Abstract
Aim It is the aim of this paper to consider whether overall patient treatment history per se and what length of patient history, matters in predicting future treatment need.
Methods This study used a data set (SN7024, available from UKDataService), consisting of treatment records for General Dental Services' (GDS) patients, this being obtained from all items of service payment records for patients treated in the GDS of England and Wales between 1990 and 2006. For the purpose of this study, the GDS dataset for patients attending in 2003 was restricted to adult patients (aged 18 or over on 31 December 1990; that is, year of birth earlier than 1973) who attended in both two-year periods 1991/2 and 2004/5. Each course of treatment was classified as 'active' (eg restoration, extraction, prosthesis) or 'not active' (eg prevention, diagnosis). Treatment costs for 2001-2005 (outcome), 2000 (one-year history), 1999-2000 (two-year history) and so on until 1991-2000 (ten-year history) were determined, and history and outcome correlated.
Results A total of 455,844 patients met the inclusion criteria, namely adults with a full history. They received 9,341,583 courses of treatment, of which 49% were classified as 'active' and 51% as 'not active'. The analysis indicated that both total costs and active treatment costs are positively correlated with their historical values, with the correlation coefficients increasing from 0.24 and 0.25 with one year of history to 0.42 and 0.44 with ten years of history. Overall, therefore, future treatment cost is correlated with past treatment costs.
Conclusions Treatment history may provide an important correlate of future dental treatment needs and the more history the better, at least up to five years. However, active treatment is the important component and should be distinguished from preventive and diagnostic treatments.
Similar content being viewed by others
Key points
-
A variety of organisations and/or persons may be interested in the prediction of future treatment need, but there has been a paucity of information on this subject.
-
This study analysed a dataset which included 455,844 adult patients with a full 15-year treatment history who attended in two two-year periods (1991/2 and 2004/5). Over 9 million courses of treatment were included, with each course of treatment being classified as 'active' (e.g restorations, prostheses, extractions) or 'non-active' (e.g examination, radiographs, prevention).
-
The results indicated that treatment history is an important correlate of future dental treatment needs and that 'active' treatment history is the more important component.
Introduction
The prediction of future treatment need has been a conundrum for clinicians, administrators/governments and indeed for patients, for as long as dental treatment has been funded. The perceived wisdom has been that previous treatment is as good an indicator for future treatment need as is available, but there is a paucity of research to determine whether this is indeed fact. It may be considered that the patient's treatment history gives information additional to other predictors, such as symptoms, lifestyle and diet, while the patient's genetic inheritance may also be of influence.
A variety of organisations and/or persons might be interested in the prediction of future treatment need, this being the total treatment need rather than the treatment of individual teeth; for example:
Dentists planning business and/or valuing practices
Insurance or capitation companies setting premiums
Health service planners anticipating population needs and future costs
Patients considering different payment plans.
In addition, at a practice level, the ability to accurately predict future treatment need will enable dentists to tailor the recall frequency for an individual patient and establish appropriate preventive programmes where needed, and to ensure that an appropriate number of clinicians are employed to treat the perceived treatment need. In addition, there may be situations when a dentist predominantly evaluates and treats new patients, providing them with a substantial course of treatment which is 'guaranteed' for a number of years, or for which it is anticipated that no or minimal treatment will be required thereafter for a number of years. In such conditions, it would be expected that there would be a negative correlation between treatment provided and future treatment need. However, it could be anticipated that, if a sufficiently large dataset is utilised (as in the present study [vide infra]) such negative correlations will be included within the main cohort of regularly attending patients.
Worthington and colleagues from Manchester (UK)1 were among the earliest to attempt to find correlates for future treatment needs of patients. They recruited 24 general dentists in the area to take part in a prospective longitudinal study into the dental health of regularly attending dentate adult patients, with each dentist recruiting c.200 patients. Clinical and demographic information was collected for each patient and, after rendering each patient dentally fit, the dentists examined each patient 12 months later, with all restorations and extractions that each patient received during that period being recorded. Upon recruitment, the patients were asked to complete a questionnaire which included questions relating to their own predicted need for treatment during the following 12 months; the dentists' observations were also recorded. The authors concluded from the results (which included data on 4,211 patients who were examined at baseline) that, although the models that they developed were probably not sufficiently discriminatory, the patients' and the dentists' own predictions of future treatment need were as good as any of the other factors investigated.
Bibby and Shern2 reported the discussions of a conference held in 1977, with the need for an accurate prediction model for caries prediction being considered desirable, and the participants 'generally agreeing' that prior caries experience and number of tooth surfaces at risk represented the best indicators of future caries experience. In addition, Abernathy and colleagues3 developed a prediction model in order to derive a method of predicting children at high risk of caries so that preventive measures could be instituted. They concluded that 'the validation of the model was positive and strengthened the applicability of the model in the field'.
Other than the above, there is a paucity of research into the factors influencing the overall influence of past treatment on future treatment need. However, other workers have evaluated factors associated with success/failure of specific treatment modalities. For example:
Fonzar and co-workers4 investigated prognostic factors affecting the long-term outcome of endodontic therapy over ten years in 1,175 endodontically treated teeth, treated by a single operator in private practice
Nagasiri and Chitmongkolsuk5 were able to correlate the amount of remaining tooth structure and type of restorative material with the longevity of endodontically treated molars without crown coverage
Kim6 examined the prevalence of apical periodontitis in a South Korean population, with the results indicating that inadequate root filling length was more predictive of treatment success than the presence of a crown on the root-filled tooth
Setzer et al.7 examined a clinical database of 42 patients and 50 molar endodontic treatments followed up for four years, with the authors concluding that 'it may be difficult to predict the prognosis of molars receiving endodontic treatment'
Alomari and colleagues from Kuwait University8 studied records of 826 patients (1,102 teeth) and used descriptive statistics to examine the association between restorative treatment and tooth loss. Teeth with no restorations or with crowns were significantly more likely to be extracted, 22% of the extractions were due to restoration failure, and teeth receiving multiple restorative therapies were also more likely to be extracted
Rinke and co-workers,9 in a practice-based study of 68 patients with a total of 323 zirconia crowns, observed these restorations for c.80 months, with the results indicating a lower survival rate for endodontically treated teeth than crowns placed on implants, and anterior crowns performing significantly more favourably than those on molar teeth
Scotti et al.,10 from the University of Turin, retrospectively evaluated the longevity of endodontically treated teeth restored with direct resin composite, with or without the insertion of fibre posts. A total of 247 patients (376 root-treated posterior teeth) were followed for three years, with the results indicating that the direct restorations with fibre posts performed better than those without fibre posts.
In addition, there have been a number of studies which evaluated the success of periodontal therapies; for example, those by Ng and co-workers in Singapore,11 with the authors concluding that the provision of periodontal maintenance led to minimal tooth loss due to periodontitis for a period of ten years, and Graetz and co-workers,12 with the authors aiming to identify long-term prognostic factors for the loss of molar teeth with different degrees of furcation involvement during periodontal therapy. Danniewitz and co-workers13 aimed to identify risk factors for loss of molar teeth during supportive periodontal therapy, retrospectively examining 136 patients (with 1,015 molars) and assessing treatment success over ten years. Finally, Pretzl and colleagues14 sought to assess the influence of endodontic status in patients under supportive periodontal therapy, and Nibali and co-workers15 retrospectively assessed tooth loss in a cohort of chronic periodontitis patients undergoing maintenance care in a UK private practice setting.
Even if the above research had produced accurate forecasts for individual patients, the costs of additional data collection are considerable and a more cost-effective method of forecasting at an aggregate level may therefore be considered desirable.
The question, therefore, generally remains unanswered; what is the relationship between patient treatment history and future treatment need? In addition, how does this vary with the length of available history, and how does this vary with the content of the history, in particular the distinction between active and non-active treatment?
Therefore, the purpose of this paper is to examine a historic NHS database in order to determine whether the data that it contains indicate that overall patient treatment history per se, and what length of patient history, is an indicator of future treatment need.
Methods
The evidence base
A dataset (SN7024, available from UKDataService)16 has been established, consisting of treatment records for General Dental Services' patients, this being obtained from all item of service payment records for patients treated in the GDS of England and Wales between 1990 and 2006. The source data, consisting of items obtained from the payment claims submitted by GDS dentists to the Dental Practice Board (DPB) in Eastbourne, Sussex, UK, contain the treatment records of an age-stratified sample of GDS patients defined by 20 different dates of birth in each year of birth, generating over a million different patients in each year from 1991 to 2005. Each record contains data about the patient, the dentist, the dates of the course of treatment and the postcode area of the dental practice where the treatment took place, together with detailed information about the treatment provided, down to the level of individual teeth.
The sample
For the purpose of this study, the GDS dataset for patients attending in 2003 was further restricted to adult patients (aged 18 or over on 31 December 1990; that is, year of birth earlier than 1973) who attended in both two-year periods 1991/2 and 2004/5. Each course of treatment was classified as (Table 1):
Active (eg restoration, extraction, prosthesis)
Not active (eg prevention, diagnosis.)
Total treatment costs for 2001-2005 (outcome), 2000 (one-year history), 1999-2000 (two-year history) and so on until 1991-2000 (ten-year history) were also determined, and history and outcome correlated.
Patients were classified by the dentist and postcode area relating to their last course of treatment (in 2004-2005).
Results
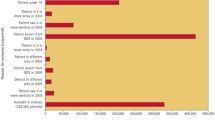
A total of 455,844 patients met the inclusion criteria, namely, adults with a full history. They received 9,341,583 courses of treatment, of which 49% were classified as 'active' and 51% as 'not active'. The analysis presented in Figure 1 shows history in years along the horizontal axis, and Pearson correlation coefficient of outcome treatment cost against history treatment cost on the vertical. The chart demonstrates that total costs are positively correlated, with the correlation coefficient increasing from 0.24 with one year of history to 0.42 with ten years of history. Overall, therefore, future treatment cost is correlated with past treatment costs.
Figure 2 presents a corresponding chart for courses of treatment containing active treatment, with the results indicating that there is a slightly higher correlation, from 0.25 to 0.44. Active treatment cost is therefore even more strongly correlated with past active treatment costs.
Figure 3 presents the correlation between active treatment outcome and history of non-active (that is, preventive) treatment. It is apparent that this correlation is negative (perhaps indicating that prevention works). As above, the correlation gets stronger with increased history, from -0.122 at one year to -0.176 at ten years.
Figure 4 presents the correlation between non-active history and non-active outcome. There is still a strong correlation, but it does not continue to strengthen if more years of history are added beyond the first five.
Figures 1 to 4 have presented the correlation, but is there an opportunity to predict future treatment need? Figure 5 presents a scatter diagram of individual patients. The horizontal axis shows the ten-year history cost for active courses of treatment and the vertical shows the corresponding five-year outcome cost. The scatter diagram indicates a significant correlation, but a wide scatter. Correlation at patient level is therefore statistically significant, but not good enough for reliable prediction at patient level.
Figure 6 presents aggregation to dentist level. In this case, all dentists with a minimum of 100 patients in the data were selected, showing mean active cost per patient. A tighter grouping emerges. There is an indication of slight nonlinearity and the fitted reference curve shown is an exponential one. Since the patient sample is only about 5% of the population, most dentists would have much larger patient populations, with a correspondingly stronger correlation between historical and future average costs per patient.
Figures 7 and 8 present dentists in a postcode area (there being 105 postcode areas in England and Wales, approximately the size of an old health authority). Here, there is a pattern which is useful for prediction and, additionally, if there is only one year of data, it is still possible to generate a useful predictive curve. Furthermore, only 5% of the data is included in the sample, so again a full set of data would provide greater predictive accuracy.
Indeed, at the sample aggregate level of dentist or postcode area, the correlation is much greater than for individual patients (>0.7). Even one year of history therefore can provide a good low-cost basis for predicting future costs at aggregate level.
Discussion
Being able to advise on future potential treatment need is important when advising patients, given the potential for adverse medico-legal situations in the UK, but also for administrators and funders of healthcare, especially those involved in capitation and/or insurance schemes. A review of the literature has indicated that there is a paucity of information on this subject.
Within the totality of patients, particular groups can be found where future costs should be negatively correlated with historical treatment costs. Examples include patients who have recently received a full clearance followed by full upper and lower dentures: high historical treatment costs, but low future maintenance costs. At an individual level, allowance can be made for such cases, but generalising is difficult. The point about this present work is that the overall positive correlations outweigh such particular cases and can still be used as a basis for aggregate prediction.
While dentists have long been known to vary in their treatment planning,17 the authors have assumed that clinicians have assessed each of their patients and carried out treatment from an ethical point of view. It may also be considered that the dentist providing long-term care for a given patient is in the best position to get to know that patient's oral condition and thereby be able to assess that patient's potential treatment needs. While the present work demonstrates that historical treatment costs are not a good basis for predicting treatment at an individual patient level, it does show that, at the level of a dental practice or health authority, the historical average amount of spend per patient could readily be translated into the amount of predicted spend in the future. The size of the dataset used in this evaluation is so large as to minimise variations in treatment planning and may be assumed to present a general picture of the prescribing of dental treatment in England and Wales at the time of the data collection. This ceased in 2006, but previous publications18,19 have demonstrated no change in restoration (of all types) survival rates over the period of data collection and, given that there are few changes in prescribing of treatment and dental materials since 2006, it appears that the dataset used in the present work can indeed provide the answer to the question: does treatment history provide a correlate for future treatment needs?
The dataset used patients who had complete records through the 15 years of the dataset, so that we could examine the effect of gradually increasing the amount of history used for possibly predicting the future. Therefore, patients who were selected were adults, and both attended at least once in the first two years and at least once in the last two years of the dataset. Having classified each course of treatment according to the treatment content as 'active' or 'non-active' (Table 1), we then used treatment costs as a measure of resources employed, adding these up for a five-year end period as outcome, and successively for one, two, three, cumulative years of history, subdivided by type of course of treatment. The selection process yielded almost half a million adults with full histories and, with over nine million courses of treatment, accordingly, the data may be considered robust. The results indicate that treatment history is indeed an important correlate of future dental treatment needs and, if the data are restricted to active courses of treatment, the association is even stronger. In that regard, it is active treatment, rather than non-active, which is the important component and therefore should be distinguished from preventive and diagnostic treatments, albeit that their value should not be underestimated. Despite these findings, however, it may be pertinent to add that, for patients with a history of high treatment need, it is never too late to seek to switch to preventively-orientated (rather than traditional intervention) care in the management of such patients.
Future active treatment costs are negatively correlated with historical non-active treatment costs; this may be considered reassuring, since this is consistent with the concept of preventive treatment. Although more history generally improves the correlation, for future non-active treatment costs, history beyond five years does not provide any additional improvement in the correlation. Indeed, treatment history of only one year on a smaller dataset may also provide a reasonable low-cost estimate of future treatment need, given the good correlation of one-year history aggregated to postcode area level.
The treatment costs used in this paper reflect the scale of fees used in the GDS, which was designed to represent the relative resource costs of different items of service, including both materials and labour. The scale of fees was reviewed each year and adjusted for inflation of each of its components. Inflation between two time periods does not affect the calculation of the coefficient of correlation, but future inflation certainly needs to be considered in any forecasting exercise. Inflation within a time period has other consequences. In particular, when cost totals are taken over several years, the earlier years have less influence and so their contribution may be understated. Conversely, the five-year outcome period considered in this work treatment in the last year is more highly priced than the same treatment would have been in the first year. The scatter diagrams reflect both inflation and changes in treatment volume, and they are illustrative rather than any attempt at a predictive model. However, they do show what actually happened over a defined time interval in the past, at a time when inflation, as reflected in the changes to the scale of fees, is well documented. They provide a proof of concept, from which further development can be taken forward.
Any operational development of a predictive model will of course require additional work and planning to allow for the treatment needs of new patients, who may be expected to exhibit very different short-term treatment needs. Forecasting the needs of the existing patient population will, however, reveal what remaining capacity is available, at practice and health authority level, to treat new entrants to the service, and so facilitate effective long-term planning for both individual dental practices and for the NHS in general.
Finally, the authors have used data which ceased to be collected in this form in 2006. They have previously argued20 that the data are robust at the present time. Indeed, analysis of the data, as presented in this paper, indicates how valuable the collection of even simplified summaries of tooth/patient/dentist/material data can be in allowing the prediction of future treatment needs.
At the time of writing, Units of Dental Activity are the means whereby dentists are remunerated within the NHS Dental Services in England and Wales, with the treatments being designated Band 1, 2 or 3. It may be considered that the treatments in Band 1 bear a remarkable resemblance to the definition of non-active treatment used in the present study, whereas Bands 2 and 3 contain active treatment modalities. It may therefore be considered that the present method of collection of data in the NHS Dental Services in England and Wales could readily be adapted to facilitate predictions of future treatment need from historical information.
Conclusions
Treatment history may provide an important correlate of future dental treatment needs, and the more history the better, at least up to five years. However, active treatment is the important component, and should be distinguished from preventive and diagnostic treatments. In addition, even one-year historical data may be sufficient for reliable forecasting at health authority level.
References
Worthington H V, Holloway P J, Clarkson J E, Davies R M. Predicting which adult patients will need treatment over the next year. Community Dent Oral Epidemiol 1997; 25: 273-277.
Bibby B G, Shern R J (eds) Methods of Caries Prediction. A special supplement of Microbiology Abstracts - Bacteriology. Washington D.C.: IRL Press, 1978.
Abernathy J R, Graves R C, Bohannan H M, Stamin J A, Greenberg B G, Disney J A. Development and application of a prediction model for dental caries. Community Dent Oral Epidemiol 1987; 15: 24-28.
Fonzar F, Fonzar A, Buttolo P, Worthington H V, Esposito M. The prognosis of root canal therapy: a 10-year retrospective cohort study on 411 patients with 1175 endodontically treated teeth. Eur J Oral Implantol 2009; 2: 201-208.
Nagasiri R, Chitmongkolsuk S. The influence of coronal restoration type on survival of endodontically treated teeth. Eur J Prosthodont Rest Dent 2004; 12: 171-176.
Kim S. Prevalence of apical periodontitis of root-canal treated teeth and retrospective evaluation of symptom-related prognostic factors in an urban South Korean population. Oral Surg Oral Med Oral Pathol Oral Radiol Oral Endod 2010; 110: 795-799.
Setzer F C, Boyer K R, Jeppson J R, Karabucak B, Kim S. Long-term prognosis of endodontically treated teeth: a retrospective analysis of preoperative factors in molars. J.Endod 2011; 37: 21-25.
Alomari Q D, Khalaf M E, Al-Shawaf N M. Relative contribution of restorative treatment to tooth extraction in a teaching institution. J.Oral Rehabil 2013; 40: 464-471.
Rinke S, Lange K, Roediger M, Gersdorff N. Risk factors for technical and biological complications with zirconia single crowns. Clin Oral Investig 2015; 19: 1999-2006.
Scotti N, Eruli C, Comba A et al. Longevity of class 2 direct restorations in root-filled teeth: A retrospective clinical study. J.Dent 2015; 43: 499-505.
Ng M C, Ong M M, Lim M P, Koh C G, Chan Y H. Tooth loss in compliant and non-compliant periodontally treated patients: 7 years after active periodontal therapy. J.Clin.Periodontol 2011; 38: 499-508.
Graetz C, Schutzhold S, Plaumann A et al. Prognostic factors for the loss of molars - an 18-years retrospective cohort study. J Clin Periodontol 2015; 42: 943-950.
Danniewitz B, Zeidler A, Husing J et al. Loss of molars in periodontally treated patients: results from 10 years and more after active periodontal therapy. J Clin Periodontol 2016; 43: 53-62.
Pretzl B, Eickholz P, Saure D, Pfefferle T, Zeidler A, Danniewitz B. Endodontic status and retention of molars in endodontically treated patients: results after 10 years or more of supportive periodontal therapy. J Clin Periodontol 2016; 43: 1116-1123.
Nibali L, Sun C, Akcali A, Meng X, Tu Y K, Donod N. A retrospective study on periodontal disease progression in private practice. J Clin Periodontol 2017; 44: 290-297.
Information Centre for Health and Social Care, NHS Business Services Authority. Longitudinal Dental Treatment, 1990-2006. 2012; DOI: 10.5255/UKDA-SN-7024-1.
Elderton R J, Nuttall N M. Variation among dentists in planning treatment. Br Dent J 1983; 154: 201-205.
Burke F J T, Lucarotti P S K. The ultimate guide to restoration longevity in England and Wales. Part 4: resin composite restorations: time to next intervention and to extraction of the restored tooth. Br Dent J 2018; 224: 945-956.
Burke F J T, Lucarotti P S K. The ultimate guide to restoration longevity in England and Wales. Part 5: crowns: time to next intervention and to extraction of the restored tooth. Br Dent J 2018;.225: 33-48.
Burke F J T, Lucarotti P S K. The ultimate guide to restoration longevity in England and Wales. Part 10: key findings from a ten million restoration dataset. Br Dent J 2018; 225: 1011-1018.
Acknowledgements
The authors acknowledge the support of the Economic and Social Data Service, the Health and Social Care Information Centre and the NHS Business Services Authority for collating and releasing this valuable data resource.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lucarotti, P., Burke, F. Patient history as a predictor of future treatment need? Considerations from a dataset containing over nine million courses of treatment. Br Dent J 228, 345–350 (2020). https://doi.org/10.1038/s41415-020-1305-4
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-020-1305-4
- Springer Nature Limited