Abstract
Careful orthodontic treatment planning should involve the delineation of clear treatment objectives within each dental arch. Treatment planning decisions are underpinned by aesthetic goals, dental health considerations and the prospect of stability, with these factors often competing. There is also a near-universal acceptance of the requirement for some form of retention. A novel hierarchy of orthodontic stability is proposed. As further evidence emerges and technical refinement continues, it is likely that this will undergo further adaptation. Ultimately, however, this knowledge will ensure that our understanding of the merits of orthodontic intervention, allied to the burden of retention, can be clearly presented to prospective orthodontic patients.
Key points
-
There is a key interplay between often competing occlusal, functional and aesthetic goals during orthodontics.
-
A novel hierarchy of orthodontic stability accounting for contemporary approaches to retention is proposed.
-
This hierarchy will be subject to adaptation but should underpin our understanding of the merits of orthodontic intervention, allied to the burden of retention, and therefore could be integral both to planning decisions and decision-making.
Similar content being viewed by others
Introduction
Orthodontics has undergone seemingly relentless growth and refinement in recent years. The last two decades, in particular, have been marked by an emphasis on refinement of appliances, to improve both experience and aesthetics; a drive to reduce treatment times, with use of surgical and non-surgical adjuncts; and continued efforts to circumvent suboptimal compliance and to reduce the need for extractions.1,2
Notwithstanding this, the health benefits of treatment remain uncertain; conversely, the aesthetic benefits of orthodontics are undeniable. The latter stem from predictable improvement in both dental and smile aesthetics, and have prompted a paradigm shift in treatment planning with increasing focus on the anteroposterior and vertical positioning of the maxillary anteriors.3 Historically, treatment planning centred on the position of the lower anterior teeth, with significant advancement held to be unstable and rarely justifiable.4,5 This philosophy appears to have less traction nowadays, with a diminishing emphasis on the positioning of the lower anteriors.
Consequently, planned tooth movements may involve a trade-off between aesthetic objectives, including both facial and dental aesthetic goals, and the prospect of long-term stability. This interplay is further influenced by the effects of tooth movement on dental health, allied to the effects of ageing and the relative stability of various tooth movements. The latter is known to be influenced by maturational change and, therefore, is almost inevitable without recourse to some form of retention.6 Notwithstanding this, planning decisions may influence the likelihood of producing more stable outcomes.
Orthodontic planning and aesthetics
Aesthetic improvement associated with orthodontic treatment may translate into improved oral health-related quality of life.7 There is also agreement that more marked malocclusions predispose to negative social experiences, including teasing and bullying, with possible related effects in terms of self-confidence and social wellbeing.8 Moreover, orthodontic intervention has proven effective in mitigating these adverse effects in these more salient malocclusions, particularly those characterised by visible impairment including excessive overjet, overbite and anterior spacing.9 The inter-relationship between stability and aesthetics is pertinent to the management of a range of malocclusions.
The achievement of a Class I incisor relationship is typically a central treatment objective. This relates to the increased prospect of stability and optimal aesthetics. Stability may stem from the combination of a normal overjet and overbite, with the maxillary incisors resting on the tips of the mandibular incisors, while the lower anteriors may in turn be stabilised with a fixed lingual retainer.10 Correction of excessive overjet involves a judgement as to whether to reduce this by means of retraction of the maxillary incisors, advancement of the mandibular incisors or a combination of these movements. Specifically, in the presence of significantly procumbent maxillary incisors and a protrusive upper lip and soft tissue pattern, retraction of the maxillary incisors may be appropriate in order to maximise the aesthetic benefit of treatment. Moreover, retraction of the maxillary incisors may promote the achievement of lip competence, which may reduce the propensity to relapse in the overjet. Similarly, by limiting advancement of the mandibular incisors, there may be less risk of lower anterior irregularity reappearing and of recurrence of the overjet. Conversely, in the presence of retrusive soft tissue patterns with relatively thin soft tissues and limited upper lip support, the scope to undertake retraction of the maxillary incisors may be limited or absent.11 As such, a decision may be made to address the overjet by advancement of the mandibular incisors, in isolation or in conjunction with minimal maxillary incisor retraction. This approach will help to optimise both facial and dental aesthetics, but does increase the risk of relapse associated with re-uprighting of the mandibular incisors in the post-treatment phase. The latter may ultimately translate both into mandibular incisor irregularity and increased overjet. Alternatively, a decision may be made to accept a residual overjet in the presence of a skeletal II discrepancy or retrusive soft tissue profile, where orthognathic surgery is not considered appropriate. Permanent bonded retention may be mandatory in these cases.
Similar logic can be applied to Class I malocclusion, with anteroposterior change of the dentition often not indicated in the presence of acceptable facial and soft tissue support. Meanwhile, protrusive soft tissues in conjunction with excessive proclination of the incisors may dictate retraction of the dentition with space creation to reduce the degree of dental and associated soft tissue protrusion. While this approach may lead to aesthetic improvement, significant retraction may place increasing onus on diligent use of removable and fixed retention (Fig. 1). Finally, advancement of the dentition could be considered in class I (or indeed class II division 2) cases with retrusive soft tissue profile in order to enhance soft tissue support.11 Again, this improvement in aesthetics is counterbalanced by increasing instability and a higher premium on diligent, prolonged retention (Fig. 2).
a, b) Class I malocclusion with bimaxillary proclination. c) There was crowding of both arches with proclination of the maxillary and mandibular incisors with protrusive soft tissues and a procumbent lower lip. d, e) A decision was made to treat this on an extraction basis with loss of four premolars in order to relieve the upper and lower crowding, aligning the arches, but f) also to facilitate retraction of the lower lip
A class II division 2 malocclusion treated on a non-extraction basis with a combination of fixed and removable appliances. Non-extraction treatment in the mandibular arch, in particular, is of mechanical benefit in terms of overbite reduction, allowing advancement of the anterior dentition. This approach may, however, place an additional premium on stability, with lower fixed retention, in particular, advisable with significant advancement of the mandibular incisors
Finally, a similar thought process may apply to class III cases, with correction of the incisor relationship necessitating either retraction of the mandibular incisors, proclination of the maxillary incisors or a combination of these movements (Fig. 3). Again, the specific objectives should be tailored but should include aesthetic considerations. In particular, the inclination of the maxillary incisor is central to dental aesthetics, with excessive proclination being unaesthetic while also predisposing to a reduction in the overbite12 as well as non-axial loading on the incisor, which may rarely lead to fremitus. A positive overbite is thought to contribute to stability of class III correction; as such, retraction of the mandibular incisors is often key to class III correction.
A class III case involving retraction of the mandibular incisors. a, b) This approach was planned to maintain the maxillary incisor inclination for aesthetic reasons, while c) retroclination of the mandibular incisors led to increase in the overbite. The latter was facilitated by use of pre-existing spacing in the mandibular arch. Establishment of a positive overbite is thought to increase the potential for stability of correction of the incisor relationship
Orthodontic planning and dental health
While the aesthetic benefit of orthodontics is clear, the health impacts are less proven, particularly in milder malocclusions. Notwithstanding this, orthodontic treatment does entail potential deleterious effects, chiefly related to the integrity of the roots, periodontal problems, and indeed demineralisation and even caries in susceptible individuals. As such, there is a balance to strike between aesthetic benefit and potential deleterious effect.
This interaction comes into sharper focus when planning significant anteroposterior and transverse change, in particular, but also to an extent during the alleviation of crowding, which may necessitate significant arch dimensional change. Clearly, there are safe limits to the magnitude of tooth movement governed by constraints related to the alveolar housing, cortical plates and the soft tissue envelope.13 Specifically, movement is restricted by the absence of sufficient alveolar bone, with attempts to overcome this risking root resorption, instability and periodontal problems.
Periodontal problems associated with orthodontic tooth movement relate to undermining of the existing support and are particularly likely in the presence of a thin gingival phenotype, characterised clinically by pre-existing recession. The latter may be associated with fenestration and dehiscence of the root surfaces.14,15 It may be inappropriate to attempt significant intra-alveolar tooth movement in these cases, instead either considering transverse change through sutural expansion or generating space conservatively in an effort to limit the onus on significant tooth movement. Moreover, incomplete correction leading to a degree of aesthetic improvement may be appropriate in order to safeguard dental health. The latter may occasionally increase the onus on prolonged retention.
A proposed hierarchy of stability
Since the post-retention studies carried out in the University of Washington from the 1980s onwards, it has become accepted that post-treatment change is highly likely but unpredictable.16 The inevitability of tooth movement following orthodontics relates to maturational change, with characteristic effects including a reduction in the mandibular intercanine width and increased irregularity of the mandibular anteriors, in particular.6 The latter may well predispose to an increase in the overbite. Unquestionably, these physiological changes predispose to deterioration in the alignment of the teeth. Consequently, we are now in an era where retention is accepted and considered indispensable in the majority of cases, certainly if indefinite occlusal perfection is targeted.
Notwithstanding this, a number of adjuncts and alternatives to the indefinite use of retention have been proposed. These include the use of surgical adjuncts including frenectomy and supracrestal circumferential fiberotomy to mitigate against specific issues, namely maxillary median diastema and significant rotation. The merits of these approaches are unclear and neither are regarded as a standalone solution.17 An alternative which has shown some promise is the use of selective, incremental inter-proximal reduction during the post-treatment period. Acceptable levels of stability were demonstrated with this approach up to three years post-treatment, although up to 5 mm of enamel reduction was necessary in the lower intercanine region.18
The requirement for a retention regime (currently mechanical rather than biological) is, almost universally accepted, with ongoing refinement to improve predictability and acceptability.19 Notwithstanding this, there has been little discourse in relation to the predictability of stability of specific occlusal features. The latter is further complicated in this era of prolonged retention against a backdrop of the aforementioned conflicting aesthetic and stability goals.
The majority of orthodontic patients present with more than a single occlusal anomaly. For example, overjet and overbite often coexist in class II cases; moreover, perfect alignment of both arches is a rarity, particularly in adults.6 Equally, transverse issues commonly present in conjunction with vertical and anteroposterior problems. Specific occlusal features may well be more stable than others and the stability of the outcome is undeniably influenced by the provision of retainers.
It would be valuable from an informed consent perspective to be able to speculate as to the prospect of stability of correction of a range of occlusal features, and to have an appreciation of the effect of retention in mitigating relapse. Indeed, Proffit et al. (2007)20 developed a hierarchy for stability of surgical orthodontic procedures. The latter was underpinned largely by prospective research; study of the likelihood of orthodontic stability is also complicated by the widespread acceptance of retention as well as the range of approaches taken to this. However, on the basis of an increasing body of evidence, a tentative hierarchy of stability (Fig. 4) can be proposed.
A tentative hierarchy for orthodontic stability based on existing approaches to retention. This hierarchy has been inferred on the basis of best available prospective evidence. The prospect of stability appears to be best for anteroposterior correction (both class II and class III), with retention often having relatively limited bearing on this. The long-term preservation of correction of spacing and malalignment may be good but is highly reliant on successful retention. Overbite reduction may be linked to preservation of alignment. Transverse correction (particularly expansion) is unstable and contingent on diligent wear of retainers, with rigidity of retainer material also important. Finally, correction of anterior open bite is often highly unstable, with passive approaches to retention often unable to mitigate relapse
Based on observational research, it appears that anteroposterior correction is the most stable form of orthodontic movement.21,22 In particular, both class III and class II correction appear to be relatively stable at the molar, canine and incisor level, particularly in skeletally mature individuals. On the basis of prospective research, relapse of more than 1 mm of severe class II cases arose in less than 25% at 12 months post-treatment.21 In a retrospective 32-year follow-up involving 14 participants, class II correction was generally stable, although changes in both overbite and lower anterior alignment were observed.22 Parameters affecting stability of class II correction are largely unclear, with Pancherz et al. (2014)21 citing the importance of optimal buccal segment interdigitation, although this has not been confirmed in allied research.21 It would also be intuitive to expect that reduction in lip incompetence would assist in promoting stability. Retention regime appears to have relatively little bearing on the stability of class II correction, however. Similarly, class III correction is thought to be stable in skeletally mature individuals, with the overbite thought to be an important contributor to stable outcomes. Again, the use of retainers appears to have little influence on stability in this spatial plane.23
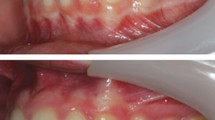
Increased overbite is generally regarded as relatively unstable. However, on the basis of long-term follow-up, it would be reasonable to conclude that this contention is influenced by successful retention to a much more meaningful degree than is the case with anteroposterior change. Based on the post-retention studies involving Little's group,24 stability of overbite reduction was found to be problematic, with instability more likely with retroclined incisors at the outset with a positive correlation between initial and post-retention overbite. However, based on an allied study involving participants who had a longer period of retention, mean relapse of just 0.8 mm arose over a follow-up period in excess of eight years.25 Establishing a corrected incisor relationship is a prerequisite permitting a centric stop for the lower incisors on the cingulum plateau on the maxillary central incisors. It is important to note that change in position of the lower anteriors may influence overbite depth, with lingual movement of one or more incisors predisposing to their overeruption and subsequent increase in overbite (Fig. 5). As such, diligent retention may assist in retaining overbite reduction in the longer term.
a) The stability of overbite reduction may be better than that alluded to in research studies. This propensity to overstate the potential for relapse in overbite is linked to the relationship between lower anterior alignment and overbite. Specifically, with perfect lower alignment in the presence of class I incisors significant, overeruption of the lower anteriors is impeded by occlusal contact with the cingulum plateau of the maxillary incisors. b) However, lower anterior malalignment often leads to lingual movement of one or more lower incisors. These teeth are then free to extrude, leading to a local increase in overbite. The latter is therefore contingent on loss of alignment
Correction of anterior open bite is known to be highly unstable. As with other orthodontic problems, the prospect of stability relates to the aetiology, with skeletal issues less amenable to correction than milder problems of dento-alveolar origin. It is therefore particularly important that there is clear delineation and appropriate management of the aetiology of the anterior open bite. Similarly, the presence of modifiable habits including digit sucking is a good prognostic indicator. Non-surgical correction may be achieved by intrusion of posterior teeth; reduction in the lower anterior facial height, related either to intrusion or mesial movement of posterior teeth; or extrusion of the anterior teeth. There is little comparative research in relation to the relative stability of these approaches; however, posterior intrusion, in particular, has been shown to have promising levels of stability.26 Extrusion of anterior teeth may be particularly unstable in the absence of a corrected habit. As such, it is often wise to limit anterior extrusion, although the feasibility of this approach is also governed by aesthetic demands including the degree of incisal display in repose and on smiling. Overall, the stability of open bite correction is limited, even when fixed or removable retention are used.
Transverse correction is also considered inherently unstable.27 Again, a range of factors govern the approach to transverse correction, including the extent of any associated crossbite, the aetiology and location of the problem, and the degree of skeletal maturity. Mid-palatal expansion may well be an option with or without adjunctive surgery to produce skeletal change in conjunction with dento-alveolar remodelling. Equally, consideration can be given to constriction of the mandibular arch to limit the magnitude of maxillary expansion required. While skeletal expansion is regarded as more stable than dento-alveolar, expansion remains relatively unstable.27 Notwithstanding this, diligent use of relatively rigid upper removable retainers may limit the amount of post-treatment change.
The bulk of research concerning the stability of post-treatment outcomes relates to maintenance of orthodontic alignment. Correction of alignment, rotations and spacing are all particularly prone to change, with movement of the lower anteriors essentially physiologic in nature.6,16 Conversely, re-opening of space typically represents a form of true relapse following treatment. There is, however, ample evidence to suggest that diligent use of either fixed or removable retainers may assist in maintaining alignment in the long term.28 While there are recognised challenges associated with both approaches, it would seem reasonable to suggest that the prospect of stability in terms of alignment is good in the presence of optimal retention.
The advent of this hierarchy may be exploited in the informed consent and treatment planning process, educating prospective patients on the likelihood of long-term stability in relation to a range of occlusal features (Fig. 4). Further appreciation and refinement is likely to occur on the basis of an expanding evidence base allied to refinement of retention regimes.
Conclusion
Careful orthodontic treatment planning should involve the delineation of clear treatment objectives within each dental arch in order to achieve occlusal, functional and aesthetic goals. Treatment decisions may involve reconciliation between the dictates associated with aesthetics, dental health and the prospect of stability. These decisions, allied to an increasing appreciation of the relative stability of various occlusal features, will ensure that our understanding of the relative merits of orthodontic intervention allied to the burden of retention can be clearly presented to prospective orthodontic patients.
References
Fleming P S, Fedorowicz Z, Johal A, El-Angbawi A, Pandis N. Surgical adjunctive procedures for accelerating orthodontic treatment. Cochrane Database Syst Rev 2015; DOI: 10.1002/14651858.CD010572.pub2.
DiBiase A T, Woodhouse N R, Papageorgiou S N et al. Effects of supplemental vibrational force on space closure, treatment duration, and occlusal outcome: A multicentre randomized clinical trial. Am J Orthod Dentofacial Orthop 2018; DOI: 10.1016/j.ajodo.2017.10.021.
Ackerman J L, Proffit W R, Sarver D M. The emerging soft tissue paradigm in orthodontic diagnosis and treatment planning. Clin Orthod Res 1999; 2: 49-52.
Mills J R. The stability of the lower labial segment. A cephalometric survey. Dent Pract Dent Rec 1968; 18: 293-306.
Williams P. Lower incisor position in treatment planning. Br J Orthod 1986; 13: 33-41.
Sinclair P M, Little R M. Maturation of untreated normal occlusions. Am J Orthod 1983; 83: 114-123.
Javidi H, Vettore M, Benson P E. Does orthodontic treatment before the age of 18 years improve oral health-related quality of life? A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop 2017; 151: 644-655.
Seehra J, Fleming P S, Newton T, DiBiase A T. Bullying in orthodontic patients and its relationship to malocclusion, self-esteem and oral health-related quality of life. J Orthod 2011; 38: 247-294.
Seehra J, Newton J T, Dibiase A T. Interceptive orthodontic treatment in bullied adolescents and its impact on self-esteem and oral-health-related quality of life. Eur J Orthod 2013; 35: 615-621.
Fleming P S, Springate S D, Chate R A. Myths and realities in orthodontics. Br Dent J 2015; 218: 105-110.
Alkadhi R M, Finkelman M D, Trotman C A, Kanavakis G. The role of lip thickness in upper lip response to sagittal change of incisor position. Orthod Craniofac Res 2019; 22: 53-57.
Eberhart B B, Kuftinec M M, Baker I M. The relationship between bite depth and incisor angular change. Angle Orthod 1990; 60: 55-58.
Ackerman J L, Proffit W R. Soft tissue limitations in orthodontics: treatment planning guidelines. Angle Orthod 1997; 67: 327-336.
Melsen B, Allais D. Factors of importance for the development of dehiscences during labial movement of mandibular incisors: a retrospective study of adult orthodontic patients. Am J Orthod Dentofacial Orthop 2005; 127: 552-625.
Bassarelli T, Melsen B. Expansion: how much can the periodontium tolerate? Clin Orthod Res 2001; 4: 235-241.
Little R M. Clinical implications of the University of Washington post-retention studies. J Clin Orthod 2009; 43: 645-651.
Sullivan T C, Turpin D L, Artun J. A postretention study of patients presenting with a maxillary median diastema. Angle Orthod 1996; 66: 131-138.
Aasen T O, Espeland L. An approach to maintain orthodontic alignment of lower incisors without the use of retainers. Eur J Orthod 2005; 27: 209-214.
Naraghi S, Ganzer N, Bondemark L, Sonesson M. Comparison of post-treatment changes with and without retention in adolescents treated for maxillary impacted canines-a randomized controlled trial. Eur J Orthod 2020; DOI: 10.1093/ejo/cjaa010.
Proffit W R, Turvey T A, Phillips C. The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: an update and extension. Head Face Med 2007; 3: 21.
Oliver G R, Pandis N, Fleming P S. A prospective evaluation of factors affecting occlusal stability of Class II correction with Twin-block followed by fixed appliances. Am J Orthod Dentofacial Orthop 2020; 157: 35-41.
Pancherz H, Bjerklin K, Lindskog-Stokland B, Hansen K. Thirty-two-year follow-up study of Herbst therapy: a biometric dental cast analysis. Am J Orthod Dentofacial Orthop 2014; 145: 15-27.
Yoshizumi J, Sueishi K. Post-treatment Stability in Angle Class III Cases. Bull Tokyo Dent Coll 2016; 57: 29-35.
Kim T W, Little R M. Postretention assessment of deep overbite correction in Class II Division 2 malocclusion. Angle Orthod 1999; 69: 175-186.
Schütz-Fransson U, Bjerklin K, Lindsten R. Long-term follow-up of orthodontically treated deep bite patients. Eur J Orthod 2006; 28: 503-512.
Scheffler N R, Proffit W R, Phillips C. Outcomes and stability in patients with anterior open bite and long anterior face height treated with temporary anchorage devices and a maxillary intrusion splint. Am J Orthod Dentofacial Orthop 2014; 146: 594-602.
Zuccati G, Casci S, Doldo T, Clauser C. Expansion of maxillary arches with crossbite: a systematic review of RCTs in the last 12 years. Eur J Orthod 2013; 35: 29-37.
Steinnes J, Johnsen G, Kerosuo H. Stability of orthodontic treatment outcome in relation to retention status: An 8-year follow-up. Am J Orthod Dentofacial Orthop 2017; 151: 1027-1033.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The author declares no conflicts of interest.
Rights and permissions
About this article
Cite this article
Fleming, P. Orthodontic treatment planning: can we plan for stability?. Br Dent J 230, 717–721 (2021). https://doi.org/10.1038/s41415-021-2891-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-021-2891-5
- Springer Nature Limited
This article is cited by
-
Five tips for orthodontic practitioners
British Dental Journal (2021)