Abstract
Introduction Head and neck cancer (HNC) patients should receive a dental assessment at an appropriate time before commencing radiotherapy (RT), to prevent complications such as osteoradionecrosis (ORN) if extractions are required. A recent orthopantomogram radiograph (OPG) is part of this assessment.
Aim To compare the delivery of pre-RT dental assessment at the Regional Oncology Centre against national guidelines in regard to OPG assessments and timing of extractions.
Materials and methods A consecutive cohort of patients treated curatively were selected within two timeframes (January to March 2018 and January to March 2019) using multidisciplinary team records at Liverpool University Hospital. Patient notes, x-ray images and records were examined.
Results In total, 145 patients were identified. Eighty-nine percent (129) had an OPG radiograph and 72% (104) had a pre-RT dental assessment. Oral and laryngeal sites had the highest number of missed assessments. Altogether, 54 patients had dental treatment, with 47 undergoing extractions. Extractions were completed a median 13 days before RT started. By November 2020, no patients had been diagnosed with ORN.
Conclusions Three-quarters of patients received a pre-RT assessment but there is scope for improvement. OPGs should be part of initial HNC staging and referral to Regional Oncology Centre dental services should be made as part of the pre-RT workup.
Key points
-
All patients should receive a pre-radiotherapy dental assessment, regardless of being dentate or edentulous and irrespective of the site of the primary tumour.
-
Effective, timely integration of dental assessment into the patient pathway before commencing radiotherapy is one of the ways to reduce the risk of post-extraction osteoradionecrosis.
-
Including an orthopantomogram radiograph with head and neck cancer staging scans, together with referral to the dental services within regional oncology centres as part of the pre-radiotherapy workup, should improve rates of pre-radiotherapy dental assessments.
Similar content being viewed by others
Introduction
Radiotherapy (RT) has been used as a primary therapy and also as an adjunct to surgery for treatment of head and neck cancers (HNC).1 A significant risk to patients undergoing radiotherapy to the head and neck region is osteoradionecrosis (ORN).1,2,3
As part of a HNC patient treatment pathway, patients should receive a dental assessment before commencing RT, to assess dental health and determine whether any teeth of poor prognosis require extraction.2,4 To avoid the development of ORN early after treatment, extractions should take place with sufficient time for healing before RT is started. Such extractions hopefully reduce the likelihood of ORN following any future extractions. This dental assessment should be completed by a suitably qualified dental practitioner.4
Although the majority of oral and maxillofacial surgeons practicing in the United Kingdom complete a Bachelor of Dental Surgery as part of their training, the pre-treatment dental assessment should be completed by a separate, dedicated, suitably-qualified dentist.2 The pre-treatment dental assessment comprises identifying teeth of poor prognosis requiring extraction, providing an alert card to inform future clinicians of the risk of ORN, a prescription for 5000 ppm fluoride toothpaste, oral hygiene instruction and reinforcement of the importance of regular dental examinations.5,6 For patients without a dentist, one will be contacted on their behalf if necessary.
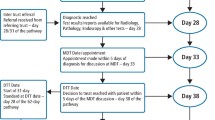
The British Association of Head and Neck Oncologists (BAHNO) provides guidance on this topic, advising all patients undergoing RT to the head and neck region that they should receive a dental assessment before treatment, including an orthopantomogram radiograph (OPG).2 Clinical standards recommend a 14-day time-period from referral to first outpatient visit and a 62-day time-period from referral to starting treatment. All patients undergoing radiotherapy with curative intent should commence within four weeks of the decision to treat (in Liverpool, identified as the multidisciplinary team [MDT] outcome), or within 42 days after surgery. Any delays in the provision of any appropriate dental assessment and treatment may cause a delay in a patient receiving their RT. The Royal College of Surgeons of England advise dental extractions to be completed a minimum of ten days before starting cancer treatment.1,7,8,9
Aims
The aim is to determine the timing and nature of pre-radiotherapy dental assessments (including OPG), at the regional oncology centre compared against national guidelines and to raise awareness of the importance of this aspect of head and neck cancer care.
Standards
-
One hundred percent of patients undergoing RT should receive a pre-radiotherapy dental assessment
-
One hundred percent of patients undergoing RT should receive an OPG before commencing radiotherapy
-
Extractions should be completed a minimum of ten days before commencement of radiotherapy.
Methods
Prior to commencing this study, approval was gained from the Clinical Audit and Management System (CAMS number 80473) at Aintree University Hospital. Information Governance was also involved due to the potential sharing of data between sites.
Consecutive cohorts of HNC patients in two timeframes (January to March 2018 and January to March 2019) were identified retrospectively by a single operator from individual MDT data at Aintree University Hospital using the Somerset Cancer Register. Included in the cohort were patients having RT (primary RT, chemo-RT and post-operative RT) with curative intent for new primary HNC, with no history of previous HNC treatment. Exclusion criteria comprised palliation, recurrence, previous RT to the head and neck region and skull-base cancers.
The presence/absence of OPGs was found through the Carestream Client Medical Imaging system. Patient notes and records from Clatterbridge Cancer Centre's (CCC's) specialist dental software system were analysed for details of pre-radiotherapy assessments, any dental treatment required, RT start dates and occurrence of ORN on clinical review. Dental assessments were held at the CCC and were scheduled alongside construction of the patient radiotherapy mask and a PET/CT scan. Patients might also see the head and neck specialist nurse at this appointment.
Patient clinical details were identified from electronic records (SIGMA) and were entered onto a pre-populated excel spreadsheet, including date of birth, date of MDT, diagnosis, tumour site and stage and treatment. The data were exported to IBM SPSS Statistics version 25 for data analysis.
Results
In total, 145 patients were included, where 73 identified at MDT from 1 January 2018 to 31 March 2018 and 72 from 1 January 2019 and 31 March 2019. Demographic and clinical characteristics of patients from both years were very similar (Table 1). Mean (standard deviation) age overall was 62 (11) years; further breakdown of the overall sample is shown in Table 1.
The majority of patients (72%, 104) had a formal dental assessment at the CCC, these being a median (interquartile range [IQR]) 12 (12-17) days before starting RT. Four patients were assessed within ten days before starting RT. A summary of the type of treatment undertaken and of the timing of extraction in relation to the MDT meeting, the CCC assessment and starting RT is given in Table 2.
The extraction rate was 45% (47/104) and extractions were completed a median (IQR) of 13 (11-19) days before RT started. Reasons for any delays were not recorded. The outlier patient at 49 days before RT had extractions at the time of surgery, with the reason for delaying RT not stated in clinical letters or notes. Any extractions before the CCC assessment and the final MDT decision to proceed to RT were done exclusively at the time of surgery.
Table 3 summarises treatment by speciality team and tumour location. For patients with CCC assessments, the extraction rates were 53% (10/19) for the maxillofacial unit team and 41% (35/85) for ear, nose and throat; rates were 58% (7/12) for oral cavity tumours, 53% (9/17) larynx, 42% (28/42) oropharynx and 38% (3/8) other locations.
The majority of patients (89%, 129) had an OPG radiograph assessment at a median (IQR) of 19 (12-55) days before RT (n = 127), with three patients having the OPG after RT (at 1, 3 and 11 days). OPGs were present at the time of CCC dental assessment for 81% of patients (104/129). On assessment of OPGs, 114 had dentate maxillae and 121 had dentate mandibles. Of these patients, 100% had teeth present on the same side as the lesion targeted for radiotherapy. It was not documented as to what proportion of patients not receiving an OPG were edentulous, or why they didn't have an OPG, suggesting it was simply overlooked.
At the time of writing, no patients (0%) were diagnosed with ORN on review of their clinical letters. Data on any other post-RT complications were not recorded.
Table 4 shows how the percentage of patients who did not have an OPG radiograph varied by patient demographic and clinical characteristics. There were statistically significant differences regarding OPG for age (older patients less likely to have an OPG), tumour site (laryngeal patients least likely), tumour stage (early tumours less likely) and treatment (RT only being least likely). These factors were inter-related, with further details shown in Table 5. There were no significant case-mix differences with regard to the absence of a formal CCC dental assessment (Table 4).
Discussion
HNC treatment planning can be very complex and timely dental assessment is an important component. It is embedded within national guidelines.2 The possible sequelae of RT on the oral cavity supports the rationale for assessments to take place before starting RT in order to reduce the risk of complications.4
Although this study indicates that the Unit currently falls short of BAHNO standards, the 75% receiving a pre-RT dental assessment was considerably higher than the 35.4% national average noted in the tenth National Head and Neck Cancer Audit of 2014.10
The Royal College of Surgeons guidelines for completing all extractions at least ten days before starting RT was met for all but four patients. However, performing pre-RT dental extractions is controversial, with multiple studies suggesting pre-RT extractions may increase the risk of developing ORN, possibly due to the effect of radiation on rapid bony turnover in the post-extraction socket.7,8,9 While a degree of ambiguity remains regarding the appropriate timing for extractions, there is consensus that prophylactic extraction of all teeth is contraindicated. Mahmood et al. explored the impact that mastication (or lack thereof) has on HNC patients, highlighting the importance of oral health optimisation in this cohort.11 Extraction of teeth should always be planned in conjunction with definitive restoration, highlighting the importance of a restorative dental presence at MDT.3,6 The timing of extractions requires future investigation and although it is encouraging that no patients in this cohort developed ORN, this is probably due to the limited length of follow-up.
Head and neck oncology patients require multi-professional assessments and there are many steps to navigate within the 62-day guidance window from referral to treatment. This includes examinations under anaesthetic for laryngopharyngeal cancers, imaging (including MRI, CT, US, PET), biopsy or fine needle aspiration, gastrostomy feeding tube placement and planning of prostheses.3 Dental assessments are one of many stages that may cause a delay in treatment.
Complications of RT to the head and neck include mucositis, recurrent candidiasis, xerostomia, trismus and ORN.6,7,12,13 These can lead to further secondary complications, such as the so-called 'radiation caries', attributable to the loss of saliva's cariostatic effects.6,14 Trismus is an additional difficulty, as provision of any complex dental treatment on an individual with limited mouth opening can be challenging, if not impossible.12,13 The resulting effects on oral health can cause a negative impact on quality of life.6,15,16 Given the impact on a patient's quality of life following a cancer diagnosis, together with the sheer volume of information they are given within the first few days and weeks, it is understandable that they cannot process or remember some of this information.16 This highlights the importance of having a separate dental assessment before starting RT, as this provides smaller pieces of information in specific settings for the patients to process more easily. Thorough dental examination and treatment before RT will limit the amount of treatment required after RT.17
One major complication following RT is ORN, defined as clinically exposed necrotic irradiated bone for a duration of more than three months in the absence of neoplastic disease.18 It can lead to significant pain, discomfort and profound reduction in a patient's quality of life.19 In severe cases it can necessitate a second major surgery for debridement of unsalvageable necrotic bone and reconstruction of resulting defects.
Our data show that the commonest site for cancer was the oropharynx, possibly reflecting the recent increase in numbers of patients with HPV-related oropharyngeal cancer. If this trend continues we can expect in future to see an increased number of HNC patients requiring RT.20,21 As these patients often present at a younger age, a more complex dentition is usually seen which can be a challenge to the dentist in deciding the appropriate management of pre-RT dentition and the prevention of post-RT complications.22 Without a pre-treatment assessment, significant challenges may be faced by any maxillofacial prosthodontist regarding the future rehabilitation of patients, with the altered oral environment generating additional prosthetic demands.6 Furthermore, given that HPV-positive patients live longer, we can expect the longer-term oral complications of RT to have profound effects on their quality of life and this implies that a careful and thorough planning of their pre-RT treatment is required.6,23 In their Delphi study of 89 consensus statements on the planning of pre-RT dental extractions, after three rounds of data collection, Moore et al. highlighted the complexity in planning treatments for patients about to undergo RT and emphasised the need for a workforce dedicated to this specialised field, with appropriate representation in HNC MDT meetings.3,24
Intensely-modulated radiotherapy (IMRT) aims to minimise the dose of radiotherapy to healthy tissues.12 For oropharyngeal cancers, this ensures the majority of dentoalveolar bone is out of the primary RT field, thereby minimising the risk of ORN.9,12 Indeed, at the time of writing, there were no cases of ORN recorded for this cohort in their patient notes. This may be a testament to the benefits of IMRT, the oral hygiene regime provided in the pre-dental assessment, or both.12 Previous studies have shown the onset of ORN to be quite variable following completion of RT, ranging from 1-69 months afterwards, though it usually occurs within 2-3 years of completion.4 8,12,22 Although the risk of developing ORN in oropharyngeal cancers is theoretically reduced with IMRT, it is not eliminated and neither are the other complications of RT.14,25,26 In fact, it has been suggested that IMRT may counterintuitively increase the risk of developing ORN, especially in the chemo-radiotherapy population.27 Radiation caries can still lead to significant morbidity to patients, especially when combined with trismus and the related difficulties in treatment.13,15
Abed et al. found the rate of active caries in patients with IMRT to be higher than anticipated, with more than half of patients diagnosed with active dental caries in more than two teeth.16 It should be noted that even in the presence of IMRT, xerostomia may still occur, as may its sequelae; therefore, even if oropharyngeal cancers are treated with IMRT, a pre-treatment dental assessment is still necessary.15,27
Within our cohort, the proportion of patients without a pre-treatment dental assessment was observed to be higher in older patients (>65 years), with laryngeal/oral cavity tumours and with less advanced disease (stage 1-2). Patients with laryngeal tumours may not be offered routine pre-RT dental assessments, as the tooth-bearing tissues will be spared from the primary beam, as noted by Bak et al.28 However, BAHNO guidelines still recommend a dental assessment irrespective of the primary site.2 ORN is not the only complication of RT and in consideration of QUANTEC (Quantitative Analyses of Normal Tissue Effects in the Clinic) guidelines, severe xerostomia is generally avoided with RT doses of less than 25 Grey (Gy) in bilaterally-exposed parotid glands, or with an average mean dose of less than 20 Gy to one parotid gland.29 Bak et al.'s study found the tooth-bearing tissues around the mandibular second molars in patients undergoing IMRT for laryngeal cancer to have an average dose of 24 Gy, with the dose increasing for more posterior tissues.28 Considering the anatomical position of the parotid glands posterior to the ramus of the mandible, it is likely the whole parotid will receive amounts of radiation sufficient to result in xerostomia and subsequent dental pathology, even in laryngeal patients receiving IMRT, thus highlighting the need for pre-treatment dental assessments irrespective of the tumour site.2,28,29
Patient HPV status was not recorded, but as the median patient age for HPV-related tumours tends to be younger than for HPV-negative patients, one might conclude that the latter have more 'traditional' HNC risk factors such as tobacco and excessive alcohol.20,22,27 Older patients with these risk factors are probably more likely to be edentulous, which might explain why an OPG or pre-RT dental assessment was not offered. Whether or not this assumption is correct, the requirement for a pre-RT dental assessment still applies for edentulous patients, as the consequences of RT are still relevant, including the possibility of poor denture retention, mucositis and candidiasis.6,15,19 Additionally, as stated by Kufta et al. and Nabil et al., current dentures may need adjustment to reduce the chance of trauma to oral tissues which may subsequently lead to ORN; therefore, edentulous patients still require a pre-RT assessment.6,14,18
Limitations
The principal weakness of this study is the relatively small number of patients and the short follow-up period. Two time-frames were used to increase patient numbers and to determine whether there were any changes in practice between each cohort, of which there were none. With longer follow-up, more patients may develop ORN and the timing of extractions relative to RT may provide further information for future guidance. The compilation of data from multiple sources, trusts and hospitals proved challenging given the requirements of information governance and data protection. Other than extractions, any treatments provided at the dental assessment were not recorded; the type of treatment completed by general dental practitioners was also not recorded.
Recommendations
A restorative dental presence should continue to be included at MDT meetings to facilitate considerations for oral health optimisation and future rehabilitation before commencing RT, as per National Institute for Health and Care Excellence recommendations.3
All patients, including edentulous patients, must receive a pre-treatment assessment before commencing RT. Mandatory dental referrals should be included within the pre-RT pathway within regional oncology centres, for example, at the same time as constructing the moulds for RT masks.
OPGs should be considered as part of HNC staging scans if patients are likely to undergo RT and should be undertaken before MDT to avoid delays in the patient pathway.
Having a dedicated dental service for pre-RT assessment and dental treatment develops a workforce of clinicians experienced in managing patients with pre and post RT complications of HNC.17,24 With their expertise they provide a valuable service for both general dental practitioners and patients and their services should be preserved as much as possible.
Conclusion
We are not currently meeting the clinical standards set for pre-treatment dental assessments, as per the BAHNO 2009 standards; however, our rate is higher than the national average.2,10 This suggests that our efforts to integrate dental assessment into the HNC pathway have been worthwhile, though there is still room for improvement. Early identification of patients requiring RT and their timely referral from MDT to the dental services are essential, regardless of their dental status or site of their primary tumour. As the incidence of oropharyngeal cancers is increasing and the mainstay treatment involves RT, there is a need for a well-organised approach to pre-RT dental assessments. Patients are potentially at risk of developing complications such as ORN, hyposalivation and mucositis as a result of untreated oral pathology and a thorough dental assessment before commencement of RT will help prevent or minimise these problems.
References
The Royal College of Surgeons of England and The British Society for Disability and Oral Health. The Oral Management of Oncology Patients Requiring Radiotherapy, Chemotherapy and/or Bone Marrow Transplantation: Clinical guidelines. 2012. Available at https://www.rcseng.ac.uk/dental-faculties/fds/publications-guidelines/clinical-guidelines/ (accessed October 2021).
British Association of Head and Neck Oncologists. BAHNO standards 2009. 2009. Available at https://bahno.org.uk/_userfiles/pages/files/bahnostandardsdoc09.pdf (accessed October 2020).
National Institute for Clinical Excellence. Guidance on Cancer Services - Improving Outcomes in Head and Neck Cancers - The Manual. 2004. Available at https://www.nice.org.uk/guidance/csg6/resources/improving-outcomes-in-head-and-neck-cancers-update.pdf-773377597 (accessed October 2020).
Brennan M T, Treister N S, Sollecito T P et al. Dental disease before radiotherapy in patients with head and neck cancer: Clinical Registry of Dental Outcomes in Head and Neck Cancer Patients. J Am Dent Assoc 2017; 148: 868-877.
MacCarthy D, Clarke M, O'Regan M. An audit of the baseline dental status and treatment need of individuals referred to Dublin Dental University Hospital for a pre-radiotherapy dental and oral assessment. J Irish Dent Assoc 2017; 63: 269-276.
Siddall K Z, Rogers S N, Butterworth C J. The prosthodontic pathway of the oral cancer patient. Dent Update 2012; 39: 98-100.
Beech N M, Porceddu S, Batstone M D. Radiotherapy-associated dental extractions and osteoradionecrosis. Head Neck 2017; 39: 128-132.
Moon D H, Moon S H, Wang K et al. Incidence of, and risk factors for, mandibular osteoradionecrosis in patients with oral cavity and oropharynx cancers. Oral Oncol 2017; 72: 98-103.
El-Rabbany M, Duchnay M, Raziee H R et al. Interventions for preventing osteoradionecrosis of the jaws in adults receiving head and neck radiotherapy. Cochrane Database Syst Rev 2019; DOI: 10.1002/14651858.CD011559.pub2.
Health and Social Care Information Centre. National Head and Neck Cancer Audit 2014. 2015. Available at https://files.digital.nhs.uk/publicationimport/pub18xxx/pub18081/clin-audi-supp-prog-head-neck-dahn-13-14.pdf (accessed October 2020).
Mahmood R, Butterworth C, Lowe D, Rogers S N. Characteristics and referral of head and neck cancer patients who report chewing and dental issues on the Patient Concerns Inventory. Br Dent J 2014; DOI: 10.1038/sj.bdj.2014.453.
Ben-David M A, Diamante M, Radawski J D et al. Lack of osteoradionecrosis of the mandible after intensity-modulated radiotherapy for head and neck cancer: likely contributions of both dental care and improved dose distributions. Int J Radiat Oncol Biol Phys 2007; 68: 396-402.
Cho H, Kumar N. Dental management of a patient with head and neck cancer: a case report. Br Dent J 2019; 227: 25-29.
Kufta K, Forman M, Swisher-McClure S, Sollecito T P, Panchal N. Pre-Radiation dental considerations and management for head and neck cancer patients. Oral Oncol 2018; 76: 42-51.
Vissink A, Jansma J, Spijkervet F K L, Burlage F R, Coppes R P. Oral sequelae of head and neck radiotherapy. Crit Rev Oral Biol Med 2003; 14: 199-212.
Abed H, Reilly D, Burke M, Daly B. Patients with head and neck cancers' oral health knowledge, oral health-related quality of life, oral health status, and adherence to advice on discharge to primary dental care: A prospective observational study. Spec Care Dentist 2019; 39: 593-602.
Waring E, Mawardi H, Woo S B et al. Evaluation of a community-based dental screening programme before radiotherapy for head and neck cancer: a single-centre experience. Supportive Care Cancer 2019; 27: 3331-3336.
Nabil S, Samman N. Incidence and prevention of osteoradionecrosis after dental extraction in irradiated patients: a systematic review. Int J Oral Maxillofac Surg 2011; 40: 229-243.
Rogers S N, Semple C, Babb M, Humphris G. Quality of life considerations in head and neck cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 2016; DOI: 10.1017/S0022215116000438.
Grønhøj C, Jensen D, Dehlendorff C et al. Impact of time to treatment initiation in patients with human papillomavirus-positive and-negative oropharyngeal squamous cell carcinoma. Clin Oncol (R Coll Radiol) 2018; 30: 375-381.
Mehanna H, Beech T, Nicholson T et al. Prevalence of human papillomavirus in oropharyngeal and nonoropharyngeal head and neck cancer - systematic review and meta-analysis of trends by time and region. Head Neck 2013; 35: 747-755.
Patel V, Patel D, Browning T et al. Pre-radiotherapy dental status of oropharyngeal cancer patients based on HPV status in a novel radiation era. Br Dent J 2020; DOI: 10.1038/s41415-020-1922-y.
Albers A E, Qian X, Kaufmann A M, Coordes A. Meta analysis: HPV and p16 pattern determines survival in patients with HNSCC and identifies potential new biologic subtype. Sci Rep 2017; DOI: 10.1038/s41598-017-16918-w.
Moore C, McLister C, O'Neill C, Donnelly M, McKenna G. Pre-radiotherapy dental extractions in patients with head and neck cancer: a Delphi study. J Dent 2020; DOI: 10.1016/j.jdent.2020.103350.
Nabil S, Samman N. Risk factors for osteoradionecrosis after head and neck radiation: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 113: 54-69.
Lee I J, Woong S K, Lee C G et al. Risk factors and dose-effect relationship for mandibular osteoradionecrosis in oral and oropharyngeal cancer patients. Int J Radiat Oncol Biol Phys 2009; 75: 1084-1091.
Patel V, Humbert-Vidan L, Thomas C et al. Radiotherapy quadrant doses in oropharyngeal cancer treated with intensity modulated radiotherapy. Faculty Dent J 2020; 11: 166-172.
Bak S Y, Qi X S, Kelly J A et al. Dosimetric distribution to tooth-bearing areas in intensity-modulated radiation therapy for head and neck cancer: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol 2016; 121: 43-48.
Deasy J O, Moiseenko V, Marks L, Chao K S C, Nam J, Eisbruch A. Radiotherapy dose - volume effects on salivary gland function. Int J Radiat Oncol Biol Phys 2010; DOI: 10.1016/j.ijrobp.2009.06.090.
Author information
Authors and Affiliations
Contributions
Rhydian King: methodology, investigation, writing - original draft, writing - review and editing. Chien Li: investigation, writing - review and editing. Derek Lowe: statistical analysis, writing - review and editing. Simon Rogers: conceptualisation, writing - review and editing, supervision.
Corresponding author
Ethics declarations
There are no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
King, R., Li, C., Lowe, D. et al. An audit of dental assessments including orthopantomography and timing of dental extractions before radiotherapy for head and neck cancer. Br Dent J 232, 38–43 (2022). https://doi.org/10.1038/s41415-021-3823-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-021-3823-0
- Springer Nature Limited