Abstract
To gain insight into the molecular pathogenesis of patients with mantle cell lymphoma (MCL), next-generation whole-exome sequencing of 16 MCL patients was performed. We identified recurrent mutations in genes that are well known to be functionally relevant in MCL, including ATM (37.5%), TP53 (31.3%), WHSC1 (31.3%), CCND1 (18.8%), NOTCH2 (6.3%), and CDKN2A (6.3%). We also identified somatic mutations in genes for which a functional role in MCL has not been previously suspected. These genes included CCDC15, APC, CDH1, S1PR1, ATRX, BRCA2, CASP8, and NOTCH3. Further, we investigated the prognostic factors associated with MCL from clinical, pathological, and genetic mutations. Mutations of TP53 (P = 0.021) was a significant prognostic factor with shorter overall survival (OS). Although there was no statistical difference, the median survival time of patients with WHSC1 mutations was shorter than those without mutations (P = 0.070). Mutations in ATM and CCND1 had no prognostic value (P = 0.552, 0.566). When adjusted for MCL International Prognostic Index (MIPI) or combined MCL-International Prognostic Index (MIPI-c), TP53 and WHSC1 mutations were the most important prognostic factors in MCL (P < 0.05). Our data provide an unbiased view of the landscape of mutations in MCL and commend that all patients benefit from mutations of TP53 and WHSC1 at diagnosis, in addition to MIPI and MIPI-c score.
Similar content being viewed by others
Introduction
Mantle cell lymphoma (MCL) is an uncommon heterogeneous subtype of non-Hodgkin lymphoma, with distinctive clinical, biologic, and molecular characteristics. MCL comprises 3−6% of non-Hodgkin lymphomas with an annual incidence of 0.5 per 100,000 populations in Western countries. MCL is an aggressive B-cell lymphoma that occurs more than four times as often in males. The median age at diagnosis is about 60 years [1,2,3,4,5]. Most MCL cases have a rapid evolution and an aggressive behavior with an unfavorable outcome. Despite advances in the development of clinical agents leading to high-remission rates in previously untreated patients, relapse within a few years is common, contributing to a rather short median survival of 5−7 years [6]. There is important significance to investigate the molecular mechanisms that contribute to MCL pathogenesis, and how improved understanding of these molecular mechanisms offers new perspectives for the treatment in MCL.
MCL typically possess the hallmark t(11;14)(q13;q32) chromosomal translocation, which causes overexpression of CyclinD1, resulting in disordered progression of the cell cycle and aggressive lymphomagenesis [7]. In addition to this constitutive dysregulation of the cell cycle, other mechanisms such as DNA damage response alterations (e.g., changes in genes ATM, CHK2, TP53) and activation of cell survival pathways (e.g., mTOR, NF-κB, and NOTCH) have been found to play crucial roles in the pathogenesis of MCL [8, 9].
Whole-exome sequencing as a powerful approach to discover novel oncogenic mechanisms has been used in tumor research [10, 11]. As the clinical course of MCL patients is variable, the genetic landscape of tumors might be quite heterogeneous. Whether there are differences in the pathogenesis of different races is unknown, and there is also no report of genomic mutations in Chinese patients with MCL. To gain insight into the molecular pathogenesis of Chinese patients with MCL, we performed next-generation whole-exome sequencing of 16 MCL patients. The clinical and biological characteristics of the patients were analyzed retrospectively. In our study, prognostic factors associated with gene mutations and clinical parameters were analyzed.
Materials and methods
Patients and samples
Patients with MCL and lymphoma tissues available at the time of diagnosis were identified by searching databases of stored formalin-fixed paraffin-embedded specimens at the Peking University Third Hospital. The specimens were collected between 2009 and 2016. In all cases, the diagnosis of MCL was made using appropriate diagnostic criteria for the 2008 WHO classification of lymphoid tumors with combinations of histologic, immunohistochemical, flow cytometric, and genetic evaluation. Medical records were reviewed for demographic and clinical data. Clinical data reviewed included physical examination, laboratory tests (blood counts, renal and hepatic function exams, lactate dehydrogenase, and β2microglobulin), bone marrow biopsy, contrast-enhanced CT scans, and PET scans. Disease stage was defined by using Ann-Arbor staging criteria, and efficacy was evaluated according to the International Working Group (IWC) standard [12]. We used two prognostic indexes for patient risk stratification, including the MCL-International Prognostic Index (MIPI) that incorporates age, performance status, normalized LDH level, WBC level and the combined MCL-International Prognostic Index (MIPI-c) that incorporates MIPI with Ki-67 proliferation index [13, 14]. All patients received combination chemotherapy regimens. Tumor DNA samples were extracted from frozen lymph node biopsies at diagnosis. The above medical records, specimens, and study protocol conform to the ethical requirements of Peking University Third Hospital.
Whole-exome sequencing and data analysis
Genomic DNA was extracted from 16 MCL samples with DNeasy Blood & Tissue Kit (cat# 69504, QIAGEN, Germany) following the manufacturer’s protocol and sequenced the whole exome. We constructed genomic DNA libraries and capture the whole exome with the Ion AmpliSeq Exome RDY Kit (A29855) and sequenced the captured libraries on the Ion S5 XL genome analyzer.
Mutations (SNV and indel) were identified from 16 MCL samples using GATK Best Practices pipeline [15, 16]. Quality control of raw data was constructed with FastQC software (Version 0.11.2). The sequencing reads were aligned to the reference of human genome hg19 using the BWA software [17]. Indel realignment of each bam files and base quality score recalibration were constructed with GATK (version 3.2) without marked PCR duplicates. Mutations and indels were identified using VarScan (version 2.3.7) [18]. Mutations (SNV and indel) of each sample were annotated with ANNOVAR software.
To filter SNP and avoid false-positive calls, we used stringent filter criteria: (a) common SNP referenced in dbSNP138; (b) SNP with a frequency more than 1% in 1000 Genomes Project were removed; (c) SNP with a frequency more than 1% in esp6500 database (with about 6500 exomes) were removed; (d) SNP with a frequency more than 1% in EXAC database (with about 60,000 exomes) were removed. The quality of these mutations was manually reviewed with Integrated Genomics Viewer (IGV).
Pathway analysis and survival statistical analysis
The Reactome tool with default parameters was used for pathway analysis [19]. Enriched pathways of mutational genes shown in main figures were manually curated, only P < 0.05 pathways were shown.
The end point of the analyses was overall survival (OS), which was defined as the time from diagnosis to death (regardless of the cause) or date of the last follow-up evaluation. Univariate analyses of the prognostic value of clinical factors, pathological factor, and genetic mutations were done using Kaplan−Meier estimates and log-rank tests. We adjusted for clinical prognostic factors summarized in the quantitative MIPI and MIPI-c score. The adjusted index was calculated using the following method: (a) High index group: with TP53 or WHSC1 mutation or high-risk group of MIPI or high-risk/middle−high-risk group of MIPI-c; (b) Low index group: without TP53 or WHSC1 mutation and low-risk group of MIPI or low/low−middle-risk group of MIPI-c.
The data meet the assumptions and there is an estimate of variation within each group data. All reported P values are two-sided and descriptive. A statistical significance level of P < 0.05 was used.
Results
Clinical features of mantle cell lymphoma patients in the study
The clinical features of 16 MCL patients who underwent whole-exome sequencing are shown at Table 1. As previously reported, median age was 61.5 years (range, 43−84 years) with male-dominated, and all cases with evaluable staging information had advanced disease. Bone marrow (n = 14) was the most commonly involved extranodal site; five cases had leukemic presentation (cases 5, 7, 8, 11, 15). Splenic involvement was seen in nine patients, one of whom had splenic rupture during treatment, and three cases had gastrointestinal tract involvement. Conventional cytogenetic and FISH analyses were performed in our study. The majority of patients had cytogenetic aberration of t(11;14)(q13;q32) chromosomal translocation and one patient also had a deletion of chromosome 13 and chromosome 17. All patients received combination chemotherapy from among the following regimens: CHOP, R-CHOP, VR-CAP, R-HyperCVAD, R-lenalidomide, Ibrutinib with Rituximab and Bendamustine in initial therapy. One patient underwent autologous hematopoietic stem cell transplantation as consolidation therapy. The overall remission rate of the initial treatment was 68.8%, with complete remission rate and partial remission rate of 18.8 and 50% respectively, and 63.6% patients relapsed after initial treatment. At last clinical follow-up, 11 patients died, 5 were alive, median OS was 37.5 months (range 8−104 months). Kaplan−Meier analysis for OS estimated the 3-year and 5-year OS rates to be 68.8 and 38.2%, respectively.
The mutational spectrum of the mantle cell lymphoma cases
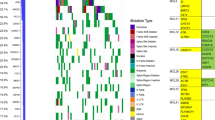
The MCL samples displayed a characteristic pattern of mutated genes. Among them, ATM, TP53, and WHSC1 had the top three mutation frequencies in the MCL cases, which contributed to 68.75% of all samples (11/15) (Fig. 1). A stop-gain was found in TP53 and WHSC1 in patient #11 with the second lowest OS (15 months). ATM had the highest mutation frequency in the MCL cases and has also been reported to have a high mutation frequency in previous studies on head and neck carcinomas [20, 21]. Twelve of 16 (75%) MCL samples have the translocation of t(11;14) (q13;q32) (Fig.1). ATM, TP53, WHSC1 gene mutations and t(11;14) (q13;q32) translocation contribute to 100% of all the 16 samples (Fig. 1). WHSC1 mutation observed in exon 18 has been recently detected in an acute lymphoblastic leukemia patient. The WHSC1 mutation in ALL seem to have an activating function because they increase the H3K36 methylation associated with a methylation decrease in H3K27 across the genome [22]. Bea et al., Zhang et al., and Rossi et al. reported WHSC1 mutation was in 10, 7, and 13% MCL patients respectively [23, 24], and the mutation rate of WHSC1 was 31.3% in our study which was higher than previous reported.
Three of 16 MCL samples (Fig. 1) had mutations in CCND1, which is located on the long arm of chromosome 11 (band 11q13, same with translocation arm). APC and CDH1 gene mutations were each observed in 2 of 16 MCL. CCDC15 gene mutations, which previous studies have shown genetic or epigenetic alterations in several CCDC genes in human cancers including MCL, were observed in 2 of 16 samples, of which a frame shift mutation was indentified [25,26,27]. S1PR1 mutation was observed in one MCL sample. ATRX and BRCA2, which are known as alternative lengthening of telomeres (ALT) and DNA repairing enzymes, respectively, were observed in two samples without ATM, TP53, WHSC1 mutations (Fig. 1). NOTCH3 and NOTCH2 mutations were observed in two and one MCL samples respectively.
The mutational signature of mantle cell lymphoma
At the exome level, the single base substitutions (SBSs) in 16 MCL samples exhibited a mutational signature with a dominant mutation pattern of C > T (equal to G > A) transitions (Fig. 2). All the SBSs were classified into six mutation types (C > A, C > G, C > T, T > A, T > C and T > G). The proportion of C > T mutations was 69%, while the T > C was 10% (Fig. 2a, b). The proportion of C > A, C > G, T > G, T > A was 8, 6, 4, 3% respectively (Fig. 2a, b). The mutational signature in individual MCL cases was also analyzed. The proportion of C > T mutations in individual MCL cases ranged from 50 to 90% (Fig. 2c). The proportion of T > C mutations in individual MCL cases ranged from 2 to 25% (Fig. 2c). The proportion of T > C mutations is relatively high in MCL3, MCL6, and MCL18 cases (Fig. 2c).
Pathway analysis of mutational genes
Pathway analysis was conducted on the mutated genes of the 16 MCL samples. The predominantly enriched pathways focused on the immune system, signal transduction, gene expression, cell cycle, and programmed cell death (Fig. 3a). Notably, ATM and TP53, which regulates transcription of DNA repair genes, were enriched. Cell cycle and cyclin D associated events in G1 are enriched. ATM, TP53, CDKN2A, BRCA2, CDH1 contribute to the cell cycle pathway. Immune system-related pathways, such as interferon gamma signaling, antigen processing, cross presentation, immunoregulatory interactions between lymphoid and non-lymphoid cells, and interleukin-2 signaling were also enriched pathways (Fig. 3b).
Prognostic factor analysis
We investigated the prognostic factors associated with MCL from clinical and pathologic data as well as genetic mutations. The results are shown in Table 2 and Fig. 4. High tumor proliferation index (Ki67 ≥ 30%) often indicates that the tumor is growing fast and the prognosis is poor. Although the risk stratification of MIPI combined with Ki67 had a good prognostic model, the Ki67 itself did not show prognostic significance in our study (P = 0.339).
The Kaplan–Meier curves for overall survival (OS) of mantle cell lymphoma patients. a−d The Kaplan–Meier curves for overall survival (OS) of mantle cell lymphoma patients in gene mutation status (TP53 and WHSC1 mutation), MIPI and MIPI-c, MIPI adjusted with gene (TP53 and WHSC1) mutation and MIPI-c adjusted with gene (TP53 and WHSC1) mutation. The log-rank test was used to compare Kaplan–Meier curves
To investigate if gene mutations offer prognostic value, we correlated genes with a high mutation rate including ATM, TP53, WHSC1, and CCND1 to OS. The results showed that patients with TP53 mutations had a poor prognosis with a 3-year survival rate of 40.0%, and were statistically significantly different from those patients without mutations in TP53 (P = 0.021; Fig. 4a). Although there was no significant difference between the two groups, the median survival time of patients with WHSC1 mutations was shorter than those without mutations (median survival time 17.0 months vs 47.0 months, P = 0.070; Fig. 4b). ATM and CCND1 mutations were not prognostic in our study (P = 0.552, 0.566).
We adjusted for clinical prognostic factors including MIPI and MIPI-c score by combining TP53, WHSC1 mutations (Table 3). The MIPI-adjusted OS hazard ratio (HR) for TP53 mutations was 3.427 (P = 0.028), whereas it was 4.047 (P = 0.040) for WHSC1 mutations. When adjusted for the MIPI-c score, the prognostic impact of TP53 mutations was modified by the inclusion of the MIPI-c index (HR unadjusted, 3.463; adjusted for MIPI-c, 4.758, P = 0.015); meanwhile, the prognostic impact of WHSC1 mutations on OS was also significant (P = 0.016).
Discussion
Despite advances in the development of clinical agents for treating MCL, treatment of MCL remains a challenge due to complexity and frequent relapse. The incorporation of conventional and novel diagnostic approaches such as genomic sequencing have helped improve understanding of the pathogenesis of MCL, and have led to development of specific agents targeting signaling pathways for MCL treatment [5, 6]. Whole-exome sequencing as a new diagnostic tool has been used to explore new targets in tumor diagnosis and treatment. For the first time, in our study, we examined the whole-exome sequencing of Chinese MCL patients. Our data identify the genetic heterogeneity underlying MCL and implicate a number of novel genes in the development of the disease.
Mutations identified in our study overlapped significantly with recently published studies of tumor exomes and transcriptomes, such as mutations in ATM, CCND1, TP53, WHSC1, and NOTCH2 [23, 24]. Similar to other lymphomas, our data indicate a striking mutational heterogeneity underlying MCLs, with relatively few genes mutated in 6−20% of the cases. Our work implicates other mutated genes, such as S1PR1, ATRX, BRCA2, rarely mentioned in MCL.
S1PR1 can promote tumor cell survival, invasion, anti-apoptosis, metastasis, and chemo-resistance in solid cancers [28, 29]. Bouska reported S1P/S1PR1-activated pathway can regulate lymphoma cell migration and associated with FL transformation [30]. The S1PR1 gene is located on chromosome 1p21, the mutation rate of S1PR1 gene was 6.3% in our study and Wu et al. reported S1PR1 mutation was 15.4% in MCL patients [31]. Whether the S1PR1 mutation is associated with extranodal invasion of MCL remains for further research, and may be potential therapeutic target in MCL patients. ATRX was known to be associated with alternative lengthening of telomeres (ALT) in gliomas [32]. ATRX mutations, previously reported in myelodysplastic syndromes, may act as a transcriptional co-factor and play an important role in the epigenetic regulation [33]. Mutations of BRCA2 gene that can inactivate BRCA pathway often occur in patients with breast and ovarian cancer [34, 35]. The BRCA pathway deficit causes an underlying deficiency in error-free DNA repair that increase the risk of leukemias and lymphomas, especially in MCL with t(11;14)(q13;q32) chromosomal translocation [36]. The ATRX and BRCA2 mutations are reported here in MCL for the first time. Notably, they were observed in samples without major mutations such as ATM, TP53, and WHSC1. The functions of ATRX/BRCA2 need further study in future.
MIPI and MIPI-c score are currently the most recognized prognostic models for MCL. However, these models lack prognostic factors in molecular biology, including genetic mutations. The prognostic value of TP53 deletions is controversial in the MCL literature, with reports either showing no or a deleterious prognostic value. However, recent studies showed that TP53 mutations are associated with significantly shorter OS and poor prognosis [37]. Compared with patients without TP53 mutations, TP53 mutations were associated with aggressive factors including age, higher serum lactate dehydrogenase, lymphocytosis, high-risk MIPI, complex karyotype, and higher occurrence of TP53 deletions [38]. Nordic Lymphoma Group study showed that TP53 was the only significant independent molecular marker that improved the prognostic value of MIPI [39]. A recent study suggests that younger MCL patients with deletions of CDKN2A and TP53 have poor prognosis, even when treated with immunochemotherapy, high-dose cytarabine, and stem cell transplant. It also suggests that TP53 deletions and CDKN2A have independent deleterious effects and should be considered for treatment decisions in addition to MIPI and Ki-67 index [40]. In our study, as previously reported, patients with TP53 mutations have a shorter survival time, and TP53 mutations have important prognostic implications in combination with MIPI and MIPI-c (P < 0.05).
An epigenetic modifier, WHSC1 encodes a histone 3 methyltransferase oflysine-36 (H3K36), WHSC1 mutation observed in exon 18 has been recently reported in a patient with acute lymphoblastic leukemia [23]. In our study, the mutation rate of WHSC1 was higher than previously reported in MCL. Patients with WHSC1 mutations had shorter survival time than those without mutations. Meanwhile, WHSC1 was the significant molecular marker that can improve the prognostic value of MIPI and MIPI-c score (P < 0.05). There is no corresponding report on the prognostic significance of WHSC1 mutations in MCL, and further expansion of the sample size is needed for validation.
In summary, with the first draft of the genomic landscape of MCL in Chinese patients now defined, we identified the genetic heterogeneity in MCL. The next step for the field should be to establish the functional consequence of the observed mutations. Our work underscores the importance of TP53 and WHSC1 mutations for the prognosis of MCL. Patients may benefit from mutation analysis of TP53 and WHSC1 at diagnosis, in addition to MIPI and MIPI-c score.
References
Ghielmini M, Zucca E. How I treat mantle cell lymphoma. Blood. 2009;114:1469–76.
Jares P, Colomer D, Campo E. Genetic and molecular pathogenesis of mantle cell lymphoma: perspectives for new targeted therapeutics. Nat Rev Cancer. 2007;7:750–62.
Leux C, Maynadie M, Troussard X, Cabrera Q, Herry A, Le Guyader-Peyrou S, et al. Mantle cell lymphoma epidemiology: a population-based study in France. Ann Hematol. 2014;93:1327–33.
Zhou Y, Wang H, Fang W, Romaguer JE, Zhang Y, Delasalle KB, et al. Incidence trends of mantle cell lymphoma in the United States between 1992 and 2004. Cancer. 2008;113:791–8.
Cheah CY, Seymour JF, Wang ML. Mantle cell lymphoma. J Clin Oncol. 2016;34:1256–69.
Vose JM. Mantle cell lymphoma: 2012 update on diagnosis, risk-stratification, and clinical management. Am J Hematol. 2012;87:604–9.
Jares P, Colomer D, Campo E. Molecular pathogenesis of mantle cell lymphoma. J Clin Invest. 2012;122:3416–23.
Jares P, Campo E. Advances in the understanding of mantle cell lymphoma. Br J Haematol. 2008;142:149–65.
Inamdar AA, Goy A, Ayoub NM, Attia C, Oton L, Taruvai V, et al. Mantle cell lymphoma in the era of precision medicine-diagnosis, biomarkers and therapeutic agents. Oncotarget. 2016;7:48692–731.
Lohr JG, Stojanov P, Lawrence MS, Auclair D, Chapuy B, Sougnez C, et al. Discovery and prioritization of somatic mutations in diffuse large B-cell lymphoma (DLBCL) by whole-exome sequencing. Proc Natl Acad Sci USA. 2012;109:3879–84.
Miranda NF, Georgiou K, Chen L, Wu C, Gao Z, Zaravinos A, et al. Exome sequencing reveals novel mutation targets in diffuse large B-cell lymphomas derived from Chinese patients. Blood. 2014;124:2544–53.
Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, et al. Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. NCI Sponsored International Working Group. J Clin Oncol. 1999;17:244.
Hoster E, Dreyling M, Klapper W, Gisselbrecht C, van Hoof A, Kluin-Nelemans HC, et al. A new prognostic index (MIPI) for patients with advanced-stage mantle cell lymphoma. Blood. 2008;111:558–65.
Hoster E, Rosenwald A, Berger F, Bernd HW, Hartmann S, Loddenkemper C, et al. Prognostic value of Ki-67 index, cytology, and growth pattern in mantle-cell lymphoma: results from randomized trials of the European Mantle Cell Lymphoma Network. J Clin Oncol. 2016;34:1386–94.
McKenna A, Hanna M, Banks E, Sivachenko A, Cibulskis K, Kernytsky A, et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010;20:1297–303.
Van der Auwera GA, Carneiro MO, Hartl C, Poplin R, Del Angel G, Levy-Moonshine A, et al. From FastQ data to high confidence variant calls: the Genome Analysis Toolkit best practices pipeline. Curr Protoc Bioinforma. 2013;43:11. 10 11-33
Li H, Durbin R. Fast and accurate long-read alignment with Burrows−Wheeler transform. Bioinformatics. 2010;26:589–95.
Koboldt DC, Zhang Q, Larson DE, Shen D, McLellan MD, Lin L, et al. Somatic mutation and copy number alteration discovery in cancer by exome sequencing. Genome Res. 2012;22:568–76.
Fabregat A, Sidiropoulos K, Viteri G, Forner O, Marin-Garcia P, Arnau V, et al. Reactome pathway analysis: a high-performance in-memory approach. BMC Bioinforma. 2017;18:142.
Ahmed M, Zhang L, Nomie K, Lam L, Wang M. Gene mutations and actionable genetic lesions in mantle cell lymphoma. Oncotarget. 2016;7:58638–48.
Cancer Genome Atlas N. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature. 2015;517:576–82.
Oyer JA, Huang X, Zheng Y, Shim J, Ezponda T, Carpenter Z, et al. Point mutation E1099K in MMSET/NSD2 enhances its methyltranferase activity and leads to altered global chromatin methylation in lymphoid malignancies. Leukemia. 2014;28:198–201.
Bea S, Valdes-Mas R, Navarro A, Salaverria I, Martin-Garcia D, Jares P, et al. Landscape of somatic mutations and clonal evolution in mantle cell lymphoma. Proc Natl Acad Sci USA. 2013;110:18250–5.
Zhang J, Jima D, Moffitt AB, Liu Q, Czader M, Hsi ED, et al. The genomic landscape of mantle cell lymphoma is related to the epigenetically determined chromatin state of normal B cells. Blood. 2014;123:2988–96.
Tamaki H, Sanda M, Katsumata O, Hara Y, Fukaya M, Sakagami H. Pilt is a coiled-coil domain-containing protein that localizes at the trans-Golgi complex and regulates its structure. FEBS Lett. 2012;586:3064–70.
Morra F, Luise C, Visconti R, Staibano S, Merolla F, Ilardi G, et al. New therapeutic perspectives in CCDC6 deficient lung cancer cells. Int J Cancer. 2015;136:2146–57.
Chen M, Ni J, Chang HC, Lin CY, Muyan M, Yeh S. CCDC62/ERAP75 functions as a coactivator to enhance estrogen receptor beta-mediated transactivation and target gene expression in prostate cancer cells. Carcinogenesis. 2009;30:841–50.
Spiegel S, Milstien S. Sphingosine 1-phosphate, a key cell signaling molecule. J Biol Chem. 2002;277:25851–4.
Selvam SP, Ogretmen B. Sphingosine kinase/sphingosine 1-phosphate signaling in cancer therapeutics and drug resistance. Handb Exp Pharmacol. 2013;216:3–27.
Bouska A, Zhang W, Gong Q, Iqbal J, Scuto A, Vose J, et al. Combined copy number and mutation analysis identifies oncogenic pathways associated with transformation of follicular lymphoma. Leukemia. 2017;31:83–91.
Wu C, de Miranda NF, Chen L, Wasik AM, Mansouri L, Jurczak W, et al. Genetic heterogeneity in primary and relapsed mantle cell lymphomas: impact of recurrent CARD11 mutations. Oncotarget. 2016;7:38180–90.
Paul Y, Mondal B, Patil V, Somasundaram K. DNA methylation signatures for 2016 WHO classification subtypes of diffuse gliomas. Clin Epigenetics. 2017;9:32.
Herbaux C, Duployez N, Badens C, Poret N, Gardin C, Decamp M, et al. Incidence of ATRX mutations in myelodysplastic syndromes, the value of microcytosis. Am J Hematol. 2015;90:737–8.
Kuchenbaecker KB, Hopper JL, Barnes DR, Phillips KA, Mooij TM, Roos-Blom MJ, Jervis S, et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA. 2017;317:2402–16.
Molina-Montes E, Perez-Nevot B, Pollan M, Sanchez-Cantalejo E, Espin J, Sanchez MJ. Cumulative risk of second primary contralateral breast cancer in BRCA1/BRCA2 mutation carriers with a first breast cancer: a systematic review and meta-analysis. Breast. 2014;23:721–42.
Friedenson B. The BRCA1/2 pathway prevents hematologic cancers in addition to breast and ovarian cancers. BMC Cancer. 2007;7:152.
Halldorsdottir AM, Lundin A, Murray F, Mansouri L, Knuutila S, Sundstrom C, et al. Impact of TP53 mutation and 17p deletion in mantle cell lymphoma. Leukemia. 2011;25:1904–8.
Dong HJ, Zhou LT, Fang C, Fan L, Zhu DX, Wang YH, et al. TP53 mutation is not an independent prognostic factor in patients with mantle cell lymphoma at advanced stage. Med Oncol. 2012;29:2166–73.
Nordstrom L, Sernbo S, Eden P, Gronbaek K, Kolstad A, Raty R, et al. SOX11 and TP53 add prognostic information to MIPI in a homogenously treated cohort of mantle cell lymphoma—a Nordic Lymphoma Group study. Br J Haematol. 2014;166:98–108.
Delfau-Larue MH, Klapper W, Berger F, Jardin F, Briere J, Salles G, et al. High-dose cytarabine does not overcome the adverse prognostic value of CDKN2A and TP53 deletions in mantle cell lymphoma. Blood. 2015;126:604–11.
Acknowledgements
The authors thank the patients and their families who contributed to this study. The authors would also like to acknowledge Professor Cuiling Liu in Department of Pathology, Peking University Third Hospital.
Funding
This work was funded by China Health Promotion Foundation, CHPF-zlkysx-001. Employees of the funding source were involved in the collection and assembly of data, genetic sequencing, performing statistical analysis, analyzing and interpreting data, and drafting, reviewing, and approving the manuscript, as reflected in the author contributions statement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Yang, P., Zhang, W., Wang, J. et al. Genomic landscape and prognostic analysis of mantle cell lymphoma. Cancer Gene Ther 25, 129–140 (2018). https://doi.org/10.1038/s41417-018-0022-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41417-018-0022-5
- Springer Nature America, Inc.
This article is cited by
-
Genetic and prognostic analysis of blastoid and pleomorphic mantle cell lymphoma: a multicenter analysis in China
Annals of Hematology (2024)
-
Beyond Bruton’s tyrosine kinase inhibitors in mantle cell lymphoma: bispecific antibodies, antibody–drug conjugates, CAR T-cells, and novel agents
Journal of Hematology & Oncology (2023)
-
A sumoylation program is essential for maintaining the mitotic fidelity in proliferating mantle cell lymphoma cells
Experimental Hematology & Oncology (2022)
-
Complex genetic and histopathological study of 15 patient-derived xenografts of aggressive lymphomas
Laboratory Investigation (2022)
-
Progress in molecular feature of smoldering mantle cell lymphoma
Experimental Hematology & Oncology (2021)