Abstract
Background/Objectives
Young Indian adults are at greater risk of overweight/obesity due to their high energy intake and sedentary lifestyle. Their energy requirement (ER) is based on their total energy expenditure (TEE) estimated from factorial method, which possibly overestimates their basal metabolic rate (BMR) and physical activity level (PAL). This study aimed to compare the accurately measured TEE with ER in young adults. Secondarily, to compare measured with predicted BMR and guideline PAL with that obtained from questionnaire and step counts.
Subjects/Methods
TEE was measured in 19 male adults (18–30 years), using the doubly labeled water technique, over 14 days. Indirect calorimetry was used to measure BMR, while the PAL was estimated by (a) the ratio of measured TEE and BMR, (b) step counts over 7 days measured using tri-axial accelerometers and (c) a physical activity questionnaire (PAQ).
Results
The measured TEE (9.11 ± 1.30 MJ/d) was significantly lower than the ER using either the Indian (15.2%) or the FAO/WHO/UNU (11.9%, both p < 0.01) recommendations. The measured BMR (6.90 ± 0.65 MJ/d) was significantly lower than that predicted using the FAO/WHO/UNU equation (6.5%, p < 0.01) but not for the Indian equation. The estimated PAL from measured TEE and BMR (1.35 ± 0.18), and from accelerometers (1.33 ± 0.11) was significantly lower than PAL obtained from PAQ (1.53 ± 0.17) or the guideline of 1.53 for Indians.
Conclusions
The predicted BMR and PAL guideline value was higher than that measured in young Indian adults, resulting in a ~13% lower measured TEE. This emphasizes the need to revisit the guidelines for predicting ER for this population.
Similar content being viewed by others
Introduction
There has been a rapid increase in the prevalence of overweight/obesity worldwide, which is a leading risk factor for non-communicable diseases. Even low-middle income countries (LMIC) like India are following this trend where overweight/obesity rates increased from 9.3 to 18.9% in men and 12.6 to 20.7% in women over last decade [1]. This is a concern when it occurs in young adults as they comprise 23.4 and 36.3% of world and Indian populations, respectively [2, 3], and can track into later life. Overweight/obesity is the result of positive energy balance due to too little daily energy expenditure from a sedentary lifestyle and too much daily energy intake, especially from high energy density processed foods containing large amounts of carbohydrates and fats [4,5,6,7,8]. The FAO/WHO/UNU (1985) suggested that the energy requirement (ER) should be based on the daily total energy expenditure (TEE) in weight stable individuals [9].
The best method to accurately measure the daily TEE is the doubly labeled water (DLW) technique [10], but the more practical and widely used method is the factorial approach, where the components of energy expenditure such as the basal metabolic rate (BMR), the thermic effect of food, and the energy expended in physical activity (measured from the physical activity level or PAL) are summed to arrive at the TEE [11]. Currently, the ER for Indians, recommended by the Indian Council of Medical Research (ICMR), is based on this factorial approach [12].
There are some limitations to this approach. First, the prediction of BMR using the FAO/WHO/UNU (2004) equation is likely to be incorrect [11], since this equation was derived from young muscular Europeans, which questions its applicability for other ethnicities with different body composition [13]. This may be particularly relevant in South Asians, including Indians, who have higher fat mass for a given body mass index (BMI) [14, 15], which could explain why the FAO/WHO/UNU (2004) equation overestimates the measured BMR in these populations by 9–12% [ref. 13, 16,17,18,19,20]. Second, the factorial method assumes a single value of PAL to define the energy expended in daily physical activity. The ICMR (2010) recommended a PAL of 1.53 for sedentary activity [12], while FAO/WHO/UNU (2004) provides a range of 1.40–1.69 rather than a single value [11]. The ICMR (2010) recommendation might be an overestimate, as there has been a decline in daily physical activity, even among the sedentary, in India over the last two decades [21, 22]. If either the BMR prediction equation overestimates or the assumed PAL value is too high, the resultant ER will be an overestimation, suggesting that the current recommendation is incorrect and could provide a basis for positive energy balance in this LMIC population.
Therefore, the present study primarily aimed to accurately measure the TEE of young adults and compare this with their factorially derived ER. As a secondary objective, the measured components of TEE (BMR and PAL) were compared with predictions based on body weight, questionnaires and step counts.
Materials and methods
Study participants
Young adult male participants aged between 18 and 30 years were recruited from student population of St. John’s Medical College, Bengaluru, India, having weight stability in last 3 months and BMI in the range of 18.5–29.9 kg/m2. A total of 19 participants were enrolled into the study; 10 normal weight and 9 overweight. Participants who reported consumption of any drug that increases energy expenditure, with history of smoking or antibiotics, those who had any medical illness and participated in any nutritional/clinical study within a month of enrollment were excluded. The habitual physical activity of the participants was assessed using a previously validated physical activity questionnaire (PAQ) based on recalls [23]. The study protocol was approved by Institutional Ethics Review Board of St. John’s Medical College (IEC study No.: 82/2019). The study was also registered at the Clinical Trials Registry India (CTRI/2020/07/026550). A written informed consent was obtained from all the participants.
Measurement of BMR
The standard procedure for measuring BMR was strictly followed, which included a post-absorptive state with 10–12 h of fasting, resting in supine position but awake with normal body temperature, ambient room temperature (25 °C) and without physical/psychological stress [13]. After screening, on a scheduled day, the recruited participants were asked to have an early dinner by 19:30 h and report to the Clinical Research Centre, Division of Nutrition at St. John’s Medical College, Bengaluru by 21:00 h. All participants retired to bed by 22:00 h on the night before the BMR measurement. The BMR measurements were carried out the following morning at 06:00 h using ventilated hood based indirect calorimetry. Participants were asked to rest for 30 min after waking up. After 30 min rest, a ventilated hood (flow rate ~40 L/min) was placed, which covered the subject’s head and chest. The air flowing into and out of the hood was sampled to measure its humidity, filtered and dried before being analyzed for its oxygen (O2) and carbon-dioxide (CO2) content (Servomex 1440, PM1158-O2, IR1520–5% CO2, Sussex, UK), to calculate amount of O2 consumed (VO2) and CO2 produced (VCO2) per minute. The gas analyzers were subjected to a 2-point calibration with a zero (99.9% nitrogen, Praxair, India) and span (21% O2 and 1% CO2, Praxair, India) gas, while the flowmeter used for measuring flow of air through the ventilated hood was calibrated with a dry-gas meter (50–6162, Harvard apparatus, United Kingdom). The error of measurement of the whole system, measured by burning ethyl alcohol within a specially designed hood, was <2% for both O2 and CO2 with a precision within 5%. Participants were instructed to keep their movements minimal and steady readings were recorded for 20 min. BMR (kcal/min) was calculated using Weir’s equation; Energy Expenditure (kcal/min) = (3.941* VO2 + 1.106*VCO2), which was extrapolated to 24 h to obtain the BMR (kcal/day or MJ/d) [24].
Anthropometric measurements
After the BMR measurement, body weight was measured in duplicate to 0.01 kg, on a calibrated digital weighing scale (Goldtech, AE038, New Delhi, India), with minimal clothing and empty bladder. Height was measured in duplicate to the nearest 0.1 cm using stadiometer (Seca 213, Hamburg, Germany).
Measurement of TEE
The TEE was measured using the DLW technique in a free-living condition over 14 days. The dose was prepared with 1.25 g/kg of 10% H218O (Sercon Ltd., UK) and 0.07 g/kg of 99.9% 2H2O (Sercon Ltd., UK) and stored in a refrigerator, one day prior to the administration. A baseline urine sample was collected from each subject to estimate background enrichment prior to dosing, following which the DLW dose was administered. The dose bottle was rinsed twice with 20–25 ml of water to ensure complete consumption of the dose. Post-dose urine samples were collected between 4–5 h after dosing and subsequently on 7th, 10th, and 14th day [10]. The timing of the urine collection was recorded accurately. In order to keep the body weight constant, the participants were asked to perform their habitual activities and refrain from consuming any food/ drug which could increase EE. The body weight of the participants was also measured at end of urine collection period. The urine samples were stored as 5 ml aliquots immediately at −20 °C, until further analysis by Isotope Ratio Mass Spectrometry (IRMS, Delta V Advantage, Thermo Fisher Scientific Inc., Bremen, Germany), for the enrichment of 18O and 2H. The precision of 18O and 2H measurements were within 0.08% and 1.0%, respectively. The isotope elimination rate constants at each point of measurement were used to calculate rate of CO2 production (rCO2) using Eq. (1) and a modified Weir’s Eq. (2) was then used to calculate TEE [10].
where, TBW is total body water, ko is 18O elimination rate and kd is 2H elimination rate constant
where, RQ is respiratory quotient; and a conversion factor of 0.004184 was used to convert TEE in kcal/d to MJ/d.
Body composition was also measured by the two-compartment model. The TBW was calculated from 2H dilution using plateau enrichment between 4th and 5th h post dose. To account for non-aqueous exchange, the 2H dilution space was converted to TBW by dividing it by 1.041 [25]. The derived TBW was then converted to fat-free mass (FFM), by assuming a hydration factor of 0.732 [26]. The fat mass (FM) was derived by subtracting FFM from body weight.
Assessment of physical activity using tri-axial accelerometer
The physical activity of the participants was assessed simultaneously during the DLW measurement using tri-axial accelerometers (GT3X+, ActiGraph LLC, Pensacola, FL, USA). The accelerometer was placed on the right side of waist and fixed using a stretchable belt. The participants were instructed to wear it throughout the day and night and recordings were made for 7 days. They were advised to remove it during bathing and wear it immediately after. At the end of the monitoring period, the participants were asked to return the accelerometer and these data were uploaded on using instrument software (ActiLife 6.2.1 from ActiGraph) for analysis. The data were expressed as 60-s epochs and when data were incomplete or showed an artifact (mostly on the first and last day while validating for wear time), these were excluded from the analysis. However, a minimum of 4 days readings were included to assess the physical activity. The PAL was calculated as the average of hourly metabolic equivalent (MET) over 24 h obtained from accelerometers.
Statistical analysis
A minimum sample size of 6 observations was calculated to observe an assumed difference in TEE of 2.092 MJ/d (500 kcal/d) with standard deviation of 1.255 MJ/d (300 kcal/d), between measured and predicted estimates from ICMR (2010) and FAO/WHO/UNU (2004) equations for young adults, with 80% power and 5% level of significance. The normality of the data was checked using Q-Q plot and Shapiro Wilk test (p > 0.05). The data are presented as mean and standard deviation (SD), unless specified. The ER was estimated using the predictive equations provided by ICMR (2010) and FAO/WHO/UNU (2004) [11, 12], which is an estimate of the TEE for an individual. In TEE estimation, an assumed PAL was used for sedentary activity; 1.53 for ICMR (2010) and 1.40 for FAO/WHO/UNU (2004) [11, 12]. A one-way analysis of variance (ANOVA) test was applied to compare the significant differences between measured TEE with the ER based on factorial approach. The other components of TEE, such as measured BMR and PAL were also compared to the predicted values. The predicted BMR was obtained using both ICMR (2010) and FAO/WHO/UNU (2004) equations [11, 12]. The PAL of each subject was calculated by dividing TEE (measured by the DLW method) with BMR (measured by indirect calorimetry). This calculated PAL was then compared to the PAL obtained from PAQ and accelerometers. A sub-analysis was carried out to compare the measured TEE, BMR, and PAL after stratifying the data into two groups based on BMI (normal and overweight group). To understand the impact of body composition on variability in BMR and TEE, a simple linear regression analysis was carried out. An intercorrelation of TEE, BMR and physical activity with body weight and FFM was assessed using Pearson’s correlation coefficient. All analyses were carried out on R (version 1.2.5033, 2009–2019) and significance level was set at p < 0.05.
Results
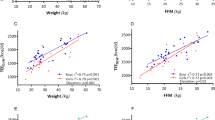
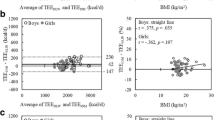
The participant’s age was 20.5 ± 2.2 years, with mean body weight and BMI of 71.2 ± 11.0 kg, and 24.0 ± 3.9 kg/m2, respectively (Table 1). The mean difference in body weight at the end of data collection was 0.02 ± 0.44 kg (p = 0.83). The habitual physical activity level as assessed by PAQ was 1.53 ± 0.17. The mean fat mass (%) was significantly lower in normal weight (18.5 ± 4.7%) group than overweight (24.5 ± 4.5%) group (p < 0.01). Overall, the measured TEE (9.11 ± 1.30 MJ/d) was significantly lower than the ER predicted using both ICMR (2010) (10.73 ± 1.02 MJ/d) and FAO/WHO/UNU (2004) (10.33 ± 0.97 MJ/d) equations (p < 0.0001) (Fig. 1a). On comparing between BMI categories, the measured TEE did not differ significantly between normal weight (8.83 ± 1.37 MJ/d) and overweight (9.56 ± 1.13 MJ/d) group (Table 2). The mean measured BMR (6.90 ± 0.65 MJ/d) was significantly lower than BMR predicted using FAO/WHO/UNU (2004) equation (7.38 ± 0.69 MJ/d, p < 0.01), but did not show significance with the ICMR (2010) equation (7.02 ± 0.67 MJ/d) (Fig. 1b). Between the BMI categories, the measured BMR was significantly higher in overweight (7.46 ± 0.59 MJ/d) group compared to normal weight (6.48 ± 0.36 MJ/d) group, but it was significantly lower in overweight (0.09 ± 0.01 MJ/kg/d) group, when expressed as per kg body weight (Table 2). The calculated PAL (1.35 ± 0.18), derived from measured TEE and measured BMR, and the PAL estimated from accelerometers (1.33 ± 0.11) were significantly lower than the PAL obtained from PAQ (1.53 ± 0.17). There was no significant difference between normal and overweight group. The linear regression analysis showed that 29% variability in TEE was attributed due to FFM (p = 0.03) while it was only 1% with FM (p = 0.7003). In case of BMR, 61% of variability seen due to FFM (p = 0.0003) and 23% due to FM (p = 0.059) (Table 3). A significant positive correlation was observed between the measured TEE (r = 0.537; p = 0.03) and FFM, while it was positive but non-significant with body weight (r = 0.429; p = 0.09). The TEE showed positive correlation with BMR (r = 0.503; p = 0.04) and PAL (r = 0.803; p < 0.01), but the relation was stronger with PAL. The measured BMR correlated positively with body weight (r = 0.778; p < 0.01) and FFM (r = 0.782; p < 0.01) but showed negative trend when BMR was expressed as per kg body weight (r = −0.808; p < 0.01). On other hand, the PAL did not show any correlation with increasing body weight (r = −0.026; p = 0.93) (Data not presented).
Comparison between measured and predicted TEE and BMR (a) measured TEE with predicted TEE using ICMR (2010) and FAO/WHO/UNU (2004) equations and (b) measured BMR with predicted BMR using ICMR (2010) and FAO/WHO/UNU (2004) equations. *Significant difference between measured and predicted values; Significance at p < 0.05. TEE (Predicted ICMR) kcal/d = [BMR − Predicted ICMR (14.5 * Body weight + 645) * 1.53]; The resultant is multiplied with 0.004184 to obtain value in MJ/d. TEE (Predicted WHO) MJ/d = BMR − Predicted WHO (0.063 * Body weight + 2.896) * 1.40. An assumed PAL of 1.53 and 1.40 was used for predicting TEE using ICMR (2010) and FAO/WHO/UNU (2004) equations, respectively, as suggested by the committees for sedentary activities. The predicted TEE is the energy requirement recommended by the respective committees. FAO/WHO/UNU: Food and Agriculture Organization/World Health Organization/United Nations University; ICMR: Indian Council of Medical Research.
Discussion
The present study accurately measured the TEE of young adults and compared it with the ER estimated using factorial approach based on BMR and PAL. The measured TEE using DLW was 9.1 (±1.3) MJ/d, which was 15.2% and 11.9% lower than the ER recommended by the ICMR (2010) and FAO/WHO/UNU (2004), respectively. The ER derived from the ICMR (2010) method had a higher difference from measured TEE due to the assumption of higher guideline PAL value of 1.53 for sedentary activity. If a PAL value of 1.40, the lower bound of the range provided by FAO/WHO/UNU (2004) for sedentary activity, is used for estimating ER based on ICMR (2010) equation, the difference between the measured TEE and ER was reduced to 7.7%. A strong positive correlation (r = 0.80) between measured TEE with PAL was observed in the study, suggesting that the low TEE could be due to low PAL. The remaining difference of 7.7% in measured TEE and ER can be attributed to a higher predicted BMR.
A comparison of the measured TEE of the present study with measurements made in similar age Indian participants about two decades ago showed that the TEE has declined [27,28,29]. Two studies that measured TEE using the DLW method in normal BMI south Indian adults aged 18–24 years reported a TEE of 9.4 (±2.0) MJ/d and 11.2 (±2.7) MJ/d, which is nearly 14% higher than TEE measured in normal BMI participants from the present study [27, 28]. In another study, the TEE was measured using the 13C labeled bicarbonate method in normal BMI Indian adults aged between 18–35 years and reported a higher TEE value of 10.3 (±1.7) MJ/d [29]. When young adults from present study were compared to population from other ethnicities, the measured TEE was higher in Caucasians (12.1 MJ/d) [30,31,32], while it was similar to other Asian populations (9.6 MJ/d) [33]. The differences observed in measured TEE between these ethnicities could be attributed to the differences in body composition and body size, as Indians have been reported to have a high body fat at lower BMI [14, 15, 34]. The results of the present study were also compared with a large database of DLW measured TEE, compiled from different studies with 547 measurements across all age groups [35]. The latter showed higher TEE and BMR estimates for adults aged 18–30 years when compared to the present study. In general, these comparisons are with measurements that were performed more than two decades ago; one of the important reasons for the lower TEE observed in the present study could be the decline in the level of physical activity across populations [22, 36], with young adults possibly being most vulnerable, with the economic and nutritional transitions, that they face as they shift from university life to office jobs [21, 36, 37]. For example, among the South Asian population, 47.4% of the Indian population were physically inactive in 2008, which increased to 54.4% in 2014 [38].
Since TEE was highly correlated with PAL, lowering the guideline PAL value recommended for estimating TEE will obviously provide closer estimates. However, there was also a small difference in measured TEE with ER even after lowering the PAL, which can be explained by the overestimation of BMR using the FAO/WHO/UNU (2004) equations. In the present study, predictive equations overestimated BMR by 6.5%. Prediction equations for BMR using FFM instead of body weight have shown to be more accurate. This is evident from a systematic review which provided the best fitting equation to predict BMR [39]. When FFM based equation was compared with the FAO/WHO/UNU (2004) equation, on a theoretical Asian male, aged 30 years, with an assumed body weight of 65 kg and 80% FFM, it was found that the FAO/WHO/UNU (2004) equation overestimated BMR by 12.9%. There is validity to this calculation; in a study on white Americans males (~34 years) with 75% FFM, the measured BMR was close to the FFM-predicted BMR, while FAO/WHO/UNU (2004) equation overestimated BMR by 15.7% [ref. 40]. Similarly, the BMR predicted using the FFM based equation [39] was closer to the measured BMR (6.7 vs 6.9 MJ/d) in the present study.
The accurate estimation of the TEE and ER is vital, as even a small overestimation of 0.4 MJ/d (~100 kcal/d) in ER, can lead to weight gain of about 4 kg over a year, crudely assuming all the additional weight is fat. In the present study, the prediction equations overestimated TEE by 1.4 MJ/d (341 kcal/d) which is equivalent to an allowance of an additional heavy snack or half a major meal. In broad terms, the resultant positive energy balance could lead to a weight gain of about 1 kg in a month, unless physical activity is increased. At a public health level, dietary recommendations are usually anchored to the ER of the population and if unnecessarily high, will have proportional impact across most nutrients.
A limitation was that the participants in this study were restricted to a small sample of male young adults, due to financial and logistic constraints. While new prediction equations cannot be derived from the present study, these data can contribute to collated large databases for TEE [41]. The study location limited the measurements to an urban population and generalizing the findings to the young adults from rural areas would be inappropriate. The strength of the study lies in accurate measurement of TEE and its components using gold standard techniques among young adults. In conclusion, the present study accurately measured the daily TEE over 14 days, using the best method available, and observed it to be lower than the current ER recommended by the expert national or international guidelines. This emphasizes the need to revisit the estimation of the ER for adults, particularly those leading a sedentary lifestyle, and flaws in the factorial approach need to be addressed accordingly.
References
International Institute of Population Science. National Family Health Survey India 2015–2016: India fact sheet. Mumbai: Ministry of Health and Family Welfare. Government of India; 2016. http://rchiips.org/NFHS/pdf/NFHS4/India.pdf. Accessed 4 May 2020.
World Bank. World Development Indicators: Data Bank. https://databank.worldbank.org/reports.aspx?source=2&series=SP.POP.2529.MA.5Y&country=#. Accessed 4 May 2020.
Office of Registrar General & Census Commissioner. Census of India: Age structure and marital status. Ministry of Home Affairs, Government of India, 2011. https://censusindia.gov.in/Census_And_You/age_structure_and_marital_status.aspx. Accessed 4 May 2020.
Tripathy JP, Thakur JS, Jeet G, Chawla S, Jain S, Prasad R. Urban rural differences in diet, physical activity and obesity in India: are we witnessing the great Indian equalisation? Results from a cross-sectional STEPS survey. BMC Public Health. 2016;16:1–10.
Arora S, Nanda K. What’s cooking with Indian Diners: understanding eating-out patterns among Indian consumers. Nielsen Featured Insights, India, 2017.
KPMG. India’s food service industry: growth recipe. Federation of Indian Chambers of Commerce and Industry (FICCI), 2016. https://assets.kpmg/content/dam/kpmg/in/pdf/2016/11/Indias-food-service.pdf. Accessed 6 May 2020.
Roberts SB, Das SK, Suen VMM, Pihlajamäki J, Kuriyan R, Steiner-Asiedu M, et al. Measured energy content of frequently purchased restaurant meals: multi-country cross sectional study. BMJ. 2018;363:1–10.
Cuthbertson DJ, Steele T, Wilding JP, Halford JC, Harrold JA, Hamer M, et al. What have human experimental overfeeding studies taught us about adipose tissue expansion and susceptibility to obesity and metabolic complications? Int J Obes. 2017;41:853–65.
FAO/WHO/UNU. Energy and protein requirements. Report of a joint FAO/WHO/UNU Expert Consultation Technical Report Series 724. FAO/WHO/UNU; Vol. 27, Geneva, 1985.
Bluck L, Forsum L, Hills A, Kurpad A, Mokhtar N, Preston T, et al. editors. Assessment of body composition and total energy expenditure in humans using stable isotope technique. IAEA Human Health Series No. 3. Vienna: IAEA; 2009.
FAO/WHO/UNU. Human energy requirements. Report of a Joint FAO/WHO/UNU Expert Consultation. FAO/WHO/UNU; Rome, 2004.
Indian Council of Medical Research. Nutrient requirements and recommended dietary allowances for Indians. A report of the expert group of the Indian Council of Medical Research National Institute of Nutrition Hyderabad. Indian Council of Medical Research; Hyderabad, 2010.
Henry C. Basal metabolic rate studies in humans: measurement and development of new equations. Public Health Nutr. 2005;8:1133–52.
Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002;3:141–6.
Hood K, Ashcraft J, Watts K, Hong S, Choi W, Heymsfield SB, et al. Allometric scaling of weight to height and resulting body mass index thresholds in two Asian populations. Nutr Diabetes. 2019;9:1–7.
Miyake RM, Tanaka ST, Ohkawara K. Validity of predictive equations for basal metabolic rate in Japanese adults. J Nutr Sci Vitaminol. 2011;57:224–32.
Razalee S, Poh BK, Ismail MN. Predictive equation for estimating the basal metabolic rate of Malaysian Armed Forces naval trainees. Singap Med J. 2010;51:635–40.
Shetty PS, Soares MJ, Sheela ML. Basal metabolic rate of South Indian males. FAO Report. Bangalore, India, 1986.
Soares M, Shetty P. Validity of Schofield’s predictive equations for basal metabolic rates of Indians. Indian J Med Res. 1988;88:253–60.
Soares MJ, Francis DG, Shetty PS. Predictive equations for basal metabolic rates of Indian males. Eur J Clin Nutr. 1993;47:389–94.
Anjana RM, Pradeepa R, Das AK, Deepa M, Bhansali A, Joshi SR, et al. Physical activity and inactivity patterns in India – results from the ICMR-INDIAB study. Int J Behav Nutr Phys Act. 2014;11:1–11.
Althoff T, Sosič R, Hicks JL, King AC, Delp SL, Leskovec J. Large-scale physical activity data reveal worldwide activity inequality. Nature. 2017;547:336–9.
Bharthi A, Sandhya N, Vaz M. The development and characteristics of a physical activity questionnaire for epidemiological studies in urban middle class Indians. Indian J Med Res. 2000;111:95–102.
Weir JBD. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109:1–9.
Racette SB, Schoeller DA, Luke AH, Shay K, Hnilicka J, Kushner RF. Relative dilution spaces of 2H- and 18O-labeled water in humans. Am J Physiol - Endocrinol Metab. 1994;267:30–34.
Scholeller D Hydrometry. In: Roche A, Heymsfield S, Lohman T editors. Human body composition. 1st ed. Champaign, IL: Human Kinetics; 1996. pp. 25–43.
Kurpad A, Borgonha S, Shetty P. Measurement of total energy expenditure by the doubly labelled water technique in free living Indians in Bangalore city. Indian J Med Res. 1997;105:212–9.
Borgonha S, Shetty PS, Kurpad AV. Total energy expenditure & physical activity level in chronically energy deficient Indian males measured by the doubly labelled water technique. Indian J Med Res. 2000;111:138–46.
Raj T, D’Souza G, Elia M, Kurpad AV. Measurement of 24 h energy expenditure in male tuberculosis patients. Indian J Med Res. 2006;124:665–76.
Tudor-Locke C, Martin CK, Brashear MM, Rood JC, Katzmarzyk PT, Johnson WD. Predicting doubly labeled water energy expenditure from ambulatory activity. Appl Physiol Nutr Metab. 2012;37:1091–100.
Whybrow S, Hughes DA, Ritz P, Johnstone AM, Horgan GW, King N, et al. The effect of an incremental increase in exercise on appetite, eating behaviour and energy balance in lean men and women feeding. Br J Nutr. 2008;100:1109–15.
Willis EA, Herrmann S, Homas J, Lee J, Donnelly J, Washburn R. Nonexercise energy expenditure and physical activity in the Midwest Exercise Trial. Med Sci Sport Exerc. 2014;46:2286–94.
Sasai H, Nakata Y, Murakami H, Kawakami R, Nakae S, Tanaka S, et al. Simultaneous validation of seven physical activity questionnaires used in japanese cohorts for estimating energy expenditure: a doubly labeled water study. J Epidemiol. 2018;28:437–42.
Yajnik CS, Yudkin JS. The YY paradox. Lancet. 2004;363:163.
Black A, Coward W, Cole T, Prentice A. Human energy expenditure in affluent societies: an analysis of 574 doubly-labelled water measurements. Eur J Clin Nutr. 1996;50:72–92.
Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Heal. 2018;6:e1077–e1086.
Swaminathan S, Sinha S, Minocha S, Makkar S, Kurpad AV. Are we eating too much? A critical reappraisal of the energy requirement in Indians. Proc Indian Natl Sci Acad USA. 2018;84:809–19.
Ranasinghe C, Ranasinghe P, Jayawardena R, Misra A. Physical activity patterns among South-Asian adults: a systematic review. Int J Behav Nutr Phys Act. 2013;10:1–11.
Sabounchi NS, Rahmandad H, Ammerman A. Best-fitting prediction equations for basal metabolic rate: informing obesity interventions in diverse populations. Int J Obes. 2013;37:1364–70.
Sharp TA, Bell ML, Grunwald GK, Schmitz KH, Sidney S, Lewis CE, et al. Differences in resting metabolic rate between White and African-American young adults. Obes Res. 2002;10:726–32.
Speakman JR, Pontzer H, Rood J, Sagayama H, Schoeller DA, Westerterp KR, et al. The International Atomic Energy Agency international doubly labelled water database: aims, scope and procedures. Ann Nutr Metab. 2019;75:114–8.
Acknowledgements
The guidance of Dr. S Devi in interpreting the DLW data for estimating TEE and body composition is acknowledged. The authors would also like to acknowledge the voluntary participation of the participants in the study, the technicians and the lab personnel in sample processing and analysis.
Funding
This research study had received funding from Indian Council of Medical Research (ICMR) in the year 2019 (Grant sanction order 5/9/1200/2019-Nut to RK and AVK).
Author information
Authors and Affiliations
Contributions
AVK and RK conceptualized the study. SS was involved in participant screening, data collection and data cleaning. SS, AVK, and RK were involved in statistical analysis of the data. The draft manuscript was prepared by SS and RK while the final approval was provided by AVK. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sinha, S., Kurpad, A.V. & Kuriyan, R. Total energy expenditure (TEE) of young adults from urban South India: revisiting their daily energy requirement. Eur J Clin Nutr 75, 845–851 (2021). https://doi.org/10.1038/s41430-020-00790-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00790-5
- Springer Nature Limited