Abstract
Background
Dietary factors may play a role in bladder cancer etiology through modulation of inflammation. The purpose of this study was to examine the relationship between the inflammatory potential of diet, as estimated by the Dietary Inflammatory Index (DII®), and bladder cancer risk.
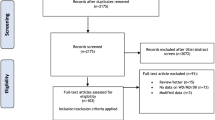
Methods
Energy-adjusted DII (E-DIITM) scores were computed among 101,721 participants in the Prostate, Lung, Colorectal, and Ovarian (PLCO) study. Hazard ratios (HRs) and 95% confidence intervals (CIs) were estimated using Cox regression analysis stratified by sex, with adjustment for smoking status and other confounding.
Results
Over a median of 12.5 years of follow-up, 776 bladder cancer cases were diagnosed. E-DII scores were not associated with bladder cancer risk in the multivariable models. The HRs (95% CIs) in the highest compared with the lowest E-DII quintile were 0.90 (0.70–1.17) and 1.22 (0.72–2.06) for men and women, respectively. The associations did not differ when DII score was set as a continuous variable. The HRs (95% CIs) of one-unit increment in the E-DII for bladder cancer risk were 0.99 (0.96–1.02) and 1.01 (0.94–1.10) for men and women, respectively.
Conclusions
Our study does not support an association between inflammatory potential of diet, as estimated by the E-DII, and bladder cancer risk.
Similar content being viewed by others
Introduction
Chronic inflammation is implicated in cancer and other chronic diseases [1] and diet can modulate inflammation [2, 3]. Numerous bioactive dietary components can interfere with selected inflammatory pathways to affect metabolic and genetic changes [2]. In addition, diet as a whole, is likely to be more important than individual foods or food constituents [4]. Therefore, the Dietary Inflammatory Index (DII®) was developed to capture the overall inflammatory potential of diet [5]. It provides a quantitative assessment of the inflammatory potential of diet and has been found to be associated with various health outcomes [6, 7].
Two case-control studies have used the DII to assess the association between dietary inflammatory potential and bladder cancer risk in Iranian [8] and Italian [9] populations, respectively. Both studies reported a significantly increased risk in the most pro-inflammatory diet group as indicated by higher DII scores. However, case-control studies are vulnerable to several types of bias, such as recall and selection biases, which may distort the true associations. By contrast, a prospective study performed in the Melbourne Collaborative Cohort Study (MCCS) reported a suggestive but not significant association between DII and the risk of urothelial cell carcinoma (HR Q5 vs. Q1: 1.24, 95% CI: 0.90–1.70) [10]. The objective of this study was to further assess the association between the inflammatory potential of diet, as estimated by the DII, and the risk of bladder cancer using data from the Prostate, Lung, Colorectal, and Ovarian (PLCO) cohort.
Materials and methods
Study population
The PLCO study is a population-based cancer screening trial that aimed to determine whether selected screening methods would reduce mortality from PLCO cancers [11]. Our study was based on 51,804 and 49,917 individuals in the intervention and control groups, respectively. The individuals completed a baseline questionnaire and a diet history questionnaire (DHQ) between 1998 and 2005 [12]. The PLCO Cancer Screening Trial was approved by the Institutional Review Board of the United States National Cancer Institute (NCI). Each participant signed an informed consent document for future additional studies as a supplement to the routine PLCO trial informed consent. The number of our approved PLCO project is PLCO-446.
Ascertainment of bladder cancer
Study participants were mailed a questionnaire annually to screen cancer cases. Cancer diagnoses were further ascertained through medical record abstraction. Vital status was obtained by the administration of the Annual Study Update questionnaires, reports from relatives, friends, or physicians, and National Death Index searches.
Dietary assessment
Diet was assessed by a self-reported food frequency questionnaire, the DHQ version 1.0 [13]. Participants reported the frequency of consumption and portion size of 124 food items and supplement use over the time period queried. Daily nutrient intake was calculated using the DietCalc software, which links responses of food frequency, portion size, and other relevant responses from the DHQ with a nutrient database based on national dietary intake data (USDA’s 1994–96 Continuing Survey of Food Intakes by Individuals [CSFII] and supplemented by the Nutrition Data Systems for Research from the University of Minnesota) [14].
Energy-adjusted DII score calculation
The energy-adjusted DII (E-DIITM) score was calculated based on the reported nutrient and food intake from the DHQ with linkage to the corresponding inflammatory effect scores designated in the DII. The DII is a literature-derived, population-based dietary index designed to estimate the overall inflammatory potential of an individual’s diet, which has been described elsewhere [5]. A higher DII score indicates a more pro-inflammatory diet, while a lower value represents a more anti-inflammatory diet.
Statistical analysis
A Cox proportional hazards regression model was used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs), according to gender. Models were adjusted for randomization arm, age, race, body mass index (BMI = weight(kg)/height(m)2), education, marital status, smoking status, and family history of any cancer. E-DII score was analyzed both as a categorical and a continuous variable. A possible nonlinear association between E-DII and bladder cancer was examined using a restricted cubic spline model [15]. In addition, we ran the models stratified by potential effect modifiers. We also performed lag analyses excluding participants diagnosed with bladder cancer within 2 years of questionnaire completion, and sensitivity analyses restricted E-DII scores from diet only were also performed. Likelihood-ratio tests were performed to test interactions. All statistical analyses were performed using the STATA software version 15 (Stata Corp, College Station, TX, USA). All tests were two-sided.
Results
This study included a total of 101,721 individuals and tracked 776 bladder cancer cases after a median of 12.5 years of follow-up. The E-DII was −2.8 ± 2.5 and −4.2 ± 2.1 for men and women, respectively (p < 0.001). Therefore, considering the substantial difference of E-DII distribution between men and women, we performed all analyses separately by sex in this study. The subject characteristics are presented in Table 1.
As can be seen from Table 2, in multivariable-adjusted analyses, E-DII, as a categorical variable, was not associated with bladder cancer risk. The HRs (95% CIs) in the highest compared with the lowest E-DII quintile were 0.90 (0.70–1.17) and 1.22 (0.72–2.06) for men and women, respectively. The direction and magnitude of the associations were similar when E-DII was fit as a continuous variable. The HRs (95% CIs) of one-unit increment in the E-DII for bladder cancer risk were 0.99 (0.96–1.02) and 1.01 (0.94–1.10) for men and women, respectively. As shown in Fig. 1, based on spline regression of bladder cancer risk in relation to E-DII, there was no statistical evidence for nonlinearity (men: p for nonlinearity = 0.799; women: p for nonlinearity = 0.688).
Solid lines represent point estimates and dashed lines represent 95% confidence intervals. Multivariable HRs were calculated by restricted cubic spline regression (using 3 knots at 10th, 50th, and 90th percentiles) adjusting for age (categorical), race (White, non-Hispanic vs. Other), body mass index at the time of enrollment (<25 kg/m2 vs. ≥25 kg/m2), education (≤high school vs. ≥some college), smoking status (never vs. former vs. current), randomization arm (intervention vs. control), family history of any cancer (yes vs. no), and marital status (married vs. not married). The histograms show the percentage of participants (left y axis) belonging to each level of E-DII.
There were no substantial associations in strata of the potential effect modifiers, and no evidence of interaction (Fig. 2). The null results from the sensitivity analyses for the diet only E-DII were consistent with that of the E-DII based on diet plus supplements (Table 3). Similar results were obtained with the exclusion of bladder cancer cases diagnosed within the first 2 years of follow-up (data not shown). For all analyses, no breach of the proportional hazard assumption was observed.
Discussion
In this large prospective PLCO cohort, we observed no statistically significant association between the inflammatory potential of diet, as estimated by E-DII, and bladder cancer risk. Similar results were obtained when excluding cases diagnosed within the first 2 years of follow-up and when calculating the E-DII based on diet only (i.e., excluding supplements). Also, the findings from subgroup analyses were consistent with the null results in main analyses.
Although existing evidence is largely consistent as to the harms of a more pro-inflammatory diet (a higher DII score), in terms of cardiovascular diseases [16], all-cause mortality [17] and various types of cancers [7, 18], there are disparate messages regarding the effect of DII on bladder cancer risk. In contrast to our findings, two previous hospital-based case-control studies reported significantly positive associations between DII scores and bladder cancer risk [8, 9]. Limitations of the case-control studies include the potential for selection bias, recall bias and reverse causation [19]. The only cohort study, performed in MCCS, recorded 379 incident urothelial cancer cases over a median follow-up period of 21.3 years. There was a suggestive but not significant association between DII and bladder cancer risk (highest vs. lowest quintile: HR 1.24, 95% CI 0.90–1.70) [10]. Compared with these previous studies, a positive association was not observed in the PLCO cohort.
Recently, Abufaraj et al. [20] assessed the association between the inflammatory potential of diet and bladder cancer risk in three prospective cohort studies using another dietary pattern, namely EDIP (Empirical Dietary Inflammatory Pattern) score. They included a total of 172,802 women and observed 1042 incident bladder cancer cases during 4,872,188 person-years of follow-up. Overall dietary patterns with pro-inflammatory potential, as reflected by high EDIP scores, were not associated with an increased risk of bladder cancer (Q5 vs. Q1 adjusted RR 0.92, 95% CI 0.75–1.12, p for trend = 0.67). These results were consistent with the findings of our study. Therefore, considering that diets associated with inflammation are not associated with the risk of bladder cancer, future studies are warranted to investigate other nutritional pathways with the potential for bladder cancer prevention.
Our study has several strengths including prospective cohort design, a comprehensive list of potential confounders, and the use of a validated DHQ, which covered major parameters that comprise the DII. However, as with any studies, some limitations should also be mentioned. First, diet intake was only assessed at baseline and it is possible that diet changed over time. Second, nutrient intake is often measured with error by commonly used dietary instruments. Nevertheless, the DHQ has been validated against 24-h dietary recalls among 1640 nationally representative participants in the Eating at America’s Table Study [12]. Still, it must be kept in mind that the E-DII scores in the PLCO are much lower than what we have seen in other studies. The entire distributions appear to be skewed toward values that are nearly 3 points lower, on average, than in other studies. For example, in the MCCS the median DII score in subjects with and without bladder cancer were −0.84 and −0.98, respectively. The corresponding values in the Italian study were +0.63 among cases and −0.93 among controls. The overall median in the Iranian study was −0.12. Third, the vast majority of subjects (over 90%) included in this study were non-Hispanic Whites, which may limit its generalizability to other populations. Finally, it is possible that the results may be biased by residual or unmeasured confounding even after adjusting for a number of factors. For example, we could not adjust for environmental and occupational exposures to chemicals, such as benzidine [21], which has been shown to be linked to bladder cancer risk.
In conclusion, we observed no significant association between the inflammatory potential of diet, as calculated by E-DII, and the risk of developing bladder cancer in PLCO cohort. Additional work in other contexts could help reconcile equivocal results across studies examining the relationship between E-DII/DII and bladder cancer.
References
Hunter P. The inflammation theory of disease. The growing realization that chronic inflammation is crucial in many diseases opens new avenues for treatment. EMBO Rep. 2012;13:968–70.
Ricordi C, Garcia-Contreras M, Farnetti S. Diet and inflammation: possible effects on immunity, chronic diseases, and life span. J Am Coll Nutr. 2015;34:10–3.
Kiecolt-Glaser JK. Stress, food, and inflammation: psychoneuroimmunology and nutrition at the cutting edge. Psychosom Med. 2010;72:365–9.
Jacobs DR, Jr., Gross MD, Tapsell LC. Food synergy: an operational concept for understanding nutrition. Am J Clin Nutr. 2009;89:1543S–8S.
Shivappa N, Steck SE, Hurley TG, Hussey JR, Hebert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014;17:1689–96.
Garcia-Arellano A, Martinez-Gonzalez MA, Ramallal R, Salas-Salvado J, Hebert JR, Corella D, et al. Dietary inflammatory index and all-cause mortality in large cohorts: the SUN and PREDIMED studies. Clin Nutr. 2018;38:1221–31.
Namazi N, Larijani B, Azadbakht L. Association between the dietary inflammatory index and the incidence of cancer: a systematic review and meta-analysis of prospective studies. Public Health. 2018;164:148–56.
Shivappa N, Hebert JR, Mirsafa F, Rashidkhani B. Increased inflammatory potential of diet is associated with increased risk of bladder cancer in an Iranian case-control study. Nutr Cancer. 2019;71:1086–93.
Shivappa N, Hebert JR, Rosato V, Rossi M, Libra M, Montella M, et al. Dietary inflammatory index and risk of bladder cancer in a large italian case-control study. Urology. 2017;100:84–9.
Dugue PA, Hodge AM, Brinkman MT, Bassett JK, Shivappa N, Hebert JR, et al. Association between selected dietary scores and the risk of urothelial cell carcinoma: a prospective cohort study. Int J Cancer. 2016;139:1251–60.
Prorok PC, Andriole GL, Bresalier RS, Buys SS, Chia D, Crawford ED, et al. Design of the prostate, lung, colorectal and ovarian (PLCO) cancer screening trial. Control Clin Trials. 2000;21:273S–309S.
Subar AF, Thompson FE, Kipnis V, Midthune D, Hurwitz P, McNutt S, et al. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: the Eating at America’s Table Study. Am J Epidemiol. 2001;154:1089–99.
National Cancer Institute. Diet history questionnaire. Risk factor monitoring and methods. Version current. 2016. http://www.riskfactor.cancer.gov/DHQ. Accessed 30 Nov 2016.
Cancer Data Access System. DQX dataset: data dictionary, appendix 2: nutrient. Washington (DC): US Department of Health and Human Services; 2013.
Marrie RA, Dawson NV, Garland A. Quantile regression and restricted cubic splines are useful for exploring relationships between continuous variables. J Clin Epidemiol. 2009;62:511–7 e1.
Shivappa N, Godos J, Hebert JR, Wirth MD, Piuri G, Speciani AF, et al. Dietary inflammatory index and cardiovascular risk and mortality-a meta-analysis. Nutrients. 2018;10:E200.
Garcia-Arellano A, Martinez-Gonzalez MA, Ramallal R, Salas-Salvado J, Hebert JR, Corella D, et al. Dietary inflammatory index and all-cause mortality in large cohorts: the SUN and PREDIMED studies. Clin Nutr. 2019;38:1221–31.
Fowler ME, Akinyemiju TF. Meta-analysis of the association between dietary inflammatory index (DII) and cancer outcomes. Int J Cancer. 2017;141:2215–27.
Melamed A, Robinson JN. Case-control studies can be useful but have many limitations: study design: case-control studies. BJOG. 2019;126:23.
Abufaraj M, Tabung FK, Shariat SF, Moschini M, Devore E, Papantoniou K, et al. Association between inflammatory potential of diet and bladder cancer risk: results of three United States prospective cohort studies. J Urol. 2019;202:484–9.
Zenser TV, Lakshmi VM, Davis BB. N-glucuronidation of benzidine and its metabolites. Role in bladder cancer. Drug Metab Dispos. 1998;26:856–9.
Acknowledgements
The authors thank the National Cancer Institute for access to NCI’s data collected by the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial. The statements contained herein are solely those of the authors and do not represent or imply concurrence or endorsement by NCI.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the work and approved the final version of the manuscript. Particularly, contributions were: study design: JL and XX; Data collection: XX; Data analyses and interpretation: XX, NS, JH; Manuscript drafting: JL and XX; Critical revision of the manuscript: XX, NS, JH.
Corresponding author
Ethics declarations
Conflict of interest
JRH owns controlling interest in Connecting Health Innovations LLC (CHI), a company that has licensed the right to his invention of the Dietary Inflammatory Index (DII®) from the University of South Carolina in order to develop computer and smart phone applications for patient counseling and dietary intervention in clinical settings. NS is an employee of CHI. This study received no external sponsorship from industry. In addition, the subject matter of this paper will not have any direct bearing on the work of CHI, nor has any CHI activity exerted any influence on this project. The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luo, J., Shivappa, N., Hébert, J.R. et al. Dietary inflammatory index and bladder cancer risk: a prospective study. Eur J Clin Nutr 74, 1428–1433 (2020). https://doi.org/10.1038/s41430-020-0602-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-0602-y
- Springer Nature Limited
This article is cited by
-
Dietary inflammatory index and prostate cancer risk: MCC-Spain study
Prostate Cancer and Prostatic Diseases (2022)