Abstract
Objective
To illustrate the role of non-contact widefield retinal imaging (NC-WFI) of retinopathy of prematurity (ROP) using the Clarus 700 high resolution true colour reflectance imaging.
Methods
All babies were examined by the vitreoretinal faculty in a tertiary eye care centre from a period of March 2021 to November 2021 using the indirect ophthalmoscope after pupillary dilatation. ROP grading was done according to the revised ICROP (2005) classification. NC-WFI was then performed using the Clarus 700 high resolution true colour reflectance imaging (Carl Zeiss Meditec, Dublin, CA) in the retina diagnostic set up of a tertiary eye care centre.
Results
A total of 22 babies (44 eyes) underwent NC-WFI from March 2021 to November 2021. 13 unique cases of retinopathy of prematurity with images captured on Clarus 700 and the clinical summary is described.
Conclusion
Clarus is a non-contact wide field imaging (NC-WFI) system that can capture high resolution and true colour images (images of the fundus appear similar colour to direct observation by ophthalmoscopy) helping in more accurate diagnosis and grading of the severity of ROP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Retinopathy of prematurity (ROP) is a potentially blinding disease if not screened and treated timely. Imaging the retina becomes important in ROP considering the medicolegal aspects, need for documentation and sharing with parents and students the disease findings. Imaging also plays vital role in screening and referral to eye care centre with paediatric vitreoretinal specialist and these images also helps in appropriate teleconsultation in the setting of pandemic where approach to services would be difficult [1, 2]. Imaging systems like the Ret-cam (Clarity Medical Systems, Pleasanton, CA, USA) or the 3Nethra Neo wide field imaging camera (Forus Health, India) are some of the commonly used contact imaging systems to screen ROP [3]. The contact imaging system can pose a risk of eye infection and can lead to lot of stress on the new-born due to indentation on the cornea. Contact imaging system cannot be used in eyes immediate post Anti vascular endothelial growth factor (VEGF) injection or post pars plana vitrectomy (PPV) [3,4,5]. It requires a lot of skill and training of eye care professionals to capture these images on contact imaging system [3,4,5]. For the recent few years, a non-contact widefield imaging (NC-WFI) modality like the Optos dual wavelength Panoramic 200Tx ultra-widefield imaging system (Optos PLC, Dunfermline, Scotland, UK) helped in capturing pseudo coloured fundus images of ROP babies [3, 6]. The non-contact imaging modality required less training to eye care professionals; it can be used in post-surgical eyes without any risk of infection and more importantly was less stressful for the new-born because of faster rate of image acquisition and non-contact nature. The pseudo colour image acquisition by Optos could be a disadvantage as previous reports have shown that staging the ROP at the periphery at times becomes difficult [3]. In our case series, we utilized another non-contact widefield imaging modality i.e., Clarus 700 which uses true colour reflectance imaging with high resolution. The aim of this case series is to describe for the first time, the observations of utilizing a true colour reflectance imaging system like the clarus 700 in accurate diagnosis and grading of ROP.
Materials and methods
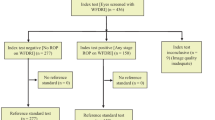
All babies were examined by the vitreoretinal faculty at a tertiary eye care centre from March 2021 to November 2021. We included all the prematurely born infants who were evaluated by our ROP team in the outpatient department of a tertiary eye care centre under the ongoing IRB approved (Ethics number LEC 08088) Indian Twin Cities ROP Study (ITCROPS) program [7,8,9]. A parent or legal guardian of the infants provided informed consent and the study adhered to the tenets of the Declaration of Helsinki. ROP grading was done according to the revised ICROP (2005) classification [10]. All babies were examined with indirect ophthalmoscope after the instillation of topical mydriatic (tropicamide 1% and phenylephrine 2.5%) 3 times at an interval of 10 min and topical proparacaine 0.5% once before inserting a paediatric Alphonso lid speculum. NC-WFI was then performed using the Clarus 700 high resolution true colour reflectance imaging (Carl Zeiss Meditec, Dublin, CA) in the retina diagnostic set up.
The babies were covered with warm clothing and held in the modified ‘flying baby position’ (Fig. 1), with one arm supporting the chest/chin and the other hand supporting the head. The head was supported towards the machine, with visual feedback on the monitor guiding the pupillary alignment and the diagnostic technician captured the images. The minimum pupillary diameter to acquire the images was 2.5 mm and the working distance (patients’ eye to front of lens) was 25 mm. Using a monochromatic camera, a broad line of illumination scans across the retina. Red, green and blue Light Emitting Diodes (LEDs) sequentially illuminate to generate true colour reflectance images which is captured on the monitor. The image acquisition speed was fast (<0.2 s) and the screen resolution was 1920 × 1080 pixels (https://www.zeiss.com/meditec/int/product-portfolio/retinal-cameras/zeiss-clarus-700/zeiss-clarus-700-specifications.html). A single image when measured from the centre of the eye gives a widefield 133-degree wide by 133-degree high field of view (FOV), 2 images stitched together gives ultra-widefield 200-degree wide in one of the dimensions and by 133-degree high in the other dimension of the FOV and montage up to six images can be constructed when we have good quality images of all 4 quadrants for the machine to create a montage (https://www.zeiss.com/meditec/int/product-portfolio/retinal-cameras/zeiss-clarus-700/zeiss-clarus-700-specifications.html). Since the babies do not fixate on the fixation target, custom montage images (2–6 images) are constructed by Clarus 700 machine which takes a series of widefield images and the technician can decide how many images to include in the montage (https://www.zeiss.com/meditec/int/product-portfolio/retinal-cameras/zeiss-clarus-700/zeiss-clarus-700-specifications.html).
Results
A total of 22 babies (44 eyes) underwent NC-WFI from period of March 2021 to November 2021. 13 unique cases of retinopathy of prematurity with images captured on Clarus 700 and the clinical summary is described below (Supplementary Table 1). None of the babies developed apnoea, cyanosis or feed intolerance during or after the procedure.
Case 1
A preterm baby with 28 weeks of gestational age, birth weight of 1200 grams and post menstrual age of 32 weeks came for ROP screening. Fundus examination showed Fig. 2A (Right eye) Fig. 2B (Left eye): Both eyes Aggressive posterior retinopathy of prematurity (APROP) with looping and shunting. Right eye is more aggressive with areas of vitreous condensation and neovascularization. The baby was planned for both eyes intravitreal Anti VEGF injection on the same day and was asked to review after 1 week post injection.
A (Right eye) B (Left eye): Both eyes Aggressive posterior retinopathy of prematurity (APROP) with looping and shunting. Right eye is more aggressive with areas of vitreous condensation and neovascularization. C (Right eye) D (Left eye): Both eyes APROP with preretinal, sub-hyaloid haemorrhage and plastered fibrin. Inferior lid artefacts were seen in both eyes fundus image.
Case 2
A preterm baby with 30 weeks of gestational age, birth weight of 1400 grams and post menstrual age of 34 weeks came for ROP screening. Fundus examination showed both eyes Aggressive posterior retinopathy of prematurity with severe looping and shunting. The baby was planned for both eyes intravitreal Anti VEGF injection on the same day and was asked to review after 1 week post injection.
Case 3
A preterm baby with 32 weeks of gestational age, birth weight of 1500 grams and post menstrual age of 39 weeks came for ROP screening. Both eyes showed Aggressive posterior retinopathy of prematurity and underwent intravitreal Anti VEGF injection on the same day and was asked to review after 1 week post injection. Status post Intravitreal Anti Vascular endothelial growth factor (VEGF) 1 week back, showed looping but reduced plus disease.
Case 4
A preterm baby with 33 weeks of gestational age, birth weight of 1500 grams and post menstrual age of 39 weeks came for ROP screening. Both eyes showed Aggressive posterior retinopathy of prematurity and underwent intravitreal Anti VEGF injection on the same day and was asked to review after 1 week post injection. Status post Anti VEGF injection given 1-week back, shows reduced plus disease in both eyes. Left eye showed significant looping and preretinal haemorrhage but with reduced plus disease.
Case 5
A preterm baby with 30 weeks of gestational age, birth weight of 1200 grams and post menstrual age of 35 weeks came for ROP screening. Figure 2C (Right eye) Fig. 2D (Left eye): Both eyes showed Aggressive posterior retinopathy of prematurity with preretinal, sub-hyaloid haemorrhage and plastered fibrin. Inferior lid artefacts were seen in both eyes fundus image. The baby was planned for both eyes intravitreal Anti VEGF injection on the same day and was asked to review after 1 week post injection.
Case 6
A preterm baby with 30 weeks of gestational age, birth weight of 1000 grams and post menstrual age of 36 weeks came for ROP screening. Both eyes showed Aggressive posterior retinopathy of prematurity with extensive pre retinal and vitreous haemorrhage. The baby was planned for both eyes intravitreal Anti VEGF injection on the same day and was asked to review after 1 week post injection.
Case 7
A preterm baby with 29 weeks of gestational age, birth weight of 900 grams and post menstrual age of 33 weeks came for ROP screening. Figure 3A (Right eye) Fig. 3B (Left eye) Both eyes Aggressive posterior retinopathy of prematurity with preretinal haemorrhage. Right eye shows plastered fibrin along the arcades. The baby was planned for both eyes intravitreal Anti VEGF injection on the same day and was asked to review after 1 week post injection. Figure 3C (Right eye) Fig. 3D (Left eye) Both eyes 1week status post Anti VEGF injection showed reduced plus disease and right eye shows preretinal haemorrhage. Right eye single image measured from the centre gives widefield 133-degree wide by 133-degree high field of view (FOV). Left eye montage of 2 images stitched together gives ultra-widefield 200-degree wide in one of the dimensions and by 133-degree high in the other dimension of the FOV.
A (Right eye) B (Left eye): Both eyes APROP with preretinal haemorrhage. Right eye shows plastered fibrin along the arcades. C (Right eye) D (Left eye): Both eyes 1week status post Anti VEGF for APROP (case number 7). Both eyes show reduced plus disease and right eye shows preretinal haem. Right eye single image measured from the centre gives widefield 133-degree wide by 133-degree high field of view. Left eye 2 images stitched to give ultra-widefield 200-degree wide in one of the dimensions and by 133-degree high in the other dimension.
Case 8
A preterm baby with 28 weeks of gestational age, birth weight of 800 grams and post menstrual age of 38 weeks came for ROP screening. Figure 4A (Right eye) Fig. 4B (Left eye) Both eyes Zone 2 stage 3 plus disease with ridge lift (Threshold ROP). The baby was planned for both eyes laser indirect ophthalmoscope on the same day and was asked to review after 1 week post laser.
Case 9
A preterm baby with 30 weeks of gestational age, birth weight of 1500 grams and post menstrual age of 40 weeks came for ROP screening. Both eyes showed Aggressive posterior retinopathy of prematurity and underwent intravitreal Anti VEGF injection in both eyes on the same day. Both eyes status post Anti VEGF 6 weeks back for Aggressive posterior retinopathy of prematurity showed reduced plus disease and the vessels reached up to zone 2 anterior.
Case 10
A preterm baby with 24 weeks of gestational age, birth weight of 770 grams and post menstrual age of 35 weeks came for ROP screening. Right eye showed zone 2 stage 4 A ROP and left eye showed zone 2 stage 3 plus disease. Both eyes underwent laser indirect ophthalmoscope on the same day. Right eye was also planned for lens sparing pars plana vitrectomy (PPV) the next day.
Case 11
A preterm baby with 30 weeks of gestational age, birth weight of 1200 grams and post menstrual age of 39 weeks came for ROP screening. Both eyes stage 4B ROP with tractional retinal detachment involving the macula. The baby was planned for both eyes lens sparing PPV.
Case 12
A preterm baby with 32 weeks of gestational age, birth weight of 1500 grams and post menstrual age of 40 weeks came for ROP screening. Both eyes showed zone 2 stage 4B ROP and was advised for same day peripheral laser in both eyes and lens sparing PPV the next day. Figure 4C (Left eye) Left eye stage 4B ROP with tractional retinal detachment (TRD) involving the fovea and disc drag noted. Figure 4D (Left eye): Fresh laser marks seen post laser indirect ophthalmoscope peripheral to the TRD just before taking the baby for vitreoretinal surgery. Right eye also showed similar features as the left eye.
Case 13
A preterm baby with 29 weeks of gestational age, birth weight of 1500 grams and post menstrual age of 32 weeks came for ROP screening. Figure 5A (Right eye) Fig. 5B (Left eye): Both eyes Aggressive posterior retinopathy of prematurity with severe looping and shunting. Two images stitched together gives ultra-widefield 200-degree wide in one of the dimensions and by 133-degree high in the other dimension of the FOV. Lid artefacts are noted in the images. The baby was planned for both eyes intravitreal Anti VEGF injection on the same day and was asked to review after 1 week post injection.
Discussion
Retinopathy of prematurity is a preventable blindness when screened and treated promptly. Imaging in new-born over the last 2 decades has revolutionized the treatment of ROP due to increased accuracy of telemedicine screening and prompt referral of treatment requiring ROP especially in areas where approach to paediatric vitreoretinal specialist services is not possible [1,2,3, 11, 12]. The most common imaging device that was used over the last decade is the Ret cam which is a contact imaging system that needs apposition on the cornea and 4–6 frames of images to capture most of the features of ROP [3, 5]. The contact imaging system needs firm corneal apposition to prevent globe rotation, it needs proper pupillary alignment to capture good images and more importantly they have slower image acquisition time even after pupillary alignment and hence needs multiple images [3, 11]. The image acquisition can be impaired in poor media clarity like corneal haze, in cases with poor pupillary dilatation and in dark pigmented fundus [3, 11]. They also impose a lot of stress on new-born and high chances of eye infection [3, 5]. Due to these limitations of the contact imaging systems (Supplementary Table 2), NC-WFI devices like Optos has been used in recent times which has faster image acquisition time and gives dual wavelength panoramic ultra-wide field pseudo-coloured images in ROP [3]. The pseudo colour image acquisition by Optos was a disadvantage as previous reports have shown that staging the ROP at the periphery at times becomes difficult [3]. NC-WFI is very much useful in stable new-born on an OPD basis. The non-contact nature makes them less stressful to babies and needs much lesser training to technicians [3]. However, in sicker babies admitted in neonatal intensive care unit, it would be difficult and Ret cam/3Nethra Neo contact imaging portable system would be handier. When compared to Optos the Clarus has the advantage of capturing high resolution, true colour reflectance images (images of the fundus appear similar colour to direct observation by ophthalmoscopy) and hence this would possibly make Clarus more accurate in diagnosis and grading the severity of ROP. It can also create ultra-wide field images when two images are stitched together into a composite image of 200-degree wide and 133-degree high field of view which is comparable with Optos field of view (https://www.zeiss.com/meditec/int/product-portfolio/retinal-cameras/zeiss-clarus-700/zeiss-clarus-700-specifications.html). Montage up to six images can be constructed when we have good quality images of all four quadrants but this would be extremely difficult to achieve as the babies do not follow the commands to get these images in every quadrant; this is one of the limitations. The other limitation of Clarus when compared to the Optos is that the Optos can capture ultra-widefield image of 200 degrees FOV in a single image. (Supplemental Table 3) Lid and eyelash artefacts especially of the lower lid can be a limitation in non-contact imaging systems and more so in Optos because of the ultra-widefield FOV in the single image. To the best of our knowledge this is the first report on ROP cases captured by Clarus NC-WF true colour reflectance imaging.
Conclusion
Clarus is a non-contact wide field imaging (NC-WFI) system that seems to be efficient in capturing high resolution true colour images in ROP. Due to its non-contact nature, it poses no threat of eye infections and requires less training to eye care professionals in capturing these images. The high resolution and true colour reflectance images (images of the fundus appear similar colour to direct observation by ophthalmoscopy) could help in more accurate diagnosis and grading the severity of ROP.
A comparative study of various contact and non-contact systems for neonatal retinal imaging could provide more insights to relative advantages of one system over the other. None of the imaging modalities currently are used exclusively for management decisions as in all cases the indirect Ophthalmoscopy remained the standard of care.
Summary
What was known before
-
Optos dual wavelength non-contact ultra-widefield imaging system helped in capturing pseudo coloured fundus images of ROP babies.
What this study adds
-
Clarus non-contact wide field imaging system can capture high resolution and true colour images helping in more accurate diagnosis and grading of the severity of ROP.
-
This helps in better explaining the ROP features to medical trainees and also in counselling the parents of the babies.
Data availability
Data set is available with author AB and at ROP database office at LV Prasad Eye Institute, Hyderabad, Telangana, India-500034.
References
Khanna RC, Garg P, Vaddavalli PK, Fernandes M, Rath S, Nayak S. et al. Response of L V Prasad Eye Institute to COVID-19 outbreak in India: experience at its tertiary eye care centre and adoption to its Eye Health Pyramid. Int J Ophthalmol. 2021;14:1–9. https://doi.org/10.18240/ijo.2021.01.01.
Sengupta S, Honavar SG, Sachdeva MS, Sharma N, Kumar A, Ram J, et al. All India Ophthalmological society-Indian Journal of Ophthalmology consensus statement on preferred practices during the COVID-19 pandemic. Ind J Ophthalmol. 2020;68:711–24.
Patel CK, Fung TH, Muqit MM, Mordant DJ, Brett J, Smith L, et al. Non-contact ultra-widefield imaging of retinopathy of prematurity using the Optos dual wavelength scanning laser ophthalmoscope. Eye (Lond). 2013;27:589–96.
Mintz-Hittner HA, Kennedy KA, Chuang AZ, BEAT-ROP Cooperative Group. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N. Engl J Med. 2011;364:603–15.
Mukherjee AN, Watts P, Al-Madfai H, Manoj B, Roberts D. Impact of retinopathy of prematurity screening examination on cardiorespiratory indices: a comparison of indirect ophthalmoscopy and retcam imaging. Ophthalmology. 2006;113:1547–52.
Patel CK, Fung TH, Muqit MM, Mordant DJ, Geh V. Non-contact ultra-widefield retinal imaging and fundus fluorescein angiography of an infant with incontinentia pigmenti without sedation in an ophthalmic office setting. J AAPOS. 2013;17:309–11.
Jalali S, Anand R, Kumar H, Dogra MR, Azad R, Gopal L. Programme planning and screening strategy in retinopathy of prematurity. Indian J Ophthalmol. 2003;51:89–99.
Jalali S, Matalia J, Hussain A, Anand R. Modification of screening criteria for Retinopathy of Prematurity in India and other middle-income group countries. Am J Ophthalmol. 2006;141:966–8.
Jalali S, Kesarwani S, Hussain A. Outcomes of a protocol-based management for zone I retinopathy of prematurity. The Indian twin cities Retinopathy of Prematurity screening program report number 2. Am J Ophthalmol. 2011;151:719–24.
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Richter GM, Williams SL, Starren J, Flynn JT, Chiang MF. Telemedicine for retinopathy of prematurity diagnosis: evaluation and challenges. Surv Ophthalmol. 2009;54:671–85. https://doi.org/10.1016/j.survophthal.2009.02.020.
Chiang MF, Wang L, Busuioc M, Du YE, Chan P, Kane SA, et al. Telemedical retinopathy of prematurity diagnosis: accuracy, reliability, and image quality. Arch Ophthalmol. 2007;125:1531–8.
Funding
Hyderabad Eye Research Foundation (2020), Hyderabad, India. The institute has received funding or support for its ongoing Retinopathy of Prematurity programs from Miriam Hyman Memorial Trust (MHMT, UK), Dalmia Holdings (India), Queen Elizabeth Diamond Jubilee Trust (UK), Public Health Foundation of India, Cognizant Foundation and the Government of India. Grant number LEC 08088.
Author information
Authors and Affiliations
Contributions
AB and SJ: Devised and designed the study, devised data collection protocol and data analysis, Literature search, wrote the Manuscript. RUR: Captured the images on Clarus. KA, DCP: Helped in Data collection, improving content and editing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Belenje, A., Reddy, R.U., Optom, B. et al. Non-contact widefield neonatal retinal imaging for retinopathy of prematurity using the Clarus 700 high resolution true colour reflectance imaging. Eye 37, 1904–1909 (2023). https://doi.org/10.1038/s41433-022-02273-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02273-2
- Springer Nature Limited