Abstract
There is limited information on the impact of CMV DNAemia episodes developing prior to engraftment (pre-CMV DNAemia) on clinical outcomes following allogeneic hematopoietic stem cell transplantation (allo-HSCT). This issue was addressed in the current retrospective multicenter study including 878 patients. All participant centers used preemptive antiviral therapy strategies for prevention of CMV disease. CMV DNA load in blood was monitored by real-time PCR assays. A total of 144 patients (cumulative incidence 16.5%, 95% CI, 14%–19%) had an episode of pre-CMV DNAemia at a median of 10 days after allo-HSCT. Patients who developed pre-CMV DNAemia had a significantly higher (P = < 0.001) probability of recurrent episodes (50%) than those who experienced post-CMV DNAemia (32.9%); Nevertheless, the incidence of CMV disease was comparable (P = 0.52). Cumulative incidences of overall mortality (OM) and non-relapse mortality (NRM) at 1-year after allo-HSCT were 32% (95% CI, 29–35%) and 23% (95% CI 20–26%), respectively. The risk of OM and NRM in adjusted models appeared comparable in patients developing a single episode of CMV DNAemia, regardless of whether it occurred before or after engraftment, in patients with pre- and post-engraftment CMV DNAemia episodes or in those without CMV DNAemia.
Similar content being viewed by others
Introduction
The incidence of Cytomegalovirus (CMV) end-organ disease following allogeneic hematopoietic stem cell transplantation (allo-HSCT) has been dramatically reduced due to the efficacy of antiviral therapy preventative strategies [1]. Nevertheless, CMV DNAemia, which is exceedingly common, has been associated with increased overall and non-relapse mortality (OM and NRM, respectively) in this setting [2,3,4,5]. Letermovir has been approved by regulatory agencies for prophylaxis of CMV infection in adult CMV-seropositive allo-HSCT recipients. Letermovir treatment decreases the risk of clinically significant CMV infection and OM through week 24 when compared to placebo [6]. Letermovir can be administered at any time point between the day of transplant and day 28 after allo-HSCT in the absence of CMV DNAemia.
CMV DNAemia developing prior to engraftment (pre-CMV DNAemia), which usually occur between the third and fourth week after allo-HSCT, may conceivably have a different course from that emerging after engraftment once patients have begun to expand donor-derived T cells (post-CMV DNAemia). There is limited information on the impact of CMV pre-DNAemia on clinical outcomes. Previous studies found no association between pre-CMV DNAemia an increased risk of CMV disease or mortality [7, 8]; these studies, however, were limited by their single center design and scarce number of events of interest. Here, we conducted a retrospective multicenter, noninterventional study to further address this issue.
Patients and methods
Study design and data collection
The current study enrolled 898 adult patients undergoing T-cell replete allo-HSCT at 20 different centers in Spain from September 2014 to December 2015 (Registry of the Working group on Infectious and Non-Infectious Complications of the GETH-Spanish Hematopoietic Transplantation and Cell Therapy Group-). A total of 218 adult patients who received an unmanipulated allo-HSCT at the Clinical University Hospital of Valencia from March 2010 to May 2019 (excluding patients recruited in the GETH registry) were also included. Out of the 1,116 patients, 238 patients were excluded from the study for one or more of the following reasons: lack of CMV DNA PCR results (n = 81), D and R CMV-seronegative status (n = 89), use of anti-CMV prophylaxis with (val)ganciclovir, foscarnet or letermovir (n = 68). Finally, the cohort consisted of 878 patients (Table 1) from 19 centers. Median age of patients at allo-HSCT was 53 years (range, 18–72). Clinical outcomes of interest included CMV DNAemia developing either before (pre-CMV DNAemia) or after (post-CMV DNAemia) engraftment, recurrent CMV DNAemia, CMV disease, OM and NRM through day 365 after transplantation. The study was approved by the Research Ethics Committees of the participating centers.
CMV DNA monitoring and management of CMV DNAemia
All centers used preemptive antiviral therapy (PET) strategies for prevention of CMV disease. Monitoring of CMV DNA load in blood was performed by commercial real-time PCRs at most centers (Table 2). Monitoring was conducted once a week through day +100 and at each scheduled visit thereafter. Patients at high risk for recurrences were also monitored on a weekly basis [1]. Patients with CMV DNAemia developing at any time point were monitored at least once a week until clearance. CMV surveillance began one or two weeks before allo-HSCT at eight out of 19 centers (42%). CMV DNA levels prompting PET are detailed in Table 2. In center 9, PET was initiated when plasma CMV DNA levels were above 1500 IU/ml or when the CMV DNA doubling time (dt) was ≤2 days, whichever occurred first [9]. (Val)ganciclovir or foscarnet at conventional doses were used for PET [1].
CMV DNA doubling time
The CMV DNA dt was calculated using the first 2 PCR positive results in the absence of antiviral treatment for analysis, as previously described [10].
Definitions
CMV DNAemia was defined as detection of CMV DNA in one or more blood specimens. Recurrent CMV DNAemia episodes were those occurring >15 after clearance of the previous one. Diagnosis and grading of aGvHD was done as previously detailed [11]. CMV disease was diagnosed according to published criteria [12]. The hematopoietic cell transplantation co-morbidity index (HCT-CI) was calculated as previously reported [13]. Engraftment was defined as absolute neutrophil count ≥500/mm3 on 3 consecutive days, the first of which being time of engraftment.
Statistical analysis
Cumulative incidences were assessed using the statistical software R (http://www.r-project.org/). OM was the total number of deaths from any cause. NRM was the total number of deaths in the absence of relapse or underlying disease progression. The causes of death were established as previously indicated [14]. Death and relapse were categorized as competing events for the cumulative incidence of CMV DNAemia. The Chi-squared test was used for frequency comparisons. Differences between medians were compared using the Mann–Whitney U-test and the Kruskal–Wallis test, when appropriate. Two-sided P values < 0.05 were deemed to be significant. Cox proportional hazards regression models were used to assess the potential risk factors for the occurrence of CMV DNAemia, OM and NRM. CMV DNAemia and aGvHD were treated as time-dependent variables. For multivariate analyses, only variables with parameter estimates showing a P value ≤ 0.10 in the univariate analyses were included. The latter statistical analyses were performed using SPSS version 20.0 (SPSS, Chicago, IL, USA).
Results
Occurrence of CMV DNAemia and CMV disease in the cohort
Out of 878 patients, 566 developed one (n = 355) or more (n = 211) episodes of CMV DNAemia through day +365 after allo-HSCT (cumulative incidence, 64%; 95% CI 61–67%). First episodes were detected at a median of 34 days after transplantation (range, −9 days to 354). Engraftment was achieved in 855 patients (97.4%) at a median of 19 days after allo-HSCT (range, 7–59 days).
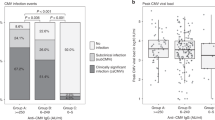
In total, 144 of the 566 episodes were detected prior to engraftment (cumulative incidence, 16.5%; 95% CI, 14–19%), at a median of 10 days (range, −9 to 59) after allo-HSCT, of which 24 developed during conditioning before stem cell infusion. PET was administered to 92 out of 144 patients with pre-CMV DNAemia (63.9%) and 300 out of 422 (71.1%) patients with post-CMV DNAemia (P = 0.12). Times to occurrence of pre-CMV DNAemia episodes (either treated with PET or self-resolving) in allo-HSCT recipients are shown in Fig. 1.
(Val)ganciclovir was used in monotherapy in 49 and 75% of pre- and post-CMV DNAemia episodes (P = <0.001). Foscarnet was prescribed alone in 19.6% and 14.3% of pre- and post-CMV DNAemia episodes (P = 0.25). Both drugs were given (sequentially) in the remaining episodes.
Among the 92 patients with pre-CMV DNAemia who underwent PET, 35 (42.7%) were treated before neutrophil’s engraftment, whereas PET was delayed until neutrophil engraftment in 47 patients (57.3%). This information was unavailable for the remaining 10 patients.
Recurrences were more frequent (P = <0.001) in patients with pre-CMV DNAemia (72 out of 144; 50%) than in those who experienced post-CMV DNAemia (139 out of 423; 32.9%). Nevertheless, PET was used comparably (P = 0.11) for recurrent CMV DNAemia that followed either pre-CMV DNAemia (50%) or post-CMV DNAemia (62%).
There were 31 cases of CMV end-organ CMV disease (n = 21 gastrointestinal, n = 6 pneumonitis; n = 2 encephalitis; n = 1 hepatitis and n = 1 retinitis) in our cohort (cumulative incidence, 3.5%; 95% CI 2–5%) that developed at a median of 72 days after transplantation (range, 2–224). Of these, 9 occurred in patients with pre-CMV DNAemia at a median of 103 days (2–158), 21 in patients with post-CMV DNAemia (median, 72 days; range, 27 to 224 days), and one in a patient without CMV DNAemia (day 44); Thus, the cumulative incidence of CMV disease was 7% (95% CI 3–13) and 5% (95% CI 3–8) in patients with pre-CMV and post-CMV DNAemia episodes, respectively (P = 0.52).
Baseline risk factors of pre-engraftment CMV DNAemia
Factors independently associated with increased risk of pre-CMV DNAemia were recipient CMV seropositivity, inclusion of post-transplant cyclophosphamide in aGvHD prophylaxis regimen and use of the Abbott PCR assay for CMV DNA monitoring (Table 3).
Kinetics of CMV DNAemia by episode type
The CMV DNA dt could be calculated for 82 episodes of pre-CMV DNAemia (56.9%) and 268 of post-CMV DNAemia (64%). The CMV DNA dt was comparable (P = 0.13) in pre-CMV DNAemia (median, 1.75 days; range, 0.44–6.42) and post-CMV DNAemia episodes (median, 2.0 days; range 0.23–6.11).
Pre-engraftment CMV DNAemia and mortality
In total, 279 patients died during the study period (mortality rate, 32%; 95% CI 29–35), at a median of 134 days after allo-HSCT (range, 2–365 days). Deaths were attributed to relapse (n = 75), aGvHD (n = 64), infection (n = 55) or other causes (n = 85). The 1-year cumulative incidence of NRM was 23% (95% CI 20–26%).
No difference (P = 0.10) was found regarding the cause of death between patients with pre-CMV DNAemia, post-CMV DNAemia and no CMV DNAemia (not shown).
As shown in Table 4, occurrence of pre-CMV DNAemia, considered as a qualitative variable, was not found to increase risk of OM or NRM. Similar data were obtained after excluding CMV D + /R− patients (not shown).
Moreover, OM and NRM risk in adjusted models appeared to be comparable in patients developing a single episode of CMV DNAemia within the study period, regardless of whether it occurred before (HR, 0.92; 95% CI, 0.53–1.60; P = 0.76 for OM and HR,0.81; 95% CI,0.41–1.58; P = 0.54) or after engraftment (HR, 0.83; 95% CI, 0.55–1.25; P = 0.38 for OM and HR, 0.78; 95% CI, 0.48–1.26; P = 0.31 for NRM), in patients with pre and post-CMV DNAemia episodes (HR, 0.87; 95% CI, 0.50–1.51; P = 0.62 for OM and HR, 0.66; 95% CI, 0.33–1.32; P = 0.24) or in those without CMV DNAemia throughout the study period (reference).
Factors independently associated with an increased risk of OM through day +365 in this series (Table 4) were HCT-CI score ≥3, UCB allograft, occurrence of CMV disease and grades III-IV aGvHD, for OM. Factors independently associated with increased risk of NRM were the use of antithymocyte globulin during the conditioning regimen, receipt of an UCB allograft and grades III-IV aGvHD (Table 4).
Finally, aGvHD developed at a comparable frequency (P = 0.79) in patients experiencing a single episode of pre-CMV DNAemia (43.1%), in those displaying post-CMV DNAemia (46.7%), or in those exhibiting pre-CMV and post-CMV DNAemia (48.6%).
Discussion
In this multicenter study we investigated the potential impact of pre-CMV DNAemia episodes on several clinical outcomes in allo-HSCT recipients. The data in the current study largely replicated those previously reported by one of the participating centers [7], and are summarized as follows. First, cumulative incidence of pre-CMV DNAemia episodes in this series was around 16%, a similar figure to the previously reported one (19%) [7], but higher than that found (6.5%) by Martin et al. [8] Differences can most likely be explained by use of a variety of real-time PCR assays displaying a wide range of LODs in the current and Martin’s studies as opposed to a single highly-sensitive PCR method in the former one [7]. In support of this view, use of the Abbott PCR assay (the most sensitive PCR assay across those used in this study) for CMV DNAemia monitoring was independently associated with increased risk of pre-CMV DNAemia. Baseline factors associated with occurrence of pre-CMV DNAemia episodes were recipient CMV seropositivity, in line with a previous report, [8] and use of post-transplant cyclophosphamide as aGvHD prophylaxis, this latter observation warranting confirmation in further series.
Second, the kinetics of CMV replication, as inferred by the CMV DNA dt, in pre-CMV DNAemia episodes appeared similar to that in post-CMV DNAemia episodes. The above parameter, in contrast to single CMV DNA load values, permits comparison between episodes monitored by different PCR assays, given their co-linearity across the entire range of viral load quantitation [15, 16]. It was assumed that plasma CMV DNA dt reflects the rate of CMV replication in organ and tissues, which is debatable.
Third, recurrent CMV DNAemia occurred at a higher frequency in patients with pre-CMV DNAemia than in those who experienced post-CMV DNAemia, yet the number of recurrences receiving PET was comparable. Delay in acquisition of protective CMV-specific T-cell responses in the former patients could account for this finding [17]; Nevertheless, arguing against this hypothesis, no difference in the incidence of CMV disease was noted across patients with pre or post-CMV DNAemia. In line with this latter finding, Martin et al. [8] reported no cases of CMV disease in their series. Moreover, in a very size-limited series, the frequency of peripheral blood CMV IE-1/pp65-specific IFN-γ-producing CD8+ T cells by day 30+ after allo-HSCT was found to be similar between groups [7].
Fourth, in a previous study including only patients from the GETH registry we failed to show an impact on mortality of CMV DNAemia occurring within the first year after allo-HSCT [18]. Here, pre-CMV DNAemia was also not found to be associated with an increased risk of OM or NRM when compared to that of post-CMV DNAemia or the absence of CMV DNAemia. The adverse effect of high HCT-CI index, use of UCB as the source of hematopoietic stem cells, and the occurrence of grades III-IV aGvHD or CMV disease on survival reported in the former study [18] was confirmed herein. As previously reported, [18] here we noticed that use of PET for CMV DNAemia was associated with higher OM and NRM in univariate, but not multivariate models. The limited number of deaths among patients with pre-CMV DNAemia undergoing to PET unfortunately precluded meaningful separate analysis.
The strength of the current study stems from its multicenter nature and the large cohort size. In addition to its retrospective design, the use of different PCR assays and blood matrices for CMV monitoring and the diversity of cut-offs for PET initiation and clinical practices across institutions could be construed as limitations of this study.
In summary, our data indicated that occurrence of pre-CMV DNAemia appeared not to have a detrimental impact on survival following allo-HSCT, despite predisposing to increased development of recurrent episodes.
References
Ljungman P, de la Camara R, Robin C, Crocchiolo R, Einsele H, Hill JA, et al. Guidelines for the management of cytomegalovirus infection in patients with haematological malignancies and after stem cell transplantation from the 2017 European Conference on Infections in Leukaemia (ECIL 7). Lancet Infect Dis. 2019;9:e260–e272.
Teira P, Battiwalla M, Ramanathan M, Barrett AJ, Ahn KW, Chen M, et al. Early cytomegalovirus reactivation remains associated with increased transplant-related mortality in the current era: a CIBMTR analysis. Blood. 2016;127:2427–38.
Green ML, Leisenring W, Xie H, Mast TC, Cui Y, Sandmaier BM, et al. Cytomegalovirus viral load and mortality after haemopoietic stem cell transplantation in the era of pre-emptive therapy: a retrospective cohort study. Lancet Hematol. 2016;3:e119–e127.
Solano C, Gimenez E, Pinana JL, Albert E, Vinuesa V, Hernández-Boluda JC et al. Impact of cytomegalovirus DNAemia on overall and non-relapse mortality in allogeneic stem cell transplant recipients. Transpl Infect Dis. 2017;19, https://doi.org/10.1111/tid.12717.
Giménez E, Torres I, Albert E, Piñana JL, Hernández‐Boluda JC, Solano C, et al. Cytomegalovirus (CMV) infection and risk of mortality in allogeneic hematopoietic stem cell transplantation (Allo‐HSCT): A systematic review, meta‐analysis, and meta‐regression analysis. Am J Transpl. 2019;19:2479–94.
Marty FM, Ljungman P, Chemaly RF, Maertens J, Dadwal SS, Duarte RF, et al. Letermovir prophylaxis for cytomegalovirus in hematopoietic-cell transplantation. N Engl J Med. 2017;377:2433–44.
Solano C, Giménez E, Albert E, Mateo EM, Gómez M, Goterris R, et al. Pre-engraftment cytomegalovirus DNAemia in allogeneic hematopoietic stem cell transplant recipients: incidence, risk factors, and clinical outcomes. Bone Marrow Transpl. 2019;54:90–98.
Martin I, Valsamakis A, Gladstone D, Jones R, Ambinder R, Avery RK. Cytomegalovirus in adult allogeneic blood and marrow transplant patients before or around the period of neutrophil recovery: a single-center, retrospective, descriptive study. Open Forum Infect Dis. 2020;7:ofaa081.
Solano C, Giménez E, Piñana JL, Vinuesa V, Poujois S, Zaragoza S, et al. Preemptive antiviral therapy for CMV infection in allogeneic stem cell transplant recipients guided by the viral doubling time in the blood. Bone Marrow Transpl. 2016;51:718–21.
Muñoz-Cobo B, Solano C, Costa E, Bravo D, Clari MÁ, Benet I, et al. Dynamics of cytomegalovirus (CMV) plasma DNAemia in initial and recurrent episodes of active CMV infection in the allogeneic stem cell transplantation setting: implications for designing preemptive antiviral therapy strategies. Biol Blood Marrow Transpl. 2011;17:1602–11.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974;18:295–304.
Ljungman P, Griffiths P, Paya C. Definitions of cytomegalovirus infection and disease in transplant recipients. Clin Infect Dis. 2002;34:1094–7.
Sorror ML. How I assess comorbidities before hematopoietic cell transplantation. Blood. 2013;121:2854–63.
Styczyński J, Tridello G, Koster L, Iacobelli S, van Biezen A, van der Werf S, et al. Death after hematopoietic stem cell transplantation: changes over calendar year time, infections and associated factors. Bone Marrow Transpl. 2020;55:126–36.
Cromer D, Tey SK, Khanna R, Davenport MP. Estimating cytomegalovirus growth rates by using only a single point. J Virol. 2013;87:3376–81.
Vinuesa V, Giménez E, Solano C, Gimeno C, Navarro D. Would kinetic analyses of plasma cytomegalovirus DNA load help to reach consensus criteria for triggering the initiation of preemptive antiviral therapy in transplant recipients? Clin Infect Dis. 2016;63:1533–5.
Navarro D, Amat P, de la Cámara R, López J, Vázquez L, Serrano D, et al. Efficacy and safety of a preemptive antiviral therapy strategy based on combined virological and immunological monitoring for active cytomegalovirus infection in allogeneic stem cell transplant recipients. Open Forum Infect Dis. 2016;3:ofw107.
Solano C, Vázquez L, Giménez E, de la Cámara R, Albert E, Rovira M, et al. Cytomegalovirus DNAemia and risk of mortality in allogeneic hematopoietic stem cell transplantation: analysis from the Spanish Hematopoietic Transplantation and Cell Therapy Group. Am J Transpl. 2020, https://doi.org/10.1111/ajt.16147.
Acknowledgements
Estela Giménez holds a Juan Rodés research contract from the Carlos III Health Institute (Ref. JR18/00053). Eliseo Albert holds a Río Hortega research contract from the Carlos III Health Institute (Ref. CM18/00221).
Funding
We thank Merck Sharp & Domme Spain (MSD) for providing the online platform for data registration. This work was funded by MSD through the Investigator Initiated Studies Program.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Solano, C., Vázquez, L., Giménez, E. et al. Clinical outcomes of allogeneic hematopoietic stem cell transplant recipients developing Cytomegalovirus DNAemia prior to engraftment. Bone Marrow Transplant 56, 1281–1290 (2021). https://doi.org/10.1038/s41409-020-01157-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-01157-x
- Springer Nature Limited
This article is cited by
-
Pre-engraftment Cytomegalovirus DNAemia after allogeneic hematopoietic stem cell transplantation and its impact on engraftment
Bone Marrow Transplantation (2022)