Abstract
Oral rehabilitation of head and neck cancer patients is an integral component of the care pathway. Maxillectomy procedures can cause significant defects, such as oronasal fistulas, loss of support for the cheek and lip, aesthetic defects in the middle third of the face and functional impairments. Orofacial rehabilitation plays a fundamental role in restoring aesthetics and functional capabilities, such as speech, mastication and deglutition.
Rehabilitation of maxillectomy patients poses a challenge for both clinicians and patients. This paper utilises case examples to demonstrate the treatment options for the oral rehabilitation of these patients. We will summarise the treatment pathways for conventional obturators, delayed (secondary) implant retained fixed rehabilitation following composite free flap and early rehabilitation using a zygomatic implant perforated flap technique. This paper aims to highlight the challenges in treatment planning and the importance of a multidisciplinary approach in improving patient outcomes.
Key points
-
Maxillectomy defects can have a significant impact on both psychological and functional capabilities.
-
Several rehabilitation options exist for these patients, with various considerations as to the most appropriate option.
-
This paper provides a summary of the rehabilitation options and the pathways for managing these patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Head and neck cancer (HNC) is the sixth most common cancer in the world, and includes cancer of the oral cavity, pharynx, larynx and oropharynx.1 Overall, 1-5% of malignant tumours of the oral cavity relate to the hard palate.2 The most common type of cancer of the oral cavity is squamous cell carcinoma (SCC); with 62% of oral SCC cases diagnosed at an advanced stage.2 In patients with a maxillary malignancy, radical treatment modalities commonly include surgical ablation, with or without reconstruction. Adjuvant radiotherapy or chemoradiotherapy are also commonly utilised. Maxillectomy procedures may result in orofacial defects, such as oronasal/oroantral communications, loss of lip support, aesthetic defects in the middle third of the face and functional impairments. These can significantly affect quality of life and can result in a substantial psychological impact.3 Following major head and neck surgery, 78% of patients experience severe difficulties with mastication and 74% of individuals with HNC report at least one unmet need, most commonly related to 'oral and eating problems' after treatment.4
Following ablative surgery for malignancy of the maxilla, surgical reconstruction of the resultant defect is based on the principles of restoring function and form, the patient's fitness for a prolonged general anaesthetic and suitability for microvascular free flap surgery.
Restorative dental rehabilitation plays a role in restoring aesthetics and functional capabilities. Treatment planning requires consideration of local and patient factors to ensure the most appropriate method of rehabilitation is utilised. Restorative management may be, in many respects, driven by the plan for a surgical reconstruction. Local factors include the tumour size and extent, planned surgical reconstruction, remaining teeth and their prognosis and the quality and quantity of available bone, along with the possible requirement for adjuvant radiotherapy.5 Patient-related factors include their general health, social support and dental health.6
This paper explores the prosthetic rehabilitation options available for patients with a range of maxillary defects. The aim is to provide an update on the treatment planning process for patients who present with maxillary tumours. We highlight the restorative and surgical challenges using cases to explore strategies to optimise patient outcomes.
Surgical and reconstructive planning
Effective communication between the restorative team and the surgical team is of the utmost importance. When planning dental implants, a discussion is required as to whether the patient is likely to be managed with surgery alone or adjuvant treatment. Individuals with a stage III or IV cancer7 are more likely to require adjuvant radiotherapy.8 A treatment planning discussion outlining the surgical objectives, extent of resection and the appropriateness for the various prosthetic rehabilitations is essential to ensure effective teamwork between the restorative and surgical teams.
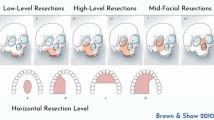
The Brown classification of maxillary defects9 (Fig. 1) is a useful guide to the most appropriate method of reconstruction, which is then further tailored to the patient's individual medical, functional and psychological needs.
Brown classification of maxillary defects describing the vertical and horizontal components. Image courtesy of Colin Sullivan. I) Maxillectomy not causing an oronasal fistula. II) Not involving the orbit. III) Involving the orbital adnexae with orbital retention. IV) With orbital enucleation or exenteration. V) Orbitomaxillary defect. VI) Nasomaxillary defect. a) Palatal defect only not involving the dental alveolus. b) Less than or equal to ½ unilateral. c) Less than or equal to ½ bilateral or transverse anterior. d) Greater than ½ maxillectomy alveolar defect without oro-nasal or oro-antral fistulae9
Pre-treatment restorative assessment
Restorative dentists are core members of the head and neck multidisciplinary team (HNMDT) and play a role in the improvement and maintenance of oral and dental health following treatment for HNC.4 Current guidance highlights the importance of a pre-treatment restorative dental assessment, which should be carried out as early as possible.4,10 The aims of a pre-treatment restorative assessment are outlined in Table 1.
Initial restorative assessment
Prior to surgical resection, a thorough oral and dental assessment should be undertaken. As with any dental examination, a thorough clinical history is crucial. The patient's oral hygiene regime, diet and dental, medical and social histories are all important factors when formulating a treatment plan. In addition, this can enable the clinician to ascertain the patient's concerns, expectations and likely engagement with dental services.
Within the examination itself, there are various factors to consider in addition to those assessed routinely. It is important to gain baseline records of mouth opening and xerostomia as radiotherapy may cause these to deteriorate further, increasing caries risk and rendering future dental treatment more difficult.
Assessment of edentulous sites aids planning of the prosthetic options and the feasibility of primary implant placement (that is, placement of dental or zygomatic implants during primary surgery for HNC). Similarly, assessment of the tumour site and size can indicate the likely resection margins, which will impact directly on the anatomy of the denture bearing tissues and therefore the retention and stability of a denture.
Pre-operative impressions enable joint planning with the dental laboratory, digital planning team and surgical team. Cone beam computed tomography (CBCT) scans can be utilised to aid implant planning. Where zygomatic implants are being considered, it is important to ensure the CBCT scan extends to the zygomatic arches and buttress. A stereolithographic print in the form of a bone model can also be provided to aid planning of implant placement. Alternatively, assessment of the scan with 3D multi-plane reformatting allows detailed assessment of the required implant length, provided the prosthetic envelope can be visualised either using a radiographic stent or by assessing the position of the teeth before surgery.
The restorative plan will be greatly influenced by the intended surgical management and reconstruction. Collaborative planning between the oral and maxillofacial and restorative teams, as well as other members of the HNMDT, is essential.
Reconstruction and rehabilitation options
The options for reconstruction are a prosthetic obturation or flap reconstruction (local, regional or microvascular free flap). Both of these options can be supplemented with dental or zygomatic implants placed at primary surgery or in a delayed manner.
While the optimal treatment modality is based on individual patient characteristics, it is often recognised that certain treatments are more appropriate for different tumour sizes.
Smaller defects can be obturated or reconstructed with a fasciocutaneous free flap.9,11 Moderate-sized defects (Class IIa and IIb defects) can be adequately reconstructed with an obturator or with surgery. Where the defect site is small, this could be treated with a local flap, while larger defects may require a fasciocutaneous flap. In posterior Class IIb defects, a composite reconstruction is not necessary, as ipsilateral incisors and canines can provide support for a partial denture/obturator. In Class IIc defects, a bone flap may be needed to compensate for loss of alar support.9 Defects that are horizontally or vertically larger rely more on surgical reconstruction as reconstruction solely with an obturator can impact negatively on function and quality of life (QOL).12 A hybrid approach which combines the best features of flap reconstruction and implant-supported prosthesis (the zygomatic implant perforated [ZIP] flap) has been described by Butterworth and Rogers in 2017.13 This approach is being increasingly utilised for the early rehabilitation of patients with larger maxillary defects in the experience of the authors.
Class III defects can be difficult to satisfactorily reconstruct. There is little role for obturation in these cases as orbital and anterior cheek support is lost, along with the dental arch. In these cases, free flap reconstruction is most appropriate.9
It has been suggested that those with larger defects have improved QOL when rehabilitated with a microvascular free flap, while those with smaller defects have similar QOL with either free flap or obturator.12 This paper was, however, presented before developments in primary implant placement into composite free flaps and before the description of the ZIP flap pathway and arguably, no longer represents outcomes with the range of treatment modalities now available. The majority of QOL concerns relate to chewing, speech and swallowing.14 Tooth replacement can clearly impact significantly on these in a way that flap reconstruction alone cannot. Part of the decision-making process should therefore consider how to optimise oral health-related QOL and planning the most appropriate method of oral/dental rehabilitation should be part of the overall plan for primary surgery.
The treatment planning considerations for each of these options is outlined further in the sections below with the support of case examples. The pathways for each of these options is summarised in Figure 2.
No flap - rehabilitation with obturator
Historically, patients were rehabilitated using an obturator prosthesis. While developments in surgical techniques have resulted in a wider use of microvascular free tissue transfer for reconstruction, the use of obturators is still an important technique for rehabilitation. Obturators are prostheses used to recreate an oronasal seal and maintain the integrity of the oral and nasal components following congenital or acquired disease. They are predominantly used in maxillectomy cases where the general medical status does not allow for larger reconstruction procedures due to increased surgical morbidity or risk. Throughout the rehabilitation process, patients will have several prostheses constructed. These are outlined in Table 2.
Obturators have the advantage of quickly providing the patient with a replacement for missing teeth while restoring cheek support with the prosthesis.15 This has been shown to significantly improve patient QOL16 and has been shown to significantly improve speech intelligibility, even at the interim obturator stage.17 They have the additional benefit of simplifying oncological surveillance. However, their success is highly dependent on defect size, position, location and the health of the abutment teeth. Where patients have a large defect with fewer teeth, an implant-retained obturator could be utilised if patients already have missing teeth distant from the defect site and the quality and quantity of remaining alveolar bone allows.3
Obturators are not without their difficulties with regard to fit, retention and comfort. In more complex defects, it will be challenging to gain an effective oronasal seal to prevent transgression of fluid from the mouth to the nose. Obturators can be difficult to tolerate due to changes in oral anatomy, contact of the obturator bung against the delicate respiratory epithelium of the nasal mucosa, oral dryness and fragility of irradiated tissues.13 Along with their physiological impact, there can also be a psychological impact of retaining a maxillectomy defect.4
While obturators have their utility, patient satisfaction decreases if more than one-quarter of the hard palate or one-third of the soft palate is resected.18
Advances in surgical options, such as the use of zygomatic implants and the ZIP flap, have introduced treatment options that afford improved QOL and functional outcomes compared to the traditional prosthetic obturator. The use of prosthesis alone may now no longer considered to be the 'gold-standard' management, except in very small localised Level 1b maxillectomy defects.13
Clinical workflow
Following the HNMDT discussion, treatment decision regarding the management of the cancer is agreed. A rehabilitation pathway will be guided by the surgical and restorative teams to determine the restorative pathway and inform restorative decisions for oral and dental 'pre-habilitation'. Where prosthetic rehabilitation involves a removable prosthesis, a surgical obturator would be required. In both dentate and edentulous patients, retention of the prosthesis initially requires some form of screw retention into the residual palate. To improve the initial post-surgical oronasal and peripheral seal, the surgical obturator may be relined with either silicone putty or impression compound.19 In addition to this, a special tray is required to allow for an intra-operative post-resection impression of the defect to construct an interim obturator.
Case 1
A patient with T3N0M0 SCC of right maxilla managed with a partial maxillectomy and adjuvant radiotherapy in 2009 (Fig. 3a). The patient was initially provided with a maxillary magnet-retained obturator (Fig. 3b). Following recent exfoliation of the 13, the patient was re-referred for provision of a new obturator (Figures 3c and 3d).
Complications
One concern with obturators is the weight of the prosthesis. Where there is a significant defect, the weight can act to dislodge the prosthesis. It is therefore important to minimise the weight as much as possible. This can be achieved with use of a hollow bulb.19
Trismus as a consequence of surgical resection of muscle attachments and radiotherapy-induced fibrosis can make construction of obturators more complex and lead to difficulty with obturator insertion. In addition, the effect of radiotherapy on the salivary glands may lead to xerostomia, which can result in soreness of the fragile irradiated tissues.4 Where a total maxillectomy has been performed, the obturator has no opportunity to gain support from the remaining tissues and therefore, it is not common practice for a total maxillectomy to be rehabilitated by a removable obturator alone.
In contrast to conventional dentures, obturators should be worn at night for the first six months following resection, especially during radiotherapy treatment, as wound contraction can occur within hours of removal.4 This necessitates impeccable oral and denture hygiene to minimise the risks associated with wearing a removable prosthesis. The obturator should be removed for oral and prosthesis hygiene. In this instance, cleaning should be undertaken using salt water or chlorhexidine gluconate.20 Where obturator removal is feasible for the patient, they should be removed following meals and cleaned with soapy water. Where persistent candidiasis is present, it may be advisable to consider relining with a tissue conditioner including nystatin.20
The maxillary defect itself also requires cleaning to prevent irritation to the soft tissues. This can be performed with chlorhexidine or warm salt water mouth rinses. Soft polygonal sponges can be used in conjunction with these. Alternatively, a regime similar to that for nasal douching can be utilised. This involves a solution of salt, bicarbonate of soda and warm water which is then circulated passively through the nose to irrigate the maxillary defect.
Soft tissue flap
In cases where the patient has a dentition that is suitable to support a prosthesis, soft tissue flaps may be indicated. In patients with missing teeth, the altered anatomy associated with soft tissue flaps can create an environment that is not conducive for an optimal conventional prosthesis. The thickness and compressibility of the soft tissue flaps often provide an unstable foundation for a prosthesis and may necessitate further 'debulking' procedures.
Composite flap
Composite flaps are able to provide support for the facial soft tissues, as well as bone for primary or delayed implant insertion to facilitate dental rehabilitation.21 Implant placement can be performed at the time of primary surgery thus limiting the number of surgical procedures and providing sufficient time for wound healing and osseointegration before radiotherapy. Planning for implant placement should ideally be incorporated into the patient-specific bone fixation plate design process, when this technology is utilised. This facilitates the preparation of cutting guides and implant placement guides to allow the placement of the implants before the free flap pedicle is divided before transfer to the recipient site.
Delayed implant placement may be preferred if there are concerns about the risk to flap viability associated with primary placement or where radiotherapy is unlikely to be part of the patient's treatment pathway. Concerns with primary implant placement into the composite flap may include compromise to the blood supply directly through stripping of the soft tissue attachments to the bone flap. A delayed rehabilitation approach allows for a more prosthodontically-driven planning of the dental implant positions and identifies patients with minimal risk factors, therefore improving implant survival.22 A significant proportion of patients will require post-operative radiotherapy; therefore, implant placement may be significantly delayed or even avoided due to the side effects of radiotherapy, such as osteoradionecrosis or trismus. Additionally, implant failure has been found to be significantly higher in immediately placed implants compared to delayed implant placement in free vascularised composite grafts.23 Case 2 shows how this delayed implant placement can be utilised to provide a fixed prosthesis.
Case 2
A 16-year-old patient with a diagnosis of myofibroblastic sarcoma (T2N0M0) (Fig. 4a). The patient underwent surgery to resect the tumour (Fig. 4b). She had a definitive cobalt-chrome obturator six months after resection (Fig. 4c). The defect was subsequently reconstructed with a composite radial forearm free flap (Fig. 4d). Due to inadequate bone for implant placement, further surgery was undertaken to debulk the flap and provide an autogenous bone graft using iliac crest before implant placement (Fig. 4e). Missing teeth were replaced with a definitive abutment level implant supported fixed bridge to restore function and aesthetics (Figures 4f and 4g).
Complications
Implant placement below the thick and mobile lining of a skin paddle can lead to suboptimal soft tissue profile around abutments, resulting in increased risk of soft tissue overgrowth, peri-implantitis and periodontal pocketing.23,24 This can be challenging for the rehabilitation team and often corrective soft tissue procedures are required. This may include flap debulking, removing skin and muscle leaving only periosteum over the alveolar crest and dressing with an acrylic plate and a tissue conditioner until the tissue re-granulates and heals by secondary intention.25 Some of these complications can be attributed to the lack of attached keratinised mucosa which is conducive to peri-implant mucosal health.23,24 In some instances, soft tissue grafting procedures may be beneficial to reduce the risk of soft tissue overgrowth (for example, free gingival grafts), although there is limited published literature to support this.26
Implant survival in autogenous bone grafts is approximately 85%.23 This is lower than implants placed into native bone in HNC patients.23,26 As previously discussed, radiotherapy following primary surgery is an important consideration when placing implants. Survival of dental implants placed into irradiated bone is reported to be lower than in non-irradiated bone (70-99%).26,27 This is reported to be dose dependent, with higher failures rates reported when radiotherapy doses to the implant site exceed 66 Gy.27
Zygomatic implant perforated flap
ZIP flaps involve reconstruction of the maxillary defect with a soft tissue flap and concurrent placement of osseo-integrated zygomatic-oncology implants for support of dental prosthesis. The free flap is perforated following insetting of the flap to facilitate access to the implant fixture head. This provides effective maxillary dental rehabilitation in a relatively rapid manner.13 The ability to achieve good primary stability by utilisation of distant bone from the zygoma facilitates early prosthetic loading.21 The ability to place implants at the time of primary surgery is advantageous, as this allows placement when access is optimal before post-treatment scarring and fibrosis and can thus allow for osseointegration before the deleterious effects of radiotherapy.21,28
In addition, these implants provide in-defect support and retention which cannot be achieved through conventional dental implants, allowing the patient to function on the defect side without the prosthesis being displaced superiorly into the maxillectomy cavity.21 When multiple zygomatic implants are placed, these are often connected with a rigid connector, resulting in better force distribution and sharing of the functional loads.29 The reported survival of zygomatic implants used to restore the dentition in oncology patients is 77-100%.30
Clinical workflow
The pre-surgical planning should involve construction of a surgical implant guide, which can be based on pre-surgical tooth positions or an idealised wax up if tooth positioning/shape is not optimised. A special tray can also be constructed based on planned implant placement sites to facilitate abutment level impressions to be taken at the time of surgery.
A CBCT scan facilitates the assessment of anatomy and planning of optimal implant sizes.
Following implant placement and flap perforation, an abutment level impression is taken along with an occlusal/incisal reference using the wax prosthetic tooth set-up. Verification of implant position can be carried out at the time of surgery using a light cure acrylic resin. In the experience of the authors, the continued contraction of light-cured acrylic between construction of a verification jig and pouring of the master cast can lead to reduced working cast accuracy and thus may lead to poorer fit of prostheses. Alternatively, verification can be carried out at an initial outpatient appointment alongside a trial tooth set-up and avoids delay to the fit of provisional implant-supported restoration.
After completion of intra-operative records, a clear polyethene washer can be secured over the flap with the use of a wide abutment cap with sufficient undercut to prevent swelling in the soft tissue flap from covering the abutments during the healing period.28 Outpatient appointments should ideally be carried out in the 2-3-week period post-operatively, before the commencement of any adjuvant radiotherapy.
Case 3
An 84-year-old patient with T4aN2bM0 SCC left maxilla. The patient was seen in the restorative department before undergoing a partial maxillectomy and reconstruction with an anterolateral free flap (AFF). In this case, two Zygex implants were placed on the left, two Zygan implants on the right and three conventional dental implants in the mandible (Fig. 5). The pronounced curvature of the zygomatic arches necessitated implants with a smooth central collar. These were positioned palatally to compensate for the anatomy of the zygoma. A second operation was carried out two weeks later to perforate the AFF, place healing abutments and place a perforated thermoplastic silastic sheet. It is preferable to delay perforation of the AFF due to the increased risk to small perforating vessels. Healing abutments of 5 mm height were placed on the oncology implants to facilitate flap retraction above the zygomatic implant fixture heads. Impression copings were then seated and splinted using light-cured acrylic. A small piece of polyvinyl mouthguard material was utilised to stop the flap covering the abutments during the healing period. The patient was initially provided with a fixed interim prosthesis and a definitive implant bar retained overdenture was provided on completion of radiotherapy.
Complications
Implant rehabilitations are associated with several different types of complication which are typically grouped into biologic and technical complications.
Lan et al. (2021) performed a systematic review and meta-analysis of atrophic maxillas restored with four zygomatic implants. They reported that biologic complications were more common with a 12% prevalence of sinusitis and 10% prevalence of local infection. Also, 11% of implants were reported to be malpositioned and 5% of cases were associated with 'prosthetic complications'.31
The risk for complications may be higher in oncology cases due to the reduced availability for bone volume to support the crestal portion of the zygomatic implant and the differences in the soft tissue connection for implants perforating soft tissue flaps (particularly where this a lack of underlying support from bone).
Chow reports the prevalence of sinusitis and rhinosinusitis complications to be 7.4%, with some cases requiring further surgery to the sinus to manage persistent inflammation.28
As with implants placed into composite flaps, the soft tissues around zygomatic implants are also susceptible to inflammation and therefore, it is crucial to ensure a prosthetic design which facilitates adequate oral hygiene.28
Zygomatic implants can be at a greater risk of complications associated with unfavourable loading due to the long lever arm associated with the use of a distant site for osteointegration. Consequently, in certain cases, it may be more appropriate to delay loading of the implants to reduce the risk of implant failure (for example, in cases where unfavourable loads would be unavoidable due to a deep overbite).
While it is possible to immediately load zygomatic implants, the importance of monitoring microvascular flaps in the immediate post-operative period may lead to a delay in prosthodontic rehabilitation until the patient is fit to attend an outpatient restorative clinic.13 However, with the use of invasive flap monitoring adjuncts, this is not a concept that should be completely excluded.32
Conclusion
Treatment planning always requires consideration of advantages and disadvantages of all rehabilitation options while taking into account patient expectations in the context of their cancer diagnosis and the treatment required to manage this. The multidisciplinary team must balance the risk of recurrence with the benefits afforded by reconstruction of an oronasal seal with a free flap. Obturators may be preferable in cases with a poor prognosis; the provision of an implant-retained prosthesis may need to be avoided in such instances in order to reduce the burden of treatment for this group of patients.
Both open defects and surgically reconstructed defects present challenges when providing a conventional prosthodontic rehabilitation. Sites rehabilitated using dental implants may also be challenging to restore due to limitations in the availability of adequate bone following ablative surgery, post-operative radiotherapy changes and soft tissue concerns, such as tissue bulk/position or inadequate vestibule depth. Zygomatic implants may provide adequate remote anchorage for support and retention of a prostheses with high patient acceptance and quality of life outcomes.33
The challenging nature of these prosthetic rehabilitations highlights the importance of early planning on the multidisciplinary team and good communication with the patient and laboratory.
References
Wells M, Cunningham M, Lang H et al. Distress, concerns and unmet needs in survivors of head and neck cancer: a cross-sectional survey. Eur J Cancer Care (Engl) 2015; 24: 748-760.
Tirelli G, Rizzo R, Biasotto M et al. Obturator prostheses following palatal resection: clinical cases. Acta Otorhinolaryngol Ital 2010; 30: 33-39.
dos Santos D M, de Caxias F P, Bitencourt S B, Turcio K H, Pesqueira A A, Goiato M C. Oral rehabilitation of patients after maxillectomy. A systematic review. Br J Oral Maxillofac Surg 2018; 56: 256-266.
The Royal College of Surgeons of England. The Oral Management of Oncology Patients Requiring Radiotherapy, Chemotherapy and/or Bone Marrow Transplantation: Clinical Guidelines. 2018. Available at https://www.rcseng.ac.uk/-/media/files/rcs/fds/publications/rcs-oncology-guideline-update--v36.pdf (accessed May 2022).
Dexter W S, Jacob R F. Prosthetic rehabilitation after maxillectomy and temporalis flap reconstruction: a clinical report. J Prosthet Dent 2000; 83: 283-286.
Barclay C W, Foster E C, Taylor C L. Restorative aspects of oral cancer reconstruction. Br Dent J 2018; 225: 848-854.
Brierley J, Gospodarowicz M, Wittekind C. TNM Classification of Malignant Tumours. 8th ed. New Jersey: Wiley-Blackwell, 2020.
Won H S, Chun S H, Kim B-S et al. Treatment outcome of maxillary sinus cancer. Rare Tumors 2009; DOI: 10.4081/rt.2009.e36.
Brown J S, Shaw R J. Reconstruction of the maxilla and midface: Introducing a new classification. Lancet Oncol 2010; 11: 1001-1008.
Butterworth C, McCaul L, Barclay C. Restorative dentistry and oral rehabilitation: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 2016; DOI: 10.1017/S0022215116000414.
Wang W H, Zou Z R, Xu B, Wang W Q, Shen S Y. Maxillary Reconstruction Using Submental Artery Island Flap and Sagittal Mandibular Ramus/Coronoid Process Graft Pedicled With Temporalis Muscle. J Oral Maxillofac Surg 2017; DOI: 10.1016/j.joms.2017.06.035.
Moreno M A, Skoracki R J, Hanna E Y, Hanasono M M. Microvascular free flap reconstruction versus palatal obturation for maxillectomy defects. Head Neck 2010; 32: 860-868.
Butterworth C J, Rogers S N. The zygomatic implant perforated (ZIP) flap: a new technique for combined surgical reconstruction and rapid fixed dental rehabilitation following low-level maxillectomy. Int J Implant Dent 2017; DOI: 10.1186/s40729-017-0100-8.
Rogers S N, Lowe D, Fisher S E, Brown J S, Vaughan E D. Health-related quality of life and clinical function after primary surgery for oral cancer. Br J Oral Maxillofac Surg 2002; 40: 11-18.
Ali R, Altaie A, Nattress B. Rehabilitation of oncology patients with hard palate defects. Part 1: The surgical planning phase. Dent Update 2015; 42: 326-328.
Breeze J, Rennie A, Morrison A et al. Health-related quality of life after maxillectomy: obturator rehabilitation compared with flap reconstruction. Br J Oral Maxillofac Surg 2016; 54: 857-862.
Dalkiz M, Dalkiz A S. The Effect of Immediate Obturator Reconstruction after Radical Maxillary Resections on Speech and other Functions. Dent J (Basel) 2018; DOI: 10.3390/dj6030022.
Ali R, Altaie A, Nattress B. Rehabilitation of oncology patients with hard palate defects Part 2: Principles of obturator design. Dent Update 2015; 42: 428-434.
Shah D, Meenakshi A. The obturator prostheses for maxillectomy. SRM J Res Dent Sci 2012; 3: 193-197.
Kumar N. Updated clinical guidelines on the oral management of oncology patients. Facult Dent J 2019; 10: 62-65.
Butterworth C J. Primary vs secondary zygomatic implant placement in patients with head and neck cancer - A 10-year prospective study. Head Neck 2019; 41: 1687-1695.
Bidra A S. Surgical and prosthodontic consequences of inadequate treatment planning for fixed implant-supported prosthesis in the edentulous mandible. J Oral Maxillofac Surg 2010; 68: 2528-2536.
Laverty D P, Kelly R, Addison O. Survival of dental implants placed in autogenous bone grafts and bone flaps in head and neck oncology patients: a systematic review. Int J Implant Dent 2018; DOI: 10.1186/s40729-018-0131-9.
Rohner D, Bucher P, Hammer B. Prefabricated fibular flaps for reconstruction of defects of the maxillofacial skeleton: planning, technique, and long-term experience. Int J Oral Maxillofac Implants 2013; DOI: 10.11607/jomi.te01.
Meloni S; Tallarico M; Canullo L; De Riu G; Massarelli O. Periimplant soft-tissue management in patients with fibula free flap reconstruction: Case series and description of a new technique. J Oral Sci Rehabil 2016; 2: 26-30.
Patel J, Antov H, Nixon P. Implant-supported oral rehabilitation in oncology patients: a retrospective cohort study. Br J Oral Maxillofac Surg 2020; 58: 1003-1007.
Burgess M, Leung M, Chellapah A, Clark J R, Batstone M D. Osseointegrated implants into a variety of composite free flaps: A comparative analysis. Head Neck 2017; 39: 443-447.
Chow J. Zygomatic Implants: Optimization and Innovation. Switzerland: Springer, 2020.
Chrcanovic B R, Albrektsson T, Wennerberg A. Survival and Complications of Zygomatic Implants: An Updated Systematic Review. J Oral Maxillofac Surg 2016; 74: 1949-1964.
Hackett S, El-Wazani B, Butterworth C. Zygomatic implant-based rehabilitation for patients with maxillary and mid-facial oncology defects: A review. Oral Dis 2021; 27: 27-41.
Lan K, Wang F, Huang W, Davó R, Wu Y. Quad Zygomatic Implants: A Systematic Review and Meta-analysis on Survival and Complications. Int J Oral Maxillofac Implants 2021; 36: 21-29.
Kanatas A, Ho M W. Monitoring of free flaps and reconstruction for oral cancer. Br J Oral Maxillofac Surg 2018; DOI: 10.1016/j.bjoms.2018.01.008.
Salvatori P, Mincione A, Rizzi L et al. Maxillary resection for cancer, zygomatic implants insertion, and palatal repair as single-stage procedure: report of three cases. Maxillofac Plast Reconstr Surg 2017; DOI: 10.1186/s40902-017-0112-6.
Author information
Authors and Affiliations
Contributions
Olivia Barraclough, Jaymit Patel, Stephanie Milne, Michael W. Ho and Zaid Ali have all equally contributed to writing and editing this manuscript.
Corresponding author
Ethics declarations
None of the authors have any conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Barraclough, O., Patel, J., Milne, S. et al. Pathways for the rehabilitation of resection defects in the maxilla. Br Dent J 232, 783–789 (2022). https://doi.org/10.1038/s41415-022-4342-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-022-4342-3
- Springer Nature Limited