Abstract
Background/objectives
To investigate outcomes of referrals for suspected angle closure and explore whether anterior segment optical coherence tomography (AS-OCT) can be used to tighten triaging criteria in a glaucoma virtual clinic.
Subjects/methods
Retrospectively collected data. The first audit (04/2018-03/2019) identified referrals for suspected angle closure without other glaucoma-related findings (primary angle closure suspect (PACS) referrals). All patients underwent gonioscopy. The second audit (04-08/2019) identified patients with suspected angle closure in a virtual clinic. Management outcomes were assessed, using gonioscopy as reference standard. The outcomes of the second audit were re-audited after changing the triaging criterion from angle width <10° to iridotrabecular contact (ITC) in ≥1 quadrants on AS-OCT.
Results
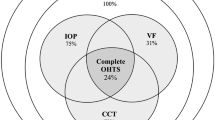
Out of 1754 glaucoma referrals (first audit), 24.6% (431/1754) were PACS referrals. Of these, only 10.7% (42/393) had an occludable angle on gonioscopy, with 97.6% (41/42) being PACS. Of these, 78% (32/41) underwent laser peripheral iridotomy. Out of 137 referrals in the virtual clinic (second audit), 66.4% (91/137) were triaged to the face-to-face clinic. Of these, 31.9% (29/91) were discharged. AS-OCT had positive and negative predictive value of 74.3% (95% confidence intervals (CI) 57.8–86.0) and 82.1% (95% CI 70.0–90.2%), respectively, in detecting ITC in ≥1 quadrants. In the re-audit 45.9% (45/98) of those with suspected angle closure were triaged for gonioscopy, with 24.4% (11/45) of them being discharged.
Conclusion
PACS referrals represent a substantial burden to hospital-based services and their accuracy is low. ITC in ≥1 quadrants on AS-OCT can be useful in triaging those who need further evaluation with gonioscopy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
The guidance for the management of angle closure by the UK National Institute for Health and Care Excellence is to “Refer to an ophthalmologist anyone with suspected intermittent angle closure or chronic angle closure glaucoma (or its precursors — primary angle closure suspect [PACS], or chronic primary angle closure [PAC])” [1]. The same guidance states that treatment options for the management of PACS, PAC and chronic primary angle closure glaucoma (PACG) are similar to the definitive treatment of acute angle closure, in most cases a laser peripheral iridotomy (LPI) [1]. Recently, two landmark trials have redefined interventions for angle closure [2, 3]. The effectiveness of early lens extraction for the treatment of angle closure (EAGLE) has provided evidence that clear-lens extraction has greater efficacy and is more cost-effective than LPI in those with established angle closure disease (intraocular pressure ≥30 mmHg or PACG) [2]. The Zhongshan angle closure prevention (ZAP) trial has shown that prophylactic LPI is of modest benefit in PACS and, therefore, does not support its widespread practice in these individuals [3].
In light of the EAGLE and the ZAP trial data, the clinical pathway for angle closure needs to be revisited [4], including virtual clinics, which have become increasingly popular to address capacity problems of hospital-based glaucoma care [5]. This is important to reduce variation, improve quality of care, and optimise clinical outcomes [6]. It is also necessary for optimal allocation of healthcare resources, which has become an even greater priority since the outbreak of the COVID-19 pandemic [7].
To this purpose, there are key questions to be asked: what is the burden of PACS referrals on glaucoma services? Considering the ZAP data [3], how many of these patients need monitoring in a hospital setting or treatment? What is the most efficient setting for examining newly referred patients? Can anterior segment optical coherence tomography (AS-OCT) [8] be used to identify those who would benefit from gonioscopy? The aim of the present report is to provide some insight into the above questions, by looking into everyday clinical data from a tertiary glaucoma specialist practice.
Materials and methods
All data were retrospectively collected in the context of two clinical audits conducted in the Glaucoma Service at Moorfields Eye Hospital, National Health Service (NHS) Foundation Trust, London, United Kingdom (UK) (Fig. 1). The study methodology for each audit was approved by the Audit Department of Moorfields Eye Hospital (project numbers: 628 and 370) and all methods adhered to the tenets of the Declaration of Helsinki.
The first audit (Moorfields Eye Hospital at Bedford) included all patients referred for suspected angle closure in the absence of other glaucoma-related findings. All patients were examined in the glaucoma face-to-face clinic with gonioscopy. The second audit (Moorfields Eye Hospital at Cayton Street) included newly referred patients who attended the virtual clinic within the above time frame and were suspected to have occludable angles, regardless of the initial reason for their referral. ZAP Zhongshan Angle Closure Prevention (ZAP) trial.
First audit (project 628)
The audit was conducted at Moorfields Eye Hospital at Bedford and covered a one-year period (April 2018 to March 2019). As part of routine clinical care, all newly referred patients during that time had a comprehensive ophthalmic examination, including gonioscopy, at the consultant-led face-to-face glaucoma clinic based on the same clinical protocol (Supplementary Table 1). In the face-to-face clinic patients are examined by various clinicians with different levels of experience, under the supervision of Glaucoma Specialists. All data were collected on Medisoft (Medisoft Limited, Leeds, UK).
The objective was to investigate outcomes of “PACS referrals”, defined as glaucoma referrals for suspected angle closure without elevated IOP or glaucomatous-like optic discs or abnormal visual fields [4]. All glaucoma referrals within the above time frame were scrutinised to identify patients ≥18 years of age who met the above referring criteria. Synonym terms for suspected angle closure were searched for in the referral letters: “narrow angles”, “narrow anterior drainage angle on Van Herick testing” [9], “narrow/shallow Van Herick”, “narrow/shallow anterior chamber”, “risk of acute angle closure”. Patients with a previous diagnosis of glaucoma or angle closure, or a previous visit to a glaucoma clinic were excluded from the audit.
Data were collected from Medisoft (automatically or manually extracted, where appropriate): demographics, data from the referral letter (including the grading of the Van Herick test by the referring optician), data from the face-to-face examination. An angle was defined as “occludable” if graded 0 on Medisoft (Shaffer grading system [10]), if there was mentioning of ≥180 degrees of iridotrabecular contact (ITC) [11] or if the term “occludable angle” had been recorded in the medical record.
The Positive predictive value (PPV) of PACS referrals was calculated using gonioscopy as the reference standard: PPVPACS = number of patients with an occludable angle in at least one eye on gonioscopy / all PACS referrals.
Second audit (project 370)
The audit was conducted at Moorfields Eye Hospital at Cayton Street (technician-led glaucoma virtual clinic) and covered a five-month period (April to August 2019). As part of routine clinical care, all newly referred patients at the time had a comprehensive ophthalmic examination, including AS-OCT (Cirrus HD-OCT, Carl Zeiss Meditec, Dublin, CA, USA) [8], at the glaucoma virtual clinic based on the same technician-led protocol (Supplementary Table 2). AS-OCT was performed in the dark, with the patient in the sitting position. Using the single-scan-mode protocol, images were captured from the temporal and nasal angles quadrants (9 o’clock and 3 o’clock meridians). Scans were not obtained from the superior and inferior quadrants (12 o’clock and 6 o’clock meridians), due to the difficulty in obtaining good quality images. All data were collected on Openeyes (Apperta Foundation CIC, Sunderland, UK) and on Forum (Carl Zeiss Meditec, Dublin, CA, USA). Medical records were reviewed remotely by one of several consultant ophthalmologists from the Glaucoma Service, who decided on discharge or further evaluation in the consultant-led face-to-face glaucoma clinic. An iridocorneal angle <20o on AS-OCT was the triaging criterion for further evaluation with gonioscopy. Based on preliminary data from the audit, several patients attending the face-to-face clinic were being subsequently discharged. To address capacity issues, in June 2019 this criterion was tightened to <10°. These cut-offs are in accordance with the original description for an occludable angle by Becker and Shaffer, who proposed that angle closure is ‘probable’ with anterior chamber width of 20° and ‘possible’ with anterior chamber width of 10° [12].
The objective was to investigate (a) outcomes of newly referred patients in the virtual clinic and were found to have suspected angle closure, regardless of the initial reason for their referral, (b) whether imaging with AS-OCT can be used to tighten the triaging criteria for further evaluation in the face-to-face clinic. A triaging optometrist (N.N) used the Cito electronic health record software to identify patients meeting the above criteria. Consultant ophthalmologists were also asked to identify eligible patients for the audit during the routine review process of the virtual clinic. Data were collected from Openeyes (automatically or manually extracted, where appropriate): demographics, data from the referral letter, data from the virtual clinic, data from the face-to-face Clinic. ITC on AS-OCT was defined as any contact between the peripheral iris and the angle wall anterior to the scleral spur [13].
The PPV and negative predictive value (NPV) of AS-OCT in capturing the presence of ITC in ≥1 quadrants were calculated using gonioscopy as the reference standard:
-
PPVASOCT = number of true positives / (number of true positives + number of false positives).
-
NPVASOCT = number of true negatives / (number of true negatives + number of false negatives).
The cut-off of ITC in ≥1 quadrants was used to minimise variability in the assessment of the anterior chamber (binary question: ITC vs no ITC). It also represents a low threshold for ‘flagging up’ patients with possible angle closure. The definitive diagnosis of angle closure relied on the assessment of the whole iridocorneal angle with gonioscopy.
Approximately one year later the outcomes of the second audit were re-audited (July to November 2020). The triaging criterion from the virtual to the face-to-face clinic was changed from an iridocorneal angle of <10° to ITC in ≥1 quadrants on AS-OCT.
For both audits, proportions are presented with corresponding 95% confidence intervals (CI).
Results
First audit (project 628)
From April 2018 to March 2019, Moorfields Eye Hospital at Bedford received 1754 glaucoma referrals. Of these, 431 (24.6%, 95% CI 22.6%–26.6%) were PACS referrals initiated by community optometrists. According to the referral letters, 0.5% (2/431, 0.01%–1.79%) were for Van Herick grade 0, 82.8% (357/431, 80.0%–86.1%) for Van Herick grade 1, 4.9% (21/431, 3.17%–7.37%) for Van Herick grade 2 and 11.8% (51/431, 9.10%–15.2%) for “narrow anterior chamber angles” without reference to a grading score.
Out of the 431 PACS referrals, 38 patients did not attend their appointment, whereas 393 had a full glaucoma assessment with gonioscopy in the glaucoma face-to-face clinic. Patients’ demographics and clinical characteristics are presented in Table 1. The mean age ± standard deviation (SD) was 61.2+/− 13.5 years; 70.7% were females and 25.2% reported a family history of glaucoma.
The PPV of PACS referrals was 10.7% (42/393, 8.0%–14.2%). Out of those with an occludable angle on gonioscopy, 97.6% (41/42, 86.6%–99.9%) were PACS. The following diagnostic outcomes were recorded: 85% (334/393, 81.1%–88.2%) no glaucoma-related pathology, 10.5% (41/393, 7.76%–13.9%) PACS, 0.3% (1/393, 0.01%–1.58%) PAC and no PACG. Also, 4.1% (16/393, 2.47%–6.56%) were found to have suspicious discs and 0.3% (1/393, 0.01%–1.58%) had ocular hypertension (IOP > 22 mmHg without other glaucoma related findings).
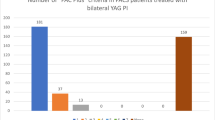
Out of the 393 patients who attended their appointments, 48.6% (191/393, 43.7%–53.5%) were discharged at first visit, 29.3% (115/393, 25.0%–34.0%) were kept under monitoring without treatment and 22.1% (87/393, 18.3–26.5%) had an intervention, either LPI or phacoemulsification. Out of the 41 PACS, 78% (32/41, 63.1%–88.2%) had LPI, 12.2% (5/41, 4.86% - 26.0%) had phacoemulsification and 9.8% (4/41, 3.30% - 23.1%) were kept under monitoring.
Second audit (project 370)
From April to August 2019, 2132 newly referred patients attended the glaucoma virtual clinic. The triaging process identified 137 patients with suspected angle closure. Of these, 75.9% (104/137, 68.1%–82.3%) had been referred by the optician and 24.1% (32/137, 17.7%–31.9%) were internal referrals. Patients’ demographics are presented in Table 1. The mean age ± SD was 57.99 ± 12.0 years; 71.5% were females and 14.6% reported a family history of glaucoma. Following the assessment in the virtual clinic, 33.6% (46/137, 26.2%–41.9%) were discharged and 66.4% (91/137, 58.2%–73.8%) were triaged for further assessment with gonioscopy in the face-to-face clinic.
Out of the 91 patients who had the face-to-face consultation, 31.9% (29/91, 23.2%–42.0%) were discharged, 34.1% (31/91, 25.1%–44.3%) were kept under monitoring and 34.1% (31/91, 25.1%–44.3%) were treated. Overall, 52% (13/25, 33.5%–70%) of PACS had LPI. Out of the 91 patients in the face-to-face clinic, 38.5% (35/91, 29.1%–48.7%) had ITC in ≥1 quadrants on gonioscopy. AS-OCT had a PPV of 74.3% (26/35, 57.8%–86.0%) and a NPV of 82.1% (46/56, 70.0%–90.2%) in detecting ITC in ≥1 quadrants. Out of the 36 patients who had ITC in ≥1 quadrants on AS-OCT, 72.2% (26/36, 55.9%–84.3%) had an intervention. Conversely, out of the 101 patients who did not have ITC on AS-OCT, only 5% (5/101, 1.9%–11.4%) had an intervention (Table 2).
From July to November 2020, 671 newly referred patients attended the glaucoma virtual clinic. The triaging process identified 98 patients with suspected angle closure for the re-audit. Management outcomes are presented in Table 3. With the change in the triaging criterion from <10° to ITC in ≥1 quadrants on AS-OCT, 54.1% (53/98, 44.3%–63.6%) were discharged back to the optician and 45.9% (45/98, 36.4%–55.8%) were triaged for further assessment in the face-to-face clinic. Among those who attended the face-to-face clinic, 24.4% (11/45, 14.1%–38.8%) were subsequently discharged to the care of their optician.
Discussion
We have audited clinical data from two settings of the same tertiary glaucoma referral centre in the UK, to explore the outcomes of newly referred patients with suspected angle closure. The audits presented in this report examine different aspects of the same clinical pathway. Given the paucity of data on the topic, our study adds to the literature. However, the audits have different objectives and, therefore, different methodologies. For this reason, direct comparisons between the outcomes of these audits (e.g. discharge rates at first visit) may not be appropriate.
Based on our data, one quarter of all glaucoma referrals within a year were for suspected angle closure in the absence of other glaucoma-related factors (PACS referrals [4]). There are very limited data on the burden of PACS referrals on hospital-based services. With the ZAP data having shifted the management of PACS away from the widespread use of LPI [3], such knowledge is important for service development and resource allocation. In a study conducted in Scotland, 4.6% (33/715) of all glaucoma referrals within a six-month period were PACS referrals, which is a lot lower than what was found it our study [14]. However, comparisons with the Scottish data may not be appropriate. Unlike the rest of the UK, the Scottish general ophthalmic services (GOS) contract reimburses optometrists to conduct supplementary eye examinations [15]. Therefore, an optometrist is likely to combine information on other risk factors before deciding on a referral [14].
The accuracy of PACS referrals was low, with only 11% of patients referred for ‘narrow angles’ found to have occludable angles on gonioscopy. Previous studies have reported low or moderate accuracy of optometrist-initiated glaucoma referrals in the UK [16,17,18,19,20,21,22,23,24], Sweden [25, 26], and Australia [27]. However, these studies focused on the detection of glaucomatous damage. To our knowledge, there are no previous studies on the accuracy of PACS referrals initiated by community optometrists. PACS referrals are based on the recommendation that patients with LACD of ≤25% (van Herick Grade 1 or 2) [9] should be referred to secondary eyecare services [28, 29]. In a recent Cochrane Review, the pooled sensitivity and specificity estimates for LACD ≤ 25% were 83% and 88%, respectively [30]. However, these estimates are likely to be overestimated due to the high risk of bias in 75% of the studies included in the meta-analysis [31]. In addition, at a population level the PPV of LACD (the probability of a patient having occludable angles, given an LACD of ≤25%) is driven low by the low prevalence of angle closure disease. In a study by Foster et, LACD ≤ 25% had sensitivity of 99% and specificity of 66% in detecting occludable angles [32]. Nonetheless, with the prevalence of angle closure at 6.8%, the PPV of the 25% cut-off was 17%. This is consistent with the 11% PPV of PACS referrals found in our study. The study by Foster et al was conducted in an Asian population and LACD was assessed by two senior Ophthalmologists. In the UK population, known to have lower prevalence of angle closure [33] and with LACD assessed by less experienced observers, the PPV of the test is expected to be lower than 17%, which is exactly what we found. The PPV of the Van Herick test can be improved by increasing the pre-test probability of angle closure disease. Therefore, the new RCOphth guidance advises that patients with suspected angle closure should only be referred on the basis of elevated IOP, glaucoma or certain ocular, systemic and social risk factors constituting “PACS plus” [4]. Our data fully support the new guidance and also suggest that such a strategy would be unlikely to put patients at risk of losing vision. Out of the 393 PACS referrals who were seen in clinic, there were no patients with glaucoma; out of the 42 patients with occludable angles on gonioscopy, only one had PAC and all other patients were PACS.
The timeframes of the two audits presented in this report should be considered in data interpretation (Fig. 1). Until the first half of 2019, all glaucoma referrals at Moorfields at Bedford were being assessed in the face-to-face clinic, whereas the virtual clinic was mainly for monitoring patients who were stable or at low risk of vision loss. With AS-OCT having enabled non-invasive high-resolution imaging of the anterior chamber angle [8, 13, 34], by the end of the same year the virtual clinic was expanded to receive all newly referred patients, including those with suspected angle closure. This model of care had been previously implemented at Cayton Street, which represents the main glaucoma virtual clinic at Moorfields Eye Hospital. This also explains the difference in the methods between the two audits. The majority (78%) of PACS in the first audit and half (52%) of PACS in the second audit underwent prophylactic LPI. The first audit covered a one-year period just before the publication of the ZAP trial [3], whereas the second audit covered a 5-month period just after the publication of this landmark study. However, it takes time to bridge the gap between a randomized controlled trial and clinical practice. Therefore, the management outcomes in these audits reflect former everyday clinical practice, with preventive LPI routinely performed in PACS [35]. Clinicians would now be less likely to perform prophylactic LPI in PACS who do not have additional risk factors. This is now recommended practice as set out in the recently published Royal College of Ophthalmologists (RCOphth) Guidelines on the management of angle closure [4]. Similarly, clinicians would be more likely to discharge PACS to their optometrists for annual review, rather than to keep them under monitoring in the hospital setting. Also, the re-audit of the second study covered the months following the first COVID-19 lockdown, which is likely to have had an impact on the number of referrals due to optometry practice closure.
Although glaucoma virtual clinics are growing in numbers [5, 36], there are no standardised criteria for further assessment in a face-to-face setting. Based on angle width criteria [12] on AS-OCT (an iridocorneal angle of <20°, later tightened to <10°), 66% of patients with suspected angle closure in the virtual clinic required further assessment with gonioscopy. Of these, 1/3 had an intervention, 1/3 were kept under monitoring and 1/3 were discharged. These management outcomes raised the question of whether the triaging process could be more efficient. Determining angle width on AS-OCT requires familiarity with the built-in software and involves the identification of the scleral spur as a reference point, which may not always be easy to discern [37]. For the same reason it often relies on the clinician’s impression, rather than an actual measurement. Conversely, determining whether there is ITC on an AS-OCT image is a binary question and, therefore, expected to be less variable. Interestingly, the recently published RCOphth guidelines define PACS as the presence of ITC, without specifying the number of quadrants [4]. Using gonioscopy as the reference standard, AS-OCT had sensitivity of 74% and specificity of 82% in detecting ITC ≥ 1 quadrants. Clinic-based studies have previously reported high sensitivity (98% [13] and 84% [38]) and moderate specificity (55% [13] and 58% [38]) of AS-OCT in detecting ITC ≥ 1 quadrants, compared with gonioscopy. Community-based studies have also confirmed that AS-OCT identifies more ITC, compared with gonioscopy [39, 40]. The reasons behind the diagnostic disagreement between gonioscopy and AS-OCT have been previously discussed [13, 34]. However, direct comparisons with the literature may not be appropriate. The above studies were conducted in Asians, with all assessments performed by senior clinicians or research-trained observers. Our data reflect every day clinical practice, with AS-OCT images assessed by various clinicians and with gonioscopy performed by various clinicians in the context of busy glaucoma clinics.
Given its high sensitivity in detecting ITC [13, 34, 38,39,40], AS-OCT is a suitable modality for the assessment of the anterior chamber angle in a glaucoma virtual clinic, because patients with occludable angles are unlikely to be missed. This is also supported by our findings: 72% of those with ITC in ≥1 quadrants versus 5% of those without ITC on AS-OCT had an intervention. In addition, ITC ≥ 1 quadrants on AS-OCT as a triaging criterion seems to be more effective in reducing false positives, compared with angle width <10°. In the re-audit, by changing the triaging criterion to ITC in ≥1 quadrants on AS-OCT, the proportion of patients who needed further assessment with gonioscopy was reduced from 66% to 46% and the proportion of patients who were discharged from the face-to-face clinic was reduced from 32% to 24%, compared to the initial phase of the audit. These data do not suggest that AS-OCT should replace gonioscopy for the detection of ITC. Gonioscopy remains the reference standard for confirming the presence of ITC and for diagnosing angle closure [4, 41,42,43]. However, it is a clinical skill that requires considerable training and experience, it involves contact with the patient’s eye and it is subject to variability [13, 34]. Therefore, gonioscopy is not suitable for a technician-led glaucoma virtual clinic.
This report presents real world data, reflecting common clinical practice. Therefore, our findings are likely to be applicable to other settings within similar healthcare systems. Real-world data and real-world evidence have become increasingly important in health care decisions [44, 45]. However, there are also shortcomings related to their use [44], and this is denoted in the limitations of this report. Gonioscopy was performed by various clinicians with different levels of experience. Although it is standard practice to perform gonioscopy in dim light, lighting conditions cannot be fully standardized in everyday glaucoma clinics. To minimise misclassification bias in the detection of occludable angles, medical records were reviewed manually to ensure that all details of the gonioscopic assessment are captured. Also, those who performed gonioscopy were not masked to the optometrist’s referral (first audit) or to the initial assessment in the virtual clinic (second audit). On the other hand, the low accuracy of PACS referrals found in our study does not suggest bias towards a higher detection of occludable angles. In addition, we have no information on the training level of each referring optometrist, which may have impacted the PPV of the Van Herick assessment. However, given that Moorfields at Bedford is the only NHS glaucoma service in the region, we are likely to have captured most, if not all, glaucoma referrals within the given period. Therefore, our data are likely to reflect all levels of experience in optometric practice. Conversely, we may have missed some patients with suspected angle closure in the second audit, because the identification of these referrals was less comprehensive. The lack of standardisation in the triaging process from the virtual to the face-to-face clinic is another limitation. While the clinicians were guided by the AS-OCT criteria, the overall decision to refer the patient for further assessment may have been affected by other factors. This is an inherent limitation of the virtual setting because, to date, there are no previously published criteria to guide this process. In addition, we do not have gonioscopic data for the patients who were discharged directly from the virtual clinic. Also, the two audits are from different clinics with possibly different referral patterns and populations, so do not necessarily reflect a full audit cycle. This may also explain some differences in the demographics and clinical characteristics of these patients.
In conclusion, using real world data from a tertiary glaucoma specialist practice in the UK, we found that PACS referrals represent a substantial burden to hospital eye services and their accuracy is low. We also found that PACS referrals mostly represent individuals at low risk of vision loss, even if occludable angles are confirmed on gonioscopy. Our data also suggest that AS-OCT is a useful modality in a glaucoma virtual clinic for the triaging of patients who need further assessment with gonioscopy. Compared to angle width <20° or <10°, the presence of ITC ≥ 1 quadrants on AS-OCT appears to be a more effective triaging criterion to identify those who need further assessment with gonioscopy.
Summary
What was known before
-
Recently, two landmark trials (EAGLE and ZAP) have redefined interventions for angle closure.
-
Therefore, the relevant clinical pathway needs to be revisited
-
There are very limited data on the burden of PACS referrals on hospital-based services or on the accuracy of PACS referrals initiated by community optometrists
-
There are no previously published criteria for further assessment from a virtual to a face-to-face setting.
What this study adds
-
Using real world data in the UK, we found that PACS referrals represent a substantial burden to hospital eye services and their accuracy is low
-
We also found that PACS referrals mostly represent individuals at low risk of vision loss, even if occludable angles are confirmed on gonioscopy
-
Our data also suggest that AS-OCT is a useful modality in a glaucoma virtual clinic for the triaging of patients who need further assessment with gonioscopy
-
The presence of iridotrabecular contact in at least one quadrants on AS-OCT appears to be a more effective than angle width as a triaging criterion to identify those who need further assessment with gonioscopy
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
NICE guidance for angle closure (Last revised in February 2023) [Available from: https://cks.nice.org.uk/topics/glaucoma/management/acute-angle-closure-angle-closure-glaucoma/.
Azuara-Blanco A, Burr J, Ramsay C, Cooper D, Foster PJ, Friedman DS, et al. Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): a randomised controlled trial. Lancet. 2016;388:1389–97.
He M, Jiang Y, Huang S, Chang DS, Munoz B, Aung T, et al. Laser peripheral iridotomy for the prevention of angle closure: a single-centre, randomised controlled trial. Lancet. 2019;393:1609–18.
The Royal College of Ophthalmologists. Clinical Guidelines. The Management of Angle-Closure Glaucoma 2022 [Available from: https://www.rcophth.ac.uk/resources-listing/management-of-angle-closure-glaucoma-guideline/.
Simons AS, Vercauteren J, Barbosa-Breda J, Stalmans I. Shared care and virtual clinics for glaucoma in a hospital setting. J Clin Med. 2021;10:4785.
Lawal AK, Rotter T, Kinsman L, Machotta A, Ronellenfitsch U, Scott SD, et al. What is a clinical pathway? Refinement of an operational definition to identify clinical pathway studies for a Cochrane systematic review. BMC Med. 2016;14:35.
Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health. 2021;9:e489–e551.
Radhakrishnan S, Rollins AM, Roth JE, Yazdanfar S, Westphal V, Bardenstein DS, et al. Real-time optical coherence tomography of the anterior segment at 1310 nm. Arch Ophthalmol. 2001;119:1179–85.
Van Herick W, Shaffer RN, Schwartz A. Estimation of width of angle of anterior chamber. Incidence and significance of the narrow angle. Am J Ophthalmol. 1969;68:626–9.
Shaffer RN, Schwartz A. Gonioscopy. Surv Ophthalmol. 1957;2:389–409.
Friedman DS. Angle closure and angle closure glaucoma: reports and consensus statements of the 3rd global aigs consensus meeting on angle closure glaucoma: The Hague, The Netherlands: Kugler Publications; 2006.
Becker BSR Diagnosis and Therapy of the Glaucomas: C.V. Mosby; 1965.
Nolan WP, See JL, Chew PT, Friedman DS, Smith SD, Radhakrishnan S, et al. Detection of primary angle closure using anterior segment optical coherence tomography in Asian eyes. Ophthalmology. 2007;114:33–9.
Annoh R, Loo CY, Hogan B, Tan HL, Tang LS, Tatham AJ. Accuracy of detection of patients with narrow angles by community optometrists in Scotland. Ophthalmic Physiol Opt. 2019;39:104–12.
Government GosGTS. https://www.sehd.scot.nhs.uk/pca/PCA2022(O)01.pdf [General ophthalmic services (GOS). The Scottish Government].
Bowling B, Chen SD, Salmon JF. Outcomes of referrals by community optometrists to a hospital glaucoma service. Br J Ophthalmol. 2005;89:1102–4.
Tuck MW, Crick RP. Efficiency of referral for suspected glaucoma. BMJ. 1991;302:998–1000.
Sheldrick JH, Ng C, Austin DJ, Rosenthal AR. An analysis of referral routes and diagnostic accuracy in cases of suspected glaucoma. Ophthalmic Epidemiol. 1994;1:31–9.
Vernon SA, Ghosh G. Do locally agreed guidelines for optometrists concerning the referral of glaucoma suspects influence referral practice? Eye (Lond). 2001;15:458–63.
Theodossiades J, Murdoch I, Cousens S. Glaucoma case finding: a cluster-randomised intervention trial. Eye (Lond). 2004;18:483–90.
Lockwood AJ, Kirwan JF, Ashleigh Z. Optometrists referrals for glaucoma assessment: a prospective survey of clinical data and outcomes. Eye (Lond). 2010;24:1515–9.
Shah S, Murdoch IE. NICE - impact on glaucoma case detection. Ophthalmic Physiol Opt. 2011;31:339–42.
Founti P, Topouzis F, Holló G, Cvenkel B, Iester M, Haidich AB, et al. Prospective study of glaucoma referrals across Europe: are we using resources wisely? Br J Ophthalmol. 2018;102:329–37.
Khan S, Clarke J, Kotecha A. Comparison of optometrist glaucoma referrals against published guidelines. Ophthalmic Physiol Opt. 2012;32:472–7.
Landgren K, Peters D. A prospective study on effectiveness of elevated intraocular pressure as a criterion for glaucoma referrals by optometric practitioners in Sweden. Acta Ophthalmol. 2021;99:e1098–e105.
Nilsson AG, Peters D. Effectiveness of elevated intraocular pressure as a criterion for glaucoma referral after 6 years of follow-up. Clin Ophthalmol. 2021;15:3041–9.
Huang J, Yapp M, Hennessy MP, Ly A, Masselos K, Agar A, et al. Impact of referral refinement on management of glaucoma suspects in Australia. Clin Exp Optom. 2020;103:675–83.
The College of Optometrists. Clinical Management Guidelines [Available from: https://www.college-optometrists.org/clinical-guidance/clinical-management-guidelines/primaryangleclosure_primaryangleclosureglaucoma_pa.
The Scottish Intercollegiate Guidelines Network (SIGN) 2015 [Available from: https://www.sign.ac.uk/our-guidelines/glaucoma-referral-and-safe-discharge/.
Jindal A, Ctori I, Virgili G, Lucenteforte E, Lawrenson JG. Non-contact tests for identifying people at risk of primary angle closure glaucoma. Cochrane Database Syst Rev. 2020;5:Cd012947.
Azuara-Blanco A. Cochrane corner: non-contact tests for identifying people at risk of primary angle closure glaucoma. Eye (Lond). 2021;35:1048–9.
Foster PJ, Devereux JG, Alsbirk PH, Lee PS, Uranchimeg D, Machin D, et al. Detection of gonioscopically occludable angles and primary angle closure glaucoma by estimation of limbal chamber depth in Asians: modified grading scheme. Br J Ophthalmol. 2000;84:186–92.
Day AC, Baio G, Gazzard G, Bunce C, Azuara-Blanco A, Munoz B, et al. The prevalence of primary angle closure glaucoma in European derived populations: a systematic review. Br J Ophthalmol. 2012;96:1162–7.
Porporato N, Baskaran M, Tun TA, Sultana R, Tan M, Quah JH, et al. Understanding diagnostic disagreement in angle closure assessment between anterior segment optical coherence tomography and gonioscopy. Br J Ophthalmol. 2020;104:795–9.
Radhakrishnan S, Chen PP, Junk AK, Nouri-Mahdavi K, Chen TC. Laser Peripheral Iridotomy in Primary Angle Closure: A Report by the American Academy of Ophthalmology. Ophthalmology. 2018;125:1110–20.
The Royal College of Ophthalmologists. The Way Forward 2017 [Available from: https://www.rcophth.ac.uk/standardspublications-research/the-way-forward/.
Sakata LM, Lavanya R, Friedman DS, Aung HT, Seah SK, Foster PJ, et al. Assessment of the scleral spur in anterior segment optical coherence tomography images. Arch Ophthalmol. 2008;126:181–5.
Wong HT, Chua JL, Sakata LM, Wong MH, Aung HT, Aung T. Comparison of slitlamp optical coherence tomography and scanning peripheral anterior chamber depth analyzer to evaluate angle closure in Asian eyes. Arch Ophthalmol. 2009;127:599–603.
Sakata LM, Lavanya R, Friedman DS, Aung HT, Gao H, Kumar RS, et al. Comparison of gonioscopy and anterior segment ocular coherence tomography in detecting angle closure in different quadrants of the anterior chamber angle. Ophthalmology. 2008;115:769–74.
Narayanaswamy A, Sakata LM, He M-G, Friedman DS, Chan Y-H, Lavanya R, et al. Diagnostic performance of anterior chamber angle measurements for detecting eyes with narrow angles: an anterior segment OCT study. Arch Ophthalmol. 2010;128:1321–7.
European Glaucoma Society. Terminology and Guidelines for Glaucoma. 5th Edition: PubliComm, Savona, Italy 2020.
Gedde SJ, Chen PP, Muir KW, Vinod K, Lind JT, Wright MM, et al. Primary angle-closure disease preferred practice pattern®. Ophthalmology. 2021;128:P30–70.
Asia Pacific Glaucoma Society. Glaucoma Guidelines. 3rd Edition. Amsterdam, The Netherlands: Kugler Publications; 2016.
Ho YF, Hu FC, Lee PI. The advantages and challenges of using real-world data for patient care. Clin Transl Sci. 2020;13:4–7.
US Food and Drug Administration. Real-World Evidence 2022 [Available from: https://www.fda.gov/science-research/science-and-research-special-topics/real-world-evidence.
Author information
Authors and Affiliations
Contributions
Design of the study: PF, WN. Data acquisition: AN, AR, NN, SBT. Data analysis: PF, WN, AN, AR, NN, SBT. Interpretation of data: PF, AN, AR, NN, SBT, RT, AS, AM, WN. Drafting the work: PF, WN. Revising the work critically for important intellectual content: PF, AN, AR, NN, SBT, RT, AS, AM, WN Final approval of the version to be published: PF, AN, AR, NN, SBT, RT, AS, AM, WN. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: PF, AN, AR, NN, SBT, RT, AS, AM, WN.
Corresponding author
Ethics declarations
Competing interests
PF and WN received honorarium from Thea. The authors declare no competing financial interests in relation to the work described.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Founti, P., Narayan, A., Raja, A. et al. Outcomes of newly referred patients with suspected angle closure: do we need to redefine the clinical pathways?. Eye 38, 514–519 (2024). https://doi.org/10.1038/s41433-023-02713-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02713-7
- Springer Nature Limited