Abstract
The current guidelines for prevention of infections in hematopoietic stem cell transplantation (HSCT) do not specify which central venous catheter (CVC) insertion site should be preferred in allogeneic HSCT recipients—internal jugular vein (IJV) or subclavian vein (SCV). We designed a multicenter prospective observational study comparing the risk of infectious and non-infectious complications between the two most common sites of CVC insertion (IJV and SCV) in allogeneic HSCT. There were in total 232 consecutive patients (86 IJV and 146 SCV) who underwent adult allogeneic HSCT reported from 11 centers in 8 countries. The center independent analysis of central line associated/related blood stream infections with ECDC criteria has shown statistically significant difference favoring SCV (23% IJV vs 13% SCV (OR 2.03 (1.01–4.06), p = 0.047)). The differences in CLABSI per 1000 days of CVC use favored SCV over IJV (7.93/1000 days IJV vs 2.79/1000 days SCV, p = 0.002). The frequency of all non-infectious complications was similar in both arms—13% IJV and 12% SCV (OR 1.1 (0.5–2.5), p = 0.8). This multicenter prospective study showed statistically significant lower confirmed number of CLABSI per 1000 days of CVC use without higher risk of noninfectious complications related to the subclavian insertion site in allogeneic HSCT recipients.
Similar content being viewed by others
Introduction
The optimal site for central venous catheter (CVC) insertion in hematopoietic stem cell transplantation (HSCT) is not resolved. The current guidelines for prevention of infections in HSCT recipients do not specify optimal CVC insertion site [1]. This situation is partly caused by lack of data on this topic. So far, there are no prospective multicenter studies published in this patient population and subsequently no systematic review nor meta-analyzes can be made in HSCT setting. In our previous study we have shown that most of the HSCT centers in Europe use either subclavian vein (SCV) or internal jugular vein (IJV) as insertion site for CVC in hematopoietic stem cell recipients [2]. In the absence of data the choice is often based on local experience—centers choosing IJV point to lower risk of noninfectious complications, while centers choosing SCV indicate lower risk of infectious complications. However, none of these claims can be supported by a multicenter prospective study in allogeneic HSCT (allo-HSCT) recipients. A small single-center study that compared the two sites of insertion has shown that IJV access might be more likely the source of central line-associated blood stream infections (CLABSI) in HSCT patients [3]. In contrast, another retrospective single-center study did not show significant superiority of SCV over IJV [4].
The meta-analyzes from non-hematologic intensive care units show that SCV access is associated with lower chances of CLABSI [5,6,7]. In one of the recent randomized studies that compared three sites of CVC insertion, SCV had the lowest number of CLABSI [8]. Moreover, the 3SITES study has demonstrated, that cumulative rate of all complications also favored the subclavian site showing that the reduction of the CLABSI is not offset by other complications [8]. However, the data from the non-hematological ICUs cannot be translated directly to HSCT setting. Neutropenia, thrombocytopenia, chemotherapy, time of catheter use, and other factors can influence the risk of complications related to different sites of CVC placement in HSCT patients [4].
Another important aspect of the prevention of CLABSI is the implementation of international guidelines. In our previous study, we were able to show that the five basic guidelines (CLABSI “prevention bundle”) such as hand hygiene, full barrier precautions, cleaning the insertion site with chlorhexidine, avoiding femoral sites for insertion, and removing unnecessary catheters—were only fully implemented in one-third of the checked HSCT centers [2]. The results of the single-center studies are very likely to be influenced by the procedures at the center and conclusions can only be drawn if the methodology is examined very carefully. Another aspect that impacts the translation of study results into clinical practice is the CLABSI or catheter-related blood stream infection (CR-BSI) definitions used at the centers, which could also affect the results of an individual center.
Having this in mind we designed a prospective observational study in allo-HSCT patients that aimed at comparing infectious and non-infectious complications connected with the insertion of CVC at the two most common insertion sites.
Materials and methods
Type of study: prospective multicenter observational study
Center selection criteria
In order to improve the quality of the study and to reduce the number of variables that influence the outcome of the study we used center inclusion criteria—based on international guidelines and data from our previous study showing the implementation of these guidelines [1]. We send the invitations only to centers that fulfilled the general [9] and specific criteria: (a) adult allo-HSCT center (b) use of non-tunneled CVC in majority of patients at the center (c) lack of policy to routinely replace the catheters after a specific period of time at the center (d) lack of policy to remove CVC on the basis of fever alone at the center (e) surgical full barrier precautions at the insertion of CVC with body drapes covering sufficient area of the patient’s body (drapes bigger than 60 × 60cm) (f) availability or use of ultrasound during the insertion. The centers were invited to participate and received link to the online questionnaire where additional study-specific data were reported.
Analysis endpoints
The primary endpoint of the analysis was to examine the difference in relative risk of infectious complications in allo-HSCT recipients depending on CVC insertion site (subclavian vs jugular) including: (a) any blood stream infection (b) confirmed CLABSI c) infections at the insertion site. The secondary endpoint was to study the difference in the relative risk of any other non-infectious catheter-related complications at the time of insertion and in follow-up care in allo-HSCT recipients.
Patient data
After center inclusion, the data of consecutive patients had to be reported to avoid patient selection bias. The center reported as many consecutive patients as possible with allocated resources. For each included patient, only the data of the first CVC inserted for allo-HSCT were to be reported. The patient data were reported by the online questionnaire. The patient inclusion criteria were: (a) over 18 years of age (b) CVC placement during current allo-HSCT hospitalization and within 7 days prior to starting the conditioning regimen (c) non-tunneled CVC placed in either internal jugular vein (IJV) or subclavian vein (SCV). The collected medical data included: date of start of hospitalization for allo-HSCT; CVC insertion date, site of insertion; CVC number of lumens, type of skin fix, type of dressing, date, and cause of removal; parenteral nutrition and neutropenic fever. More specific data on non-infectious and infectious complications included data on all positive microbiologic cultures and all clinical symptoms of infections during study observation period. As there was possibility that chlorhexidine-containing skin disinfectants might not be available in all participating countries the use of chlorhexidine for disinfection prior to insertion was not set as center inclusion criteria.
Definitions
The selection of definition of central line-associated blood stream infections or catheter-related blood stream infections (either Centers for Diseases Control and Prevention (CDC) [10] or European Centre for Disease Prevention and Control (ECDC) [11]) was center specific. Practices were uniform at each center. The patient questionnaire was structured so that data could be used for a center-independent analysis of the occurrence of central line-associated/related blood stream infections.
Blood sampling
The blood sampling was similar in all centers and included at least two sets of bacterial cultures in patients with symptoms of infection—one set from central line and the other from peripheral vein. The blood was cultured in aerobic and anaerobic bottles. One center performed additional surveillance with routine once-a-week sampling from all catheter lumens (2 patients with jugular CVC and 28 patients with subclavian CVC).
Statistical analysis
Descriptive statistics was reported for all the variables: mean, standard deviation, median, and range for the continuous variables; percentage for categorical variables.
The percentage of infectious complications in the two groups (internal jugular vs subclavian insertion site) was compared using Chi-square test or Fisher exact test as appropriate. Logistic regression models were performed in order to detect the risk factors related to the infectious complication. The incidence of any blood stream infection confirmed CLABSI and infections at the insertion site were compared between the two groups. A p value < 0.05 was considered statistically significant; all the analysis was performed using the statistical software SAS ver 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
There were in total 232 consecutive adult patients who underwent allo-HSCT and their medical data were reported from 11 centers in 8 countries. Among them, there were 146 patients with SCV CVC and 86 with IJV CVC. The groups had similar demographic characteristics (Table 1). There were differences in care of the CVC in relation to the site of insertion. In case of the jugular CVC the transparent dressing with antibacterial sponge was used more often. On the other hand, the catheters used for subclavian access had more lumens. The subclavian CVCs were used for a longer period of time (31 days SCV vs 27 days IJV) and were removed more frequently due to complications during the treatment (cumulative 21.1% SCV vs 12.8% IJV)
Analysis of the primary endpoints (Table 2) has shown similar numbers of positive microbiologic cultures in both groups of patients during the use of first CVC for allo-HSCT (39.5% for IJV vs 37% for SCV; OR IJV vs SCV: 1.11 (0.6–1.9), p = 0.7). The center-reported CLABSI was more common in internal jugular access, but the difference was not statistically significant (16.3% for IJV vs 8.9% for SCV, OR IJV vs SCV: 2.0 (0.9–4.5), p = 0.095). The analysis revealed that the definitions used at the centers varied with 4 centers using ECDC and other 7 CDC criteria. When the ECDC criteria were independently applied to the collected data CLABSI were significantly more common in IJV than SCV (23.3% for IJV vs 13.0% for SCV OR IJV vs SVC: 2.03 (1.01–4.06), p = 0.047). With CDC criteria independently applied to the data the CLABSI were more common in IJV than SCV, however, the difference was not statistically significant (18.6% for IJV vs 9.6% for SCV OR IJV vs SVC: 2.16 (0.99–4.67), p = 0.052). The most common bacteria causing blood stream infections were Coagulase-negative staphylococci in both access sites (detailed data are shown in Table 3).
Confirmed infections at the insertion site were uncommon in both patient groups with 0 in 86 patients in the IJV group and 1 in 146 patients in the SCV group.
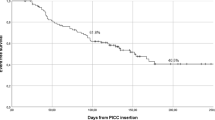
The non-infectious complications had similar frequency in both groups (12.8% IJV vs 11.8% SCV, OR IJV vs SVC: 1.1 (0.5–2.5), p = 0.8.). Thrombosis (2.3% IJV vs 0.7% SCV, p = 0.6) and bleeding (4.7% IJV vs 2.1% SCV, p = 0.4) did not show statistically significant differences between the groups. Figure 1 shows cumulative infection rates with positive blood stream cultures within 30 days from transplantation. The cumulative percentage of complications is shown in Fig. 2. The number of patients developing both types of complications was similar in both groups (3.5% IJV and 2.1% SCV; p = 0.5).
The primary endpoint (confirmed CLABSI) differed significantly between the groups (p = 0.047). The secondary endpoint (any other noninfectious complications connected with central catheter) did not differ between the groups (p = 0.8). ECDC criteria for catheter-related blood stream infection were used for analysis.
Per 1000 days of catheter use, CLABSI incidence was significantly lower in SCV compared with IJV (7.93 /1000 days in IJV vs 2.79/1000 days in SCV group, p = 0.002). An independent analysis of our data set with ECDC and CDC criteria has also shown statistically significant differences favoring the use of subclavian access (CLABSI incidence: ECDC—10.43/1000 days in IJV vs 4.36/1000 days in SCV, p = 0.002; CDC—8.34/1000 days in IJV vs 2.96/1000 days in SCV, p = 0.0002).
Discussion
In this prospective observational multicenter study catheterization of subclavian vein was associated with lower chances of CLABSI per 1000 days of catheter use without increased risk of noninfectious complications when compared with internal jugular vein in adult allo-HSCT patients. The differences in all primary and secondary endpoints favored the subclavian access—however, only when ECDC criteria were applied the difference reached statistical significance for the risk of catheter-related blood stream infection.
Our results show much higher rates of bloodstream infections, thrombosis and bleeding in patients with CVC undergoing hematopoietic stem cell transplantation compared with recent trial in standard ICU setting [8]. This finding is not surprising since aplasia and immunosuppression impact the complications rates in allo-HSCT patients. Moreover, the average time of catherization in general ICU in 3SITES study was around 6 days compared to 28 days in our study. One of the contributing factors could also be almost routine use of CVC in allo-HSCT patients for blood sampling [2]. Taken together this raises the question whether the use of CVC in allo-HSCT patients can be as safe as in general ICU population. The cumulative percentage of complications in the mentioned 3SITES study in ICU setting is below 4% for any access site. The cumulative of all complications that can be contributed to CVC in allo-HSCT setting is between 20 and 30% (including confirmed CLABSI and noninfectious complications of CVC). The high complication rates seen in our study can be partly attributed to the extremely high quality of data reported and the prolonged insertion time of CVC in allo-HSCT patients. Data for all patients’ complications (infectious and noninfectious) have been recorded with no missing records (in each case of complication center had to specify the nature of this complication). This distinguishes the quality of the present study from other trials [8]. Moreover, being aware of variation in CVC insertion and care practices that could impact the results [2], we included center qualification criteria to make sure that the practices are uniform at the centers on the level of actual procedures performed in patients and not only on the level of documents and declarations.
The comparison with single-center retrospective studies in allo HSCT recipients shows other interesting differences [3, 4]. First, the single-center studies report on different populations of patients: a group of patients having SCV CVC implanted for allo HSCT are compared to IJV CVC autologous HSCT, or patients with CVC inserted prior to allo-HSCT are compared to CVC specifically inserted for treatment of complications [3, 4]. This is a confounding factor making the data hard to interpret. To make our data even more uniform we included only the data for the first CVC in allo-HSCT patients. In contrast to our study, study of Heidenreich et al. demonstrated very high number of patients with local inflammation (up to 71%) [4]. The difference could explained by underreporting in our study—since only culture-positive infections were reported, or by center-specific factors influencing this specific complication at that center [4].
Another interesting finding of this study is the differences between CLABSI reported by the center and the rates of CLABSI identified using the CDC and ECDC definition parameters. This indicates a possible limitation of single-center studies that provide the number of CLABSI measured by center personnel rather than the results and symptoms that could be independently analyzed. We reduced this limitation by reporting not only infections, but also clinical and laboratory parameters required for diagnosis of CLABSI/CR-BSI according to CDC and ECDC. In this way, studies can be constructed that limit a possible tendency of a center to under- or over-report the catheter-related blood stream infections.
There were some limitations to our study. The results of the study should only be translated to the centers that have implemented a set of minimal guidelines specified in the methodology of this study. It is clearly not only the site of insertion, but also procedures of insertion and follow-up care that impact the rates of CVC complications [12]. We ensured that only those centers that were shown in an independent study to follow all essential procedures for prevention of CLABSI could participate this study [2]. We can expect that the results will be different in the centers that did not implement bundles of CVC infection prevention—which are also likely to impact single-center studies. This is important as there are often differences between the recommendations included in the SOP (and later reported in the studies as methodology) and clinical practice at the center [2].
No further study data were collected after removal of the CVC and we did not have specific follow-up ultrasonography preformed to check for deep venous thrombosis at catheter site. Thus, it is possible that some post-CVC-associated thromboses have not been reported. In addition, the follow-up of CVC-related complications was continued after discharge. We also did not have external validation of the data reported by the centers – and were only able to perform analysis on parameters reported by centers. Another factor possibly influencing results was type of CVC dressing. A higher proportion of jugular CVCs had transparent dressing with chlorhexidine patch. The lower number of CLABSI is expected with chlorhexidine-impregnated patch [13]. This may have influenced the final results of our study in favor of jugular access. Patients with IJC CVC had more parental nutrition (PN) administered during hospitalization for allo-HSCT. The PN was shown to be a factor predisposing to CLABSI at the rates around 1 CLABSI per 1000 days during the long term CVC use in oncologic patients [14]. A recent study did not show impact of PN on BSI rates in allo-HSCT patients [15]—so it is unlikely that PN use meaningfully impacts the results of this study. We also cannot exclude that the ongoing BSI was one of the factors for patient deterioration and need for parenteral nutrition.
Conclusion
This is the first international multicenter prospective observational study demonstrating that subclavian access for CVC is favorable in adult patients undergoing allo-HSCT as CLABSI rates per 1000 days of catheter are significantly lower when compared with internal jugular access. This advantage of subclavian access is not offset by number of non-infectious complications, that remained similar with internal jugular access. These findings reflect the results in recent study in general ICU patients [8] and the CDC guidelines that recommend use of subclavian rather than jugular or femoral site in general ICU patients [12]. Our study shows that subclavian CVC insertion should also be recommended in the adult allo-HSCT setting specifically and will lead to a significant reduction of catheter-related infectious complications.
Keypoints
First multicenter prospective observational study in adult allogenic hematopoietic stem cell recipients that showed superiority of subclavian vein insertion site over internal jugular vein insertion site (lower number of CLABSI per 1000 days with similar number of noninfectious complications).
References
Tomblyn M, Chiller T, Einsele H, Gress R, Sepkowitz K, Storek J, et al. Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: a global perspective. Biol Blood Marrow Transpl. 2009;15:1143–238. https://doi.org/10.1016/j.bbmt.2009.06.019. Available from
Snarski E, Mank A, Iacobelli S, Hoek J, Styczyński J, Babic A, et al. Current practices used for the prevention of central venous catheter-associated infection in hematopoietic stem cell transplantation recipients: a survey from the Infectious Diseases Working Party and Nurses’ Group of EBMT. Transpl Infect Dis. 2015;17:558–65.
Martinho GH, Romanelli RMC, Machadoteixeira G, Macedo AV, Chaia JMC, Nobre V. Infectious complications associated with the use of central venous catheters in patients undergoing hematopoietic stem cell transplantation. Am J Infect Control 2013;32:1–3.
Heidenreich D, Hansen E, Kreil S, Nolte F, Jawhar M, Hecht de Gutierrez A, et al. Influence of the insertion site on central venous catheter-related complications in patients undergoing allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2020;26:1189–94.
Parienti J-J, du Cheyron D, Timsit J-F, Traore O, Kalfon P, Mimoz O, et al. Meta-analysis of subclavian insertion and non-tunneled central venous catheter-associated infection risk reduction in critically ill adults. Crit Care Med. 2012;40:1627–34.
Marik PE, Flemmer M, Harrison W. The risk of catheter-related bloodstream infection with femoral venous catheters as compared to subclavian and internal jugular venous catheters: a systematic review of the literature and meta-analysis. Crit Care Med. 2012;40:2479–85. http://www.ncbi.nlm.nih.gov/pubmed/22809915 Available from
Arvaniti K, Lathyris D, Blot S, Apostolidou-Kiouti F, Koulenti D, Haidich A-B. Cumulative evidence of randomized controlled and observational studies on catheter-related infection risk of central venous catheter insertion site in ICU patients: a pairwise and network meta-analysis. Crit Care Med 2017;45:e437–48.
Parienti JJ, Mongardon N, Mégarbane B, Mira JP, Kalfon P, Gros A, et al. Intravascular complications of central venous catheterization by insertion site. N Engl J Med. 2015;373:1220–9.
Yokoe D, Casper C, Dubberke E, Lee G, Muñoz P, Palmore T, et al. Infection prevention and control in health-care facilities in which hematopoietic cell transplant recipients are treated. Bone Marrow Transplant 2009;44:495–507.
National Healthcare Safety Network (NHSN) Patient Safety Component Manual. 2020; https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual_current.pdf.
Surveillance of healthcare-associated infections and prevention indicators in European intensive care units HAI-Net ICU protocol, version 2.2. 2015.
O’Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control 2011;39:S1–34. 4 Suppl 1
Safdar N, O’Horo JC, Ghufran A, Bearden A, Didier ME, Chateau D, et al. Chlorhexidine-impregnated dressing for prevention of catheter-related bloodstream infection: a meta-analysis*. Crit Care Med. 2014;42:1703–13.
Touré A, Chambrier C, Vanhems P, Lombard-Bohas C, Souquet J-C, Ecochard R. Propensity score analysis confirms the independent effect of parenteral nutrition on the risk of central venous catheter-related bloodstream infection in oncological patients. Clin Nutr. 2013;32:1050–4.
Catchpoole EM, Thirunavukarasu CE, Varelias A, Schlebusch S, Olver S, Zomerdijk N, et al. Early blood stream infections after BMT are associated with cytokine dysregulation and poor overall survival. Biol Blood Marrow Transplant. 2018;24:1360–6.
Author information
Authors and Affiliations
Contributions
Concept and design: ES, JS, MM, LG, IA, GT, JS; Acquisition of data: ES, LG, MK, SZ, CL, NB, IG, MOW, MG, ISO, IA, LY, MAB; Analysis and interpretation of data: ES, GT, PB, AL, JH, JS; Drafting of the manuscript: ES; Critical revision of the paper for important intellectual content: JS, MM, LG, AL, JH, MK, CL, NB, IA, JS; Statistical analysis: GT; Provision of study materials or patients: ES, LG, MK, SZ, CL, NB, IG, MOW, MG, ISO, IA, LY, MAB; Administrative, technical, or logistic support: PB, AL, JH, JS; Supervision: MM, JS.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
There are none relevant funding sources that supported this work.
Infectious Diseases Working Party and Nurses Group of the European Group for Blood and Marrow Transplantation.
Rights and permissions
About this article
Cite this article
Snarski, E., Stringer, J., Mikulska, M. et al. Risk of infectious complications in adult patients after allogeneic hematopoietic stem cell transplantation depending on the site of central venous catheter insertion—multicenter prospective observational study, from the IDWP EBMT and Nurses Group of EBMT. Bone Marrow Transplant 56, 2929–2933 (2021). https://doi.org/10.1038/s41409-021-01430-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-021-01430-7
- Springer Nature Limited
This article is cited by
-
Central venous access device terminologies, complications, and reason for removal in oncology: a scoping review
BMC Cancer (2024)
-
Impact of the insertion site of central venous catheters on central venous catheter-related bloodstream infections in patients with cancer: results from a large prospective registry
Infection (2023)