Abstract
Purpose
To compare the safety and efficacy of subconjunctival injection of Mitomycin C(MMC) with sponge-applied MMC during trabeculectomy.
Methods
This prospective, randomised, interventional study was conducted on consecutive patients with uncontrolled glaucoma. 137 patients were randomised into an Injection group (Group 1, n = 66) and a sponge group (Group 2, n = 71). Trabeculectomy was performed in all patients who were followed up on days 1, 15, 30, 3 months, 6 months, 1 year, 2 years & 3 years postoperatively. Baseline & follow-up visits were compared to find out difference in the number of antiglaucoma medications (AGM), Intraocular pressure (IOP), and Best Corrected Visual Acuity (BCVA). In Group 1, the surgeon used MMC 0.2 mg/ml as subconjunctival injection and two separate semicircular surgical sponges soaked with MMC solution of 0.2 mg/mL were inserted subconjunctivally in Group 2.
Results
Mean preop IOP was 34.21 ± 13.3 mmHg & 34.17 ± 10.6 mmHg in group 1 & 2 respectively, which reduced to 11.34 ± 3.7& 12.57 ± 4.7 mmHg(6 months),11.97 ± 4.2 & 13.60 ± 5.3 mmHg(1 year),12.42 ± 4.4 & 11.77 ± 2.8 mmHg (2 years) &11.25 ± 3.2 & 11.81 ± 3.2 mmHg at final visit(P < 0.001 in both groups)with no significant difference between the groups. The mean number of preoperative AGM was 2.32 ± 0.7 & 2.32 ± 0.8 in group1 & 2 respectively which reduced to 0.78 ± 0.9 (P < 0.001) & 1.13 ± 1.1(P = 0.930) at 3 years. Overall success rates were 75.3% in group 1 and 70.7% in group 2 at 3 years(p = 0.512). Postoperative complications and the final post-operative visual outcomes were similar between the groups.
Conclusion
Subconjunctival Injection of MMC is as safe and effective as sponge application with comparable surgical outcomes and complications in the long term.
Similar content being viewed by others
Introduction
Trabeculectomy was described as a method for the reduction of intraocular pressure (IOP) more than 50 years ago by Cairns [1]. Since then the procedure has undergone multiple evolutions and advancements. The introduction of antifibrotics like Mitomycin C (MMC) is one such landmark change that has helped to improve surgical success [2, 3]. The most commonly used method of application of MMC is via soaked sponges over the scleral surface [4]. Literature describes varying concentrations and time of application of sponges with varying success rates [5]. MMC application by sponges has limitations like the possibility of retention [6], granulomas [7], blebitis [8] etc.
Another technique that has gained momentum is the application of subconjunctival injection of MMC, which is reported to have good surgical outcomes [9,10,11,12,13,14,15,16,17]. However, out of these very few studies were randomised [10, 11, 15] and studies with long-term follow-up are sparse [15] (Table 1). Our prospective, randomised study aimed to compare the two modalities of MMC application and study the effects over a long term of three years.
Materials and methods
This was a prospective, interventional, randomised study conducted in a tertiary eye care centre in South India. The study protocol was approved by the institutional review board and adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all participants before recruitment.
Patients with uncontrolled glaucoma (both primary and secondary) either on maximal medical or manifesting a progression of visual field loss were recruited for the study. Monocular patients, patients with a history of prior ocular surgeries, other ocular pathologies like active uveitis, neovascularisation, suspected scleral thinning, patients with systemic comorbidities like connective tissue disorders, immunodeficiency, pregnant or nursing women, and those unwilling to provide an informed consent were excluded. One eye of each eligible patient was included.
Patients included in the study were divided into two treatment groups – Injection group (Group 1) and sponge group (Group 2). They were randomly allocated into either groups on the day of surgery, using a pre-determined random list of 150 numbers generated using the unweighted Bernoulli distribution protocol of the AnalysisToolPak™ add-in of 72 Microsoft Excel© (Microsoft Corporation, Redmond, Washington, USA). Subjects, masked to the randomisation, were assigned to a treatment group, based on the value at their rank (0 = Sponge group, 1 = Injection group). Follow up examinations were performed by glaucoma specialists masked to the patients assignment. A sample size calculation to detect an IOP difference of 2.2 mmHg between the study groups, where the standard deviation was 4.7 and 4.6 in sponge and injection respectively with 80% power and 5% level of significance was utilised. For each group, a sample size of 72 was required.
Surgical procedure
All surgeries were performed by a single experienced glaucoma surgeon (D.M.). In the sponge group, two separate semi-circular surgical sponges prepared by dissecting PVA sponge spears (Madhu Instruments Pvt Ltd, New Delhi, India) soaked in a solution of 0.02% MMC (Mitomycin 2, Zydus Celexa, SPAL Private Ltd, Telangana, India) were used for each case. These two sponges were placed underneath the conjunctival flap for 2 min and were removed. Thereafter, the surgical site was washed with 20 ml of balanced salt solution.
In the injection group,0.1 ml of 0.02%(0.2 mg/ml) of MMC solution was injected into the subconjunctival space with a 30-gauge needle 6–8 mm away from the limbus (Supplemental Fig. 1). After injection, the drug is gently pushed posteriorly with the aid of spatula to avoid limbal migration. The conjunctival dissection was initiated after a contact period of 2 min.
The fornix-based conjunctival peritomy was performed, followed by bipolar wet field cautery. A 4 × 4 mm partial thickness triangular scleral flap was fashioned using a size 15 blade. After creating a 1 mm corneal side port, the anterior chamber was entered. Sclerotomy was performed using a Kelly’s punch and peripheral iridectomy was created. The scleral flap was then repositioned and closed using one releasable and two fixed 10–0 monofilament nylon sutures. Conjunctival closure was achieved using 8–0 polyglactin sutures. The postoperative regimen consisted of 2 hourly Dexamethasone (0.1%) with Chloramphenicol (0.5%) eye drops and topical cycloplegic for four weeks from the first post-operative day. The topical steroids were tapered over 6–8 weeks. The patients were reviewed on days 1, 15, 30 and at 3 months,6 months,1 year,2 year and 3 years after surgery.
During the time of recruitment and in the follow up visits, the Best Corrected Visual Acuity (BCVA) was measured using a Snellen’s chart and converted to logMAR for statistical evaluation. IOP was measured using Goldmann applanation tonometer (AT 900; Haag Streit International, Koeniz, Switzerland). A comprehensive slit lamp examination was performed in each postoperative visit and BCVA, IOP, number of antiglaucoma medications, postoperative complications and interventions like suture release, digital ocular massage and bleb needling were noted.
The primary outcome measure was surgical success. This was defined as
-
A.
Complete success – IOP ≥ 6 and ≤ 21 mmHg or a 20% reduction from baseline without AGM
-
B.
Qualified success -Achieving treatment success with the aid of AGM.
-
C.
Failure was defined as an inability to meet the criteria for success or need for resurgery.
Statistical methods
All statistical analysis were performed using STATA, version 14.2 (StataCorp, USA). Normality of the data were assessed using Shapiro-Wilk test. Descriptive statistics of the data was reported using frequencies (n) and percentages (%) for categorical variables and mean (standard deviation, SD) for continuous variables. Chi-square test was performed to assess the association between groups of categorical variables. Visual acuity values were converted into logarithm of minimal angle of resolution (log MAR) from Snellen’s equivalent value for statistical analysis and were reported in median (interquartile range, IQR). To adjust for possible biases derived from the inclusion of both eyes of the same patient and for difference in the follow-up visits of pre-operative IOP and IOP measured at 1 day, 2 weeks, 1 month 3 months, 6 months, 1 year, 2 years and 3 years post-operatively were compared using a mixed effect regression model. In which each subject’s identification number was regarded as random effect and the time (follow-up periods) was considered as a fixed effect. Post-operative changes in the number of anti-glaucoma medications (AGM) and BCVA were also analysed using the mixed effect model. Comparison of IOP between the sponge and injection group were assessed using independent t test. The between group comparison of AGM and BCVA were evaluated using Wilcoxon rank sum test. Successful IOP control was defined and the cumulative probabilities were assessed using Kaplan–Meier (KM) survival analysis. The success curve between the sponge and injection group were compared using log-rank test. P-value less than 0.05 considered statistically significant.
Results
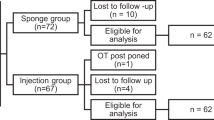
A total of 144 patients who met the inclusion criteria were randomised into two groups; 72 in each group. Six patients in Group 1 (3 patients-lost to follow-up, 2 died and 1 patient-Trauma) and 1 patient in Group 2 (lost to follow-up) were excluded. Overall, 66 patients in Group 1 and 71 patients in Group 2 were eligible for analysis at the end of 3 years. (Supplemental Fig. 2)
Demographic details of the study participants are described in Table 2. Both primary and secondary glaucomas were included in the study. The IOP reduced significantly from 34.21(13.3) to 11.25(3.2) at the end of 3 years in group 1(P < 0.001) and 34.17(10.6) to 11.81(3.2) in group 2(P < 0.001) (Table 3). No significant difference was found between the two groups by the end of three years(P = 0.289)
The use of AGM reduced in both group 1{(2.32(0.7) to 0.78(0.9)}and group 2{(2.32(0.8) to 1.13(1.1)} (Table 3). The postoperative decrease in the AGM was significant in the injection group (P < 0.001) but was not significant in sponge group (P = 0.930) at the final visit.
At the end of 3 years, the complete success in Group 1 was 59.1 % and in group 2 was 47.6% (IOP ≤ 21 mmHg and >6 mmHg/20 % reduction from baseline without AGMs).Overall success (complete + qualified) was 75.3% in Group 1 and 70.7% in group 2(P = 0.512). Figure 1 shows KM survival curve showing the cumulative probability of success between the groups with IOP ≥ 6 and ≤21 mmHg or a 20% reduction from baseline.
The post-operative complications were more in Group 2. But there was no significant difference between the groups. The interventions required also were more in Group 2, with more patients undergoing cataract surgery and bleb needling (Table 4)
At the end of 3 years, there was no significant difference between the baseline and final visual acuity in both groups (P = 0.349 and P = 0.617)
Discussion
Trabeculectomy remains a powerful tool in the surgical armamentarium for lowering IOP even in the era of minimally invasive glaucoma surgery [18]. Numerous technological advancements have been made since the procedure was first described, including the use of antimetabolites, releasable sutures, and newer instruments etc [19].The method of application of MMC is a major contributory factor which determines the long term survival of a bleb [20].MMC application by sponges is considered as a benchmark method. But the technique is not without pitfalls. Some of the major complications of MMC application like bleb leak, hypotony, thin cystic blebs, overhanging blebs can be attributed to the variable and unpredictable MMC concentration by sponge application [21, 22].
Lee et al. [13] described a novel technique of MMC application involving subconjunctival Intra Tenon injection of MMC during trabeculectomy surgery and reported favourable outcomes. Subconjunctival MMC injection has several advantages over the traditional method of sponge application. These include the reduced risk of unwanted exposure of areas of the conjunctiva and limbal epithelium to MMC, less conjunctival damage during manipulation of MMC soaked sponge and eliminating the risk of inadvertently retained sponge material [6].It also allows the administration of a more precise dose of MMC, whereas MMC soaked sponges have been shown to have high intra and inter observer variability in quantification [23, 24]. Sub conjunctival injection of MMC also offers a better coverage area from subconjunctival dissipation and can thus result in better bleb morphology and filtering function [11]. In our study, we used a similar concentration of MMC in both the groups (0.1 ml of 0.2 mg/ml).This was similar to the study by Khouri [14] et al. Comparatively, the concentration of MMC used by Pakravan et al. [10] and Kandarakis et al. [11] was 0.1 ml of 0.1 mg/ml MMC, though Kandarakis et al used a larger injection volume of 0.15 ml.Lim [9] et al used variable concentrations of 0.1 ml and up to a concentration of 0.4 mg/ml.
In our study, there was a statistically significant reduction of IOP from the baseline in both the groups. However, there was no statistically significant difference between the two groups. This was found to be consistent with studies by Khouri et al. [14], Chiew et al. [25] and Kandarakis et al. [11]. In the Lim et al. [9] study, the change in IOP from baseline was significantly lower in the MMC sponge group at post operative month 24. This could be because of the lower preoperative IOP in the injection group which might have made it difficult to exert a change.
The reduction in the number of AGMs from the baseline was statistically significant in the injection group (p < 0.001), but not in the sponge group (p = 0.930) and this was significantly different between the groups (p = 0.041).This is contrast with the previous comparative studies [9,10,11, 14, 15, 17] which did not report any significant difference, though some studies showed less AGM in the injection group [15].
In our study, the complete success rate was 47.6% in the sponge group and 59.1%in the injection group at the end of three years. Kaplan–Meier survival analysis which was used to compare the cumulative probability of success between the two groups revealed an overall success of 70.7% in the sponge group and 75.3% in the injection group at the end of three years. This is consistent with previous trials which also reported comparable success with the two modalities of Mitomycin application [10, 11, 15]
Although complication rates were similar in both the groups, the incidence of choroidal detachments and conjunctival retraction were more in the sponge group. Several previous studies suggest that intraoperative subconjunctival injection of MMC is not associated with increased risk.
This study has its limitations as well. The inclusion of bleb morphology comparison over the long term would have added value to the study. Also, comparisons were not made between primary versus secondary glaucomas and open angle versus angle closure glaucoma.
In conclusion, MMC application by both sponge and injection is safe and effective with comparable success rates. Relatively lower complication rates and lower need of antiglaucoma medications were noted with subconjunctival injections. This is supportive of the trend favouring the use of injection MMC over the conventional sponge application.
Summary
What was known before
-
Subconjunctival injection of Mitomycin is comparable to sponge application in terms of safety and efficacy.
What this study adds
-
The surgical success and efficacy are comparable and maintained over the long term also.
-
The reduction of antiglaucoma medications were more with the subconjunctival injection of MMC.
-
Lesser postoperative complications were noted in patients receiving injections when compared to sponge applied MMC.
Data availability
The data that support the findings of this study are available on request from the corresponding author and approval by the Clinical Audit Committee of the institute. The data are not publicly available due to them containing information that could compromise research participant privacy.
References
Cairns JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol. 1968;66:673–9.
Wilkins, M, Indar, A & Wormald, R Intra-operative mitomycin C for glaucoma surgery. Cochrane Database Syst Rev. CD002897 (2001) https://doi.org/10.1002/14651858.CD002897.
Khaw PT, Chiang M, Shah P, Sii F, Lockwood A, Khalili A. Enhanced trabeculectomy: the moorfields safer surgery system. Dev Ophthalmol. 2017;59:15–35.
Robin AL, Ramakrishnan R, Krishnadas R, Smith SD, Katz JD, Selvaraj S, et al. A long-term dose-response study of mitomycin in glaucoma filtration surgery. Arch Ophthalmol Chic Ill 1960. 1997;115:969–74.
Neelakantan A, Rao BS, Vijaya L, Grandham SB, Krishnan N, Priya VS, et al. Effect of the concentration and duration of application of mitomycin C in trabeculectomy. Ophthalmic Surg. 1994;25:612–5.
Shin DH, Tsai CS, Kupin TH, Olivier MM. Retained cellulose sponge after trabeculectomy with adjunctive subconjunctival mitomycin C. Am J Ophthalmol. 1994;118:111–2.
Choudhary S, Sen S, Gupta O. An unusual case of posttrabeculectomy conjunctival granuloma. Oman J Ophthalmol. 2018;11:52–4.
Khamar M, Bhojwani D, Patel P, Vasavada A. Leftover mitomycin-c sponge causing blebitis. Indian J Ophthalmol. 2019;67:1753–5.
Lim MC, Hom B, Watnik MR, Brandt JD, Altman AR, Paul T, et al. A comparison of trabeculectomy surgery outcomes With Mitomycin-C applied by intra-tenon injection versus sponge. Am J Ophthalmol. 2020;216:243–56.
Pakravan M, Esfandiari H, Yazdani S, Douzandeh A, Amouhashemi N, Yaseri M, et al. Mitomycin C-augmented trabeculectomy: subtenon injection versus soaked sponges: a randomised clinical trial. Br J Ophthalmol. 2017;101:1275–80.
Kandarakis SA, Papakonstantinou E, Petrou P, Diagourtas A, Ifantides C, Georgalas I, Serle J. One-year randomized comparison of safety and efficacy of trabeculectomy with mitomycin C sub-tenon injection versus Mitomycin C-Infused Sponges. Ophthalmol Glaucoma. 2022;5:77–84.
Maheshwari D, Kanduri S, Rengappa R, Kadar MA. Intraoperative injection versus sponge-applied mitomycin C during trabeculectomy: one-year study. Indian J Ophthalmol. 2020;68:615–9.
Lee E, Doyle E, Jenkins C. Trabeculectomy surgery augmented with intra-Tenon injection of mitomycin C. Acta Ophthalmol. 2008;86:866–70.
S Khouri A, Huang G, Y Huang L. Intraoperative injection vs sponge-applied Mitomycin C during trabeculectomy: one-year study. J Curr Glaucoma Pract. 2017;11:101–6.
Esfandiari H, Pakravan M, Yazdani S, Doozandeh A, Yaseri M, Conner IP. Treatment outcomes of Mitomycin C-Augmented trabeculectomy, sub-tenon injection versus soaked sponges, after 3 years of Follow-up. Ophthalmol Glaucoma. 2018;1:66–74.
Swogger J, Conner IP, Rosano M, Kemmerer M, Happ-Smith C, Wells A, et al. Injected versus sponge-applied Mitomycin C (MMC) during modified trabeculectomy in New Zealand White Rabbit Model. Transl Vis Sci Technol. 2020;9:23.
Guimarães ME, de Pádua Soares Bezerra B, de Miranda Cordeiro F, Carvalho CH, Danif DN, Prata TS, et al. Glaucoma surgery with soaked sponges with Mitomycin C vs sub-tenon injection: short-term outcomes. J Curr Glaucoma Pract. 2019;13:50–54.
Kalarn S, Le T, Rhee DJ. The role of trabeculectomy in the era of minimally invasive glaucoma surgery. Curr Opin Ophthalmol. 2022;33:112–8.
Sawchyn AK, Slabaugh MA. Innovations and adaptations in trabeculectomy. Curr Opin Ophthalmol. 2016;27:158–63.
You Y, Gu Y, Fang C, Ma X. Long-term effects of simultaneous subconjunctival and subscleral Mitomycin C application in repeat trabeculectomy. J Glaucoma. 2002;11:110–8.
Holló G. Wound healing and glaucoma surgery: modulating the scarring process with conventional antimetabolites and new molecules. Dev Ophthalmol. 2012;50:79–89.
Georgopoulos M, Vass C, Vatanparast Z. Impact of irrigation in a new model for in vitro diffusion of mitomycin-C after episcleral application. Curr Eye Res. 2002;25:221–5.
Mehel E, Weber M, Stork L, Péchereau A. A novel method for controlling the quantity of mitomycin-C applied during filtering surgery for glaucoma. J Ocul Pharmacol Ther. 1998;14:491–6.
Mietz H, Diestelhorst M, Rump AF, Theisohn M, Klaus W, Krieglstein GK. Ocular concentrations of mitomycin C using different delivery devices. Ophthalmologica. 1998;212:37–42.
Chiew W, Guo X, Ang BH, Lim AH, Yip LL. Comparison of surgical outcomes of sponge application versus subconjunctival injection of Mitomycin-C during combined phacoemulsification and trabeculectomy surgery in Asian eyes. J Curr Ophthalmol. 2021;33:253–9.
Author information
Authors and Affiliations
Contributions
CONCEPTION: Constructing an idea or hypothesis for research and/or manuscript: DM, MRP. DESIGN: Planning methodology to reach the conclusion: DM, MRP. SUPERVISION: Organising and supervising the course of the project or the article and taking the responsibility: DM, MRP, RR, MAK, NP. FUNDINGS: Providing personnel, environmental and financial support and tools and instruments that are vital for the project: NIL. MATERIALS: Biological materials, reagents and referred patients: DM, RR, MAK. DATA COLLECTION AND/OR PROCESSING: Taking responsibility in execution of the experiments, patient follow-up, data management and reporting: DM, MRP, PHM. ANALYSIS AND/OR INTERPRETATION: Taking responsibility in logical interpretation and presentation of the results: DM, MRP. LITERATURE REVIEW: Taking responsibility in this necessary function: DM, MRP, PHM. WRITER: Taking responsibility in the construction of the whole or body of the manuscript: DM, MRP. CRITICAL REVIEW: Reviewing the article before submission not only for spelling and grammar but also for its intellectual content.: DM, MRP, NP. OTHER.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maheshwari, D., Pillai, M.R., HM, P. et al. Long-term outcomes of Mitomycin-C augmented trabeculectomy using subconjunctival injections versus soaked sponges: a randomised controlled trial. Eye 38, 968–972 (2024). https://doi.org/10.1038/s41433-023-02816-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02816-1
- Springer Nature Limited
This article is cited by
-
Efficacy and safety of intraoperative injection of mitomycin C during trabeculectomy: a systematic review and meta-analysis
International Ophthalmology (2024)