Abstract
Outside of clinical trials and before commercial availability for acute and chronic graft-versus-host disease (GVHD), the Janus kinase (JAK) 1/JAK2 inhibitor ruxolitinib was available to US patients with steroid-refractory GVHD through an open-label, multicenter expanded access program (EAP) sponsored by Incyte Corporation. To assess the safety of ruxolitinib, data on serious adverse events (SAEs) reported among patients in the EAP were collected. Patients ≥12 years old who received allogeneic hematopoietic cell transplantation for a hematologic malignancy and developed any-grade acute or chronic steroid-refractory GVHD received ruxolitinib at a starting dose of 5 mg twice daily (BID; acute GVHD) or 10 mg BID (chronic GVHD). At data extraction (May 8, 2020), 60 patients with acute GVHD and 549 with chronic GVHD were enrolled. In the acute and chronic GVHD cohorts, 41 (68.3%) and 186 (33.9%) patients, respectively, had ≥1 SAE. Sepsis (8.3%) and respiratory failure (6.7%) were the most common SAEs in the acute GVHD cohort, and pneumonia (4.9%), sepsis (3.8%), and lung infection (3.5%) in chronic GVHD. Infection SAEs were reported in 23.3% and 20.0% of patients with acute and chronic GVHD, respectively. Overall, these safety findings demonstrate the tolerability of ruxolitinib in steroid-refractory GVHD.
Similar content being viewed by others
Introduction
Allogeneic hematopoietic cell transplantation (HCT) is a potentially curative treatment modality indicated for several advanced malignant and nonmalignant hematologic disorders [1,2,3]. Graft-versus-host disease (GVHD), a serious and potentially life-threatening complication of HCT, represents a significant barrier to successful HCT outcomes [4, 5]. Patients who develop GVHD often report impaired physical functioning and quality of life [6, 7], and both acute and chronic forms of GVHD are leading causes of nonrelapse mortality following HCT [1, 8, 9]. Clinically significant acute GVHD occurs in 30% to 60% of HCT recipients, depending on donor characteristics and type of transplant conditioning regimen and GVHD prophylaxis [10,11,12]. Chronic GVHD occurs in ~30% to 40% of long-term HCT survivors within the first year after transplant and can occur following acute GVHD or arise de novo [10, 13]. Involvement of the skin, liver, and gastrointestinal tract is common to both acute and chronic GVHD [4, 14], whereas the pleomorphic multi-organ pathology observed in chronic GVHD additionally may include involvement of the mouth, nails, scalp, eyes, joints, genitals, and lungs [14].
There are no US Food and Drug Administration (FDA)-approved agents for the initial treatment of acute or chronic GVHD, and corticosteroids are the standard-of-care first-line treatment for both diseases [15, 16]. However, 35% to 60% of patients with acute GVHD and 40% to 60% with chronic GVHD become refractory to corticosteroid treatment and require additional systemic therapy [10, 17,18,19]. Steroid-refractory GVHD is characterized by high mortality rates, and there were no standard therapies in this setting at the time of this analysis [15]. Therefore, an unmet need exists for agents that can safely and effectively treat GVHD and improve long-term outcomes of HCT.
Ruxolitinib, a Janus kinase (JAK) 1/JAK2 inhibitor, demonstrated efficacy versus best available therapy in phase 3 trials of patients with steroid-refractory acute [20] or chronic GVHD [21] and is now approved for the treatment of steroid-refractory acute or chronic GVHD in patients ≥12 years of age [22]. Outside of clinical trials (and before commercial availability), access to ruxolitinib was available to patients with steroid-refractory acute or chronic GVHD in the United States through an expanded access program (EAP) sponsored by Incyte Corporation. The objective of this analysis is to report safety and overall survival data for patients with steroid-refractory GVHD who received ruxolitinib through the EAP.
Methods
Study design and patients
The Incyte-sponsored EAP was an open-label, multicenter study conducted at 33 US study locations across 22 states (Arizona, California, Colorado, Florida, Illinois, Indiana, Kansas, Massachusetts, Michigan, Minnesota, Missouri, New Jersey, New Mexico, New York, Ohio, Oregon, Pennsylvania, South Carolina, South Dakota, Texas, Washington, and Wisconsin). Eligible patients were ≥12 years old, received an allogeneic HCT from any donor source for a hematologic malignancy, and developed any-grade acute (per Minnesota-Center for International Blood and Marrow Transplant Research criteria) [23] or chronic (per National Institutes of Health Consensus Criteria) [14] steroid-refractory GVHD; clinical and diagnostic confirmation of steroid-refractory GVHD was determined by the treating physician. Patients were required to have evidence of myeloid engraftment (e.g., absolute neutrophil count ≥ 1.0 × 109/L for 3 consecutive days if ablative therapy was used previously) and platelet engraftment (i.e., platelets ≥20 × 109/L) and an Eastern Cooperative Oncology Group performance status of 0 to 3. Patients who had inadequate liver function not attributed to GVHD, end-stage renal dysfunction regardless of hemodialysis requirement, active uncontrolled infection; or those on any anticancer therapy, receiving any secondary GVHD therapy due to insufficient response/progression on treatment or a concomitant JAK inhibitor; or who were eligible for an active Incyte-sponsored clinical trial for ruxolitinib for the treatment of GVHD were excluded from participation.
Patients were enrolled into the acute GVHD program beginning on August 25, 2017 and into the chronic GVHD program beginning on August 9, 2017; the acute GVHD program was discontinued after ruxolitinib received FDA approval for steroid-refractory acute GVHD (data cutoff, May 8, 2020), whereas the chronic GVHD program was ongoing at the time of data extraction (data cutoff, September 8, 2020). The program is registered at ClinicalTrials.gov (NCT03147742).
The program was conducted in accordance with the principles originating in the Declaration of Helsinki and Good Clinical Practice and in adherence to the study protocol. All patients and/or their legal guardians provided written informed consent before the conduct of any program-related procedures. The institutional review board approved the protocol and all amendments.
Ruxolitinib treatment
Patients received ruxolitinib at a starting dose of 5 mg twice daily (BID) for acute GVHD (per the starting dose administered in the REACH1 clinical study and based on FDA guidance received during the design of REACH1) [24] and 10 mg BID for chronic GVHD (per REACH3) [20]. As of September 2021, the ruxolitinib label also recommends starting doses of 5 and 10 mg BID for the treatment of acute and chronic GVHD, respectively [22]. Patients with acute GVHD could have their dose escalated to 10 mg BID after 3 days if hematologic parameters were stable in the absence of treatment-related toxicity. Stable hematologic parameters were defined as the absence of a ≥ 50% decrease in platelet count and/or absolute neutrophil count relative to the date of the first ruxolitinib dose. Dose escalations were not permitted for chronic GVHD, as the protocol-defined maximum recommended dose for ruxolitinib treatment was 10 mg BID. Dose reductions were allowed at any time during the course of treatment based on safety and laboratory assessments; the ruxolitinib dose could be re-escalated if toxicity management thresholds were met or if the patient experienced a GVHD flare and had adequate hematologic parameters. Patients could receive ruxolitinib treatment for as long as they continued to derive clinical benefit and treatment withdrawal criteria were not met per the discretion of the treating physician. Withdrawal criteria included unacceptable toxicity; relapse of the underlying malignancy; inability to tolerate ruxolitinib at a dose of 5 mg once daily (QD); investigator decision that further participation would be injurious to the patient’s health or well-being; pregnancy; withdrawn consent; program termination by the sponsor, FDA, or institutional review board; transition to commercially available ruxolitinib; or death. Patients could receive or continue to use any nonrestricted or prohibited medications (Table S1), including anti-infective medications, GVHD prophylaxis medications (including calcineurin inhibitors), transfusion support, or topical steroid therapy, as deemed necessary by the physician to manage GVHD or any other complication.
Assessments and statistical analyses
Data on patient demographics, medical history, disease characteristics (e.g., hematologic malignancy type, transplant setting, GVHD staging at treatment initiation, date of diagnosis, sites of disease), treatment history, and concomitant GVHD medications were collected at screening. Serious adverse events (SAEs) were coded using the Medical Dictionary for Regulatory Activities v22.0 and graded per National Cancer Institute Common Terminology Criteria for Adverse Events v4.03 and assessed from the screening period through safety follow-up. SAEs were defined as an event that met ≥1 of the following criteria: (1) was fatal or life threatening; (2) required inpatient hospitalization or prolongation of existing hospitalization (unless hospitalization was a result of a routine treatment or monitoring of the study indication not associated with any deterioration in condition; an elective surgery or preplanned treatment for a pre-existing condition that was unrelated to the indication under the program and had not worsened since signing the informed consent form; a treatment or emergency outpatient basis for an event not fulfilling any of the definitions of an SAE and not resulting in hospital admission; or any social reasons and respite care, in the absence of any deterioration in the patient’s general condition); (3) resulted in persistent or significant disability, incapacity, or a substantial disruption of the patient’s ability to conduct normal life functions; (4) constituted a congenital anomaly or birth defect; or (5) was considered an important medical event or a medically significant event that may have jeopardized the patient or required medical or surgical intervention to prevent one of the outcomes listed above. For patients discontinuing treatment, the safety follow-up period lasted 30 days following the date of the final ruxolitinib dose (not applicable to patients who transitioned to commercial product). Safety data were summarized using descriptive statistics. Ruxolitinib treatment duration and overall survival were assessed for each patient cohort using Kaplan–Meier methodology.
Results
Patients
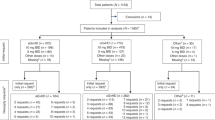
A total of 60 patients with acute GVHD and 549 patients with chronic GVHD were enrolled in the EAP. Among patients with acute GVHD, median (range) age at time of transplant was 58.5 (24–76) years, and 35 patients (58.3%) were male; 36 (60.0%), 35 (58.3%), and 10 patients (16.7%) had acute GVHD involvement of the gastrointestinal tract, skin, and liver, respectively (Table 1). Among patients with chronic GVHD, median (range) age was 60.0 (15–81) years, and 294 patients (53.6%) were male; the most commonly involved organs were skin (n = 390; 71.0%), eyes (n = 333; 60.7%), and mouth (n = 303; 55.2%). At treatment initiation, most patients with acute GVHD had GVHD grade II (33.3%) or grade III (35.0%) disease, and those with chronic GVHD were rated as having moderate (43.5%) or severe (41.3%) disease. Aside from previous glucocorticoid therapy (acute GVHD, 96.7%; chronic GVHD, 54.1%), the most common treatment received at the time of study initiation was calcineurin inhibitors (acute GVHD, 45.0%; chronic GVHD, 37.7%; Fig. 1).
GVHD treatments received at the time of study initiation for patients with (a) acute and (b) chronic GVHD*. ATC Anatomical Therapeutic Chemical, GVHD graft-versus-host disease. *Patients could have received >1 treatment; treatment types are per ATC code and as reported at the time of ruxolitinib initiation. Per study eligibility criteria, all patients were previously exposed to corticosteroids at the time of or before ruxolitinib initiation. †Previous therapies reported in >1% of patients are shown.
In the acute GVHD cohort, 47 patients (78.3%) received the protocol-recommended starting dose of 5 mg BID ruxolitinib; at the time of last dose, 36 patients (60.0%) were receiving 5 mg BID ruxolitinib, and 6 (10.0%) and 18 patients (30.0%) were receiving 5 mg QD and 10 mg BID ruxolitinib, respectively (Fig. 2a). All patients in the acute GVHD cohort discontinued treatment, most commonly owing to program discontinuation (23.3%), death (21.7%), and GVHD progression and relapse of the underlying malignancy (6.7% each). The median (95% CI) treatment duration was 93.0 (50–151) days (Fig. 3a).
Among patients with chronic GVHD, 258 (47.0%) received the protocol-recommended starting dose of 10 mg BID ruxolitinib; at the time of last dose, 302 patients (55.0%) were receiving 10 mg BID ruxolitinib, and 31 (5.6%), 206 (37.5%), and 10 patients (1.8%) were receiving 5 mg QD, 5 mg BID, and other doses of ruxolitinib, respectively (Fig. 2b). At the time of data extraction, 206 patients (37.5%) had discontinued treatment; the most common reasons were death (8.2%), GVHD progression (4.9%), relapse of the underlying malignancy (3.8%), and adverse events (AEs; 3.6%). The median (95% CI) treatment duration was 712.0 (572–1014) days (Fig. 3b).
Safety
In the acute GVHD cohort, 41 patients (68.3%) had ≥1 SAE. The most common SAEs were sepsis (8.3%) and respiratory failure (6.7%; Table 2). Median (range) time from ruxolitinib initiation to first SAE was 25.0 (3–253) days. Fourteen patients (23.3%) had infections reported as SAEs, none of which were cytomegalovirus (CMV) infections (Table 2). Treatment-related SAEs were reported in six patients (10.0%; Table 2); the only treatment-related SAE reported in >1 patient was respiratory failure (n = 2). Twenty-three patients (38.3%) had SAEs with fatal outcomes. Two patients (3.3%) had fatal SAEs suspected to be related to ruxolitinib, which were respiratory failure (n = 2) and shock (n = 1).
In the chronic GVHD cohort, SAEs occurred in 186 patients (33.9%). The most frequently reported SAEs were pneumonia (4.9%), sepsis (3.8%), and lung infection (3.5%; Table 3). Median (range) time from ruxolitinib initiation to first SAE was 80.0 (1–1014) days. Overall, 110 patients (20.0%) had infections reported as SAEs, with pneumonia being the most commonly reported (n = 27 [4.9%]; Table 3). One patient (0.2%) and 2 patients (0.4%) had reported SAEs of CMV infection and viremia, respectively. There were 42 patients (7.7%) who had SAEs deemed related to ruxolitinib (Table 3); the most common treatment-related SAEs were pneumonia (2.7%), lung infection (0.5%), and sepsis (0.5%). Sixty-one (11.1%) patients had fatal SAEs, most commonly attributed, at least in part, to infections (n = 19 [31.1% of SAE-related fatalities]). Eight patients (1.5%) had fatal SAEs suspected to be related to ruxolitinib; pneumonia was the only fatal SAE reported in >1 patient (n = 2).
Survival
At the time of data extraction, 12 patients (20.0%) in the acute GVHD cohort had died due to any cause; median overall survival was not reached (95% CI, 345 days—not reached; Fig. 4a). In the chronic GVHD cohort, 45 patients (8.2%) had died from any cause at the time of data cutoff; median overall survival was not reached (95% CI, 1001 days—not reached; Fig. 4b).
Discussion
This study describes the largest safety analysis of patients treated with ruxolitinib for GVHD to date. In summary, patients with steroid-refractory GVHD in the ruxolitinib EAPs were heavily pretreated, with nearly half of patients with acute GVHD and approximately one-third of patients with chronic GVHD having received ≥3 lines of prior therapy. More than half of patients with acute GVHD had involvement of the gastrointestinal tract or skin, whereas patients with chronic GVHD primarily had involvement of the skin, eyes, and mouth. Although this study was not designed to collect efficacy data, we observed few patients in either cohort who discontinued ruxolitinib treatment because of GVHD progression (7% and 5% in the acute and chronic GVHD cohorts, respectively) or relapse of the underlying malignancy (7% and 4%, respectively). Response rates cannot be determined from this primarily safety-driven dataset. Only 2% and 4% of patients with acute and chronic GVHD, respectively, discontinued treatment due to AEs. SAEs were reported in approximately two-thirds of patients with acute GVHD and in one-third of patients with chronic GVHD; however, no new or unexpected SAEs were reported. Overall, the toxicity profile of ruxolitinib in acute and chronic GVHD was favorable and consistent with that observed in the REACH clinical trials [20, 21, 24]. Rates of relapse-related discontinuations were not suggestive of an increased incidence of malignancy relapse with ruxolitinib; however, the EAP did not capture data on malignancy relapses independent of program discontinuation.
At the time of study initiation, there were no standard second-line therapies for acute or chronic GVHD, and prognosis is poor among patients with steroid-refractory disease [10, 15]. Ruxolitinib has demonstrated efficacy in patients with steroid-refractory acute GVHD in phase 2 (REACH1) and 3 (REACH2) clinical trials [20, 24]. Additionally, ruxolitinib treatment resulted in improved response rate, failure-free survival, and symptoms compared with best available therapy in patients with steroid-refractory chronic GVHD in an open-label phase 3 study (REACH3) [21]. In the REACH trials, ruxolitinib appeared tolerable, with cytopenias (e.g., thrombocytopenia, anemia, neutropenia) typically reported as the most frequently occurring AEs. Notably, transient cytopenias manageable with dose modifications and supportive measures have also been observed with ruxolitinib in the treatment of other disorders, including myelofibrosis [25]. CMV infection events were common in clinical trials of ruxolitinib [20, 24] but rarely qualified as SAEs in the EAP; however, the EAP only captured SAEs, so the overall frequency of CMV events of any severity is unknown in the current study. Insufficient mature data from the REACH trials are available to draw conclusions regarding the survival benefit of ruxolitinib in steroid-refractory GVHD, but failure-free survival was improved with ruxolitinib versus best available therapy in both acute (REACH2) and chronic (REACH3) studies [20, 21], and median overall survival appeared longer with ruxolitinib in REACH2 (11.1 vs. 6.5 months in the control arm) [20].
The EAP was not designed to evaluate efficacy; however, the median duration of ruxolitinib treatment was ~3 months in the acute GVHD cohort and nearly 2 years in the chronic GVHD cohort. This highlights the potential clinical benefit derived from ruxolitinib therapy. Although clinical benefit was not formally assessed on study, potential benefits may include stabilization of disease symptomatology and facilitation of concomitant steroid and immunosuppressant tapering. There was also encouraging survival data seen, as median overall survival was not reached in either cohort.
Several limitations to this study should be considered. First, criteria for establishing GVHD diagnosis and severity were determined by the treating physician. Additionally, only SAEs and not all treatment-emergent AEs were captured, so unexpected toxicities of mild to moderate severity may have been missed. By design, there was no specific prospective follow-up, so the study may be subject to underreporting of safety events. Additionally, the acute GVHD cohort had limited follow-up, as patients who remained on treatment were transitioned to commercial ruxolitinib supply (May 2020) following FDA approval of ruxolitinib for this indication; FDA approval of ruxolitinib for the treatment of steroid-refractory chronic GVHD (September 2021) occurred after data extraction and did not affect the analysis. Finally, the intended scope of the EAP was to collect prospective toxicity data and not detailed efficacy information, and response data are therefore unavailable.
In conclusion, in this analysis of patients with steroid-refractory GVHD receiving ruxolitinib via an EAP, no new or unexpected SAEs were observed. Relatively few patients discontinued the program owing to malignancy relapse, and overall survival was not reached in either cohort at the time of data cutoff. This study provides a comprehensive safety evaluation from a large patient cohort, with findings demonstrating the tolerability of ruxolitinib in acute and chronic GVHD patient populations. Although no formal efficacy analyses were conducted, the long duration of therapy and survival suggests a benefit of ruxolitinib therapy in both acute and chronic GVHD.
Data availability
Incyte Corporation (Wilmington, DE, USA) is committed to data sharing that advances science and medicine while protecting patient privacy. Qualified external scientific researchers may request anonymized datasets owned by Incyte for the purpose of conducting legitimate scientific research. Researchers may request anonymized datasets from any interventional study (except Phase 1 studies) for which the product and indication have been approved on or after 1—January 2020 in at least one major market (e.g., US, EU, JPN). Data will be available for request after the primary publication or 2 years after the study has ended. Information on Incyte’s clinical trial data-sharing policy and instructions for submitting clinical trial data requests are available at: https://www.incyte.com/Portals/0/Assets/Compliance%20and%20Transparency/clinical-trial-data-sharing.pdf?ver=2020-05-21-132838-960.
References
Phelan R, Arora M, Chen M. Current use and outcome of hematopoietic stem cell transplantation: CIBMTR US summary slides, 2020. https://www.cibmtr.org/ReferenceCenter/SlidesReports/SummarySlides/pages/index.aspx. Accessed 2 July 2021.
Passweg JR, Baldomero H, Basak GW, Chabannon C, Corbacioglu S, Duarte R, et al. The EBMT activity survey report 2017: a focus on allogeneic HCT for nonmalignant indications and on the use of non-HCT cell therapies. Bone Marrow Transplant. 2019;54:1575–85.
Duarte RF, Labopin M, Bader P, Basak GW, Bonini C, Chabannon C, et al. Indications for haematopoietic stem cell transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe, 2019. Bone Marrow Transplant. 2019;54:1525–52.
Zeiser R, Blazar BR. Acute graft-versus-host disease—biologic process, prevention, and therapy. N Engl J Med. 2017;377:2167–79.
Zeiser R, Blazar BR. Pathophysiology of chronic graft-versus-host disease and therapeutic targets. N Engl J Med. 2017;377:2565–79.
Lee SJ, Kim HT, Ho VT, Cutler C, Alyea EP, Soiffer RJ, et al. Quality of life associated with acute and chronic graft-versus-host disease. Bone Marrow Transplant. 2006;38:305–10.
Fiuza-Luces C, Simpson RJ, Ramirez M, Lucia A, Berger NA. Physical function and quality of life in patients with chronic GvHD: a summary of preclinical and clinical studies and a call for exercise intervention trials in patients. Bone Marrow Transplant. 2016;51:13–26.
Holtan SG, DeFor TE, Lazaryan A, Bejanyan N, Arora M, Brunstein CG, et al. Composite end point of graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation. Blood. 2015;125:1333–8.
Atsuta Y, Hirakawa A, Nakasone H, Kurosawa S, Oshima K, Sakai R, et al. Late mortality and causes of death among long-term survivors after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2016;22:1702–9.
Axt L, Naumann A, Toennies J, Haen SP, Vogel W, Schneidawind D, et al. Retrospective single center analysis of outcome, risk factors and therapy in steroid refractory graft-versus-host disease after allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2019;54:1805–14.
Al Malki MM, Gendzekhadze K, Yang D, Mokhtari S, Parker P, Karanes C, et al. Long-term outcome of allogeneic hematopoietic stem cell transplantation from unrelated donor using tacrolimus/sirolimus-based GVHD prophylaxis: impact of HLA mismatch. Transplantation. 2020;104:1070–80.
Jagasia M, Arora M, Flowers ME, Chao NJ, McCarthy PL, Cutler CS, et al. Risk factors for acute GVHD and survival after hematopoietic cell transplantation. Blood. 2012;119:296–307.
Arai S, Arora M, Wang T, Spellman SR, He W, Couriel DR, et al. Increasing incidence of chronic graft-versus-host disease in allogeneic transplantation: a report from the Center for International Blood and Marrow Transplant Research. Biol Blood Marrow Transplant. 2015;21:266–74.
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 diagnosis and staging working group report. Biol Blood Marrow Transplant. 2015;21:389–401.e1.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology. Hematopoietic cell transplantation (HCT): pre-transplant recipient evaluation and management of graft-versus-host disease (Version 2.2021). https://www.nccn.org/professionals/physician_gls/pdf/hct.pdf. Accessed 9 June 2021.
Penack O, Marchetti M, Ruutu T, Aljurf M, Bacigalupo A, Bonifazi F, et al. Prophylaxis and management of graft versus host disease after stem-cell transplantation for haematological malignancies: updated consensus recommendations of the European Society for Blood and Marrow Transplantation. Lancet Haematol. 2020;7:e157–67.
Major-Monfried H, Renteria AS, Pawarode A, Reddy P, Ayuk F, Holler E, et al. MAGIC biomarkers predict long-term outcomes for steroid-resistant acute GVHD. Blood. 2018;131:2846–55.
Garnett C, Apperley JF, Pavlu J. Treatment and management of graft-versus-host disease: improving response and survival. Ther Adv Hematol. 2013;4:366–78.
Flowers ME, Storer B, Carpenter P, Rezvani AR, Vigorito AC, Campregher PV, et al. Treatment change as a predictor of outcome among patients with classic chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2008;14:1380–4.
Zeiser R, von Bubnoff N, Butler J, Mohty M, Niederwieser D, Or R, et al. Ruxolitinib for glucocorticoid-refractory acute graft-versus-host disease. N Engl J Med. 2020;382:1800–10.
Zeiser R, Polverelli N, Ram R, Hashmi SK, Chakraverty R, Middeke JM, et al. Ruxolitinib for glucocorticoid-refractory chronic graft-versus-host disease. N Engl J Med. 2021;385:228–38.
JAKAFI® (ruxolitinib). Full Prescribing Information. Wilmington, DE, USA: Incyte Corporation; 2021.
MacMillan ML, DeFor TE, Weisdorf DJ. What predicts high risk acute graft-versus-host disease (GVHD) at onset?: Identification of those at highest risk by a novel acute GVHD risk score. Br J Haematol. 2012;157:732–41.
Jagasia M, Perales MA, Schroeder MA, Ali H, Shah NN, Chen YB, et al. Ruxolitinib for the treatment of steroid-refractory acute GVHD (REACH1): a multicenter, open-label phase 2 trial. Blood. 2020;135:1739–49.
Harrison C, Kiladjian J-J, Al-Ali HK, Gisslinger H, Waltzman R, Stalbovskaya V, et al. JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis. N Engl J Med. 2012;366:787–98.
Acknowledgements
Support for this study was provided by Incyte Corporation (Wilmington, DE, USA). Writing assistance was provided by Jane Kovalevich, Ph.D., an employee of ICON (Blue Bell, PA, USA), and was funded by Incyte Corporation.
Author information
Authors and Affiliations
Contributions
MAS contributed to data acquisition, data interpretation, and paper writing. PNH contributed to data acquisition, data interpretation, and paper writing. AB contributed to study conceptualization, data management, and paper writing. DP contributed to study conceptualization, statistical analyses, data interpretation, and paper writing. VB contributed to study conceptualization, data interpretation, and paper writing. JFD contributed to data acquisition, data interpretation, and paper writing. All authors approved the final submitted version of the paper.
Corresponding author
Ethics declarations
Competing interests
MAS has served on advisory boards and received honoraria or consultancy fees unrelated to the present work from CareDx, Incyte Corporation, and Sanofi Genzyme. PNH has received consulting fees from Amgen, BMS, GSK, Incyte Corporation, Janssen, Karyopharm, and Takeda. AB, DP, and VB are employees and shareholders of Incyte Corporation. JFD served on advisory boards for Arch, Bioline, Incyte Corporation, Macrogenics, and Rivervest and is a cofounder of Magenta Therapeutics and WUGEN.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Schroeder, M.A., Hari, P.N., Blithe, A. et al. Safety analysis of patients who received ruxolitinib for steroid-refractory acute or chronic graft-versus-host disease in an expanded access program. Bone Marrow Transplant 57, 975–981 (2022). https://doi.org/10.1038/s41409-022-01673-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01673-y
- Springer Nature Limited
This article is cited by
-
Ruxolitinib in patients with graft versus host disease (GvHD): findings from a compassionate use program
Bone Marrow Transplantation (2024)
-
Ruxolitinib for GVHD: no unexpected serious AEs in EAP
Reactions Weekly (2022)