Abstract
Background
Glaucoma is the commonest cause of irreversible blindness worldwide. As it is typically asymptomatic until advanced, the risk of blindness from late presentation is higher than other eye diseases. This study aims to investigate the risk factors for late presentation of primary glaucoma patients.
Methods
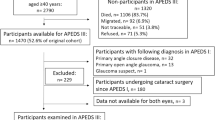
We undertook a hospital-based case-control study of a random sample of glaucoma patients from a hospital in Hong Kong. Structured questionnaires and existing information from the electronic patient record were used, and the odds of presenting late were analysed by logistic regression.
Results
Of 210 recruited participants, 83 (39.5%) presented with advanced glaucoma unilaterally or bilaterally. The mean age of participants was 61.1 ± 11.9 years, with 110 males (52.4%). Univariate analysis revealed that male sex and primary angle-closure glaucoma (PACG) have 3.06 (CI95:1.71–5.48; P < 0.001) and 2.47 (CI95:1.11–5.49; P = 0.03) times higher odds of late presentation, respectively. Multivariate analysis revealed late presenters were 3.54 (CI95:1.35–9.35; P = 0.01) times more likely to have PACG than primary open-angle glaucoma (POAG). Patients with elevated baseline intraocular pressure (IOP) also had 1.06 times higher odds of presenting with advanced glaucoma (CI95:1.02–1.11; P = 0.002). Linear regression revealed that PACG patients present with 7.12 mmHg higher IOP than POAG patients (CI95:4.23–10.0; P < 0.001).
Conclusion
In conclusion, a high proportion of glaucoma patients present late in Hong Kong, with gender and type of glaucoma being significant determinants. Our study shows that PACG presents with higher IOP and, along with male gender, are more likely to have advanced disease than POAG.
Similar content being viewed by others
Introduction
Glaucoma is defined as an optic neuropathy with a characteristic pattern of visual field (VF) loss and structural damage to the optic nerve [1]. The clinical features of glaucoma are related to the progressive loss of retinal nerve fibres, manifesting as detectable changes to the optic nerve head, and thinning of the peripapillary retinal nerve fibre layer, as well as functional impairment such as VF loss or reduction in visual acuity. There are multiple risk factors for glaucoma development, including age [2], gender [3], and family history. Currently, elevated intraocular pressure (IOP) is the only modifiable risk factor [4].
Glaucoma blindness is the commonest cause of irreversible blindness worldwide, and patients with visual impairment due to glaucoma experience a significant drop in quality of life [5, 6]. In 2010, 6.5% of the global blindness was due to glaucoma. In Hong Kong (HK), the prevalence of glaucoma is estimated to be 3.8% using data from the Guangzhou province [7], and glaucoma contributes to 11% of all visual impairment [8]. With an ageing population worldwide, it is predicted that in 2040, the number of patients affected by glaucoma globally will reach 112 million [6], with 81 million in Asia [9].
Late presentation has been shown to be a major risk factor for glaucoma blindness in several studies [10,11,12,13]. In Hong Kong (HK), there are no existing data on the proportion of glaucoma patients that present late but there is a general lack of public knowledge about glaucoma [14]. As a result, despite most of the population in HK having ready access to high-quality eye care services [15], referral to ophthalmologists may be delayed until the glaucoma is advanced or end-stage. In addition, long waiting times for public hospital appointments, high cost of healthcare care in the private sector, and relatively low uptake of private medical insurance, can all contribute to a delayed diagnosis of glaucoma.
While primary open angle glaucoma (POAG) is around six times more prevalent than primary angle closure glaucoma (PACG) globally, PACG is more prevalent in some Asian populations [16]. Studies have suggested that PACG frequently presents with higher IOP and more rapid VF loss, and thus more advanced glaucoma, compared to POAG [17, 18]. However, one study reported that among Chinese, POAG presents with higher IOP than PACG [19].
Studies have demonstrated that a positive family history of glaucoma is associated with late presentation [20, 21]. Genetic predisposition may contribute to more advanced VF loss at presentation due to a more aggressive disease subtype. However, positive family history of glaucoma can also be protective by enabling earlier presentation due to greater awareness of symptoms. It has been previously reported that patients with family history of glaucoma were three times less likely to present late compared to those with no family history [22]. It would be interesting, therefore, to investigate the effect of known first-degree family history on late presentation in HK.
This study aims to measure the stage of disease for a cohort of glaucoma patients who initially presented to the Lo Fong Shiu Po (LFSP) Eye Centre, Grantham Hospital. This is a tertiary referral and main clinical teaching centre for the Department of Ophthalmology, University of Hong Kong. Potential factors for late presentation, including mechanism of glaucoma, IOP level, age, gender, family history, and socioeconomic status, are analysed to determine if they have significant correlation with late presentation.
There are 11 public hospitals and 8 private hospitals in HK that provide ophthalmic services, as well as 96 private ophthalmologists in private clinics, with the public sector providing ophthalmic care for around 90% of patients in Hong Kong [15, 23]. Despite referral of glaucoma patients being based on geographical proximity to hospitals, HK is a small region with little variation of glaucoma prevalence between districts. Therefore, the sample recruited in Grantham Hospital is likely to be representative and generalisable to the entire city.
The prevalence of primary glaucoma in the HK population is also comparable to nearby urbanized regions in Southeast Asia with similar demographics and healthcare system, such as Singapore (2.7%) [19], Japan (3.0%) [24], and Korea (1.1%) [25].
Materials and methods
The study was a hospital-based, case-control study carried out at LFSP Eye Centre, Grantham Hospital, from May to June 2021. This study was approved by the London School of Hygiene and Tropical Medicine Ethics Committee and the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West cluster (HKU/HA HKW IRB no. UW 21–376).
Identification and recruitment of participants
Primary glaucoma patients were identified retrospectively from the hospital records and included as potential participants according to the inclusion and exclusion criteria. They were then put on a spreadsheet and randomly sampled to reduce possibilities of investigator-induced selection bias, and subsequently classified into case (late presentation of glaucoma) or control by the mean deviation (MD) value, in decibels (dB), on their VF at their first diagnosis. All patients recruited had been initially diagnosed in our hospital, with their records stored in the Electronic Patients Record (EPR). This allowed us to classify patients into cases and controls by their VF at first diagnosis.
Inclusion and exclusion criteria
Inclusion criteria:
-
(1)
Age 18 years or above
-
(2)
Diagnosed with either:
-
a.
POAG (including normal tension glaucoma); or
-
b.
PACG
-
a.
on 1st January 2016 or later (but before study recruitment date).
Exclusion criteria:
-
(1)
Secondary glaucoma
-
(2)
Other eye or neurological diseases that can affect VF, for example: retinal detachment, corneal scarring, moderate to severe cataract, other optic neuropathies or neurological disorders affecting the visual pathway
-
(3)
Unable to give informed consent
-
(4)
Participants with unreliable VF, defined as fixation loss ≥20%, false positive ≥10%, or false negative ≥10%.
Case and control definition
In this study, the MD value from a reliable automated threshold VF test at, or soon after, glaucoma diagnosis was used as the parameter for classification into either case or control [26]. The definition for severe visual glaucoma is referenced from the LiGHT trial by Gazzard et al. [27].
Cases were defined as severe glaucoma according to their level of VF loss in the following criteria for the worse eye:
-
(1)
MD ≤ -12 dB; or
-
(2)
Any point with sensitivity <0 dB within central 5 degree; or
-
(3)
Points with sensitivity <15 dB within central 5 degree in both hemifields (superior and inferior).
Controls were defined as mild or moderate glaucoma according to the following VF criteria for the worse eye:
-
(1)
VF MD > -12 dB; or
-
(2)
At least 1 point that is <15 dB within central 5 degree, but none <0 dB, and only 1 hemifield with central point <15 dB.
Due to possible learning effect, results obtained from the first VF may be unreliable. Therefore, if there was a second VF within 3 months of diagnosis, the MD of the second test was used as the presenting VF instead.
EPR were obtained for cases and controls and the following data recorded.
-
Age
-
Gender
-
Type of glaucoma
-
Cup-disc ratio
-
Visual acuity
-
VF indices (including MD)
-
Baseline IOP at presentation (before treatment)
-
Individual history of mild ocular diseases, for example, mild cataract and its grading
-
Residential address to identify housing standard.
Chosen participants were contacted individually to obtain informed consent to complete a standardized questionnaire on their income, education, occupation. Recall of first-degree family history of glaucoma, behavioural factors such as smoking and drinking habits were also obtained from the questionnaire.
Measuring social deprivation
Due to the diversity between countries on the importance of each dimension, it is difficult to form a unified guideline on the measurement of deprivation level. It can be measured on either district or individual levels. The Indices of Multiple Deprivation (IMD) is a tool developed in the UK for the measurement of social deprivation [28]. The 3 most heavily weighted domains (income, education, and occupation) were chosen in this study as measurements of social deprivation in HK, while housing is also included for analysis since there is a large gap observed in living environment between those that are deprived and their counterparts. These dimensions will be compared between the case and control group for possible association between social deprivation and glaucoma severity at diagnosis.
Income level of the individual is divided into 4 categories by their monthly household income (in HK dollars): $0–10000, $10001–25000, $25001–50000, and $50001 or above. Education is classified into 3 levels by the ISCED 2011 [29], while participants’ occupations are classified into low (skill level 1), medium (skill level 2), and high (skill levels 3–4) by the ISCO-08 [30]. Housing is classified into public and non-public.
Statistical analysis
There are no relevant data to inform an estimate of the expected difference in rates of late presentation between those of different levels of deprivation in HK. A previous UK study has shown that socioeconomically deprived patients had approximately 3 times the risk of late presentation [22], and this seems a clinically important difference hence was selected for the power calculation. We calculated that at least 48 cases and 95 controls are required to detect a threefold increase in odds of late presentation in a factor among 20% of control at a power of 80% and significance level at 5%.
Analysis was completed on STATA/SE 16.1. The odds of late presentation were analyzed by univariate and multivariate logistic regression on 3 models to estimate the significance of observed differences between case and control. Central tendency measures were performed on descriptive statistics for analysis.
Results
There were 210 participants, among which 83 (39.5%) presented with advanced glaucoma in at least one eye. Table 1 summarizes the demographics, socioeconomic, and medical characteristics of recruited participants with respect to their case-control status. The mean age was 61.10 ± 11.88 (mean ± SD), with 110 males (52.4%) and 100 females (47.6%). More than 60% were unemployed/retired and economically dependent. Most were POAG (86.2%).
Univariate analysis
Table 2 summarised the findings of univariate analysis of each study factor. Males (P < 0.001), PACG (P = 0.03), and higher IOP (P = 0.001) had significantly greater odds of late presentation.
Multivariate models
To determine if our study factors were independently correlated with the odds of late presentation, the odds ratios (ORs) were adjusted by 3 multivariate models, summarised in Table 3. Model I, II, and III adjusted for age; age and gender; or age, gender, behavioral and cognitive factors, respectively, which can facilitate to demonstrate the possible effect of aggressive diseases [31].
In model I, adjustment by age alone had negligible effects on the ORs of all study factors except for high education level, which had lower odds after adjustment. In model II, additional adjustment for gender showed lower odds for participants living in non-public housing. Participants with PACG had increased odds in model II and III when compared to unadjusted model and model I. There was weak evidence of higher odds for participants in the low skilled occupation group (group I) to present late in model III (P = 0.06), but not in model I and II. Multivariate analysis on IOP (left, right and worse eye) showed that higher baseline pressures were associated with increasing risk of late presentation in all 3 models.
PACG and high baseline IOP both increased the odds of presenting with advanced glaucoma (late presentation). Subsequent two-sample independent t-test confirm mean baseline IOP in PACG is significantly higher than in POAG (P < 0.001). Both univariate and multivariate linear regression by these models showed a significantly higher presenting (baseline) IOP in PACG than POAG (P < 0.001) (Table 4). This hinted at a possible causal relationship in which PACG patients have higher IOP and thus faster progression of glaucoma in diagnosis.
Discussion
Almost 40% of our randomly selected participants presented with advanced glaucoma based on perimetric mean deviation criteria, which was surprisingly high considering that Hong Kong has a well-developed and easily accessible public health system. However, this is comparable to previous studies from regions with similar level of healthcare, such as Canada (47.9%) [12] and Sweden (42.2%) [13]. Both males and PACG patients were more likely to present with advanced glaucoma in our study.
Although not statistically significant from univariate analysis, the odds of late presentation according to age appear to show a U-shaped trend with those <40 two to four times the risk compared to 41–50 (P = 0.06), 51–60 (P = 0.10) and 61–70 (P = 0.10) (Fig. 1); while the risk appears to increase slightly again for >80. Since glaucoma is more common above age 50, patients presenting below age 40 may either have a more rapidly progressive form of the disease or are more reluctant to seek early assessment, which could be due to lower incidence of major eye disorders in younger people, or greater inconvenience in scheduling consultations in working age adults (especially in the HK’s public sector where there’s less flexibility in appointment booking).
In this study, there is very strong evidence that male gender (P < 0.001) is a significant risk factor. This is consistent with other studies reporting male gender as a risk factor associated with late presentation [22, 31, 32]. Although both genders have ready access to public healthcare in HK, it is likely that most men are the main household income earner and the inconvenience of arranging for an ophthalmic assessment, especially in the public health sector, may explain their higher risk for late presentation. This is particularly relevant in our study, as most of participants are still working with a mean age of 61.
PACG and elevated IOP were identified as significant risk factors for late presentation, while both univariate and multivariate linear regression have demonstrated strong evidence that PACG presents with higher IOP. This result is comparable to those from other studies showing PACG patients have higher IOP, which is a significant risk factor for glaucoma progression, and therefore more likely to present with more advanced disease [17, 18].
Previous studies from different regions have suggested social deprivation as a risk factor for late presentation of multiple chronic diseases, including glaucoma [12, 21, 22, 32,33,34]. This finding is not confined to low-and-middle-income regions but include high-income ones too. In contrast, our current study did not find any significant relationship between socioeconomic status of an individual and their late presentation of glaucoma in univariate or multivariate analysis. There was weak evidence in univariate analysis (P = 0.10) and multivariate analysis Model III (P = 0.07) of possibly higher risk in the low-skilled occupation group, but a larger sample size may be required to confirm this. As participants in lower skilled occupations often have longer working hours (for example, security guard) and, as for younger and male participants, may have greater difficulty in scheduling healthcare consultations.
Interestingly, a first-degree family history of glaucoma conferred no significant reduction to the odds of late presentation. A possible reason may be a lack of awareness that primary glaucoma may present with genetic clustering. Further research on glaucoma knowledge and awareness of patients would help to confirm this hypothesis.
Healthcare implications
Almost 40% of our glaucoma patients presented late, possibly due to the lack of any glaucoma screening programme and low disease awareness. While a population-wide screening programme for glaucoma specifically may not be cost-effective [35], recent advancements in artificial intelligence and machine learning may have, or will likely, change this situation, especially when combined with screening for other common and treatable eye conditions (age-related or myopia-related macular degenerations) in high risk populations (age > 50, family history, high myopia) [36].
There are possible barriers to early glaucoma diagnosis in the public sector faced by certain population groups in HK, such as age <40, men, and those in low-skilled occupations. A common factor among these groups may be difficulty scheduling ophthalmic assessment at a convenient time and place. Our current study was not designed to explore this issue, but future studies looking into the role of working culture (including normal working hours and ease of obtaining medical leave) for different occupations would be warranted. Here again, advancement in telemedicine will likely improve access to ophthalmic care and mitigate this problem in the future [37].
There are some weaknesses of our study. This includes recall bias, as the social deprivation status relies on the participants’ recollection of the period when they were first diagnosed with glaucoma. This may be difficult or inaccurate if this had occurred many years ago. However, we believe our results should not have been significantly affected, as social deprivation status tends to be stable over short periods of time and we had intentionally only recruited participants diagnosed with glaucoma within 5 years of the study.
Another limitation lies in the scope of the study. Data collection was confined to a single hospital, out of 11 public hospitals providing ophthalmic service in HK, and no participants using private medical services were included. However, we do not believe there would be a significant difference between public hospital patients from different regions of HK, given the small geographic area of this city (1106 km2). Since around 90% of patients in HK are under the care of public health services, we believe our results is generalizable to the majority of glaucoma patients in this city.
In conclusion, this study has highlighted the high proportion of glaucoma patients who present with advanced disease in Hong Kong. Male gender and PACG were significant risk factors for late presentation, while age <40 and low-skilled occupation may also be possible risk factors that warrants further exploration with a larger sample size. Our study also confirms that PACG presents with higher baseline IOP, as previously reported, which may explain their more advanced disease on presentation.
Summary
What was known before
-
Late presentation is a risk factor for glaucoma blindness
-
PACG patients may present with higher intraocular pressure than POAG patients
What this study adds
-
Late presentation is common in urban Southeast Asian regions e.g. Hong Kong
-
Male and PACG patients are more prone to late presentation of glaucoma
-
Higher intraocular pressure explains why PACG presents with more advanced glaucoma
Data availability
Deidentified individual participant data that underlies the results reported in this article are available for sharing. Data will be available upon request immediately following publication and ending 5 years following article publication, with investigators whose proposed use of the data has been approved by an independent review committee identified for this purpose. Proposals should be directed to laianakinlai2@gmail.com.
References
Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86:238–42.
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–7.
Vajaranant TS, Nayak S, Wilensky JT, Joslin CE. Gender and glaucoma: what we know and what we need to know. Curr Opin Ophthalmol. 2010;21:91–9.
Wu J, Mak HK, Chan YK, Lin C, Kong C, Leung CKS, et al. An in vitro pressure model towards studying the response of primary retinal ganglion cells to elevated hydrostatic pressures. Sci Rep. 2019;9:9057.
Quaranta L, Riva I, Gerardi C, Oddone F, Floriani I, Konstas AG. Quality of Life in Glaucoma: A Review of the Literature. Adv Ther. 2016;33:959–81.
Jonas JB, Aung T, Bourne RR, Bron AM, Ritch R, Panda-Jonas S. Glaucoma. Lancet. 2017;390:2183–93.
He M, Foster PJ, Ge J, Huang W, Zheng Y, Friedman DS, et al. Prevalence and Clinical Characteristics of Glaucoma in Adult Chinese: A Population-Based Study in Liwan District, Guangzhou. Investig Opthalmol Vis Sci. 2006;47;2782–88.
You QS, Choy BKN, Chan JCH, Ng ALK, Shih KC, Cheung JJC, et al. Prevalence and Causes of Visual Impairment and Blindness among Adult Chinese in Hong Kong—The Hong Kong Eye Study. Ophthalmic Epidemiol. 2020;27:354–63.
Chan EW, Li X, Tham YC, Liao J, Wong TY, Aung T, et al. Glaucoma in Asia: regional prevalence variations and future projections. Br J Ophthalmol. 2016;100:78–85.
Wilson R, Walker AM, Dueker DK, Crick RP. Risk Factors for Rate of Progression of Glaucomatous Visual Field Loss. Arch Ophthalmol. 1982;100:737–41.
Jay JL, Murdoch JR. The rate of visual field loss in untreated primary open angle glaucoma. Br J Ophthalmol. 1993;77:176–8.
Buys YM, Jin YP. Canadian Glaucoma Risk Factor Study G. Socioeconomic status as a risk factor for late presentation of glaucoma in Canada. Can J Ophthalmol. 2013;48:83–7.
Peters D, Bengtsson B, Heijl A. Lifetime risk of blindness in open-angle glaucoma. Am J Ophthalmol. 2013;156:724–30.
Wong PW, Lau JK, Choy BN, Shih KC, Ng AL, Chan JC, et al. Epidemiological factors associated with health knowledge of three common eye diseases: A community-based pilot survey in Hong Kong. SAGE Open. Medicine. 2020;8:1–13.
Kong X, Yang Y, Gao J, Guan J, Liu Y, Wang R, et al. Overview of the health care system in Hong Kong and its referential significance to mainland China. J Chin Med Assoc. 2015;78:569–73.
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90.
Lee Y-H, Kim C-S. Hong S-p. Rate of Visual Field Progression in Primary Open-angle Glaucoma and Primary Angle-closure Glaucoma. Korean J Ophthalmol. 2004;18:106–15.
Yip JL, Nolan WP, Davaatseren U, Baasankhuu J, Lee PS, Khaw PT, et al. Primary angle closure glaucoma in East Asia: educational attainment as a protective factor. Ophthalmic Epidemiol. 2011;18:217–25.
Baskaran M, Foo RC, Cheng CY, Narayanaswamy AK, Zheng YF, Wu R, et al. The Prevalence and Types of Glaucoma in an Urban Chinese Population: The Singapore Chinese Eye Study. JAMA Ophthalmol. 2015;133:874–80.
Adekoya BJ, Shah SP, Onakoya AO, Ayanniyi AA. Glaucoma in southwest Nigeria: clinical presentation, family history and perceptions. Int Ophthalmol. 2014;34:1027–36.
Gogate P, Deshpande R, Chelerkar V, Deshpande S, Deshpande M. Is glaucoma blindness a disease of deprivation and ignorance? A case-control study for late presentation of glaucoma in India. Indian J Ophthalmol. 2011;59:29–35.
Fraser S, Bunce C, Wormald R, Brunner E. Deprivation and late presentation of glaucoma: case-control study. Br Med J. 2001;322:639–43.
Society THKO. Ophthalmologist Directory 2021.
Shiose Y, Kitazawa Y, Tsukahara S, Akamatsu T, Mizokami K, Futa R, et al. Epidemiology of glaucoma in Japan–a nationwide glaucoma survey. Jpn J Ophthalmol. 1991;35:133–55.
Seo SJ, Lee YH, Lee SY, Bae HW, Hong S, Seong GJ, et al. Estimated Prevalence of Glaucoma in South Korea Using the National Claims Database. J Ophthalmol. 2016;2016:1690256.
Garg A, Vickerstaff V, Nathwani N, Garway-Heath D, Konstantakopoulou E, Ambler G, et al. Primary Selective Laser Trabeculoplasty for Open-Angle Glaucoma and Ocular Hypertension: Clinical Outcomes, Predictors of Success, and Safety from the Laser in Glaucoma and Ocular Hypertension Trial. Ophthalmology. 2019;126:1238–48.
Gazzard G, Konstantakopoulou E, Garway-Heath D, Garg A, Vickerstaff V, Hunter R, et al. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicentre randomised controlled trial. Lancet. 2019;393:1505–16.
Noble S, McLennan D, Noble M, Plunkett E, Gutacker N, Silk M, et al. The English Indices of Deprivation 2019.
Statistics UIf. International Standard Classification of Education: ISCED 2011. 2012.
Office IL. International Standard Classification of Occupations: Structure, group definitions and correspondence tables.
Fraser S, Bunce C, Wormald R. Retrospective analysis of risk factors for late presentation of chronic glaucoma. Br J Ophthalmol. 1999;83:24–8.
Kyari F, Abdull MM, Wormald R, Evans JR, Nolan W, Murthy GV, et al. Risk factors for open-angle glaucoma in Nigeria: results from the Nigeria National Blindness and Visual Impairment Survey. BMC Ophthalmol. 2016;16:78.
Odayappan A, Kavitha S, Ramulu ST, Upadhyaya S, Venkatesh R. Assessment of Reasons for Presentation in New Primary Glaucoma Patients and Identification of Risk Factors for Late Presentation. Ophthalmic Glaucoma. 2020;S2589-4196:30318–5.
Sukumar S, Spencer F, Fenerty C, Harper R, Henson D. The influence of socioeconomic and clinical factors upon the presenting visual field status of patients with glaucoma. Eye. 2009;23:1038–44.
Boland MV, Ervin AM, Friedman DS, Jampel HD, Hawkins BS, Vollenweider D, et al. Comparative effectiveness of treatments for open-angle glaucoma: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;158:271–9.
Ting DSW, Cheung CY, Lim G, Tan GSW, Quang ND, Gan A, et al. Development and Validation of a Deep Learning System for Diabetic Retinopathy and Related Eye Diseases Using Retinal Images From Multiethnic Populations With Diabetes. JAMA. 2017;318:2211–23.
Hark LA, Myers JS, Ines A, Jiang A, Rahmatnejad K, Zhan T, et al. Philadelphia Telemedicine Glaucoma Detection and Follow-up Study: confirmation between eye screening and comprehensive eye examination diagnoses. Br J Ophthalmol. 2019;103:1820–6.
Acknowledgements
This project would not be possible without the help from the staff at ICEH, LSHTM and the Grantham Hospital.
Author information
Authors and Affiliations
Contributions
ACKL was responsible for the development of the methodology, data analysis method, and the drafting of the article under the supervision of JCC, JCB, and WN, JCC, JCB and WN advised on the development of the methodology, interpretation of the findings and drafting of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the London School of Hygiene and Tropical Medicine Ethics Committee and the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lai, A.C.K., Buchan, J.C., Chan, J.CH. et al. Determinants of late presentation of glaucoma in Hong Kong. Eye 37, 1717–1724 (2023). https://doi.org/10.1038/s41433-022-02235-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02235-8
- Springer Nature Limited