Abstract
Functional interleukin-7 receptor α-chain (IL-7Rα) genetic variants, which affect alternative splicing and expression of the soluble IL-7Rα, are associated with susceptibility to autoimmunity. We previously described aberrant IL-7Rα expression and impaired IL-7-mediated T-cell functions in tuberculosis patients. In the present study, we investigated a possible role of IL7RA gene variants. Six exonic IL7RA polymorphisms were genotyped and two minor alleles were found at lower frequencies in tuberculosis patients as compared to healthy contacts from Ghana (rs11567764, p = 0.002; rs1494558, p = 0.01). The rs11567764 polymorphism tags an IL7RA haplotype exclusively found in African populations and was predicted to affect splicing of exon 5. Reduced mRNA expression of the Δexon_5-6 variant was found in T-cells from carriers of the protective rs11567764 allele. Although we were not able to demonstrate the causative effect of rs11567764, our findings suggested functional implications of genetic variants on IL-7Rα splicing and with potential impact on T-cell protection against tuberculosis.
Similar content being viewed by others
Introduction
Tuberculosis is a life-threatening mycobacterial disease of global relevance. The vast majority of Mycobacterium tuberculosis-infected individuals, however, does not develop tuberculosis but rather controls infection by immune surveillance [1]. An important role of genetic factors for immune protection against tuberculosis has been demonstrated in animal models [2] and in humans [3]. Previous studies indicated the capacity of IL-7 to improve protection against M. tuberculosis [4] and found impaired IL-7-promoted T-cell response during acute tuberculosis [4, 5]. IL-7 promotes several functions of T-cell immunity including proliferation, cell survival, and cytokine expression [6].
The T-cell response to IL-7 is critically regulated on the IL-7Rα (CD127, gene: IL7RA) level, and membrane-associated (m)IL-7Rα as well as a soluble (s)IL-7Rα expression are of central relevance for IL-7-response and availability [7]. The sIL-7Rα variant is generated by alternative splicing and has been described to exert IL-7 reservoir functions for T cells [8]. A single nucleotide polymorphism (SNP) (C>T) [9, 10] located in IL7RA exon 6 affects alternative splicing, thereby altering the sIL-7Rα plasma concentration [9, 11]. Alternative splicing events also generate IL7RA variants lacking exon 5-6, but the biological relevance hereof remains elusive [12]. Exonic IL7RA SNPs were previously found to be associated with susceptibility to develop autoimmune diseases, like multiple sclerosis [9].
Own previous studies revealed reduced mIL-7Rα and sIL-7Rα expression during tuberculosis. Minor differences in the frequency of the rs6897932T IL7RA allele between the study groups contributed to decreased sIL-7Rα plasma concentrations in tuberculosis patients [5]. Here, we investigated a possible role of exonic IL7RA SNPs in tuberculosis and evaluated functional effects of the rs11567764 polymorphism.
Methods
Study participants
Patients with clinically confirmed tuberculosis (n = 114) and exposed, healthy contacts (n = 170) were recruited from 2011 to 2016 in Kumasi/Ghana. Diagnosis of tuberculosis was based on patient’s history, symptoms (i.e., persistent cough and fever, weight loss) and chest X-ray. For adults, tuberculosis was additionally confirmed by sputum smear test and, in case of a negative sputum test, by M. tuberculosis sputum culture. Healthy contacts were recruited from households of patients with confirmed tuberculosis. Venous blood was collected into heparinised Vacutainer Tubes (BD Biosciences). Anti-tuberculous medication according to the Ghanaian guidelines was initiated immediately after the first blood sample was taken. Analysis of mRNA from enriched CD4+ T cells was performed on a subset of samples. Part of this patient group has been used previously for the analysis of IL-7 and IL-7Rα and results are published elsewhere [5].
The study was approved by the Committee on Human Research, Publication and Ethics (CHRPE) at the School of Medical Sciences (SMS) at the Kwame Nkrumah University of Science and technology (KNUST) in Kumasi, Ghana (Ref.: CHRPE/AP/275/14, CHRPE/AP/221/14, CHPRE/AP/328/15). The aims and procedures of the study were explained to participants aged ≥18 years, and all adult participants gave written informed consent. For children, the aims and procedures of the study were explained to participants (if appropriate) and to their parents or legal guardians. Assent of children and written informed consent was obtained from parents/guardians. In some cases, consent was confirmed by thumbprint, a procedure approved by the review board. All participants were free to drop out at any time of the study.
Genotyping of IL7RA single nucleotide polymorphisms
DNA was isolated from peripheral blood mononuclear cells (Biocoll, Biochrom) or whole blood using QIAamp DNA Mini kit (Qiagen) or GenoType DNA Isolation Kit (Hain Lifescience). The sample size was chosen based on previous studies that identified associations of the rs6897932 SNP with other immune pathologies and immune interventions. Genotyping was perfomed with predesigned TaqMan SNP Genotyping Assays (Applied Biosystems) and analysed on a 7500 Real-Time PCR machine (Applied Biosystems). A call rate ≥97% was found for all SNPs, and none of the SNPs deviated from the Hardy–Weinberg equilibrium.
Real-time PCR of IL-7Rα variants
CD4+ T cells from freshly isolated peripheral blood mononuclear cells (at least 1.5 × 107 cells) were isolated using anti-human CD4 magnetic particles (BD Biosciences) obtaining a cell purity generally >95% as evaluated by flow cytometry. RNA was isolated and cDNA was generated as described previously [13]. RT-PCR was performed with the QuantiTect SYBR Green PCR kit (Qiagen) as described before [5].
IL7RA minigenes: generation and analyses in HEK293T cells
IL7RA minigenes were generated as shown in Fig. 1c by PCR of human DNA from exon 1 including 242 bp of the downstream intron, and exon 7 including 287 bp of the upstream intron. A complementary overhang containing XbaI/XhoI restriction enzyme sites was included downstream and upstream of the introns, respectively. The construct was inserted into the LeGO iB2 vector [14] using BamHI-BglII/NotI restriction enzyme sites. Exon 5 and exon 6 of IL7RA—including part of the upstream and downstream introns—were inserted into the minigene vector using XbaI/XhoI restriction enzyme sites. To generate mutants, PCR was performed with Phusion High-Fidelity PCR Master Mix with GC Buffer (New England BioLabs) and appropriate primers (sequences are given in Supplementary Table 2). The reactions were run for 30 s at 98 °C followed by 18 cycles of 7 s at 98 °C, 30 s at 60 °C, and 8 min at 72 °C, followed by 10 min at 72 °C. Plasmid of bacterial origin was removed by DpnI digestion prior to transformation. Successful mutation was verified by DNA sequencing.
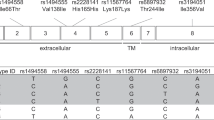
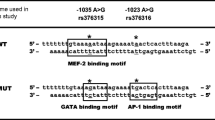
IL7RA single nucleotide polymorphisms (SNPs) and influence of genetic variants on IL7RA splicing. a Position of six selected SNPs in the exons of IL7RA. The full-length IL-7R including the transmembrane domain (TM) as well as two alternative splice variants lacking exon 6 (Δ6, coding for sIL-7Rα) or exon 5-6 (Δ5-6) are shown. Premature stop codons caused by a change in the reading frame are indicated by arrows for the Δ6 and the Δ5-6 variants. b Expression of IL7RA transcripts coding for IL-7Rα lacking exon 6 (Δ6) or exon 5-6 (Δ5-6) in CD4+ cells from tuberculosis patients (squares) and households contacts (circles) carrying rs11567764GG (n = 93) or rs11567764AG/AA (n = 63). Expression level is normalised to full-length IL-7Rα or Δ6. Median and interquartile range for cycle threshold differences (2−ΔCt) are indicated. Exact Mann–Whitney U-tests were used for comparison of groups. rs11567764AG and rs11567764AA were combined as one group due to a low number of rs11567764AA carriers. c, d Effects of IL7RA rs11567764 alleles on alternative splicing were determined using a minigene-based approach. c Schematic depiction of IL7RA minigene generation. Exon 5 or exon 6 of the IL7RA (including ~300 bp of the introns upstream and downstream of the exons) were inserted into a construct generated from IL7RA exon 1 and exon 7 including part of the downstream and upstream introns, respectively. Exon 5 and exon 6 were mutated to obtain rs11567764G/A and rs6897932C/T variants. On the right side, primer positions for PCR are indicated by arrows and expected product lengths are shown. d HEK293T cells were transfected in triplicate with minigene constructs. The proportion of transcript with exon5/exon6 skipped is indicated in the plots with mean ± SEM. One representative experiment of four (rs11567764G/A) and two (rs6897932C/T) is shown. Data analysed by exact Mann–Whitney test stratifying for experiment, and p-values are based on data from all experiments
HEK293T cells were kindly provided by the group of B. Fehse (University Hospital Eppendorf, Hamburg) and are regularly tested for mycoplasma contamination. HEK293T cells were transfected with minigene vectors, and after 24 h incubation, mRNA was isolated from cells using the NucleoSpin RNA kit (Macherey-Nagel) followed by generation of cDNA using Maxima H Minus First Strand cDNA Synthesis kit (Thermo Fisher Scientific). PCR was performed with Phusion High-Fidelity PCR Master Mix with GC Buffer (New England BioLabs) and primers covering exon 1 to exon 7 (forward 5′-ATGACAATTCTAGGTACAACTTTTGG-3′, reverse 5′-AAGATGTTCCAGAGTCTTCTTATG-3′). The reactions were run for 30 s at 98 °C followed by 30 cycles of 7 s at 98 °C, 15 s at 60 °C, and 45 s at 72 °C, followed by 8 min at 72 °C. PCR products were mixed with Hi-Density TBE Sample Buffer and separated on a 10% Novex TBE gel in Novex TBE Running Buffer (Thermo Fisher Scientific) at 200 V. Subsequently, the gel was stained with GelRed (Biotium) and analysed on a ChemiDoc Touch Imaging System (Bio-Rad).
Statistical analysis
Haplotypes of selected SNPs in IL7RA were predicted from 1000 Genomes data set using HaploView version 4.2. Statistical analyses were performed in R version 3.3.0. Due to non-normality of the data (Shapiro–Wilk test of normality), exact Mann–Whitney U test from the package coin was applied for group comparisons. SNP associations were evaluated by logistic regression using the package SNPassoc [15]. Plots were generated in GraphPad Prism version 6.07. Two-tailed p-values <0.05 were considered significant.
Results and discussion
We genotyped six exonic IL7RA SNPs (Fig. 1a) in tuberculosis patients (n = 114) and healthy contacts (n = 170). For two SNPs, i.e., rs1494558C>T and rs11567764G>A, minor alleles were present at higher frequencies among healthy contacts as compared to tuberculosis patients (Table 1). The major effects were seen for recessive models (rs11567764: OR 0.10, 95% CI: 0.01–0.75; rs1494558: OR 0.35, 95% CI: 0.15–0.84). Only 0.9% of tuberculosis patients were homozygous for the minor rs11567764A allele whereas 8.3% of contacts had this genotype (Table 1). These differences are comparable to heterozygous hemoglobin S variant carrier frequencies, a well-known example for a protective allele against malaria [16]. rs11567764 is a synonymous SNP located in exon 5 (Fig. 1a), and its minor allele is almost exclusively found in African populations (Supplementary Table 1). rs1494558 is located in exon 2 of IL7RA and causes a nonsynonymous substitution (i.e., 197C>T, Thr66Ile; Fig. 1a). In combination, the associated minor alleles of both SNPs, i.e., rs11567764A and rs1494558T tag a haplotype frequently present in African populations (Supplementary Table 1). Genome-wide association studies (GWAS) in tuberculosis patients and healthy controls have been performed previously [3, 17]. However, both associated SNPs were not included in these studies of tuberculosis patients. This instance, and the restricted sensitivity of applied statistical methods for detection of recessive allele effects [18], may explain that the IL7RA genomic region on chromosome 5 was not identified as a candidate [3].
IL7RA transcripts lacking exon 6 (Δ6, coding for sIL-7Rα) or exon 5-6 (Δ5-6) are generated by alternative splicing [12, 19]. Since the SNP rs6897932 located in exon 6 has been shown to influence exon 6 splicing [9], we predicted the potential effect of the exon 5 SNP rs11567764 on alternative splicing using HEXplorer [20]. Marked differences in HEXplorer scores indicated a potential negative effect of the rs11567764A allele on exon 5 splicing (Supplementary Figure 1). Consequently, we measured IL-7Rα mRNA of enriched CD4+ T cells from study group donors for Δ5-6, Δ6 (sIL-7Rα), and full-length (mIL-7Rα) IL-7Rα and compared relative amounts of variants between different rs11567764 allele carriers. Donors with the minor rs11567764A allele had a tendency of lower Δ5-6 mRNA levels in comparison to full-length IL-7Rα mRNA (p = 0.07; Fig. 1b, left graph) and significantly lower Δ5-6 levels as compared to Δ6 IL-7Rα mRNA (p = 0.004; Fig. 1b, middle graph). No effect was seen when comparing Δ6 mRNA with full-length IL-7Rα mRNA (p = 0.92; Fig. 1b, right graph). Because of a low number of homozygous rs11567764A carriers, subgroup analysis of tuberculosis patients and healthy contacts for the recessive effect of rs11567764A on Δ5-6 mRNA expression was not possible. To investigate if differential Δ5-6 mRNA expression could be ascribed to the rs11567764 SNP, we generated exon 5 minigenes containing either rs11567764A or rs11567764G (Fig. 1c). The rs6897932 exon 6 variants were also included since these have been proven to affect IL-7Rα exon 6 alternative splicing [9] (Fig. 1c). In accordance, we detected reduced levels of exon 6 skipping for the minigene including the rs6897932T variant (Fig. 1d, left graph). However, no differences of exon 5 splicing were seen between rs11567764G and 11567764A variants (Fig. 1d, right graph). Therefore, we could not assign differential Δ5-6 mRNA expression specifically to the rs11567764 SNP. However, linkage of rs11567764 to another functional SNP or regulatory elements not covered by the minigene could potentially account for this. The function of the Δ5-6 variant remains unclear. It is predicted to be a target for nonsense-mediated decay due to a premature stop codon located upstream of the exon 7/exon 8 junction [21] (Fig. 1a). In addition, the Δ5-6 variant lacks several structural parts of the D2 domain coded by exon 5 [22]. Therefore, we assume that Δ5-6 variant effects are indirect, e.g., by increasing expression of the other IL-7Rα variants. Further studies are needed to elucidate the role of the Δ5-6 variant.
These results indicated protective effects of IL7RA rs1494558T/rs11567764A alleles against the development of tuberculosis. Genetic polymorphisms in IL7RA were shown to affect several immune pathologies including chronic viral [23, 24], autoimmune [9, 10], and inflammatory diseases [25] as well as immune interventions (e.g., graft-versus-host disease after transplantation [26]). Our results may form the basis for further investigations to address the question how different IL7RA polymorphisms and combinations affect T-cell function and immune pathologies.
There is a strong evidence that IL-7 has a decisive role in the generation of protective T-cell memory against chronic infections [27, 28], and the protective capacity of IL-7-mediated effects on T cells against tuberculosis has also been shown [4]. IL-7 can revert T-cell exhaustion [29] and is considered an important candidate for immune-modulatory therapy against chronic infectious diseases [30]. However, we demonstrated previously that acute tuberculosis is accompanied by impaired IL-7 responses of antigen-specific T-cells and aberrant low sIL-7Rα plasma levels [5]. How genetic variants promote protective IL-7Rα functions against the development of tuberculosis needs further clarification. Beyond the field of tuberculosis, this study may generally add to our understanding of crucial processes involving IL-7 in T-cell response of autoimmune and infectious diseases.
References
Zumla A, Raviglione M, Hafner R, von Reyn CF. Tuberculosis. N Engl J Med. 2013;368:745–55.
Apt AS, Logunova NN, Kondratieva TK. Host genetics in susceptibility to and severity of mycobacterial diseases. Tuberculosis. 2017;106:1–8.
Thye T, Vannberg FO, Wong SH, Owusu-Dabo E, Osei I, Gyapong J, et al. Genome-wide association analyses identifies a susceptibility locus for tuberculosis on chromosome 18q11.2. Nat Genet. 2010;42:739–41.
Maeurer MJ, Trinder P, Hommel G, Walter W, Freitag K, Atkins D, et al. Interleukin-7 or interleukin-15 enhances survival of Mycobacterium tuberculosis-infected mice. Infect Immun. 2000;68:2962–70.
Lundtoft C, Afum-Adjei Awuah A, Rimpler J, Harling K, Nausch N, Kohns M, et al. Aberrant plasma IL-7 and soluble IL-7 receptor levels indicate impaired T-cell response to IL-7 in human tuberculosis. PLoS Pathog. 2017;13:e1006425.
Mackall CL, Fry TJ, Gress RE. Harnessing the biology of IL-7 for therapeutic application. Nat Rev Immunol. 2011;11:330–42.
Mazzucchelli R, Durum SK. Interleukin-7 receptor expression: intelligent design. Nat Rev Immunol. 2007;7:144–54.
Lundstrom W, Highfill S, Walsh ST, Beq S, Morse E, Kockum I, et al. Soluble IL7Rα potentiates IL-7 bioactivity and promotes autoimmunity. Proc Natl Acad Sci USA. 2013;110:E1761–70.
Gregory SG, Schmidt S, Seth P, Oksenberg JR, Hart J, Prokop A, et al. Interleukin 7 receptor alpha chain (IL7R) shows allelic and functional association with multiple sclerosis. Nat Genet. 2007;39:1083–91.
Todd JA, Walker NM, Cooper JD, Smyth DJ, Downes K, Plagnol V, et al. Robust associations of four new chromosome regions from genome-wide analyses of type 1 diabetes. Nat Genet. 2007;39:857–64.
Jager J, Schulze C, Rosner S, Martin R. IL7RA haplotype-associated alterations in cellular immune function and gene expression patterns in multiple sclerosis. Genes Immun. 2013;14:453–61.
Rose T, Lambotte O, Pallier C, Delfraissy JF, Colle JH. Identification and biochemical characterization of human plasma soluble IL-7R: lower concentrations in HIV-1-infected patients. J Immunol. 2009;182:7389–97.
Afum-Adjei Awuah A, Ueberberg B, Owusu-Dabo E, Frempong M, Jacobsen M. Dynamics of T-cell IFN-gamma and miR-29a expression during active pulmonary tuberculosis. Int Immunol. 2014;26:579–82.
Weber K, Bartsch U, Stocking C, Fehse B. A multicolor panel of novel lentiviral “gene ontology” (LeGO) vectors for functional gene analysis. Mol Ther. 2008;16:698–706.
González JR, Armengol L, Solé X, Guinó E, Mercader JM, Estivill X, et al. SNPassoc: an R package to perform whole genome association studies. Bioinformatics. 2007;23:654–5.
Modiano D, Luoni G, Sirima BS, Simpore J, Verra F, Konate A, et al. Haemoglobin C protects against clinical Plasmodium falciparum malaria. Nature. 2001;414:305–8.
Curtis J, Luo Y, Zenner HL, Cuchet-Lourenco D, Wu C, Lo K, et al. Susceptibility to tuberculosis is associated with variants in the ASAP1 gene encoding a regulator of dendritic cell migration. Nat Genet. 2015;47:523–7.
Lettre G, Lange C, Hirschhorn JN. Genetic model testing and statistical power in population-based association studies of quantitative traits. Genet Epidemiol. 2007;31:358–62.
Rane L, Vudattu N, Bourcier K, Graniar E, Hillert J, Seyfert V, et al. Alternative splicing of interleukin-7 (IL-7) and interleukin-7 receptor alpha (IL-7Rα) in peripheral blood from patients with multiple sclerosis (MS). J Neuroimmunol. 2010;222:82–6.
Erkelenz S, Theiss S, Otte M, Widera M, Peter JO, Schaal H. Genomic HEXploring allows landscaping of novel potential splicing regulatory elements. Nucleic Acids Res. 2014;42:10681–97.
Maquat LE. Nonsense-mediated mRNA decay: splicing, translation and mRNP dynamics. Nat Rev Mol Cell Biol. 2004;5:89.
McElroy CA, Dohm JA, Walsh ST. Structural and biophysical studies of the human IL-7/IL-7Rα complex. Structure. 2009;17:54–65.
Limou S, Melica G, Coulonges C, Lelievre JD, Do H, McGinn S, et al. Identification of IL7RA risk alleles for rapid progression during HIV-1 infection: a comprehensive study in the GRIV cohort. Curr HIV Res. 2012;10:143–50.
Rajasuriar R, Booth DR, Gouillou M, Spelman T, James I, Solomon A, et al. The role of SNPs in the alpha-chain of the IL-7R gene in CD4+ T-cell recovery in HIV-infected African patients receiving suppressive cART. Genes Immun. 2012;13:83–93.
O’Doherty C, Alloza I, Rooney M, Vandenbroeck K. IL7RA polymorphisms and chronic inflammatory arthropathies. Tissue Antigens. 2009;74:429–31.
Broux B, Shamim Z, Wang T, Spellman S, Haagenson M, Stinissen P, et al. The influence of interleukin-7 receptor alpha-chain haplotypes on outcome after allogeneic hematopoietic cell transplantation. Int J Immunogenet. 2014;41:521–7.
Kaech SM, Tan JT, Wherry EJ, Konieczny BT, Surh CD, Ahmed R. Selective expression of the interleukin 7 receptor identifies effector CD8 T cells that give rise to long-lived memory cells. Nat Immunol. 2003;4:1191–8.
Wherry EJ, Barber DL, Kaech SM, Blattman JN, Ahmed R. Antigen-independent memory CD8 T cells do not develop during chronic viral infection. Proc Natl Acad Sci USA. 2004;101:16004–9.
Pellegrini M, Calzascia T, Toe JG, Preston SP, Lin AE, Elford AR, et al. IL-7 engages multiple mechanisms to overcome chronic viral infection and limit organ pathology. Cell. 2011;144:601–13.
Pellegrini M, Calzascia T, Elford AR, Shahinian A, Lin AE, Dissanayake D, et al. Adjuvant IL-7 antagonizes multiple cellular and molecular inhibitory networks to enhance immunotherapies. Nat Med. 2009;15:528–36.
Acknowledgements
We gratefully thank all donors for participating in this study.
Funding
The study was supported by the German Research Foundation (DFG, JA 1479/5-1) and the German Leprosy and TB relief association (DAHW) project: TB Biomarkers to MJ. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Lundtoft, C., Awuah, A.AA., Güler, A. et al. An IL7RA exon 5 polymorphism is associated with impaired IL-7Rα splicing and protection against tuberculosis in Ghana. Genes Immun 20, 514–519 (2019). https://doi.org/10.1038/s41435-018-0049-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41435-018-0049-5
- Springer Nature Limited