Abstract
Background/objectives:
Clinical trials of eicosapentaenoic acid (EPA) among high-risk groups in Japan in which consumption of mairne-omega-3 fatty acids (OM3) is much higher than other countries showed slower progression of coronary atherosclerosis. We aimed to determine the cross-sectional associations of coronary artery calcification (CAC) and calcium density with OM3, EPA, and docosahexaenoic acid (DHA), two principal OM3, in the general population in Japan.
Subjects/methods:
The Shiga Epidemiological Study of Subclinical Atherosclerosis examined a population-based sample of 1074 men aged 40–79 in 2006–08 for computed tomography-measured CAC score (CCS), a well-established biomarker of coronary atherosclerosis, CAC density score (CDS), a potential marker of plaque stabilization, serum levels of OM3, and risk factors.
Results:
Prevalence of CCS > 0, ≥ 100, and ≥ 300 was 65.8%, 25.9%, and 12.9%, respectively; the mean (SD) OM3, EPA, and DHA were 10.1% (3.2), 3.2% (1.7), and 5.9% (1.6), respectively. Odds ratios (95% CI, p-value) of CCS 0, 100, and 300 in ordinal logistic regression associated with 1 SD increase of OM3, EPA, and DHA were 0.91 (0.81–1.03, p = 0.12), 0.99 (0.88–1.11, p = 0.87) and 0.84 (0.74–0.94, p = < 0.01), respectively. The inverse association of DHA with CCS remained significant in multivariate-adjusted model: odds ratio of 0.87 (0.77–0.99, p = 0.03). Blood levels of OM3, EPA, or DHA did not have any significant associations with CDS.
Conclusions:
DHA but not EPA had a significant inverse association with coronary atherosclerosis in the general population with high levels of OM3. Future trials are warranted comparing the effect of high-dose DHA and EPA on atherosclerosis and cardiovascular outcomes.
Similar content being viewed by others
Introduction
Recent long-term large randomized clinical trials (RCTs) of marine omega-3 fatty acids (OM3) on coronary heart disease (CHD) among high-risk groups all failed to show clinical benefit of OM3, i.e., Alpha-Omega Trial, Outcome Reduction With Initial Glargine Intervention Trial (ORIGIN), Supplementation en Folates et Aomega-3 (SU.FOM.OM3) and the Risk and Prevention Study [1,2,3,4] of which doses of administered OM3 ranged from 0.3 to 0.9 g/day. In contrast, JELIS (Japan Eicosapentaenoic acid (EPA) Lipid Intervention Study), which randomized 18,465 patients with hypercholesterolemia with and without cardiovascular disease to receive a statin plus 1.8 g/day of EPA, one of the two principal OM3, or statin alone, showed a significant 19% relative reduction in major coronary events with no significant changes between treatment groups in low-density lipoprotein cholesterol (LDL-C) [5]. Another RCT of 241 Japanese patients with acute coronary syndrome showed a significant 11% relative reduction in cardiovascular events in a statin plus 1.8 g/day of EPA compared to statin alone [6]. Of note, we and others pointed out that 1.8 g/day of EPA in Japanese trials (on top of the high consumption of OM3 in Japan) will generate blood levels of OM3 that would require about 3.6 g/day of OM3 on a US background diet [7, 8] (the median background dietary intake of OM3 (g/day) in Japan is 1.1 compared to < 0.1 in the US [9, 10]). Additionally, three recent RCTs of 1.8 g/day of EPA conducted in Japan showed significantly slower progressions of coronary plaque among patients with CHD [11, 12] and carotid intima-media thickness (CIMT) among patients with diabetes [13]. These results indicate that high-dose OM3 is anti-atherogenic in high-risk groups. A cross-sectional study of 261 inhabitants in the fishing village and 209 in the farming village in Japan showed a significant inverse association of blood levels of OM3 with the number of carotid plaque [14] implying that OM3 may be anti-atherogenic even in the general population with high consumption of OM3.
Coronary artery calcification (CAC) is a well-established biomarker of coronary atherosclerosis. CAC predicts future cardiovascular events much better than carotid plaque [15]. In studies of Western population, CAC shows no significant association with dietary intake of OM3 [16, 17] potentially due to much lower consumption of OM3 in Western than Japanese populations. A recent observational study documents that calcium density of the coronary plaque is inversely associated with cardiovascular events at a given level of CAC [18], suggesting that higher calcium density represents more stable plaque. RCTs of OM3 among patients with endarterectomy reported that OM3 increases plaque stability [19, 20].
In this study, we hypothesized that blood levels of OM3 in Japanese would have a significant inverse association with CAC and that the inverse association of OM3 with CAC is primarily attributed to docosahexaenoic acid (DHA), another principal OM3, based on our previous study in Japanese showing that blood levels of DHA but not EPA had a significant inverse association with CIMT [21]. We also hypothesized that blood levels of OM3 would have a significant positive association with CAC density. We tested these hypotheses in a population-based sample of 1094 Japanese from the Shiga Epidemiological Study of Subclinical Atherosclerosis (SESSA).
Subjects and methods
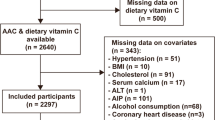
SESSA is a population-based study of a random sample from a general Japanese population as previously described in detail [22,23,24,25,26]. Briefly, a total of 1094 men aged 40 to 79 years were recruited in 2006–2008. After excluding eight participants with missing data (n = 7 for LDL-C and n = 1 for volume score), a total of 1086 participants were analyzed for the current study. There were 102 participants with a history of myocardial infarction (MI), stroke or chronic kidney disease (CKD). The study was approved by the Institutional Review Boards of Shiga University of Medical Science and University of Pittsburgh. All participants provided written informed consent.
CAC measurements
CAC was assessed using either electron-beam computed tomography (EBCT, n = 756) using a C-150 scanner (Imatron, South San Francisco, CA, US) or 16-channel multi-detector-row computed tomography (MDCT, n = 330) using an Aquilion scanner (Toshiba, Tokyo, Japan) [24,25,26]. Images were obtained from the level of the root of the aorta through the heart at a 3-mm slice thickness with a scan time of 100 milliseconds (EBCT) or 320 milliseconds (MDCT). CAC was quantified using AccuImage software (AccuImage Diagnostics, South San Francisco, CA, US). The presence of CAC was defined as a minimum of three contiguous pixels (area = 1 mm2) with density ≥ 130 Hounsfield Units. CAC score (CCS) was calculated according to the Agatston method [27]. A volume score was also calculated [28]. CAC density score (CDS) was calculated as Agatston score divided by area score where the area score was calculated as the volume score divided by the slice thickness: 3 mm [18]. All images were read by a single physician trained at the Cardiovascular Institute, University of Pittsburgh, who was blinded to participant’s characteristics. The reproducibility of the scans showed an intraclass correlation of 0.98 for both CCS and CDS.
Blood levels of OM3 and other fatty acids
Venipuncture was performed early in the clinic visit after a 12-h fast. Serum samples were stored at −80 °C and shipped on dry ice to University of Pittsburgh. Fatty acids were analyzed by capillary-gas-liquid chromatography (PerkinElmer Clarus 500) [29]. OM3 was defined as the sum of EPA, docosapentaenoic acid (DPA) and DHA. The coefficients of variation for EPA, DPA, and DHA were 4.5%, 4.5%, and 7.2%, respectively. Those for plant-based omega-3 fatty acid: alpha-linolenic acid (ALA), and two major omega-6 fatty acids: linoleic (LA) and arachidonic fatty acids (ARA), were 7.9%, 1.6%, and 4.5%, respectively.
Other measurements
A self-administered questionnaire was used to obtain information from participants on demography, smoking, alcohol drinking, medication (hypertension, dyslipidemia, and diabetes mellitus), and medical history as previously described [22,23,24,25,26]. Pack-years of smoking were calculated as years of smoking multiplied by the number of cigarettes per day divided by 20. Alcohol drinking was assessed based on the quantity and frequency of beer, wine, liquor, or sake (Japanese rice wine) consumption by the participant. An alcohol drinker was defined as an individual who consumed alcohol ≥ two times a week. Ethanol consumption per day was estimated, assuming that concentrations of alcohol were 5%, 12%, 40%, and 16% for beer, wine, liquor, and sake, respectively.
Body mass index (BMI) was calculated as weight in kilograms divided by the square of the height in meters. Blood pressure (BP) was measured in the right arm of the seated participant after the participant sat quietly for 5 min, using an appropriate-sized cuff, with an automated sphygmomanometer (BP-8800, Omron Health Care Co. Ltd, Tokyo, Japan). The average of two measurements was used to determine BP. Hypertension was defined as systolic BP ≥ 140 mm Hg, diastolic BP ≥ 90 mm Hg, or use of anti-hypertensive medication. Diabetes mellitus was defined as a hemoglobin A1c ≥ 6.5% [30], a fasting blood glucose ≥ 7.0 mmol/L or use of anti-diabetic medication. CKD was defined as an estimated glomerular filtration rate < 30 mL/min [31].
Total cholesterol and triglycerides were measured using enzymatic assays, and high-density lipoprotein cholesterol (HDL-C) using a direct method. LDL-C was estimated using Friedewald’s formula [32]. When triglycerides exceeded 4.52 mmol/L, we did not estimate LDL-C and excluded these participants from the study (n = 7). Lipid measurements were standardized according to the protocol for the US Centers for Disease Control and Prevention/Cholesterol Reference Method Laboratory Network. C-reactive protein (CRP) was measured by nephelometry using a BN II Analyzer.
Statistics
Participant characteristics were shown as means and standard deviations (SDs) for continuous variables with approximately normal distributions, medians, and inter-quartile ranges for continuous variables with skewed distributions, and frequencies and percentages for categorical variables. To examine the univariate associations of the CCS with participant’s characteristics, we used a general linear model to compare characteristics across four groups of CCS using cutoff points of CCS 0, 100 and 300 (CCS = 0, CCS < 100, CCS > 300 and CCS ≥ 300), adjusting for age because CCS was age dependent. These cutoff points are widely used and clinically relevant [33, 34]. To examine multivariable associations of CCS with each of OM3, EPA, and DHA, we used both ordinal logistic and robust linear regressions because the distribution of CCS was highly skewed. For ordinal logistic regression, we chose cutoff points of CCS 0, 100, and 300. For multivariable adjustments in both ordinal logistic and robust linear regressions, we first adjusted for age and CT type (Model I), then further adjusted for hypertension, diabetes, LDL-C, HDL-C, pack-years of smoking and BMI (Model II) based on previous studies [35, 36]. In Model III, we additionally adjusted for CRP, triglycerides, ethanol intake, and medications for lipids and hypertension as well as cardio-renal disease (a past history of MI, stroke or CKD). To examine the univariate association of CDS with the participant’s characteristics, we used a general linear model to compare characteristics across three even groups of CDS adjusting for age. To examine multivariable associations of CDS with each of OM3, EPA, and DHA at a given CAC score, we used robust linear regression using the same modeling strategy as described above except that we adjusted for log-transformed CCS in Model I. As sensitivity analyses, the association was examined excluding those with cardio-renal disease. Additionally, the associations of CDS with each of OM3, EPA, and DHA were analyzed excluding participants on lipid-lowering medication because statin therapy might increase calcium density [18]. As our supplemental analyses, the associations of CCS and CDS with each of ALA, LA, and ARA were examined. Two-tailed p-values of < .05 were considered to indicate statistical significance. Although we had two outcomes (CAC and CDS) no adjustment was made for the multiple testing. All these statistical analyses were performed with SAS version 9.3 (SAS Institute, Cary, NC, US).
Results
Among 1086 participants the mean (SD) age was 64.1 (9.9) years (Table 1); 56.1% were hypertensive, 22.2% had diabetes, and 31.9% were current smokers. The mean (SD) LDL-C was 3.22 (0.82) mmol/L. CAC was present in 714 subjects (65.8%), and prevalence of CCS ≥ 100 and ≥ 300 was 25.9% and 12.9%, respectively. The mean (SD) OM3, EPA, and DHA were 10.1 (3.2), 3.2 (1.7), and 5.9 (1.6), respectively.
Generally, cardiovascular risk factors had a positive significant association with the CCS categories including age, BMI, systolic BP, total cholesterol, CRP, pack-years of smoking, and rates of hypertension and diabetes (Table 2). In contrast, neither OM3, EPA, DHA nor other fatty acids had significant associations with the CCS categories.
In contrast to CCS, the category of CDS had no significant associations with cardiovascular risk factors (Table 3). Likewise, levels of fatty acids including OM3, EPA, and DHA were very similar across the three groups. Although rates of participants on lipid-lowering medication tended to be higher in the higher categories of CDS, the association did not reach statistical significance.
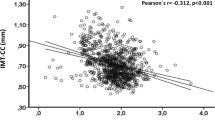
Ordinal logistic regressions showed that DHA had a significant inverse association with CCS after adjusting for age and CT type (odds ratio (OR): 0.84, 95% confidence interval (CI): 0.74–0.94, p < 0.01) (Table 4). The inverse association remained significant after further adjusting for traditional cardiovascular risk factors (OR: 0.88, 95% CI: 0.0.78–0.99, p = 0.045) and other factors (OR: 0.87, 95% CI 0.77–0.99, p = 0.03). Robust linear regression also showed a significant inverse association of DHA with CCS, which remained after adjusting for various risk factors. In contrast, EPA had almost null associations with CCS in all models and in both ordinal logistic and robust regression analyses. OM3 had an inverse association with CCS in all models without statistical significance. The above results did not materially change when we excluded individuals with cardio-renal disease (Supplemental Table 1). The association of ALA, LA, or ARA with CCS was null and non-significant (Supplemental Table 2).
The associations of CDS with each of OM3, EPA, and DHA were inverse (Table 5) without statistical significance except for Model II for OM3 and EPA. The above results did not change when we excluded individuals with cardio-renal disease (Supplemental Table 3). Even after excluding participants on lipid-lowering medications, the association was non-significant (Supplemental Table 4). The association of ALA, LA, or ARA with CDS was virtually null (Supplemental Table 5).
Discussion
This population-based cross-sectional study of 1086 men showed that serum levels of OM3 had a non-significant inverse association with CCS. When the association of EPA and DHA was examined separately, DHA but not EPA had a significant inverse association with CCS. The significant inverse association of DHA with CCS remained after adjusting for various factors or after excluding participants with cardio-renal disease. In contrary to our hypothesis, serum levels of OM3, EPA, or DHA had no significant associations with CDS. The associations of serum levels of ALA, LA, and ARA with CCS and CDS were virtually null. This study is the first to document the significant inverse association of DHA with CCS in the general population.
Numerous preclinical studies have documented the anti-atherogenic properties of OM3 [37], yet epidemiological studies in Western countries do not show any significant association of OM3 with CAC. The Multi-Ethnic Study of Atherosclerosis found no significant cross-sectional association of dietary intake of OM3 with CAC in 5488 subjects [17]. The Rotterdam Study found no significant longitudinal association of dietary intake of OM3 with CAC in 1570 subjects [16]. Median dietary intake of OM3 in these two populations was about 100 mg/day, which is less than one-tenth of the Japanese general population [9, 10].
It is perceived that increasing dietary intake of OM3 more than 1.0 g/day has no cardiovascular benefit in the general population [38]. Three recent large prospective cohort studies in Japan, however, showed that higher dietary intake of OM3 (median dietary intake ranges from 1.7 to 2.3 g/day in the highest quartile or quintile) was inversely associated with cardiovascular outcomes. A 10-year prospective cohort study of 41,578 men and women documented a significant inverse association of dietary intake of OM3 with non-fatal MI (multivariable-adjusted hazard ratio (m-HR) of 0.33, 95% CI: 0.17–0.63, comparing the highest to the lowest quintile) [39]. A 12.7-year prospective cohort study of 57,972 men and women showed a significant inverse association of dietary intake of OM3 with cardiovascular events (m-HR of 0.81, 95% CI: 0.67–0.98, comparing the highest to the lowest quartile) [40]. A 24-year prospective cohort study of 9190 men and women demonstrated a significant inverse association of dietary intake of OM3 with cardiovascular death (m-HR of 0.80, 95% CI: 0.66–0.96, comparing the highest to the lowest quintile) [41]. The latter two studies reported an inverse but non-significant association of dietary intake of OM3 with CHD, yet the non-significant association was likely due to the relatively small numbers of CHD cases [42]. These results were consistent with our finding that serum levels of OM3 had a significant inverse association with CAC the general population in Japan.
We observed a significant inverse association of CAC with DHA but not EPA. This observation was consistent with some previous observational studies reporting significant inverse associations of DHA but not EPA with coronary atherosclerosis in women with CHD (longitudinal) [43] and CIMT in the general population in Japan (cross-sectional) [21]. Additionally, a review of case–control studies reported that DHA had stronger inverse association with CHD than EPA [44]. However, a more recent systematic review on observational studies and RCTs showed that the relative risks of EPA and DHA associated with CHD were very similar [45]. Short-term (6 weeks) RCTs of high-dose OM3 (4 g/day) documented somewhat differential effects of purified EPA and DHA on cardiovascular risk factors in patients without CHD, e.g., DHA but not EPA significantly increased HDL-C and reduced BP and heart rate [46,47,48]. No RCTs have compared the differential effect of EPA and DHA on atherosclerosis or cardiovascular outcomes.
Evidence from RCTs in Japan demonstrated that high-dose pure EPA had anti-atherogenic properties in patients with CHD [11, 12] and diabetes [13]. In these Japanese RCTs [12, 13], blood levels of EPA increased, whereas those of DHA decreased in the intervention group indicating that the anti-atherogenic properties of OM3 in these RCTs among high-risk groups were attributed to EPA. Whether high-dose (4.0 g/day) purified EPA or primarily EPA is anti-atherogenic (EVAPORATE: NCT02926027) or reduces cardiovascular outcome (REDUCE IT: NCT 01492361, STRENGTH: NCT02104817) is currently under investigation in high-risk groups. Our results suggest that DHA may have more potent anti-atherogenic properties than EPA in the general population. Future trials are warranted comparing the effect of DHA and EPA on atherosclerosis and cardiovascular outcomes.
Contrary to our hypothesis that OM3 would have a positive association with CDS based on an RCT of OM3 among patients with endarterectomy, which reported that OM3 increases plaque stability [19], we observed inverse associations of OM3 with CDS. In this RCT, plaque stabilization was partly associated with well-formed fibrous caps in the invention group and increasing calcium density may not necessarily be a mechanism for plaque stabilization of OM3.
Our study showed no significant association of CAC or CDS with serum levels of ALA, LA, or ARA. This finding is consistent with the results from a recent meta-analysis of blood levels of these fatty acids with coronary outcomes in ten large prospective cohort studies and RCTs [49] except for ARA. This meta-analysis documented a significant inverse association of coronary outcomes with ARA. Our finding of the null association of ARA with CCS or CDS might suggest that ARA may be cardioprotective through mechanisms other than anti-atherosclerosis.
Limitations of this study include first: blood levels of OM3 reflect short-term dietary intake and may not reflect long-term dietary intake. However, in populations where intake of OM3 is high like Japanese, a single measurement of blood levels of EPA and DHA reflects habitual intake of EPA and DHA, respectively [50]. Second, the study was observational thus we cannot rule out the possibility of residual or unmeasured confounding. Third, the participants were men only and the results cannot be extended to women. Third, we did not make any adjustment to alpha level to conserve the power, though we had two outcomes (CAC and CDS). However, even after the Bonferroni correction to alpha for two different outcomes (i.e., 0.05/2 = 0.025), the result did not change materially: the inverse association of DHA with CAC remained significant. Fourth, although pure EPA and pure DHA are available to conduct intervention studies in human [46], pure DPA is not. Thus, we did not show the results of DPA. However, DPA did not have any significant association with CAC or CAC density (data not shown). Finally, about 25% of individuals had CDS slightly greater than 4.0 though the score theoretically ranges from 1.0 to 4.0. The reason for this is unknown. The results did not materially change when we excluded participants with CDS > 4.0 (data not shown).
Three RCTs of high-dose pure EPA conducted in Japan demonstrated the anti-atherogenic properties of EPA in high-risk subjects [11,12,13]. This study documents the significant inverse association of DHA but not EPA with coronary atherosclerosis in the general population with high consumption of OM3 suggesting that DHA may be more anti-atherogenic than EPA. Studies of comparing high-dose DHA and EPA to prevent atherosclerotic cardiovascular disease are justified.
References
Kromhout D, Giltay EJ, Geleijnse JM. n–3 fatty acids and cardiovascular events after myocardial infarction. New Engl J Med. 2010;363:2015–26.
Galan P, Kesse-Guyot E, Czernichow S, Briancon S, Blacher J, Hercberg S. Effects of B vitamins and omega 3 fatty acids on cardiovascular diseases: a randomised placebo controlled trial. BMJ. 2010;341:c6273.
The ORIGIN Trial Investigators. n-3 fatty acids and cardiovascular outcomes in patients with dysglycemia. N Engl J Med. 2012;367:309–18.
Roncaglioni MC, Tombesi M, Avanzini F, Barlera S, Caimi V, Longoni P, et al. n-3 fatty acids in patients with multiple cardiovascular risk factors. N Engl J Med. 2013;368:1800–8.
Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet. 2007;369:1090–8.
Nosaka K, Miyoshi T, Iwamoto M, Kajiya M, Okawa K, Tsukuda S, et al. Early initiation of eicosapentaenoic acid and statin treatment is associated with better clinical outcomes than statin alone in patients with acute coronary syndromes: 1-year outcomes of a randomized controlled study. Int J Cardiol. 2017;228:173–9.
Sekikawa A, Doyle MF, Kuller LH. Recent findings of long-chain n-3 polyunsaturated fatty acids (LCn-3 PUFAs) on atherosclerosis and coronary heart disease (CHD) contrasting studies in Western countries to Japan. Trends Cardiovasc Med. 2015;25:717–23.
Bays HE, Ballantyne CM, Doyle RT, Jr., Juliano RA, Philip S. Icosapent ethyl: Eicosapentaenoic acid concentration and triglyceride-lowering effects across clinical studies. Prostaglandins Other Lipid Mediat. 2016;125:57–64.
Sekikawa A, Steingrimsdottir L, Ueshima H, Shin C, David Curb J, Evans RW, et al. Serum levels of marine-derived n-3 fatty acids in Icelanders, Japanese, Koreans, and Americans-A descriptive epidemiologic study. Prostaglandins Leukot Essent Fat Acids. 2012;87:11–6.
Stamler J, Elliott P, Chan Q. Intermap appendix tables. J Hum Hypertens. 2003;17:665–775. (for the INTERMAP Research Group)
Niki T, Wakatsuki T, Yamaguchi K, Taketani Y, Oeduka H, Kusunose K, et al. Effects of the addition of eicosapentaenoic acid to strong statin therapy on inflammatory cytokines and coronary plaque components assessed by integrated backscatter intravascular ultrasound. Circ J. 2016;80:450–60.
Watanabe T, Ando K, Daidoji H, Otaki Y, Sugawara S, Matsui M, et al. A randomized controlled trial of eicosapentaenoic acid in patients with coronary heart disease on statins. J Cardiol. 2017;70:537–44.
Mita T, Watada H, Ogihara T, Nomiyama T, Ogawa O, Kinoshita J, et al. Eicosapentaenoic acid reduces the progression of carotid intima-media thickness in patients with type 2 diabetes. Atherosclerosis. 2007;191:162–7.
Yamada T, Strong JP, Ishii T, Ueno T, Koyama M, Wagayama H, et al. Atherosclerosis and [omega]-3 fatty acids in the populations of a fishing village and a farming village in Japan. Atherosclerosis. 2000;153:469–81.
Gepner AD, Young R, Delaney JA, Tattersall MC, Blaha MJ, Post WS, et al. Comparison of coronary artery calcium presence, carotid plaque presence, and carotid intima-media thickness for cardiovascular disease prediction in the Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Imaging. 2015;8:002262.
Heine-Broring RC, Brouwer IA, Proenca RV, van Rooij FJ, Hofman A, Oudkerk M, et al. Intake of fish and marine n-3 fatty acids in relation to coronary calcification: the Rotterdam Study. Am J Clin Nutr. 2010;91:1317–23.
He K, Liu K, Daviglus ML, Mayer-Davis E, Jenny NS, Jiang R, et al. Intakes of long-chain n-3 polyunsaturated fatty acids and fish in relation to measurements of subclinical atherosclerosis. Am J Clin Nutr. 2008;88:1111–8.
Criqui MH, Denenberg JO, Ix JH, McClelland RL, Wassel CL, Rifkin DE, et al. Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA. 2014;311:271–8.
Thies F, Garry JMC, Yaqoob P, Rerkasem K, Williams J, Shearman CP, et al. Association of n-3 polyunsaturated fatty acids with stability of atherosclerotic plaques: a randomised controlled trial. Lancet. 2003;361:477–85.
Cawood AL, Ding R, Napper FL, Young RH, Williams JA, Ward MJA, et al. Eicosapentaenoic acid (EPA) from highly concentrated n−3 fatty acid ethyl esters is incorporated into advanced atherosclerotic plaques and higher plaque EPA is associated with decreased plaque inflammation and increased stability. Atherosclerosis. 2010;212:252–9.
Sekikawa A, Kadowaki T, El-Saed A, Okamura T, Sutton-Tyrrell K, Nakamura Y, et al. Differential association of docosahexaenoic and eicosapentaenoic acids with carotid intima-media thickness. Stroke. 2011;42:2538–43.
Kadota A, Miura K, Okamura T, Fujiyoshi A, Ohkubo T, Kadowaki T, et al. Carotid intima-media thickness and plaque in apparently healthy Japanese individuals with an estimated 10-year absolute risk of CAD death according to the Japan Atherosclerosis Society (JAS) Guidelines 2012: The Shiga Epidemiological Study of Subclinical Atherosclerosis (SESSA). J Atheroscler Thromb. 2013;20:755–66.
Fujiyoshi A, Miura K, Kadowaki S, Azuma K, Tanaka S, Hisamatsu T, et al. Lifetime cigarette smoking is associated with abdominal obesity in a community-based sample of Japanese men: The Shiga Epidemiological Study of Subclinical Atherosclerosis (SESSA). Prev Med Rep. 2016;4:225–32.
Fujiyoshi A, Miura K, Ohkubo T, Kadowaki T, Kadowaki S, Zaid M, et al. Cross-sectional comparison of coronary artery calcium scores between Caucasian men in the United States and Japanese men in Japan: The Multi-Ethnic Study of Atherosclerosis and the Shiga Epidemiological Study of Subclinical Atherosclerosis. Am J Epidemiol. 2014;180:590–8.
Ueshima H, Kadowaki T, Hisamatsu T, Fujiyoshi A, Miura K, Ohkubo T, et al. Lipoprotein-associated phospholipase A2 is related to risk of subclinical atherosclerosis but is not supported by Mendelian randomization analysis in a general Japanese population. Atherosclerosis. 2016;246:141–7.
Hisamatsu T, Miura K, Arima H, Kadota A, Kadowaki S, Torii S, et al. Smoking, Smoking cessation, and measures of subclinical atherosclerosis in multiple vascular beds in Japanese men. J Am Heart Assoc. 2016;5:e003738.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr., Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32.
Rumberger JA, Kaufman L. A rosetta stone for coronary calcium risk stratification: agatston, volume, and mass scores in 11,490 individuals. AJR Am J Roentgenol. 2003;181:743–8.
Sekikawa A, Curb JD, Ueshima H, El-Saed A, Kadowaki T, Abbott RD, et al. Marine-derived n-3 fatty acids and atherosclerosis in Japanese, Japanese-American, and white men: a cross-sectional study. J Am Coll Cardiol. 2008;52:417–24.
Zaid M, Miura K, Fujiyoshi A, Abbott RD, Hisamatsu T, Kadota A, et al. Associations of serum LDL particle concentration with carotid intima-media thickness and coronary artery calcification. J Clin Lipidol. 2016;10:1195–202.e1.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Arad Y, Goodman KJ, Roth M, Newstein D, Guerci AD. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: the St. Francis Heart Study. J Am Coll Cardiol. 2005;46:158–65.
Pletcher MJ, Sibley CT, Pignone M, Vittinghoff E, Greenland P. Interpretation of the coronary artery calcium score in combination with conventional cardiovascular risk factors: The Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2013;128:1076–84.
Bild DE, Detrano R, Peterson D, Guerci A, Liu K, Shahar E, et al. Ethnic Differences in coronary calcification: The Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2005;111:1313–20.
Sekikawa A, Ueshima H, Kadowaki T, El-Saed A, Okamura T, Takamiya T, et al. Less subclinical atherosclerosis in Japanese men in Japan than in White men in the United States in the post-World War II birth cohort. Am J Epidemiol. 2007;165:617–24.
Massaro M, Scoditti E, Carluccio MA, Campana MC, De Caterina R. Omega-3 fatty acids, inflammation and angiogenesis: basic mechanisms behind the cardioprotective effects of fish and fish oils. Cell Mol Biol (Noisy-Le-Grand). 2010;56:59–82.
Mozaffarian D, Rimm EB. Fish intake, contaminants, and human health: evaluating the risks and the benefits. JAMA. 2006;296:1885–99.
Iso H, Kobayashi M, Ishihara J, Sasaki S, Okada K, Kita Y, et al. Intake of fish and n3 fatty acids and risk of coronary heart disease among Japanese: the Japan Public Health Center-Based (JPHC) Study Cohort I. Circulation. 2006;113:195–202.
Yamagishi K, Iso H, Date C, Fukui M, Wakai K, Kikuchi S, et al. Fish, [omega]-3 Polyunsaturated fatty acids, and mortality from cardiovascular diseases in a nationwide community-based cohort of Japanese men and women: The JACC (Japan Collaborative Cohort Study for Evaluation of Cancer Risk) Study. J Am Coll Cardiol. 2008;52:988–96.
Miyagawa N, Miura K, Okuda N, Kadowaki T, Takashima N, Nagasawa SY, et al. Long-chain n-3 polyunsaturated fatty acids intake and cardiovascular disease mortality risk in japanese: a 24-year follow-up of NIPPON DATA80. Atherosclerosis. 2014;232:384–9.
Ueshima H, Sekikawa A, Miura K, Turin TC, Takashima N, Kita Y, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008;118:2702–9.
Erkkila AT, Matthan NR, Herrington DM, Lichtenstein AH. Higher plasma docosahexaenoic acid is associated with reduced progression of coronary atherosclerosis in women with CAD. J Lipid Res. 2006;47:2814–9.
Harris WS, Poston WC, Haddock CK. Tissue n-3 and n-6 fatty acids and risk for coronary heart disease events. Atherosclerosis. 2007;193:1–10.
Del Gobbo LC, Imamura F, Aslibekyan S, Marklund M, Virtanen JK, Wennberg M, et al. Omega-3 polyunsaturated fatty acid biomarkers and coronary heart disease: Pooling project of 19 cohort studies. JAMA Intern Med. 2016;176:1155–66.
Mori TA, Woodman RJ. The independent effects of eicosapentaenoic acid and docosahexaenoic acid on cardiovascular risk factors in humans. Curr Opin Clin Nutr Metab Care. 2006;9:95–104.
Cottin SC, Sanders TA, Hall WL. The differential effects of EPA and DHA on cardiovascular risk factors. Proc Nutr Soc. 2011;70:215–31.
Mozaffarian D, Wu JH. (n-3) fatty acids and cardiovascular health: are effects of EPA and DHA shared or complementary? J Nutr. 2012;142:614S–25S.
Chowdhury R, Warnakula S, Kunutsor S, Crowe F, Ward HA, Johnson L, et al. Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Ann Intern Med. 2014;160:398–406.
Kobayashi M, Sasaki S, Kawabata T, Hasegawa K, Akabane M, Tsugane S. Single measurement of serum phospholipid fatty acid as a biomarker of specific fatty acid intake in middle-aged Japanese men. Eur J Clin Nutr. 2001;55:643–50.
Acknowledgements
This research project is supported by the following grants: NIH R01 HL068200 and RF1 AG051615; Grants-in-aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology, Japan: (A) 13307016, (A) 17209023, (A) 21249043, (A) 23249036, (A) 25253046, (A) 15H02528, (B) 15H04773, (B) 26293140, and (B) 21790579; and a grant from Glaxo-Smith Klein, GB.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Sekikawa, A., Mahajan, H., Kadowaki, S. et al. Association of blood levels of marine omega-3 fatty acids with coronary calcification and calcium density in Japanese men. Eur J Clin Nutr 73, 783–792 (2019). https://doi.org/10.1038/s41430-018-0242-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-018-0242-7
- Springer Nature Limited
This article is cited by
-
Marine natural products and human immunity: novel biomedical resources for anti-infection of SARS-CoV-2 and related cardiovascular disease
Natural Products and Bioprospecting (2024)
-
New Insights into Prospective Health Potential of ω-3 PUFAs
Current Nutrition Reports (2023)
-
Cross-sectional association of equol producing status with aortic calcification in Japanese men aged 40–79 years
Scientific Reports (2022)
-
Intake of fish and long-chain n-3 polyunsaturated fatty acids and risk of diseases in a Japanese population: a narrative review
European Journal of Clinical Nutrition (2021)
-
Associations of dietary patterns and nutrients with coronary artery calcification and pericardial adiposity in a longitudinal study of adults with and without type 1 diabetes
European Journal of Nutrition (2021)