Abstract
Background/objectives
We previously demonstrated that fruit and vegetable consumption, was associated with less weight gain over 6 years in young women for all body mass index (BMI) categories. This study evaluated the relationship between diet quality and 6-year weight change, in Australian women initially in the healthy weight range (≥18.5 BMI <25 kg/m2) at baseline.
Subjects/methods
A total of 4083 young women (27–31 years) in the healthy weight range (≥18.5 BMI <25 kg/m2) enroled in the Australian Longitudinal study on Women’s Health (ALSWH) were analysed. Diet quality was measured by the Australian Recommended Food Score (ARFS) and the Fruit and Vegetable Index (FAVI) using dietary data derived from a validated food frequency questionnaire. Weight change was calculated as the difference between baseline and 6-year follow-up weight (kg). Multiple linear regression models were used to analyse the association between baseline ARFS and FAVI and 6-year weight change.
Results
At baseline, mean diet quality was low for both indices [ARFS (maximum 72) = 29.9 and FAVI (maximum 333) = 94.2] and women gained 3.7 kg of weight during 6 years of follow-up. Regression modelling revealed that every one point increase over 6 years in either the ARFS or FAVI score was associated with statistically significantly less weight gain over 6 years, although the amount was small (33 and 12 g, respectively).
Conclusions
Higher diet quality predicts lower prospective weight gain in young women however, further research is needed over a longer follow-up period and in diverse population groups.
Similar content being viewed by others
Introduction
Worldwide, non-communicable diseases are the leading cause of morbidity and mortality, contributing to 73% of all-cause mortality and 62% of disability adjusted-life years [1]. Overweight and obesity are major risk factors contributing to the development of non-communicable diseases [2]. In 2016, the World Health Organization (WHO) estimated that in adults (≥18 years), 39% were overweight (39% men, 40% women), and 13% were obese (11% men, 15% women) [3]. In the 2017–2018 Australian National Health Survey, prevalence of overweight and obesity in young adults increased by 12% between the age groups of 18–24 years and 25–34 years, which is the largest increase in prevalence between consecutive age groups [4].
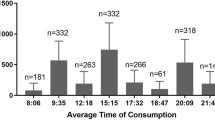
Young adults have poorer diet quality compared with older age groups [5, 6]. Lifestyle changes (e.g. moving away from home) during young adulthood may contribute to unhealthy eating habits including skipping breakfast [7] and frequent consumption of fast food [8, 9] and meals outside the home [8]. These eating habits in young adults can contribute to greater consumption of energy-dense, nutrient-poor foods and increase the risk of overweight and obesity [10, 11]. Evidence has shown that Australian women are gaining weight at a faster rate compared with their parents, with the prevalence of overweight and obesity significantly increasing in cohorts born after 1960 [6]. Furthermore, young women are at higher risk of weight gain compared with all other age groups [5, 6, 12, 13]. The 2017–2018 Australian National Health Survey, reported that the prevalence of overweight and obesity in women increased from 40% amongst those aged 18–24 years to 49% for those aged 25–34 years [4]. Research from the Australian Longitudinal Study of Women’s Health (ALSWH) found that young women gained weight at a faster rate compared with the previous generation of Australian women [13].
While the causes of overweight and obesity are multi-factorial and complex, diet is a leading modifiable risk factor [14]. Studies have reported that food habits, dietary patterns, diet quality, and total food intake predict future weight gain in adults [15]. Our systematic review highlighted that only a limited number of studies have examined the relationship between diet quality and prospective weight change [16, 17]. We previously examined the association between two diet quality indices, the Australian Recommended Food Score (ARFS) and the Fruit and Vegetable Index (FAVI), and weight gain during 6 years of follow-up in a sample of young women (n = 3945) from the ALSWH. Overall, women with the highest FAVI scores [mean (SD): 117.2 (18.9) out of a maximum total of 333 points] gained less weight had by 72 g (p = 0.04) compared with those with the lowest FAVI scores [mean (SD) 34.6 (28.0) points]. We found that higher ARFS scores were associated with less weight gain, only amongst those in the sub-sample reporting plausible total energy intakes (TEIs) (n = 1356) (p > 0.05) [18]. However, this analysis included women of all BMI categories and health status groups. Understanding the role of diet quality in maintaining a healthy body weight in women of child-bearing age is essential for developing effective dietary interventions for weight gain prevention in a high-risk population [13, 19]. Therefore, the aim of the current analysis was to examine the association between diet quality, measured by ARFS and FAVI indices, with prospective 6-year weight change in young women initially in the healthy weight range.
Subjects and methods
Participants
The current study analysed data from young women (aged 27–31 years) participating in the ALSWH cohort study at two timepoints, 2003 and 2009. Further details are reported elsewhere [20, 21]. Participants were excluded at baseline if they reported having a diagnosis of type 2 diabetes, heart disease or any type of cancer (excluding skin cancer), were currently pregnant, or were not in a healthy weight range (18.5 ≤ BMI < 25 kg/m2). Figure 1 summarises the participant selection criteria for the current analysis. The study was approved by the University of Newcastle and the University of Queensland Human Research Ethics committees. All participants gave written informed consent prior to their inclusion in the study.
Anthropometry
Weight [kilograms (kg)] and height [metres (m)] were self-reported at baseline and follow-up. Weight change (∆) was defined as the absolute difference (kg) in weight between baseline and follow-up. BMI was calculated at each timepoint by dividing body weight (kg) by height (m2). Women were classified according to the World Health Organization (WHO) criteria as: underweight, BMI < 18.5; healthy weight, 18.5 ≤ BMI < 25; overweight, 25 ≤ BMI < 30; or obese, 30 ≤ BMI.
Confounders
Participants self-reported their baseline walking and moderate and strenuous physical activity (PA) frequency, which was used to derive a PA score in metabolic equivalents per minute (MET. Mins) [22]. Education level was self-reported as: ‘no formal’ or ‘nil’, ‘school certificate’, ‘trade/apprenticeship’, ‘university degree’ or ‘higher degree’. The participants location of residence were categorised using the Australian Bureau of Statistics definitions: urban (with 100,000 or more people), rural (with 200–999 people) and remote (<200 people). Participants self-reported their smoking status as: ‘current smoker’, ‘never smoked’, or ‘ex-smoker’. Marital status was defined as: ‘married’, ‘defacto’, ‘separated’, ‘divorced’, ‘widowed’, or ‘single’.
Dietary intake assessment and diet quality indices
Dietary intake was self-reported using the Dietary Questionnaire for Epidemiological Studies Version 2 (DQESv2) food frequency questionnaire (FFQ) which assesses the consumption of 74 food items over the previous 12 months [23]. The DQESv2 has been previously validated in young women in ALSWH [24]. Participants reported their usual consumption of each food item using a 10-point Likert scale, ranging from ‘never’ up to ‘three or more times per day’. Photographs were used to represent different serving sizes for vegetables, potatoes, and meat casserole dishes, enabling a portion factor to be calculated that accounted for serving size variability. Nutrient intakes were quantified using the Australian nutrient composition database and the Nutrient Data Table (NUTTAB) [25] and software developed by the Cancer Council of Victoria.
The Australian Recommended Food Score (ARFS)
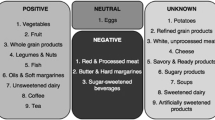
The ARFS was adapted from the USA Recommended Food Score (RFS) [26] and has been previously validated in Australian women [27, 28]. Points in the ARFS are awarded based on regular consumption of FFQ items that align with recommendations in the National Dietary Guidelines [27, 29]. The ARFS contains a total of 74 items that are categorised into seven sub-scales for specific food groups (based on the Australian Guide to Healthy Eating food groups [29]), with scores ranging from zero to 74 points. The sub-scale scores are calculated by awarding one point for each food item reported to be consumed at least once a week. The total score within each sub-scale for the following food groups are: 22 points for vegetables (including cooked potato without fat); 14 points for fruit; 14 points for protein foods; 14 points for grains; seven points for dairy; 1 point for fats and 2 points for alcoholic beverages. Zero points are awarded when alcohol is not consumed due to the U-shaped association between alcohol intake and health status [27]. The maximum ARFS score is 74, reflecting the highest diet quality score and the most optimal score for meeting nutrient requirements [27].
The Fruit and Vegetable Index (FAVI)
The baseline DQESv2 fruit and vegetable consumption data [22], were used to inform the development of the FAVI score [18]. The FAVI was divided into two sub-scales: fruit including fresh fruit, canned or frozen fruit and fruit juices (24 items), and vegetables including cooked potatoes with fat (24 items). The frequency of consumption for all fruit and vegetable items were scored using the 10-point Likert scale from ‘never’, scored as zero, up to ‘≥3 times per day’ scored as nine points. The maximum possible score was 117 points for the fruit sub-scale and 216 points for the vegetable sub-scale, giving a maximum total FAVI score of 333 points. A higher FAVI score indicates a more frequent and wide variety of fruits and vegetables usually consumed [18].
Statistical analysis
Descriptive data were presented as means and standard deviations. Social-demographic variables were reported across tertiles of diet quality indices. P values from analysis of variance (ANOVA) and chi-square tests were reported to compare between co-variables across tertiles of diet quality indices. Multiple linear regressions were used to evaluate 6-year weight change, to test the relationship between each diet quality and longitudinal weight change. Three regression models were applied: (1) a crude model (unadjusted), where the dependent variable was weight change, and the independent variables were baseline diet quality index of interest; (2) a specifically adjusted model, where model 1 was adjusted for PA, education, number of births, area of residence, marital status, smoking, and weight at baseline; and (3) a fully adjusted model, where the same variables were used as in model 2, but with the addition of TEI. All statistical analyses were carried out using STATA 11 (College Station, TX: StataCorp LP 2011). Weight change was checked and shown to follow a normal distribution. Statistical analyses were considered statistically significant if p < 0.05.
Results
In the study cohort (n = 9081) at baseline, 4083 young women in the healthy weight range met the inclusion criteria and provided data at baseline and follow-up. While 4983 young women were excluded as their BMI was classified as underweight (n = 298), overweight (n = 1343) or obesity (n = 935). Figure 1 shows the flow of participants through the study. There were no significant differences in diet quality scores (ARFS and FAVI) or confounders (level of PA, smoking status, and level of education), between those with or without missing data for weight change, p > 0.05 (data not shown). Participant characteristics at baseline and follow-up are summarised in Table 1. On average, women were aged 27.6 ± 1.5 years and gained 3.5 ± 6.7 kg over 6 years of follow-up. Baseline diet quality scores were relatively low: ARFS 28.3 ± 9.2 (maximum 74) and FAVI 73.1 ± 44.2 (maximum 333), with a total daily energy intake of 6848.5 ± 2620.9 kJ.
When women were categorised into ARFS tertiles, there were significant differences in weight change, energy intake (baseline), level of education (baseline), level of PA (baseline and follow-up), smoking status (baseline and follow-up), and location of residence (baseline and follow-up) (p < 0.05). Weight change was [+4.1 (6.8) kg], [+3.6 (6.5) kg], and [+3.7 (6.7) kg] for women in the lowest (the worst diet quality scores), middle and highest ARFS tertiles, p = 0.04 (Table 2).
When women were categorised into FAVI tertiles, there were significant differences in weight change, energy intake (baseline), level of education (baseline), BMI (baseline and follow-up), level of PA (baseline and follow-up), smoking status (baseline and follow-up), and location of residence (baseline and follow-up) (p < 0.05). Weight change was [+4.9 (7.3) kg], [+3.8 (6.3) kg], and [+3.5 (6.7) kg] for women in the lowest (the worst diet quality scores), middle, and highest FAVI tertiles, p = 0.00 (Table 3).
Table 4 reports the multivariate linear regression analyses between ARFS and FAVI and weight change over 6 years. ARFS was significantly associated with less weight gain in the crude and fully adjusted models, while the FAVI was significantly associated with less weight gain in all the three models. In the fully adjusted model, for every one point increase in the ARFS and FAVI, weight gain over 6 years reduced by 33 and 12 g, respectively.
Discussion
The current analysis indicates that those in the highest ARFS tertile (highest diet quality scores) gained significantly less weight compared with women in the lowest ARFS tertile (3.7 ± 6.7 kg compared with 4.1 ± 6.8 kg). Although this association was statistically significant, the difference in mean weight gain was very small (0.4 kg) so the results of this study should be interpreted with caution. These findings are consistent with previously reported results highlighting that ALSWH young women, across all BMI categories (n = 4287) with the highest ARFS scores gained 1.1 kg less weight over 6 years of follow-up compared with women with the lowest ARFS scores [18]. However, in the current analysis the full impact of high diet quality scores (i.e. a score of ≥45) on weight may not be captured, as the mean ARFS was 28 out of a maximum score of 74, indicating that poor diet quality was common. However, a cross-sectional study of Australian adults (n = 7441) within the Australian Diabetes, Obesity, and Lifestyle study, indicated that even small improvements in dietary quality can be beneficial for cardiometabolic risk factors, including abdominal obesity [30].
Analysis of Australian women (n = 1242) aged 36.9(7.5) years within the Resilience for Eating and Activity Despite Inequality (READI) cohort study indicated that each unit increase in diet quality, measured by the Australian Dietary Guideline Index (DGI), resulted in a decrease in BMI by 0.014 kg/m2 over 5 years of follow-up [31]. Furthermore, greater change in BMI was found in women with a lower diet quality score at baseline compared with those with a higher diet quality score (p < 0.10) [31]. The US Nurses’ Health Study II (NHS II) cohort of women aged 25–42 years (n = 116,671) found that for each one standard deviation increase in diet quality score, using the Alternate Health Eating Index-2010 (AHEI-2010), −0.66 kg less weight was gained (95% CI: −0.68, −0.64) over 4 years of follow-up [32]. The US Framingham Offspring and Spouse cohort study found that women (n = 590) initially of a healthy weight (BMI < 25 kg/m2), aged 25–71 years with poorer diet quality, measured by the Framingham Nutritional Risk Score (FNRS) were more likely to develop overweight or obesity (OR 1.76; 95% CI 1.16, 2.69) compared with those with higher diet quality [33]. In the current study, women in the lowest ARFS tertile reported lower TEIs compared with those in the highest ARFS tertile (6274.0 ± 2535.5 kJ compared with 7412.6 ± 2731.0 kJ). Even factoring in likely mis-reporting of TEI, this finding suggests that higher energy intakes and higher dietary quality scores did not exacerbate weight gain over time. Results from the Framingham Offspring and Spouse cohort are also in agreement with these findings [33]. This highlights the complexity of the diet–obesity relationship and more specifically, the difficulties of estimating TEI. Further analysis of dietary patterns rather than an over emphasis on total energy and nutrient intakes is warranted.
In the current study, women who had higher FAVI scores also gained significantly less weight, compared with those who had lower scores at baseline (3.5 ± 6.7 kg compared with 4.9 ± 7.3 kg, p = 0.00) however, the difference in mean weight gain was small (1.4 kg) however, the difference in mean weight gain was small (1.4 kg), so results should be interpreted with caution. This is consistent with our previous study [18] in women of all BMI categories which found that higher FAVI scores were associated with less weight gain by 1.6 kg over 6 years follow-up. A systematic review and meta-analysis of 17 cohort studies (n = 563,277 adults) reported that every 100 g increase in fruit consumption was associated with weight loss of 13.7 g per year (95% CI, −22.97 to −4.40) [34]. No significant association was found between vegetable consumption and weight change in adults [34]. However, greater consumption of all vegetables and fruit, both together and separately were associated with a 9–17% reduced risk of overweight, abdominal obesity, and weight gain [34]. The authors of this study advised that the overall quality of the evidence was low and results should be interpreted with caution. Bertoia et al., [35] conducted a combined analysis of three large prospective cohort studies, including US adults (n = 133,468) aged 25–75 years, and found that a higher consumption of vegetables and fruit was associated with weight change −0.25 lb (95% CI: −0.35 to −0.14 lb) and −0.53 lb (95% CI: −0.61 to −0.44 lb) over 4 years. More specifically, the results indicated that a higher consumption of starchy vegetables including baked, boiled, or mashed potatoes (0.74 lb; 95% CI 0.19–1.30 lb) or corn (2.04 lb; 95% CI: 0.94–3.15 lb) were independently associated with weight gain [35]. These findings highlight the importance of analysing sub-groups such as starchy vegetables, as the impact on weight management may vary compared with the overall vegetable food group.
Limitations of the current study need to be acknowledged. Firstly, when comparing participants with the highest diet quality scores versus those with the lowest diet quality scores the difference in weight change was small despite the relationship being statistically significant. However, the use of self-reported dietary data may have obscured the magnitude of this relationship, as previous findings from the ALSWH cohort indicated that women under-reported their weight by 0.95 kg (95% CI: 0.44–1.47 kg) therefore, results should be interpreted with caution [36]. Body weight were self-reported and thus the potential for recall bias cannot be excluded however, a validation study concluded the level of agreement between self-reported and objectively measured weight and height was acceptable [36]. Another limitation was the use of self-reported FFQ data, which is associated with mis-reporting, particularly as body weight increases [37]. Although the DQESv2 has been validated in women of child-bearing age [24], it does not include a wide range of energy-dense, nutrient-poor foods and therefore may not be a true representation of dietary patterns, particularly for those with the poorest diet quality.
Strengths of this study are the use of two diet quality indices. The ARFS was based on variety and frequency of healthful food items that align with recommendations in the Australian Dietary Guidelines, while the FAVI index considered only fruit and vegetable variety and frequency. In addition, the current study used data from a sub-sample of healthy weight women from a national dataset (ALSWH), followed-up over 6 years.
In conclusion, women in the healthy weight range from the young ALSWH cohort gained weight over 6 years of follow-up. However, those with higher diet quality scores gained slightly less weight, suggesting that consuming a diet that aligns more closely with recommendations in the national dietary guidelines, including consumption of plenty of vegetables and fruit, may help to slow the rate of weight gain. However, this alone is not likely to prevent the risk of weight gain at this life stage. Further research is needed over a longer follow-up period, and in other populations to further examine the relationship between diet quality and weight change.
References
Kyu HH, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1859–922.
Stanaway JD, Afshin A, Gakidou E, Lim SS, Abate D, Abate KH, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–94.
World Health Organization (WHO). Overweight and obesity: key facts. Geneva, Switzerland World Health Organization (WHO); 2018.
Australian Bureau of Statistics (ABS). Australian Health Survey. National Health Survey: first results. Key Findings 2017–2018. Canberra, Australia Australian Bureau of Statistics (ABS); 2018.
Hiza HA, Casavale KO, Guenther PM, Davis CA. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J Acad Nutr Diet. 2013;113:297–306.
Allman-Farinelli MA, Chey T, Bauman AE, Gill T, James WPT. Age, period and birth cohort effects on prevalence of overweight and obesity in Australian adults from 1990 to 2000. Eur J Clin Nutr. 2007;62:898.
Pendergast FJ, Livingstone KM, Worsley A, McNaughton SA. Examining the correlates of meal skipping in Australian young adults. Nutr J. 2019;18:24.
Pereira MA, Kartashov AI, Ebbeling CB, Van Horn L, Slattery ML, Jacobs DR Jr., et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365:36–42.
Watts AW, Mason SM, Loth K, Larson N, Neumark-Sztainer D. Socioeconomic differences in overweight and weight-related behaviors across adolescence and young adulthood: 10-year longitudinal findings from Project EAT. Preventive Med. 2016;87:194–9.
Mendoza JA, Drewnowski A, Christakis DA. Dietary energy density is associated with obesity and the metabolic syndrome in U.S. adults. Diabetes Care. 2007;30:974.
Ledikwe JH, Blanck HM, Kettel Khan L, Serdula MK, Seymour JD, Tohill BC, et al. Dietary energy density is associated with energy intake and weight status in US adults. Am J Clin Nutr. 2006;83:1362–8.
Norman JE, Bild D, Lewis CE, Liu K, West DS. The impact of weight change on cardiovascular disease risk factors in young black and white adults: the CARDIA study. Int J Obes. 2003;27:369.
Adamson L, Brown W, Byles J, Chojenta C, Dobson A, Fitzgerald D, et al. Women’s weight: findings from the Australian longitudinal study on women’s health. The University of Newcastle, The University of Queensland; 2007.
Pengpid S, Peltzer K. Associations between behavioural risk factors and overweight and obesity among adults in population-based samples from 31 countries. Obes Res Clin Pr. 2017;11:158–66.
McCrory MA, Suen VM, Roberts SB. Biobehavioral influences on energy intake and adult weight gain. J Nutr. 2002;132:3830s–4s.
Aljadani H, Patterson A, Sibbritt D, Collins CE. Diet quality and weight change in adults over time: a systematic review of cohort studies. Curr Nutr Rep. 2015;4:88–101.
Aljadani H, Patterson A, Sibbritt D, Collins C. The association between dietary patterns and weight change in adults over time: a systematic review of studies with follow up. JBI Database Syst Rev Implement Rep. 2013;11:272–316.
Aljadani HM, Patterson A, Sibbritt D, Hutchesson MJ, Jensen ME, Collins CE. Diet quality, measured by fruit and vegetable intake, predicts weight change in young women. J Obes. 2013;2013:525161.
Ebrahimi-Mameghani M, Scott JA, Der G, Lean ME, Burns CM. Changes in weight and waist circumference over 9 years in a Scottish population. Eur J Clin Nutr. 2008;62:1208–14.
Brown W, Bryson L, Byles J, Dobson A, Manderson L, Schofield M, et al. Women’s Health Australia: Establishment of The Australian Longitudinal Study on Women’s Health. J Women’s Health. 1996;5:467–72.
Brown WJ, Bryson L, Byles JE, Dobson AJ, Lee C, Mishra G, et al. Women’s Health Australia: recruitment for a national longitudinal cohort study. Women Health. 1998;28:23–40.
Australian Longitudinal Study for Womens Health (ALSWH). Australian longitudinal study for womens health Canberra, ACT Australian Government Department of Health; 2014. http://www.alswh.org.au.
Ireland P, Jolley D, Giles G, O’Dea K, Powles J, Rutishauser I, et al. Development of the Melbourne FFQ: a food frequency questionnaire for use in an Australian prospective study involving an ethnically diverse cohort. Asia Pac J Clin Nutr. 1994;3:19–31.
Hodge A, Patterson AJ, Brown WJ, Ireland P, Giles G. The Anti Cancer Council of Victoria FFQ: relative validity of nutrient intakes compared with weighed food records in young to middle-aged women in a study of iron supplementation. Aust N Z J Public Health. 2000;24:576–83.
Lewis J, Milligan G, Hunt A. NUTTAB 1995: nutrient data table for use in Australia. Canberra, Australia Australia New Zealand Food Authority; 1995.
Kant AK, Thompson FE. Measures of overall diet quality from a food frequency questionnaire: National Health Interview Survey, 1992. Nutr Res. 1997;17:1443–56.
Collins CE, Young AF, Hodge A. Diet quality is associated with higher nutrient intake and self-rated health in mid-aged women. J Am Coll Nutr. 2008;27:146–57.
Collins CE, Burrows TL, Rollo ME, Boggess MM, Watson JF, Guest M, et al. The comparative validity and reproducibility of a diet quality index for adults: the Australian Recommended Food Score. Nutrients. 2015;7:785–98.
National Health and Medical Research Council (NHMRC). Eat for Health: Australian Dietary Guidelines. 2013. https://www.eatforhealth.gov.au/sites/default/files/content/n55_australian_dietary_guidelines.pdf.
McNaughton SA, Dunstan DW, Ball K, Shaw J, Crawford D. Dietary quality is associated with diabetes and cardio-metabolic risk factors. J Nutr. 2009;139:734–42.
Olstad DL, Lamb KE, Thornton LE, McNaughton SA, Crawford DA, Minaker LM, et al. Prospective associations between diet quality and body mass index in disadvantaged women: the Resilience for Eating and Activity Despite Inequality (READI) study. Int J Epidemiol. 2017;46:1433–43.
Fung TT, Chiuve SE, Tobias DK, Hu FB, Willett WC, Hou T, et al. Long-term change in diet quality Is associated with body weight change in men and women. J Nutr. 2015;145:1850–6.
Wolongevicz DM, Zhu L, Pencina MJ, Kimokoti RW, Newby PK, D’Agostino RB, et al. Diet quality and obesity in women: the Framingham Nutrition Studies. Br J Nutr. 2010;103:1223–9.
Schwingshackl L, Hoffmann G, Kalle-Uhlmann T, Arregui M, Buijsse B, Boeing H. Fruit and vegetable consumption and changes in anthropometric variables in adult populations: a systematic review and meta-analysis of prospective cohort studies. PLoS ONE. 2015;10:e0140846–e.
Bertoia ML, Mukamal KJ, Cahill LE, Hou T, Ludwig DS, Mozaffarian D, et al. Changes in intake of fruits and vegetables and weight change in United States men and women followed for up to 24 years: analysis from three prospective cohort studies. PLoS Med. 2015;12:e1001878–e.
Burton NW, Brown W, Dobson A. Accuracy of body mass index estimated from self-reported height and weight in mid-aged Australian women. Aust N. Z J Public Health. 2010;34:620–3.
Trijsburg L, Geelen A, Hollman PC, Hulshof PJ, Feskens EJ, Van’t Veer P, et al. BMI was found to be a consistent determinant related to misreporting of energy, protein and potassium intake using self-report and duplicate portion methods. Public Health Nutr. 2017;20:598–607.
Acknowledgements
The analysis presented was conducted as part of the Australian Longitudinal Study on Women’s Health, the University of Newcastle and the University of Queensland. We are grateful to the Australian Government Department of Health and Ageing (DOHA) and to the women who provided the survey data. We also thank Graham Giles and Alison Hidge of the Cancer Epidemiology Centre of The Cancer Council Victoria for permission to use the Dietary Questionnaire for Epidemiological Studies (version 2), Melbourne, VIC Australia; The Cancer Council Victoria, 1996.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. HMA was funded by a PhD scholarship from the King Abdulaziz University and the Ministry of Higher Education, Kingdom of Saudi Arabia and the University of Newcastle supported the research. CEC is supported by the National Health and Medical Research Council of Australia Senior Research Fellowship, and the Gladys M Brawn Senior Research Fellowship from the Faculty of Health and Medicine, the University of Newcastle, Australia.
Author information
Authors and Affiliations
Contributions
Contribution of each author; HMA, AP, DS, and CEC conceptualised the research project; all authors were involved in the design of the study; HMA conducted the research with statistical support from DS; HMA conducted the analysis and HMA, RMT drafted the paper; all authors edited and provided feedback and approved the final paper. The content in this paper is the original work of all authors involved. The paper is not under consideration nor published elsewhere in the same or in a similar form. All authors have read and approved the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aljadani, H.M., Patterson, A., Sibbritt, D. et al. Frequency and variety of usual intakes of healthy foods, fruit, and vegetables predicts lower 6-year weight gain in young women. Eur J Clin Nutr 74, 945–952 (2020). https://doi.org/10.1038/s41430-019-0532-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-019-0532-8
- Springer Nature Limited