Abstract
Vital pulp therapies (VPTs) aim to preserve the vitality of the pulp. The European Society of Endodontology have begun a campaign to raise awareness on the efficacy of VPTs following on from the publication of their 2019 position statement, aimed at both specialists and general dental practitioners. This review examines the current evidence surrounding VPTs and provides a rational approach to the management of the exposed pulp with the aid of case studies. Success lies in accurate diagnosis and case selection, along with well-executed treatment and appropriate follow-up protocols. The introduction of calcium silicate cements has made these treatments more predictable.
Key points
-
There is sufficient evidence to recommend calcium silicate cements ahead of calcium hydroxide for all vital pulp therapies, but consideration must be given to potential discolouration in material selection.
-
The main driver for a decision between different vital pulp therapies is the visual appearance of the pulp and the ability to control haemorrhage.
-
Following careful case selection, teeth receiving vital pulp therapies with calcium silicate cements have a good prognosis, equal to pulpectomy and root canal treatment, which still remains an option in the event of failure.
Similar content being viewed by others
Introduction
Where deep caries management, trauma or iatrogenic damage results in pulp exposure, traditional approaches have advocated complete pulpectomy and root canal treatment (RCT). The aim of vital pulp therapy (VPT) is to assess and manage pulpal inflammation and maintain pulp vitality by preventing the progression of inflammation through to pulpal necrosis, avoiding the need for complex RCT.1,2 Success rates of VPTs have been reported to be comparable at five years to conventional pulpectomy and RCT,3 even in teeth with irreversible pulpitis,4,5 with the advantage of dentine preservation and that the pulp retains its ability to react to future insults and noxious stimuli.
VPT techniques have the potential to be simple and both cost- and time-efficient. If they are unsuccessful, RCT may still remain a viable treatment option in the future. While conventional RCT has excellent outcome survival and success rates, particularly in 'vital' cases,6 it is not without its technical challenges.7 We are now in a position to better understand the complexities that conventional RCT possesses, particularly anatomically, with the advent and now wider use of cone beam computerised tomography (CBCT) in endodontology demonstrating the intricacies and challenges of chemo-mechanical disinfection of the root canal anatomy.8
This paper builds on the discussion around diagnosis and treatment options for managing deep caries, and will consider the range of VPTs available. Appropriate diagnosis and careful case selection is essential, as are the use of appropriate operative management techniques. A review of pulpal diagnoses was considered in the first paper of this two-part series.
The categorisation of pulpitis as 'reversible' or 'irreversible' remains clinically useful and is almost universally accepted,9 but a patient's symptoms and clinical appearance may not fit exactly into either category. Furthermore, definitive treatment planning resulting in extraction or conventional endodontics based on pre-operative symptoms alone may be inappropriate. These are very much diagnoses of convenience as it is impossible to determine clinically the histological status of the pulp without removal of the tooth.10,11
Newer proposed classifications go some way to removing this diagnostic dichotomy and recognising that the various stages of inflammation are much more of a continuum (Table 1).11 VPTs work on the assumption that, biologically, the pulp has the capacity to regenerate and repair as long as the insult is removed and the inflammation can be successfully managed. The exposed pulp's ability to heal should be assessed on its appearance, and in particular, the ability to control bleeding.12 This clinical feature is used as a surrogate marker to determine the severity of pulp inflammation and inform decision-making as to whether to carry out a direct pulp cap (DPC), partial pulpotomy, full pulpotomy or pulpectomy (Table 2).
Operative management
The success of VPTs rely on the ability to control inflammation alongside managing any potential bacterial contamination of the exposed pulp. As with the management of deep caries, rubber dam is mandatory where VPT is being considered.2 As well as limiting bacterial contamination, this allows adequate disinfection using sodium hypochlorite as well as enhancing moisture control for definitive restoration.
If effective rubber dam isolation is not immediately possible due to the depth of an interproximal carious lesion, the periphery of the lesion should be cleared to sound tooth structure, staying away from the pulp. The papillae should then be appropriately managed to allow effective rubber dam isolation before proceeding with caries removal centrally, thereby preventing contamination of the pulp.13 If isolation is still not possible, the decision-making process may favour initial stabilisation of the tooth by ensuring a four-walled cavity, pulp extirpation and RCT. As with all deep caries management, magnification is important for undertaking VPTs, enabling assessment of caries removal and pulpal status with greater accuracy.14
Direct pulp cap
Placement of a DPC aims to create an environment which prevents bacterial ingress while also promoting dentine bridge formation and pulp healing, ultimately aiming to preserve pulp vitality.15,16,17 Bacterial microleakage around restorations has been shown to be an important determinant in pulp inflammation.18 In the absence of bacteria, the pulp is capable of maintaining vitality and forming a dentine bridge, even in the presence of food debris.19 A dentine bridge is considered essential to prevent the ingress of bacteria and allow re-establishment of the healthy pulp.20,21 If pulp tissue were to lose its homeostatic union with dentine, it would eventually undergo localised degeneration, atrophy and shrinkage away from the defect.22
It has been discussed that, although the absence of symptoms indicative of irreversible pulpitis is a positive prognostic factor,2,23 other factors may be more important in driving the decision between which approach to use. The size of a pulp exposure may contribute to the decision between which VPT approach to use,12 although it may be less important than previously thought. There is now evidence that exposures up to 2.5 mm can be predictably treated, but larger exposures (>2.5-5 mm) have a less predictable outcome.2,23,24,25,26,27 More important than exposure size is the ability to control bleeding,12,28,29 which is a likely indicator of the level of inflammation and may affect the seal achieved by a DPC material.29 Where the pulp is vital and haemorrhage can be controlled, the tooth is a good candidate for a DPC.
The tooth should be isolated with rubber dam, especially when considering the importance of preventing bacterial contamination. Haemostasis should be attempted using a cotton pellet soaked in sodium hypochlorite (1-5%) and should be achieved in less than five minutes (Figures 1 and 2).2,30 Following this, a calcium silicate cement (CSC; sometimes referred to as bioceramics) should be placed directly onto the pulp and the tooth restored with a definitive restoration, thus obtaining a definitive seal against bacterial and substrate ingress. Due to the long setting times of conventional CSCs and even newer CSCs (for example, Biodentine),31 it may be necessary to place a glass ionomer cement (GIC) or self-etching resin (for example, RelyX Unicem 2) over the DPC before placing a definitive restoration. Delaying the placement of a definitive restoration may be associated with a reduced prognosis.32 The success of DPC procedures using CSCs in extensively carious teeth is reported to be 80.3-94.7% at 1-3 years in healthy or reversibly inflamed pulps.16,30,33,34
Suggested decision tree encompassing options for managing deep caries. Note that, upon pulp exposure where bleeding is uncontrollable, further pulp is resected until controllable bleeding is reached, suggesting 'healthy' tissue. Partial or full pulpotomy procedures are now an option. Where 'healthy' tissue is never reached, pulpectomy and conventional endodontics is indicated
Direct pulp cap: patient presented with worsening sensitivity to cold following attempted indirect pulp cap. The tooth was initially restored with interim GIC as part of a stepwise excavation technique; however, the patient presented with worsening sensitivity to cold, but no spontaneous pain. Clinical diagnosis: reversible pulpitis 26. a) Initial presentation of secondary caries under a deep composite. b) Presence of soft caries centrally after GIC removal. c) Soft dentine remained over pulp chamber. d) Removal of soft dentine resulted in exposure showing hyperaemic pulp. e) Partial pulpotomy performed using sterile bur to depth of around 2 mm. f) Control of bleeding achieved following application of 2.5% sodium hypochlorite on a cotton wool pellet for five minutes. g) Application of MTA directly to pulp. h) Application of GIC over MTA. i) Use of bulk-fill composite. j) Final application of definitive capping composite restoration. k) Post-operative radiograph showing direct pulp cap at six months (images courtesy of Luca Moranzoni and Jonathan Cowie)
Partial and full pulpotomy
Pulpotomy procedures using calcium hydroxide (Ca[OH]2) were first described by Bernhard Hermann in 1920.35 Cvek recognised that only part of the coronal pulp required excising and first described the 'partial pulpotomy' for traumatised incisors in 1978 (now known as the 'Cvek' pulpotomy),36 which was later translated into carious exposures in 1993.37 Pulpotomy techniques now have a large body of evidence showing clinical success.3,38,39,40,41,42,43,44,45 Similar success rates for pulpotomies and pulpectomy followed by subsequent root filling have been identified,41 making pulpotomy techniques a viable alternative.
Definitions for partial or full pulpotomies are described in Table 2. The rationale for pulpotomy is that cariously exposed pulps may be contaminated by bacteria, as well as other debris from the caries removal process, and it aims to remove inflamed, necrosing or necrotic pulp tissue, leaving a healthy, functioning pulp with a regenerative capacity.25
Aguilar and Linsuwanont (2011) completed a meta-analysis looking at DPCs and partial and full pulpotomies using CSCs.3 In the short term (6-12 months), all three approaches were successful (87.5-97.6%), but in the longer term (>3 years), pulpotomy (full or partial) was more successful. This emphasises the need to consider resecting to healthy pulp once exposed and, although it may be counter-intuitive for such a procedure, it may be better to be slightly less conservative in pulp tissue removal.
Despite some studies finding parity between CSCs and Ca(OH)2 when used for pulpotomies,25 there is emerging evidence that CSCs offer superior outcomes in the longer term, including cases where there are signs of irreversible pulpitis.43 Success of full pulpotomy procedures using CSCs is reported to be 92-95% in healthy pulps or those with reversible pulpitis at one year40 and 71.3-95% in teeth with either reversible or irreversible pulpitis at 1-5 years.39,41,42,46 Interestingly, one study found no difference in outcome (in terms of maintaining pulp vitality) between pre-operative reversible and irreversible pulpitis for pulpotomy procedures.38 Partial pulpotomy success in teeth with pre-operative reversible or irreversible pulpitis is reported to be 85-98.4% at 1-2 years.24,43,44 The use of a definitive full pulpotomy in cases of irreversible pulpitis has an increasing evidence base behind it and shows potential as an alternative to conventional endodontics.4
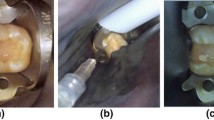
As with DPCs, haemorrhage should be controlled using a cotton wool pellet (soaked in 0.5-5% sodium hypochlorite) (Figures 1 and 3). Where haemorrhage cannot be controlled within five minutes, further pulp tissue may be removed using sterile burs under rubber dam, progressing from a partial pulpotomy to a complete pulpotomy. This may also be considered where there are signs or symptoms of irreversible pulpitis.2 Certainly where 'moderate pulpitis' is identified (Table 1),11 these are good candidates for pulpotomy, providing haemorrhage can be controlled.
Full pulpotomy: clinical diagnosis of irreversible pulpitis 26. a) Periapical radiograph showing deep caries under onlay 26 with possible slight apical radiolucency palatal root. b) Presentation following gross caries removal with soft dentine remaining over pulp. c) Pulp exposure following hand excavation. d, e) Bleeding could not be controlled within five minutes using microbrush soaked in 2.5% hypochlorite so a full pulpotomy was completed until healthy vital pulp was reached. f) Six-month review periapical radiograph following full pulpotomy, showing the preservation of tooth tissue compared to conventional endodontics. g) Twelve-month review periapical radiograph showing no increase in apical radiolucency. Tooth has remained symptom-free (images courtesy of Luca Moranzoni and Jonathan Cowie)
In all cases, a CSC should be placed directly onto the pulp tissue.2 Again, considering the importance of bacterial contamination, a definitive restoration should be placed as soon as possible to prevent bacterial ingress.
Material considerations
Given that the prevention of subsequent bacterial ingress is considered to be a key determinant in maintaining pulp vitality,17,18 dentine bridge formation, dentine bonding and solubility will all be important considerations in material selection for VPT. Biocompatible materials that will promote pulpal healing are required. Ca(OH)2 and CSCs have been used with varying degrees of success. Ca(OH)2 was initially established as the material of choice for DPCs because of its inhibition of bacterial growth and stimulation of reparative dentine.47,48,49,50,51,52,53 More recently, CSCs have emerged as a more predictable alternative.
Calcium silicate cements
MTA was introduced as a root-end filling material over 25 years ago and was largely based on Portland cement consisting of calcium oxide, silicon dioxide and bismuth oxide.54 Once hydrated, they release Ca(OH)2,55 accounting for their high pH.56 Once set, they develop high compressive strength57 and are considered to be of low solubility,56 in contrast to Ca(OH)2 (Table 3).
CSCs have excellent sealing ability, especially compared to Ca(OH)2, which may be important in preventing the ingress of microorganisms.58,59 CSCs are considered moderately antibacterial, mainly against facultative anaerobes,56 and are reported to be of higher biocompatibility than Ca(OH)2.60
A number of studies have found the dentine bridge in DPCs forms more quickly and is thicker with less tunnel defects where CSCs are used compared to Ca(OH)2.54,60,61,62,63,64,65,66 This dentine bridge may help prevent bacterial ingress,67 and may therefore help explain the increasing failure of Ca(OH)2 DPCs observed over time.16,23,30,68,69 CSCs also induce less prolonged and lower levels of pulp inflammation and necrosis during healing compared to Ca(OH)2.51,54,60,63,64,65,66
Newer synthetic CSCs have similar properties to MTA, but have refined the constituents to improve their mechanical and handling properties. This results in a higher sheer bond strength,70 foregoing some of the disadvantages of MTA, such as the long setting time. The bismuth oxide in earlier MTA materials was reported to cause significant discolouration, but newer synthetic CSCs (for example, Biodentine [Septodont, St Maur-des-Fossés, France]) have been reported to cause less tooth discolouration.71,72,73,74 Alterations in composition mean that there are now a wide range of CSCs available for a number of applications.
One concern of VPTs with CSCs is the perceived problems of re-access because of pulp sclerosis, given that they actively encourage the formation of a dentine barrier. Subsequent endodontics may therefore be more challenging.
Materials and treatment outcome
For DPCs, there is significant evidence that MTA or CSCs perform better than Ca(OH)2 both histologically and in terms of the maintenance of vitality. Success of DPCs using Ca(OH)2 has been reported to range from 21.3-80.1% at 1-13 years.24,68,69
Despite difficulties undertaking trials for a relatively rare and unplanned event, two recent randomised controlled trials have demonstrated a statistically significant improved outcome for MTA compared to Ca(OH)2 for DPCs at 1-3 years,30,34 and a recent systematic review concluded that there is now strong evidence for CSC's superiority over Ca(OH)2.75 Overall, considering all available evidence, there is sufficient evidence to recommend CSCs ahead of Ca(OH)2 for DPCs.3,16,22,23,30,34,68,69,76,77,78 There is emerging evidence that newer CSCs and traditional MTA perform similarly for DPCs, which is not surprising due to their fundamental similarities. A recent study found no significant difference between MTA and Biodentine up to three years (Biodentine success = 91.7%, MTA success = 96.0%).79
Evidence for pulpotomies is less clear. Two randomised controlled trials considering radiographic and clinical findings found no significant difference between Ca(OH)2 and MTA used for pulpotomies in permanent molars with healthy pulps or reversible pulpitis,80,81 and a recent meta-analysis found no significant difference between Ca(OH)2 and MTA in mature teeth, with both materials having favourable outcomes.82 However, in mature molars with irreversible pulpitis, a recent randomised controlled trial found a superior success rate using the partial pulpotomy technique with MTA over Ca(OH)2.43 The latest European Society of Endodontology (ESE) position statement recommends using CSCs for complete or partial pulpotomies.2
Prognostic considerations in VPT
Pulp exposures may be categorised as:
-
1.
Type 1 - traumatic, iatrogenic/mechanical, carious exposure through sound dentine with no pre-operative deep caries, in which case the pulp will not be significantly inflamed; or
-
2.
Type 2 - carious exposure through deep caries, where there is an assumption that there is more extensive inflammatory change.2,83
There is conflicting evidence around the significance of the type of exposure on the outcome of VPT.36,38,69,84,85,86 Although the type of exposure may affect prognosis, operative technique must always include rubber dam isolation and disinfection with sodium hypochlorite.
The location of the exposure is also an important determinant, with better success reported in occlusal rather than proximal exposures.28,34,85,86
Age may also be an important prognostic indicator for the success of VPTs, more so than for deep caries management using indirect pulp caps (IPCs), selective caries removal or stepwise excavation.87 Teeth may respond differently to VPT depending on their maturity, vascularity and degree of previous degeneration.86 The older a permanent tooth, the more secondary and potentially tertiary dentine is present in the pulp. Allied with an increased pulpal fibrosity, this results in a reduced blood supply, which is considered key to its regenerative capacity.1,88,89 How this translates into clinical outcomes has been debated, but there is considerable evidence suggesting decreasing success with age.24,33,83,84,90 It is acknowledged that other studies have not identified this trend.17,42
ESE guidelines for VPT recommend attempting to control haemorrhage using a cotton pellet soaked in 0.5-5% sodium hypochlorite (first choice) or 0.2-2% chlorhexidine for five minutes.2 The five-minute guideline is derived from expert opinion, but there is evidence that inability to control bleeding may lead to decreased success in DPCs,12 reinforcing the need to use direct clinical observation in diagnosis and decision-making. The use of sodium hypochlorite or chlorhexidine aims to control bleeding while also disinfecting the dentine and superficial pulp. Again, there is no robust evidence to support this recommendation, but it has become established practice in published research.
Follow-up
A successful VPT procedure is defined as 'absence of symptoms and maintenance of pulp vitality after at least one year'.2 The ESE recommend a 6- and 12-month review following any VPT procedure, after which annual review is recommended for up to four years, if required. This should include history taking, sensibility testing and radiography to identify any periapical periodontitis. This almost aligns with FGDP selection criteria for endodontic radiography.91 Radiographs may be considered, even where teeth are symptom-free, with additional periapical pathology identified despite the assumption of success.18 In the future, limited field CBCT may be of use for more comprehensive evaluation of the periapical status following management of deep caries with GIC and Biodentine for IPCs;92 however, there must be clear and strong justification for the increased radiation exposure with a net benefit to the patient (that is, a likely change in treatment approach).8,93
Caution must be applied to pulp testing in teeth that have received a full pulpotomy, as they may not respond in a similar way to adjacent or contralateral teeth to electric pulp testing or cold thermal tests. As a result, studies evaluating the outcome of pulpotomies tend to rely more on radiography and CBCT. Caution should also be applied to the assessment of colour, given that CSCs are capable of discolouring teeth to variable degrees,56 albeit less than traditional MTA.
Conclusion
VPTs using CSCs should be recommended as first-line treatments for frank exposures of the vital dental pulp, when isolation of the tooth is possible and bleeding can be controlled. Where symptoms are suggestive of irreversible pulpitis, exposing the pulp and cutting back to healthy pulp tissue before placing a CSC is a viable alternative to conventional pulpectomy and endodontics. However, long-term outcome studies are required to provide robust evidence to support VPT in addition to the opinion and guidance of specialist societies.
References
Trope M. Regenerative potential of dental pulp. J Endod 2008; 34(7 Suppl): S13-S17.
Duncan H F, Galler K M, Tomson P L et al. European Society of Endodontology position statement: Management of deep caries and the exposed pulp. Int Endod J 2019; 52: 923-934.
Aguilar P, Linsuwanont P. Vital pulp therapy in vital permanent teeth with cariously exposed pulp: a systematic review. J Endod 2011; 37: 581-587.
Cushley S, Duncan H F, Lappin M J et al. Pulpotomy for mature carious teeth with symptoms of irreversible pulpitis: A systematic review. J Dent 2019; 88: 103158.
Li Y, Sui B, Dahl C et al. Pulpotomy for carious pulp exposures in permanent teeth: A systematic review and meta-analysis. J Dent 2019; 84: 1-8.
Ng Y L, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: Part 1: Periapical health. Int Endod J 2011; 44: 583-609.
Ng Y-L, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: part 2: tooth survival. Int Endod J 2011; 44: 610-625.
Patel S, Durack C, Abella F et al. European Society of Endodontology position statement: The use of CBCT in Endodontics. Int Endod J 2014; 47: 502-504.
American Association of Endodontists. Endodontic Diagnosis. 2013. Available at https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/07/endodonticdiagnosisfall2013.pdf (accessed March 2020).
Hashem D, Mannocci F, Patel S et al. Clinical and radiographic assessment of the efficacy of calcium silicate indirect pulp capping: a randomized controlled clinical trial. J Dent Res 2015; 94: 562-568.
Wolters W J, Duncan H F, Tomson P L et al. Minimally invasive endodontics: a new diagnostic system for assessing pulpitis and subsequent treatment needs. Int Endod J 2017; 50: 825-829.
Matsuo T, Nakanishi T, Shimizu H, Ebisu S. A clinical study of direct pulp capping applied to carious-exposed pulps. J Endod 1996; 22: 551-556.
Bailey O, O'Connor C. Papilla management in sub-gingival, interproximal, direct composite restoration: A key concept to success. Br Dent J 2019; 226: 933-937.
Bogen G, Kim J S, Bakland L K. Direct pulp capping with Mineral Trioxide Aggregate: An observational study. J Am Dent Assoc 2008; 139: 305-315.
Caliskan M K, Guneri P. Prognostic factors in direct pulp capping with mineral trioxide aggregate or calcium hydroxide: 2-to 6-year follow-up. Clin Oral Investig 2017; 21: 357-367.
Hilton T J, Ferracane J L, Mancl L. Comparison of CaOH with MTA for Direct Pulp Capping: A PBRN Randomized Clinical Trial. J Dent Res 2013; 92: S16-S22.
Mente J, Geletneky B, Ohle M et al. Mineral trioxide aggregate or calcium hydroxide direct pulp capping: an analysis of the clinical treatment outcome. J Endod 2010; 36: 806-813.
Murray P E, Hafez A A, Smith A J, Cox C F. Bacterial microleakage and pulp inflammation associated with various restorative materials. Dent Mater 2002; 18: 470-478.
Kakahashi S, Stanley H S, Fitzgerald R J. The effects of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surg 1965; 20: 340-349.
Farges J C, Alliot-Licht B, Renard E et al. Dental pulp defence and repair mechanisms in dental caries. Mediators Inflamm 2015; DOI: 10.1155/2015/230251.
Stanley H R. Criteria for standardizing and increasing credibility of direct pulp capping studies. Am Dent J 1998; 1: 17-34.
Li Z, Cao L, Fan M, Xu Q. Direct Pulp Capping with Calcium Hydroxide or Mineral Trioxide Aggregate: A meta-analysis. J Endod 2015; 41: 1412-1417.
Dammaschke T, Leidinger J, Schafer E. Long-term evaluation of direct pulp capping-treatment outcomes over an average period of 6.1 years. Clin Oral Investig 2010; 14: 559-567.
Mejàre I, Cvek M. Partial pulpotomy in young permanent teeth with deep carious lesions. Endod Dent Traumatol 1993; 9: 238-242.
Chailertvanitkul P, Paphangkorakit J, Sooksantisakoonchai N et al. Randomized controlled trial comparing calcium hydroxide and mineral trioxide aggregate for partial pulpotomies in cariously exposed pulps of permanent molars. Int Endod J 2014; 47: 835-842.
Bogen G, Kim J S, Bakland L K. Direct pulp capping with mineral trioxide aggregate: an observational study. J Am Dent Assoc 2008; 139: 305-315.
Parinyaprom N, Nirunsittirat A, Chuveera P. Outcomes of direct pulp capping using either ProRoot mineral trioxide aggregate or biodentine in permanent teeth with carious pulp exposure in 6-to 18-year-old patients: A randomized controlled trial. J Endod 2018; 44: 341-348.
Schroder U. Effects of Calcium Hydroxide-containing Pulp-capping Agents on Pulp Cell Migration, Proliferation, and Differentiation. J Dent Res 1985; 64: 541-548.
Hilton T J. Keys to clinical success with pulp capping: A review of the literature. Oper Dent 2009; 34: 615-625.
Kundzina R, Stangvaltaite L, Eriksen H M, Kerosuo E. Capping carious exposures in adults: a randomized controlled trial investigating mineral trioxide aggregate versus calcium hydroxide. Int Endod J 2017; 50: 924-932.
Grech L, Mallia B, Camilleri J. Investigation of the physical properties of tricalcium cilicate cement-based root-end filling materials. Dent Mater 2013; 29: 20-28.
Mente J, Hufnagel S, Leo M et al. Treatment outcome of Minteral Trioxide Aggregate or Calcium Hydroxide Direct Pulp Capping: Long-term results. J Endod 2014; 40: 1746-1751.
Marques M S, Wesselink P R, Shemesh H. Outcome of direct pulp capping with mineral trioxide aggregate: A prospective study. J Endod 2015; 41: 1026-1031.
Suhag K, Duhan J, Tewari S, Sangwan P. Success of direct pulp capping using mineral trioxide aggregate and calcium hydroxide in mature permanent molars with pulps exposed during carious tissue removal: 1-year follow-up. J Endod 2019; 45: 840-847.
Hermann B. Calcium hydroxyd als mitten zum behandeln und fullen von Wurzelkanallen. Würzburg: University of Würzburg, 1920. Dissertation.
Cvek M. A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture. J Endod 1978; 4: 232-237.
Mcjare I, Cvek M. Partial pulpotomy in young permanent teeth with deep carious lesions. Endod Dent Traumatol 1993; 9: 238-242.
Asgary S, Hassanizadeh R, Torabzadeh H, Eghbal M J. Treatment outcomes of 4 vital pulp therapies in mature molars. J Endod 2018; 44: 529-535.
Asgary S, Eghbal M J, Bagheban A A. Long-term outcomes of pulpotomy in permanent teeth with irreversible pulpitis: A multi-centre randomized controlled trial. Am J Dent 2017; 30: 151-155.
Asgary S, Eghbal M J. Treatment outcomes of pulpotomy in permanent molars with irreversible pulpitis using biomaterials: A multi-centre randomized controlled trial. Acta Odontol Scand 2013; 71: 335-341.
Galani M, Tewari S, Sangwan P, Mittal S, Kumar V, Duhan J. Comparative evaluation of postoperative pain and success rate after pulpotomy and root canal treatment in cariously exposed mature permanent molars: A randomized controlled trial. J Endod 2017; 43: 1953-1962.
Linsuwanont P, Wimonsutthikul K, Pothimoke U, Santiwong B. Treatment outcomes of mineral trioxide aggregate pulpotomy in vital permanent teeth with carious pulp exposure: The retrospective study. J Endod 2017; 43: 225-230.
Taha N A, Khazali M A. Partial Pulpotomy in Mature Permanent Teeth with Clinical Signs Indicative of Irreversible Pulpitis: A Randomized Clinical Trial. J Endod 2017; 43: 1417-1421.
Kang C M, Sun Y, Song J S et al. A randomized controlled trial of various MTA materials for partial pulpotomy in permanent teeth. J Dent 2017; 60: 8-13.
Tan S Y, Yu V S H, Lim K C et al. Long-term pulpal and restorative outcomes of pulpotomy in mature permanent teeth. J Endod 2020; 46: 383-390.
Asgary S, Eghbal M J, Fazlyab M, Baghban A A, Ghoddusi J. Five-year results of vital pulp therapy in permanent molars with irreversible pulpitis: A non-inferiority multicentre randomized clinical trial. Clin Oral Investig 2015; 19: 335-341.
Kim D, Kim E. Antimicrobial effect of calcium hydroxide as an intracanal medicament in root canal treatment: a literature review - Part II. in vivo studies. Restor Dent Endod 2015; 40: 97-103.
Prosser H J, Groffman D M, Wilson A D. The effect of composition on the erosion properties of calcium hydroxide cements. J Dent Res 1982; 61: 1431-1435.
Pacios M G, Silva C, Lopez M E, Cecilia M. Antibacterial action of calcium hydroxide vehicles and calcium hydroxide pastes. J Investig Clin Dent 2012; 3: 264-270.
Estrela C, Sidney G B, Bammann L L, Felipe Jr O. Mechanism of action of calcium and hydroxyl ions of calcium hydroxide on tissue and bacteria. Braz Dent J 1995; 6: 85-90.
Accorinte L, Holland R, Reis A et al. Evaluation of mineral trioxide aggregate and calcium hydroxide cement as pulp-capping agents in human teeth. J Endod 2008; 34: 1-6.
Tomson P L, Lumley P J, Smith A J, Cooper P R. Growth factor release from dentine matrix by pulp-capping agents promotes pulp tissue re-air-associated events. Int Endod J 2017; 50: 281-292.
Tomson P L, Grover L M, Lumley P J, Sloan A J, Smith A J, Cooper P R. Dissolution of bio-active dentine matrix components by mineral trioxide aggregate. J Dent 2007; 35: 636-642.
Eskandarizadeh A, Shahpasandzadeh M H, Shahpasandzadeh M, Torabi M, Parirokh M. A comparative study on dental pulp response to calcium hydroxide, white and grey mineral trioxide aggregate as pulp capping agents. J Conserv Dent 2011; 14: 351-355.
Camilleri J, Montesin F E, Brady K, Sweeny R, Curtis R V, Pitt Ford T R. The constitution of mineral trioxide aggregate. Dent Mater 2005; 21: 297-303.
Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review - Part I: chemical, physical, and antibacterial properties. J Endod 2010; 36: 16-27.
Torabinejad M, Hong C U, Mcdonald F, Pitt Ford T R. Physical and chemical properties of a new root-end filling material. J Endod 1995; 21: 349-353.
Al-Hezaimi K, Naghshbandi J, Oglesby S, Simon J H S, Rotstein I. Human saliva penetration of root canals obturated with two types of mineral trioxide aggregate cements. J Endod 2005; 31: 453-456.
Ferk Luketic S, Malcic A, Jukic S, Anic I, Segovic S, Kalenic S. Coronal microleakage of two root-end filling materials using a polymicrobial marker. J Endod 2008; 34: 201-203.
Aeinehchi M, Eslami B, Ghanbariha M, Saffar A S. Mineral trioxide aggregate (MTA) and calcium hydroxide as pulp-capping agents in human teeth: a preliminary report. Int Endod J 2003; 36: 225-231.
Nowicka A, Wilk G, Lipski M, Kolecki J, Buczkowska-Radlinska J. Tomographic evaluation of reparative dentine formation after direct pulp capping with Ca(OH)2, MTA, Biodentine, and dentine bonding system in human teeth. J Endod 2015; 41: 1234-1240.
Min K, Park H, Lee S et al. Effect of mineral trioxide aggregate on dentin bridge formation and expression of dentin sialoprotein and haem oxygenase-1 in human dental pulp. J Endod 2008; 34: 666-670.
Parolia A, Kundabala M, Rao N N et al. Comparative histological analysis of human pulp following direct pulp capping with Propolis, mineral trioxide aggregate and Dycal. Aust Dent J 2010; 55: 59-64.
Sawicki L, Pameijer C, Emerich K, Adamowicz-Klepalska B. Histological evaluation of mineral trioxide aggregate and calcium hydroxide in direct pulp capping of human immature permanent teeth. Am J Dent 2008; 21: 262-266.
Nair P N R, Duncan H F, Pitt ford T R, Luder H U. Histological, ultrastructural and quantitative investigations on the response of healthy human pulps to experimental capping with mineral trioxide aggregate: A randomized controlled trial. Int Endod J 2009; 42: 422-444.
Swarup S J, Rao A, Boaz K, Srikant N, Shenoy R. Pulpal response to nano hydroxyapatite, mineral trioxide aggregate and calcium hydroxide when used as a direct pulp capping agent: an in vivo study. J Clin Pediatr Dent 2014; 38: 201-206.
Kitasako Y, Ikeda M, Tagami J. Pulpal responses to bacterial contamination following dentin bridging beneath hard-setting calcium hydroxide and self-etching adhesive resin system. Dent Traumatol 2008; 24: 201-206.
Willershausen B, Willershausen I, Ross A, Velikonja S, Kasaj A, Blettner M. Retrospective study on direct pulp capping with calcium hydroxide. Quintessence Int 2011; 42: 165-171.
Barthel C R, Rosenkranz B, Leuenberg A, Roulet J F. Pulp capping of carious exposures: treatment outcome after 5 and 10 years: a retrospective study. J Endod 2000; 26: 525-528.
Kaup M, Dammann C H, Schafer E, Dammaschke T. Shear bond strength of Biodentine, ProRoot MTA, glass ionomer cement and composite resin on human dentine ex vivo. Head Face Med 2015; 11: 14.
Camilleri J. Staining potential of Neo MTA Plus, MTA Plus and Biodentine used for pulpotomy procedures. J Endod 2015; 41: 1139-1145.
Keskin C, Demiryurek E O, Ozyurek T. Colour stabilities of calcium silicate-based materials in contact with different irrigation solutions. J Endod 2015; 41: 409-411.
Beatty H, Svec T. Quantifying coronal tooth discolouration caused by Biodentine and EndoSequence root repair material. J Endod 2015; 41: 2036-2039.
Marciano M A, Costa R M, Camilleri J, Mondelli R F, Guimarães B M, Duarte M A. Assessment of colour stability of white mineral trioxide aggregate angelus and bismuth oxide in contact with tooth structure. J Endod 2014; 40: 1235-1240.
Edwards D C, Burns L, Witton R, Tredwin C. MTA or calcium hydroxide for direct pulp capping in fully developed permanent teeth: a systematic review. ENDO 2020; 14: 91-102.
Schwendicke F, Brouwer F, Stolpe M. Calcium Hydroxide versus Mineral Trioxide Aggregate for Direct Pulp Capping: A Cost-effectiveness Analysis. J Endod 2015; 41: 1969-1974.
Zhu C, Ju B, Ni R. Clinical outcome of direct pulp capping with MTA of calcium hydroxide: a systematic review and meta-analysis. Int J Clin Exp Med 2015; 8: 17055-17060.
Akhlaghi N, Khademi A. Outcomes of vital pulp therapy in permanent teeth with different medicaments based on review of the literature. Dent Res J 2015; 12: 406-417.
Awawdeh L, Al-Qudah A, Hamouri H, Chakra R J. Outcomes of vital pulp therapy using Mineral Trioxide Aggregate or Biodentine: A prospective randomised controlled trial. J Endod 2018; 44: 1603-1609.
Kumar V, Juneja R, Duhan J, Sangwan P, Tewari S. Comparative evaluation of platelet-rich fibrin, mineral trioxide aggregate, and calcium hydroxide as pulpotomy agents in permanent molars with irreversible pulpitis: A randomized controlled trial. Contemp Clin Dent 2016; 7: 512-518.
Özgür B, Uysal S, Güngör H C. Partial pulpotomy in immature permanent molars after carious exposures using different haemorrhage control and capping materials. Pediatr Dent 2017; 39: 364-370.
Alqaderi H, Lee C T, Borzangy S, Pagonis T C. Coronal pulpotomy for cariously exposed permanent posterior teeth with closed apices: A systematic review and meta-analysis. J Dent 2016; 44: 1-7.
Bjørndal L, Demant S, Dabelsteen S. Depth and activity of carious lesions as indicators for the regenerative potential of dental pulp after intervention. J Endod 2014; 40(4 Suppl): S76-S81.
Horsted P, Sandergaard B, Thylstrup A, El Attar K, Fejerskov O. A retrospective study of direct pulp capping with calcium hydroxide compounds. Endod Dent Traumatol 1985; 1: 29-34.
Al-Hiyasat A S, Barrieshi-Nusair K M, Al-Omari M A. The radiographic outcomes of direct pulp-capping procedures performed by dental students: a retrospective study. J Am Dent Assoc 2006; 137: 1699-1705.
Cho S Y, Seo D G, Lee S J et al. Prognostic factors for clinical outcomes according to time after direct pulp capping. J Endod 2013; 39: 327-331.
Bjørndal L, Fransson H, Bruun G et al. Randomized clinical trials on deep carious lesions: 5-year follow-up. J Dent Res 2017; 96: 747-753.
Goodis H E, Kahn A, Simon S. Aging and the pulp. In Hargreaves K M, Goodis H E, Tay F R (eds) Seltzer and Bender's Dental Pulp. 2nd ed. Berlin: Quintessence, 2012.
Ricketts D. Management of the deep carious lesion and the vital pulp dentine complex. Br Dent J 2001; 191: 606-610.
Miles J P, Gluskin A H, Chambers D, Peters O A. Pulp capping with Mineral Trioxide Aggregate (MTA): a retrospective analysis of carious pulp exposures treated by undergraduate students. Oper Dent 2010; 35: 20-28.
FGDP (UK). FGDP selection criteria for dental radiography standards. 2018. Available online at https://www.fgdp.org.uk/selection-criteria-dental-radiography (accessed January 2020).
Hashem D, Mannocci F, Patel S, Manoharan A, Watson T F, Banerjee A. Evaluation of the efficacy of calcium silicate vs. glass ionomer cement indirect pulp capping and restoration assessment criteria: a randomised controlled clinical trial-2-year results. Clin Oral Investig 2019; 23: 1931-1939.
Rushton V E. Justification of CBCT and guidelines for clinical use. 2011. Available at http://www.sedentexct.eu/system/files/Dr%20Rushton.pdf (accessed March 2020).
Acknowledgements
Thank you to Luca Moranzoni and Jonathan Cowie for supplying the pictures of the clinical cases.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare no conflict of interests.
Rights and permissions
About this article
Cite this article
Edwards, D., Stone, S., Bailey, O. et al. Preserving pulp vitality: part two - vital pulp therapies. Br Dent J 230, 148–155 (2021). https://doi.org/10.1038/s41415-020-2599-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-020-2599-y
- Springer Nature Limited
This article is cited by
-
Pulp therapy and root canal treatment techniques in immature permanent teeth: an update
British Dental Journal (2022)