in our total population and the insignificant relationship between diabetes and HI among women might be ascribed to insufficient statistical power. Several confounding factors were adjusted for, yet we could not rule out residual confounding effects.
Conclusions
The present cross-sectional study in Japan suggests that hypertension may be associated with an increased prevalence of HI and that having at least two risk factors among hypertension, dyslipidemia, and diabetes mellitus may be positively related to the prevalence of HI in men. Hypertension might be a risk factor for age-related HI. Further well-designed research on the relationship between hypertension, dyslipidemia, and diabetes and age-related HI is needed, especially in the form of large-scale prospective cohort studies of Asian populations. In addition, the possibility of improving or preventing age-related HI by treatment of such risk factors should be considered.
References
World Health Organization. Deafness and hearing loss. World Health Organization. 2019. http://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss. Accessed 12 June 2019.
Davis A, McMahon CM, Pichora-Fuller KM, Russ S, Lin F, Olusanya BO, et al. Aging and hearing health: the life-course approach. Gerontologist. 2016;56:S256–S267.
Umesawa M, Sairenchi T, Haruyama Y, Nagao M, Kobashi G. Association between hypertension and hearing impairment in health check-ups among Japanese workers: a cross-sectional study. BMJ Open. 2019;9:e028392.
Park HJ, Yoo MH, Woo SY, Kim SW, Cho YS. Prevalence of hearing loss and associated factors in subjects with normal otoscopy: a national cross-sectional study. Int J Audio. 2017;56:951–7.
Lin BM, Curhan SG, Wang M, Eavey R, Stankovic KM, Curhan GC. Hypertension, diuretic use, and risk of hearing loss. Am J Med. 2016;129:416–22.
Shargorodsky J, Curhan SG, Eavey R, Curhan GC. A prospective study of cardiovascular risk factors and incident hearing loss in men. Laryngoscope. 2010;120:1887–91.
Agrawal Y, Platz EA, Niparko JK. Prevalence of hearing loss and differences by demographic characteristics among US adults: data from the National Health and Nutrition Examination Survey, 1999-2004. Arch Intern Med. 2008;168:1522–30.
Sakuta H, Suzuki T, Yasuda H, Ito T. Type 2 diabetes and hearing loss in personnel of the Self-Defense Forces. Diabetes Res Clin Pr. 2007;75:229–34.
Helzner EP, Cauley JA, Pratt SR, Wisniewski SR, Zmuda JM, Talbott EO, et al. Race and sex differences in age-related hearing loss: the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53:2119–27.
Akinpelu OV, Mujica-Mota M, Daniel SJ. Is type 2 diabetes mellitus associated with alterations in hearing? A systematic review and meta-analysis. Laryngoscope. 2014;124:767–76.
Gupta S, Eavey RD, Wang M, Curhan SG, Curhan GC. Type 2 diabetes and the risk of incident hearing loss. Diabetologia. 2019;62:281–5.
Nagahama S, Kashino I, Hu H, Nanri A, Kurotani K, Kuwahara K, et al. Haemoglobin A1c and hearing impairment: longitudinal analysis using a large occupational health check-up data of Japan. BMJ Open. 2018;8:e023220.
Kim MB, Zhang Y, Chang Y, Ryu S, Choi Y, Kwon MJ, et al. Diabetes mellitus and the incidence of hearing loss: a cohort study. Int J Epidemiol. 2017;46:717–26.
Michikawa T, Mizutari K, Saito H, Takebayashi T, Nishiwaki Y. Glycosylated hemoglobin level is associated with hearing impairment in older Japanese: the Kurabuchi Study. J Am Geriatr Soc. 2014;62:1231–7.
Spiegelman D. Easy SAS Calculations for Risk or Prevalence Ratios and Differences. Am J Epidemiol. 2005;162:199–200.
Brant LJ, Gordon-Salant S, Pearson JD, Klein LL, Morrell CH, Metter EJ, et al. Risk factors related to age-associated hearing loss in the speech frequencies. J Am Acad Audio. 1996;7:152–60.
Rigters SC, Metselaar M, Wieringa MH, Baatenburg de Jong RJ, Hofman A, Goedegebure A. Contributing determinants to hearing loss in elderly men and women: results from the population-based rotterdam study. Audio Neurootol. 2016;21:10–15.
Przewoźny T, Gójska-Grymajło A, Kwarciany M, Gąsecki D, Narkiewicz K. Hypertension and cochlear hearing loss. Blood Press. 2015;24:199–205.
Yamasoba T, Lin FR, Someya S, Kashio A, Sakamoto T, Kondo K. Current concepts in age-related hearing loss: epidemiology and mechanistic pathways. Hear Res. 2013;303:30–38.
Statistics Bureau, Ministry of Internal Affairs and Communications, Japan. 2010 Population Census of Japan, Vol. 3-2-10, Results of basic complete tabulation on industries. Prefectures and municipalities. Shikoku. Tokyo, Japan: Statistics Bureau, Ministry of Internal Affairs and Communications, Japan; 2012.
Yasuda M, Kiyohara Y, Hata Y, Arakawa S, Yonemoto K, Doi Y, et al. Nine-year incidence and risk factors for age-related macular degeneration in a defined Japanese population the Hisayama study. Ophthalmology. 2009;116:2135–40.
Acknowledgements
The authors would like to thank the Yawatahama City Government, the Uchiko Town Government, and the Ehime Prefecture Medical Association for their valuable support. The AICOS is funded by the Research Unit of Ehime University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hara, K., Okada, M., Takagi, D. et al. Association between hypertension, dyslipidemia, and diabetes and prevalence of hearing impairment in Japan. Hypertens Res 43, 963–968 (2020). https://doi.org/10.1038/s41440-020-0444-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-020-0444-y
- Springer Nature Singapore Pte Ltd.
Keywords
This article is cited by
-
Prevalence and risk factors of self-reported hearing loss, tinnitus, and dizziness in a population-based sample from rural northeastern Germany
Scientific Reports (2024)
-
Study on the correlation of C-reactive protein/albumin ratio with sudden sensorineural hearing loss complicated by hypertension: a prospective study
European Archives of Oto-Rhino-Laryngology (2024)
-
Functional AGXT2 SNP rs180749 variant and depressive symptoms: Baseline data from the Aidai Cohort Study in Japan
Journal of Neural Transmission (2024)
-
Prevalence and risk factors of hearing loss among the middle-aged and older population in China: a systematic review and meta-analysis
European Archives of Oto-Rhino-Laryngology (2023)
-
Hypertension and the development of hearing loss
Hypertension Research (2022)