Abstract
Aims
To present current practice patterns in the diagnosis and management of Cytomegalovirus anterior uveitis (CMV AU) by uveitis experts worldwide.
Methods
A two-round modified Delphi survey with masking of the study team was performed. Based on experience and expertise, 100 international uveitis specialists from 21 countries were invited to participate in the survey. Variation in the diagnostic approaches and preferred management of CMV AU was captured using an online survey platform.
Results
Seventy-five experts completed both surveys. Fifty-five of the 75 experts (73.3%) would always perform diagnostic aqueous tap in suspected CMV AU cases. Consensus was achieved for starting topical antiviral treatment (85% of experts). About half of the experts (48%) would only commence systemic antiviral treatment for severe, prolonged, or atypical presentation. The preferred specific route was ganciclovir gel 0.15% for topical treatment (selected by 70% of experts) and oral valganciclovir for systemic treatment (78% of experts). The majority of experts (77%) would commence treatment with topical corticosteroid four times daily for one to two weeks along with antiviral coverage, with subsequent adjustment depending on the clinical response. Prednisolone acetate 1% was the drug of choice (opted by 70% of experts). Long-term maintenance treatment (up to 12 months) can be considered for chronic course of inflammation (88% of experts) and those with at least 2 episodes of CMV AU within a year (75–88% of experts).
Conclusions
Preferred management practices for CMV AU vary widely. Further research is necessary to refine diagnosis and management and provide higher-level evidence.
Similar content being viewed by others
Introduction
Uveitis comprises a spectrum of intraocular inflammatory processes of infectious or non-infectious origin that, in addition to the uvea, may affect adjacent structures, including the vitreous, retina, and optic nerve [1]. Infectious uveitis accounts for about 20% and 50% of cases in developed and developing countries, respectively [2, 3]. The predominant causative organisms of infectious uveitis also show regional differentiation, with toxoplasmosis and tuberculosis being particularly common in developing countries and herpes virus infections in developed countries [2, 3]. Accurate diagnosis is thus paramount in the choice of appropriate antimicrobial treatment [4].
A wide array of pathogens can cause infectious uveitis; management is challenged by the lack of non-invasive diagnostic tests, as well as the heterogeneous clinical presentation of each pathogen. Each specific aetiology may present variably, and conversely, several infectious agents may present similarly; thus, a high index of clinical suspicion is required [5]. Useful investigations include intraocular fluid polymerase chain reaction (PCR) testing, multimodal imaging, and other laboratory investigations [6,7,8]. For some uncommon infections, data on best management is sparse, and consensus on management is difficult to achieve. The Infectious Uveitis Treatment Algorithm Network (TITAN) group was established to address this and to provide concise and practical information for ophthalmologists who manage patients with infectious uveitis.
Viral uveitis, in general, is not uncommon. Recently Cytomegalovirus anterior uveitis (CMV AU) has increasingly been reported, especially from Asia [9]. CMV AU has been associated with several clinical signs, many specific, including coin-shaped corneal lesions with keratic precipitates (KPs) in a ring, nodular corneal endothelial lesions, severely elevated intraocular pressure (IOP), and reduced corneal endothelial cell count. Anterior chamber paracentesis for aqueous analysis may be used if clinical signs are insufficient. Treatment involves controlling both inflammation and raised IOP while suppressing CMV viral activity with local and systemic antivirals [9, 10]. However, there are no expert consensus recommendations; most evidence is based on case reports or series with heterogeneous outcomes [11]. This study investigates the current state of preferred management practise for CMV AU based on a two-round modified Delphi survey of uveitis experts worldwide, aiming to reveal areas of strong consensus that can be put forth as guidelines, as well as areas of disagreement, so as to better inform the ophthalmic community and establish a baseline for further higher-level research into CMV AU.
Methods
Study design
A two-round online modified Delphi survey of CMV AU diagnosis, treatment, and prognosis was conducted [12, 13]. A TITAN working group consisted of 23 international uveitis specialists and three fellowship-trained uveitis specialists to identify management knowledge in the existing scientific evidence. The first survey was disseminated to 100 selected uveitis experts worldwide with consent. The core team members selected experts for the study based on their experience as uveitis specialists acknowledged by membership in the International Uveitis Study Group or relevant published works on uveitis topic. A literature review was provided for reference, and its level of evidence (Supplementary file 1) was graded using the Oxford Centre for Evidence-Based Medicine Levels of Evidence criteria [14]. Anonymity of participants was achieved by masking the study team. A follow-up survey followed, addressing topics requiring clarification. Ethics approval for the study was obtained from the Postgraduate Institute of Medical Education and Research in North India (No: INT/IEC/2020/SPL-405).
Survey questions
For the first round, responses were gathered using an online platform by providing multiple-choice questions or questions that needed to be answered with the Likert scale (scale 0 to 5). A hypothetical clinical scenario was provided as a CMV AU case in a healthy immunocompetent individual with classical signs and symptoms and no complications. Thirty-one questions were distilled from the literature review, comprising 7 on diagnosis and investigation, 17 on therapy, and 7 on follow-up. Additional open-comment sections were provided for every question to capture relevant thoughts that could be potentially explored in the second round. The core members then analysed responses from the first round of the survey for further deliberation to construct questions for the second round. Items with less than 65% agreement (for multiple-choice responses) and IQR > 1 (for Likert-scale responses) from the first-round survey were discarded as they were considered to have insufficient agreements among experts. In the second round of the survey, general results obtained from the first round were shown. Questions were distilled as further explanatory questions with either multiple-choice or Likert-scale responses comprising 4 questions on diagnostics, 10 on treatment approach, and 3 on follow-up and complications. The details of the survey questions are provided in Supplementary Files 2 and 3.
Data analysis
Statistical analysis was performed using IBM® SPSS® Statistics version 27. We presented the most frequent response to a particular question/statement. Median score and interquartile range (IQR ranging from 0–3) were presented for the Likert scales. We then determined strong agreement or consensus to be achieved if a particular response reached ≥75% of agreement or IQR ≤ 1 as previously suggested for achieving agreements from a Delphi survey [12]. These cut-offs were selected to represent a high level of consensus for those concerning items so that reliable guidelines that the group can recommend can be generated from it. Otherwise, the range of answers for a particular topic or question was presented as proportions and percentages.
Results
One hundred uveitis specialists from 21 countries were invited to participate in the first questionnaire;76 (76%) responded (Supplementary File 4). These 76 experts were subsequently asked to complete a second questionnaire, and 75 responded. The number of participants from each region is shown in Table 1.
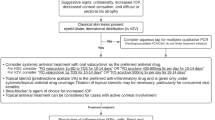
Diagnosis and initial investigations
Unilaterality and raised IOP were considered as quite specific signs for CMV AU by 30 (39%) and 34 (44%) of experts, respectively. Decreased corneal sensation (56 experts, 73%), anterior synechiae (70, 91%), posterior synechiae (70, 91%), iridoplegia (55, 71%), and engorged iris vessels (58, 75%) were considered not specific at all for CMV AU. Based on the further analysis in the second survey, only a minority of experts stated that corneal oedema (28 experts, 37%), diffuse KPs (37, 49%), stellate KPs (25, 33%), granulomatous KPS (22, 29%), or diffuse iris atrophy (36, 48%) could be considered highly suspicious of CMV AU at the first presentation. Corneal oedema, diffuse KPs, and diffuse iris atrophy were listed more by Asian experts as suggestive signs to suspect CMV AU than experts from other regions (Table 2).
Almost three-quarters of experts would consider always performing a diagnostic aqueous tap for suspected CMV AU. Most experts (70%) would send aqueous samples for qualitative multiplex PCR if an aqueous analysis is performed. Only 36% of experts would perform serology to aid diagnosis. However, half of the European experts would perform both CMV serology and PCR of aqueous (Table 2).
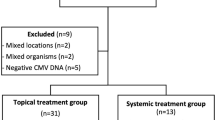
Treatment
There was strong agreement (68 experts, 85.5%) to commence topical antivirals, with 42.1% (32 experts) combining it with systemic antiviral treatment. Ganciclovir gel 0.15% was the antiviral of choice of 70% of experts. However, there was variation in systemic antiviral indication: 48% would prescribe it only for severe, prolonged or atypical CMV AU. In contrast, 33% would use a combination of topical and systemic antiviral routinely, and 13% would stick only to topical antiviral. Thematic analysis indicated that experts favouring sole or initial use of topical antivirals are concerned about the cost and side effects of systemic antivirals. Additional reasons for using systemic antiviral routinely include local unavailability of topical antiviral and the wish to achieve rapid disease control. Oral valganciclovir was the choice of drug for 78% of experts if a systemic antiviral was to be given. Opinions on antiviral dosage varied. Although 67% of experts would use ganciclovir gel 0.15% three to four times daily for one month and oral valganciclovir 900 mg twice daily for two to three weeks, of the subset of USA experts, only 45% agreed with this regimen; Table 3. Thematic analysis revealed a consideration to give intravitreal ganciclovir and intravenous foscarnet as local and systemic options for severe disease or in the case of complications/contraindications to oral valganciclovir. For maintenance antiviral following an acute episode, 60% would select ganciclovir gel 0.15% twice daily for up to 12 months (and oral valganciclovir 450 mg once or twice daily for up to 12 months if required).
If a patient had experienced at least two episodes of CMV AU within one year, 88% would consider long-term topical antiviral. 44% of them would add a long-term systemic antiviral. If inflammation flared during maintenance, 88% would restart antiviral at the initial dosage and taper more slowly. For patients with a chronic course of inflammation (noticeable persistent anterior chamber inflammation for >3 months [9]), 88% would use long-term antiviral with or without anti-inflammatory treatment.
Compared to non-steroidal anti-inflammatory drugs (NSAID), topical corticosteroids were generally preferred by 95% of experts. The majority (71%) agreed that topical corticosteroids should only be initiated with appropriate antiviral coverage (topical or systemic). The topical corticosteroid of choice was prednisolone acetate 1% (71%). Of note, 25% of USA experts preferred dexamethasone 0.1%. There was strong agreement (88%) that periocular and systemic corticosteroids should be avoided. A four-times daily topical corticosteroid regimen for one to two weeks with subsequent adjustment depending on the response was preferred by 77% of experts. It was agreed by 84% that topical corticosteroid required tapering over up to 12 months, according to clinical response. For patients who experienced at least two episodes of CMV AU within one year, 75% would use long-term topical anti-inflammatory therapy; most (88%) would restart this at initial dosages with a more gradual taper. The drug of choice to lower IOP was a topical beta-blocker (opted by 79% of experts). Thematic analysis showed a preference for combination therapy with alpha agonist or carbonic anhydrase inhibitors (topical or systemic) as second-line drugs and avoidance of prostaglandin analogues when IOP is uncontrolled with topical beta-blocker.
Follow-up and complications
Ninety-two percent of experts felt that clinical monitoring of the response to treatment was sufficient without repetition of PCR testing. Normalisation of IOP and resolution of signs of inflammation (i.e. AC cells and KP) were the primary endpoints (77% and 96%, respectively). No other clinical feature reached consensus in monitoring CMV AU patients. In patients on systemic antiviral therapy, there was consensus (87%) on the need to monitor complete blood counts, renal and liver function 2 to 4 times yearly. For patients who prematurely discontinued treatment, 78% felt no need to recommence antiviral treatment unless inflammation of CMV AU recurred. The summary of the current practice pattern with ≥75% experts is presented in Table 4. The table shows areas of significant expert agreement ranging from the route and type of antiviral, anti-inflammatory, and anti-glaucoma medication to be used, as well as general monitoring principles for resolution and treatment suggestions for chronic cases.
Discussion
With 80% of the global population estimated to be CMV seropositive, it is currently amongst the commonest viral infections [15, 16]. In recent years, it has been better appreciated that CMV can cause retinitis in the immunocompromised and CMV AU in the immunocompetent. It is more frequent in Asia, accounting for up to 66% of viral AU [17,18,19,20,21]. CMV AU data from the western part of the world was mainly reported from case reports, making it difficult to estimate the overall prevalence [19, 22]. CMV can present as self-limiting AU; acute relapsing hypertensive AU resembling Posner-Schlossman syndrome (PSS); or chronic AU resembling Fuchs uveitis syndrome (FUS) [23]. The disease is believed to result from either CMV activation in the anterior segment or local immunomodulatory cell activation in response to the virus, possibly resident macrophages [23, 24]. The role of antiviral and anti-inflammatory treatment in CMV AU has been discussed previously but without consensus on the mode of treatment or duration and with variable outcomes [25,26,27]. The absence of international agreement on diagnostic criteria, investigation, treatment, and follow-up represents an unmet need in the management of CMV AU that precipitated this study. This study does not restrict discussion to PCR-positive CMV AU cases, and suspicion of CMV can be based on clinical judgment.
This report involved 76 uveitis specialists worldwide experienced in treating CMV AU. A high response rate, large sample size (n = 75, 75%), and respondent anonymity ensured accurate sampling of current CMV AU management with limited response bias. The hypothetical case of a classical, uncomplicated presentation of CMV AU replicated the most common clinical scenario and thus provoked the most thoughts on CMV AU daily management. In this study, From the study results, many aspects of CMV AU ranging from diagnosis to treatment were not able to reach the predetermined threshold for a strong consensus for this study group to confidently recommend to the wider ophthalmic community for adoption. These will be further discussed below.
Only unilaterality and raised IOP were considered quite specific signs of CMV AU. Corroborative signs and diagnostic profiles for CMV AU are widely described in the literature, including specific KP morphology such as coin-shaped or linear distribution and iris atrophy but intact corneal sensation [23, 28]. However, there was a significant overlap with signs seen with other viral AU. Also, variations in CMV AU presentation, especially chronic in Asian and Western patients, might contribute to the differing opinions on the diagnosis [23]. Based on the previous meta-analysis [29], pooled frequency of raised IOP among PCR-positive CMV AU was 95.31% (90.45–98.60) despite the range of presentations of CMV AU, from acute hypertensive AU (i.e., Posner-Schlossman Syndrome) to chronic AU with and without endotheliitis. Moreover, iris atrophy was only encountered in 34.14% (25.32–43.54) cases. Description of the corneal lesion and specific KPs morphology was not further elaborated on due to variable clinical presentation reports [29]. Thus we also did not exhaustively elaborate on the survey questions. As clinical evidence of treatment outcomes with the current regimen is obtained mainly from studies in Asia [29], CMV AU prevalence is probably higher in Asian countries and populations compared to the West, as mentioned above, and even in confirmed CMV AU cases, ethnicity might alter the disease phenotype. Hence, ophthalmologists treating patients from varying backgrounds may have to consider more definitive ways of achieving a diagnosis, i.e., through invasive means like an AC paracentesis and PCR test.
There was a variation on whether AC paracentesis for PCR testing was necessary for suspected CMV AU cases, although the results almost reached a strong consensus at 73.3%. We postulate that the high proportion of respondents moving on to perform invasive testing is due to the lack of specific clinical signs, as mentioned above, for CMV AU to make a confident clinical diagnosis. From our previous meta-analysis, only low-grade anterior chamber inflammation (AC cells ≤2 + ) with high IOP was prevalent in CMV AU with positive PCR for CMV DNA, although we did not quantify its sensitivity and specificity [29]. This is in contradiction to HSV or VZV AU, where crops of vesicles, dermatomal skin lesions, and decreased corneal sensation may enable one to clinch the diagnosis clinically. CMV AU classification criteria had been developed by the Standardisation of Uveitis Nomenclature Working Group [30]. In their paper, it is mandatory to have a positive aqueous PCR due to the lack of diagnostic clinical signs for CMV AU, though they did qualify that as a research classification criterion, their emphasis was on specificity, whereas a clinical diagnostic criteria may prioritise sensitivity. Moreover, our meta-analysis suggested that CMV treatment for acute hypertensive and chronic CMV AU with and without endotheliitis in PCR-proven cases resulted in satisfactory clinical resolution [29]. In the meantime, treatment for PCR-unproven cases was not thoroughly investigated [29]. The implications of a negative PCR test in a patient with suspicious signs were not further discussed. Such cases must be interpreted in the context of regional disease prevalence and pre-test probability. There was general agreement that CMV serology was unnecessary in routine cases, but with significant regional variation: 50% in Europe would do CMV serology compared to only 17.6% from Asia and 18.2% from the USA. Paracentesis in uveitis is generally a safe procedure [31, 32]. The availability and high specificity of PCR testing have probably made GWC analysis less popular [33]. While our study did not deep dive into the reasons why some might opt to do or defer an anterior chamber paracentesis, we believe that it is likely multifactorial ranging from clinical reasons such as local disease prevalence and pretest probabilities to technical reasons such as the availability of the tests and cost, not forgetting the individual patient’s wishes and preferences. Individual analysis of those potentially contributing factors in each centre is out of the scope of this paper.
There was an agreement with previous studies on the use of topical antiviral [27, 34], but there was variation in the use of systemic antiviral. One-third of specialists would start systemic antiviral routinely (30% in the Americas; 23% in Europe; 42% in Asia-Pacific), whereas some experts would reserve it for recalcitrant CMV AU [26]. This reflects the challenge of balancing the risks of bone marrow suppression from systemic treatment against the risk of CMV AU progression and potential visual loss. In addition, as the usage of both ganciclovir eye gel 0.15% and oral valganciclovir is considered off label treatment in CMV AU, respondents in different healthcare settings may have to navigate through regulatory hurdles. Cost and availability of such antivirals are also issues to consider, which may have prevented consensus from being achieved. Nonetheless, the survey shows a clear preference for topical antivirals as a minimum for first line therapy. This is also strongly supported by our previous meta-analysis finding [29], which is complementary in terms of treatment. Our previous meta-analysis suggests giving 0.15% ganciclovir ophthalmic gel ≥5×/day for ≥ 2 weeks and oral valganciclovir 900 mg 2×/day for 2–3 in acute hypertensive CMV AU. However, chronic CMV AU might require an increased antiviral regimen: 1–2% topical ganciclovir ≥ 6×/day for 2–4 or oral valganciclovir 900 mg 2×/day for 3 weeks. For those presenting with significant endotheliitis, the regimen still can be leveraged: 0.5–2% topical ganciclovir ≥6×/day for 4 weeks or oral valganciclovir 900–1,800 mg 2×/day for 4 weeks [29]. This was based on the evidence that both routes may considerably achieve inflammation control. The selection of the drug can be tailor-made considering the available options. The result of our survey complements the previous meta-analysis: topical antiviral could be the initial wise option when available. However, if chronic inflammation is encountered or significant endotheliitis is present, one may switch to oral valganciclovir if a higher concentration of topical ganciclovir is unavailable. Since the consensus on the dosage of antivirals was not achieved, suggestions from our meta-analysis can be adopted.
Concern has been expressed that topical corticosteroid might trigger CMV AU [35,36,37], and this is reflected in the cautious approach shown by our experts, who would only use topical corticosteroids with antiviral cover for CMV AU. In line with this, the selection and dosage of topical corticosteroid in CMV AU were highly variable in the available literature [29] and our finding on selecting topical prednisolone acetate 1% at least 4 times per day with a slow taper can be applied in practice. Meanwhile, topical beta-blockers were the choice to treat raised IOP. The safety and efficacy of beta-blockers coupled with low cost and evidence of idiosyncratic granulomatous AU or even CMV AU with some other IOP-lowering medications may explain this preference [38,39,40].
More than 70% of CMV AU patients will experience recurrences [17, 33, 41]. This may be attributed to ganciclovir being virostatic rather than virucidal, emergence of drug-resistant strains, and an imbalance of anti-inflammatory and antiviral [33, 42, 43]. In our study, experts agreed that the treatment response could be determined clinically by observing the resolution of AC cells, KPs, and raised IOP without subsequent PCR. There were also several important follow-up management principles. The majority of experts agreed that the ophthalmologist should monitor patients on systemic antiviral therapy (valganciclovir) with CBC, renal, and liver function 2 to 4 times yearly.
The limitation of this study was participants included a greater proportion from Asia and Western Europe than North America and Africa. The annual CMV AU caseload of participants was not queried. The affordability of medications, especially valganciclovir, and accessibility of investigations and therapy are also likely to affect expert choices. Our study used a modified Delphi survey to generate variations in CMV AU management. The implementation of Delphi can vary between studies and may be affected by responses from each round [44]. Clinical scenarios or questions about some ancillary tests may introduce bias from the core members’ experience. Many aspects of CMV AU management still could not reach consensus after two rounds of the survey. However, this report is still beneficial for giving a broad picture of CMV AU management by experts worldwide.
In conclusion, the approach for CMV AU management varied among uveitis experts worldwide. The presented variation in the current practise of CMV AU management, based on region, can help ophthalmologists consider some selected options of the currently applied management approach to CMV anterior uveitis, given the lack of a standardised protocol for this disease entity. The summary table included (Table 4) represents a current snapshot of the limited but important areas of consensus on CMV AU and will serve as a platform for further research to generate more high-level data with the aim of developing CMV AU management guidelines.
Summary
What was known before
-
Cytomegalovirus (CMV) is one of the significant pathogens to cause infectious uveitis anterior. The management approach for CMV anterior uveitis lack high-level evidence and guideline.
What this study adds
-
Variable management approach for CMV anterior uveitis management is noted based on our survey involving uveitis experts worldwide. The presented variation in the current practice of CMV anterior uveitis management, based on region, can help ophthalmologists consider some selected options of the currently applied management approach to CMV anterior uveitis, given the lack of standardized protocol for this disease entity. Many aspects of CMV anterior uveitis need further elaboration from high-level evidence studies.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–16.
Zhang Y, Amin S, Lung KI, Seabury S, Rao N, Toy BC. Incidence, prevalence, and risk factors of infectious uveitis and scleritis in the United States: a claims-based analysis. PLoS One. 2020;15:e0237995.
Miserocchi E, Fogliato G, Modorati G, Bandello F. Review on the worldwide epidemiology of uveitis. Eur J Ophthalmol. 2013;23:705–17.
Sallam AB, Kirkland KA, Barry R, Soliman MK, Ali TK, Lightman S. A Review of Antimicrobial Therapy for Infectious Uveitis of the Posterior Segment. Med Hypothesis Discov Innov Ophthalmol J. 2018;7:140–55.
Rao NA. Editorial on Uveitis and Intraocular Inflammations. Asia-Pac J Ophthalmol. 2021;10:3–4.
Tabbara KF. Infectious uveitis: a review. Arch Soc Esp Oftalmol. 2000;75:215–59.
Patel A, Kelgaonkar A, Kaza H, Tyagi M, Murthy S, Pathengay A, et al. Recent Advances in Diagnosis and Treatment of Infectious Uveitis Prevalent in Asia-Pacific Region. Asia-Pac J Ophthalmol. 2021;10:99–108.
Agarwal A, Aggarwal K, Gupta V. Infectious uveitis: an Asian perspective. Eye. 2019;33:50–65.
Chan NSW, Chee SP. Demystifying viral anterior uveitis: a review. Clin Exp Ophthalmol. 2019;47:320–33.
Relvas LJ, Caspers L, Chee S-P, Zierhut M, Willermain F. Differential diagnosis of viral-induced anterior uveitis. Ocul Immunol Inflamm. 2018;26:726–31.
Harizolan D, Pleyer U. Viral aetiology in anterior uveitis-the tip of an iceberg. Eur Ophthal Rev. 2012;6:119.
Niederberger M, Köberich S. Coming to consensus: the Delphi technique. Eur J Cardiovasc Nurs. 2021;20:692–5.
Nasa P, Jain R, Juneja D. Delphi methodology in healthcare research: How to decide its appropriateness. World J Methodol. 2021;11:116–29.
Oxford Centre for Evidence-Based Medicine - levels of evidence. 2009. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009.
Lin P. Infectious uveitis. Curr Ophthalmol Rep. 2015;3:170–83.
Zuhair M, Smit GSA, Wallis G, Jabbar F, Smith C, Devleesschauwer B, et al. Estimation of the worldwide seroprevalence of Cytomegalovirus: a systematic review and meta-analysis. Rev Med Virol. 2019;29:e2034.
Chee SP, Bacsal K, Jap A, Se-Thoe SY, Cheng CL, Tan BH. Clinical features of Cytomegalovirus anterior uveitis in immunocompetent patients. Am J Ophthalmol. 2008;145:834–40.
Teoh S-B, Thean L, Koay E. Cytomegalovirus in aetiology of Posner-Schlossman syndrome: evidence from quantitative polymerase chain reaction. Eye. 2005;19:1338–40.
van Boxtel LAA, van der Lelij A, van der Meer J, Los LI. Cytomegalovirus as a cause of anterior uveitis in immunocompetent patients. Ophthalmology. 2007;114:1358–62.
Kongyai N, Sirirungsi W, Pathanapitoon K, Tananuvat N, Kunavisarut P, Leechanachai P, et al. Viral causes of unexplained anterior uveitis in Thailand. Eye. 2012;26:529–34.
Hsiao YT, Kuo MT, Chiang WY, Chao TL, Kuo HK. Epidemiology and clinical features of viral anterior uveitis in southern Taiwan—Diagnosis with polymerase chain reaction. BMC Ophthalmol. 2019;19:87.
Bhoopat T, Takhar JS, Oldenburg CE, Keenan JD, Gonzales JA, Margolis TP. Treatment of Cytomegalovirus Anterior Uveitis at a North American Tertiary Center with Oral Valganciclovir. Cornea. 2020;39:584–9.
Chan NSW, Chee SP, Caspers L, Bodaghi B. Clinical features of CMV-associated anterior uveitis. Ocul Immunol Inflamm. 2018;26:107–15.
Carmichael A. Cytomegalovirus and the eye. Eye 2012;26:237–40.
de Schryver I, Rozenberg F, Cassoux N, Michelson S, Kestelyn P, Lehoang P, et al. Diagnosis and treatment of Cytomegalovirus iridocyclitis without retinal necrosis. Br J Ophthalmol. 2006;90:852–5.
Chee SP, Jap A. Cytomegalovirus anterior uveitis: outcome of treatment. Br J Ophthalmol. 2010;94:1648–52.
Su C-C, Hu F-R, Wang T-H, Huang J-Y, Yeh P-T, Lin C-P, et al. Clinical outcomes in Cytomegalovirus-positive Posner-Schlossman syndrome patients treated with topical ganciclovir therapy. Am J Ophthalmol. 2014;158:1024–1031.e2.
Hwang Y-S, Shen C-R, Chang SHL, Lai C-C, Liu C-L, Chen K-J, et al. The validity of clinical feature profiles for cytomegaloviral anterior segment infection. Graefe’s Arch Clin Exp Ophthalmol. 2011;249:103–10.
La Distia Nora R, Putera I, Mayasari YD, Hikmahwati W, Pertiwi AM, Ridwan AS, et al. Clinical characteristics and treatment outcomes of Cytomegalovirus anterior uveitis and endotheliitis: a systematic review and meta-analysis. Surv Ophthalmol. 2022;67:1014–30.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for Cytomegalovirus anterior uveitis. Am J Ophthalmol. 2021;228:89–95.
Cheung CMG, Durrani OM, Murray PI. The safety of anterior chamber paracentesis in patients with uveitis. Br J Ophthalmol. 2004;88:582–3.
Van der Lelij A, Rothova A. Diagnostic anterior chamber paracentesis in uveitis: a safe procedure? Br J Ophthalmol. 1997;81:976–9.
Pleyer U, Chee S-P. Current aspects on the management of viral uveitis in immunocompetent individuals. Clin Ophthalmol. 2015;9:1017–28.
Wong JXH, Agrawal R, Wong EPY, Teoh SC. Efficacy and safety of topical ganciclovir in the management of Cytomegalovirus (CMV)-related anterior uveitis. J Ophthalmic Inflamm Infect. 2016;6:10.
Park UC, Kim SJ, Yu HG. Cytomegalovirus endotheliitis after fluocinolone acetonide (Retisert) implant in a patient with Behçet Uveitis. Ocul Immunol Inflamm. 2011;19:282–3.
Ufret-Vincenty RL, Singh RP, Lowder CY, Kaiser PK. Cytomegalovirus retinitis after fluocinolone acetonide (Retisert) implant. Am J Ophthalmol. 2007;143:334–5.
Tugal-Tutkun I, Araz B, Cagatay A. CMV retinitis after intravitreal triamcinolone acetonide injection in a patient with Behçet’s uveitis. Int Ophthalmol. 2010;30:591–3.
Cates CA, Jeffrey MN. Granulomatous anterior uveitis associated with 0.2% topical brimonidine. Eye. 2003;17:670–1.
Warwar RE, Bullock JD, Ballal D. Cystoid macular edema and anterior uveitis associated with latanoprost use. Experience and incidence in a retrospective review of 94 patients. Ophthalmology. 1998;105:263–8.
Babu K, Murthy GJ. Cytomegalovirus anterior uveitis in immunocompetent individuals following topical prostaglandin analogues. J Ophthalmic Inflamm Infect. 2013;3:1–3.
Touhami S, Qu L, Angi M, Bojanova M, Touitou V, Lehoang P, et al. Cytomegalovirus anterior uveitis: clinical characteristics and long-term outcomes in a French series. Am J Ophthalmol. 2018;194:134–42.
Wong VWY, Chan CKM, Leung DYL, Lai TYY. Long-term results of oral valganciclovir for treatment of anterior segment inflammation secondary to Cytomegalovirus infection. Clin Ophthalmol. 2012;6:595–600.
Cheng Y-C, Kang EY-C, Hwang Y-S, Hsiao C-H. Treatment of Cytomegalovirus anterior segment infection with intravitreal injection of ganciclovir in adjunction with or without oral valganciclovir: a long-term results. Sci Rep. 2021;11:3105.
Barrios M, Guilera G, Nuño L, Gómez-Benito J. Consensus in the delphi method: What makes a decision change? Technol Forecast Soc Change. 2021;163:120484.
Funding
HNS’s work is supported by the NIH Intramural research program (IRP). The funding organisation had no role in the design or conduct of this research. Rupesh Agrawal has received NMRC Clinician Scientist Award from National Medical Research Council, Singapore, but the funding organisation has no role in the design or conduct of this research.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the intellectual development of this paper. RA and VG conceived and planned the study. ZXT and IP wrote the first draft of the paper. ZXT, IP, IT, KC performed the literature review. ZXT, IP, IT, KC, MW, SPC, ADD, JHK, BB, JET, TBA, MDD, JRS, PM, RLDN, DAJ, JHDB, HNS, DAG, MK, JLD, JTR, NPJ, QDN, CP, RA and VG contributed to interpreting the results and provided critical feedback to the paper. The final version of the paper has been seen and approved by all authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thng, Z.X., Putera, I., Testi, I. et al. The Infectious Uveitis Treatment Algorithm Network (TITAN) Report 2—global current practice patterns for the management of Cytomegalovirus anterior uveitis. Eye 38, 68–75 (2024). https://doi.org/10.1038/s41433-023-02631-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02631-8
- Springer Nature Limited
This article is cited by
-
Treatment outcomes in cytomegalovirus anterior uveitis
Scientific Reports (2024)