Abstract
In the absence of an HLA-matched donor, the best treatment for acquired aplastic anemia patients refractory to immunosuppression is unclear. We collected and analyzed data from all acquired aplastic anemia patients who underwent a haploidentical transplantation with posttransplant cyclophosphamide in Europe from 2011 to 2017 (n = 33). The cumulative incidence of neutrophil engraftment was 67% (CI95%: 51–83%) at D +28 and was unaffected by age group, stem cell source, ATG use, or Baltimore conditioning regimen. The cumulative incidence of grades II–III acute GvHD was 23% at D +100, and limited chronic GvHD was 10% (0–20) at 2 years, without cases of grade IV acute or extensive chronic GvHD. Two-year overall survival was 78% (64–93), and 2-year graft-versus-host disease-free survival was 63% (46–81). In univariate analysis, the 2-year OS was higher among patients who received the Baltimore conditioning regimen (93% (81–100) versus 64% (41–87), p = 0.03), whereas age group, stem cell source, and ATG use had no effect. Our results using unmanipulated haploidentical transplantation and posttransplant cyclophosphamide for treating refractory AA patients are encouraging, but warrant confirmation in a prospective study with a larger number of patients and longer follow-up.
Similar content being viewed by others
Introduction
About 30% of patients with severe aplastic anemia (SAA) treated with standard immunosuppressive treatment (IST) who lack a human leukocyte antigen (HLA)-matched sibling donor might be refractory [1, 2], and 30 to 60% may eventually relapse [2]. Allogeneic hematopoietic stem cell transplantation (HSCT) is the sole curative option; however, this choice depends on the patient’s eligibility to undergo HSCT and the availability of an HLA-matched unrelated donor (MUD) [3]. Strategies for transplant-eligible patients without an HLA-matched donor remain unsatisfactory.
Most refractory patients will remain unresponsive to second-line treatments and are at risk of life-threatening complications [4]. Eltrombopag provides hematological improvement to nearly 40% of refractory patients [5,6,7], and less than 30% respond to another cycle of IST [8, 9]. Furthermore, clonal evolution to myelodysplastic syndromes and acute myeloid leukemia are more frequent among refractory patients [10, 11] and are associated with a dismal prognosis.
HSCT using alternative sources (mismatched unrelated, cord blood, or haploidentical) may be curative and reduce the risk of clonal evolution. However, the risks of graft failure, severe infectious complications, and graft-versus-host disease (GvHD) might be higher than in transplantations using HLA-matched donors [3].
Nevertheless, the number of HSCTs using alternative donors for treating SAA patients has increased in Europe. In particular, the use of haploidentical donors leaped from six in 2007 to 58 in 2016 [12], especially with posttransplant cyclophosphamide (PTCy) as GvHD prophylaxis. Cyclophosphamide seems to deplete donor’s expanding alloreactive T cells between day +3 and day +4, reducing GvHD incidence and improving engraftment [13]. Yet few studies addressed this strategy in aplastic anemia (AA), and most are pediatric.
Here, we report the outcomes of SAA patients who underwent an unmanipulated haploidentical transplantation with PTCy in European Society for Blood and Bone Marrow Transplantation (EBMT) centers.
Methods
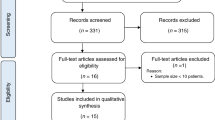
Study population and definitions
We extracted patient information from the EBMT ProMise database. We included all consecutive patients from 2010 to 2017 that fulfilled the three inclusion criteria: (a) diagnosis of acquired AA; (b) who received a mismatched-related donor transplantation; and (c) PTCy. Informed consent for transplantation was obtained according to European regulations and the Helsinki Declaration. The Severe Aplastic Anemia Working Party (SAA WP) scientific council approved this study. By EBMT guidelines, the SAA WP Data Office collected and analyzed data.
Definitions
The definitions used for data entry in the EBMT database are described elsewhere [14]. We classified patients younger than 18 years as pediatrics. Full donor chimaerism consisted in 95% cells of donor's origin; mixed chimaerism consisted in cells from both donor and recipient’s origin; autologous reconstitution consisted in cells of recipient’s origin; aplasia consisted in insufficient cells to measure chimaerism. The source of cells for chimaerism measurement was not available for this cohort. GvHD-free/relapse-free survival (GRFS) was defined as being alive without AA, acute GvHD (aGvHD) III/IV, extensive chronic GvHD (cGvHD) and graft loss [15]. GvHD-free survival (GFS) was defined as being alive without aGvHD grades III and IV, and no limited or extensive cGvHD. Neutrophil engraftment was defined as the time by which the absolute neutrophil count was >0.5 × 109/L for 3 consecutive days, and platelet engraftment as a platelet count >20 × 109/L or >50 × 109/L for seven consecutive days without transfusion support. The Baltimore conditioning regimen consisted of fludarabine 30 mg/m2 IV daily from day −6 to day −2 (total dose: 150 mg/m2), cyclophosphamide 14.5 mg/kg IV daily from day −6 to day −5 (total dose: 29 mg/kg) and total body irradiation (TBI) of 200 cGy on day −1 [13]. Cyclophosphamide was given at a dose of 50 mg/kg at D +3 and +4. We were unable to collect information regarding donor-specific antibodies. We did not evaluate the effect of graft cellularity on outcome variables due to insufficient data for 11 patients. Information about ABO matching was unavailable for the majority of patients and was therefore not included. We did not include patients who received combined peripheral blood (PB) and bone marrow grafts in comparisons of outcome variables stratified by stem cell source.
Statistics
We presented continuous variables as medians and range, and categorical variables as counts and percentages, and used the Fisher exact test for comparisons. Overall survival (OS), GFS and GRFS were calculated using the Kaplan–Meier product limit estimation method, and differences in subgroups were assessed by the log-rank test.
Median follow-up was determined using the reverse Kaplan–Meier method. Competing risks analyses were separately applied to estimate the incidences of aGvHD, cGvHD, neutrophil, and platelet engraftment. For each of the outcomes, the competing events were no engraftment, graft loss, relapse, second transplant, and death. Events for GRFS calculation were grade III–IV aGVHD, extensive cGVHD, no engraftment, graft loss, relapse, second transplant, and, death. Subgroup differences in competing risks analyses were assessed using the Gray’s test. OS, GFS, GRFS and cGvHD were evaluated at 2 years. Two-year outcomes were of specific interest; after 2 years, 17 patients were lost to follow-up. Estimates were provided at 12 months if the number of patients at risk in any of the subgroups being compared dropped below five by 24 months. Acute GvHD, platelet, and neutrophil engraftment endpoints were evaluated by day +100. All estimates were reported with 95% confidence intervals (CI95%). We did not include patients who received combined PB and bone marrow grafts in comparisons of outcome variables stratified by stem cell source. All p-values were two-sided and p < 0.05 was considered significant. Statistical results were reported following the EBMT statistical guidelines [16]. Statistical analyses were performed using the SPSS software, version 22 (SPSS Inc., Chicago, IL) and R statistical platform, version 3.0.3 (The R Foundation for Statistical Computing, Vienna, Austria) using packages ‘prodlim’, ‘survival’, and ‘cmprsk’.
Results
Patient, disease, and transplant characteristics
We identified and analyzed the total of 33 patients that fulfilled the inclusion criteria. Data were complete on all variables of interest for 26 individuals (78.7%). Thirty-two patients (97%) underwent at least one previous line of treatment (Table 1). Three patients received the haploidentical transplantation following a relapse after a previous transplant, and two patients after two transplantations. Four of these five previously transplanted patients had received transplants from a MUD. One patient had undergone two transplantations with a same haploidentical donor, but without PTCy (therefore not included in this study); a different haploidentical donor and PTCy were used for the third transplantation.
The median interval from diagnosis to transplant was 9.3 (1.9–201.2) months. One patient, diagnosed in 1998 with nonsevere AA, was treated with IST in 2013 because of disease progression, and subsequently transplanted the following year.
Donor and transplant characteristics are presented in Table 2. Two patients received a combined PB and bone marrow (BM) graft, but there is not enough information to specify whether it was part of a protocol. Five of the 12 patients transplanted with BM grafts for whom this information was available received less than 3 × 108 TNC/kg. Seven patients (21.2%) received a myeloablative conditioning and Baltimore was the most frequently used reduced-intensity conditioning regimen. Ten patients received in vivo T-cell depletion with antihuman thymocyte immunoglobulin (ATG) and none with alemtuzumab.
One 21-year-old man with very severe AA received an upfront haploidentical transplantation in 2016. He was transplanted from his 24-year-old brother 1.9 months after diagnosis, with a T-replete PB graft, and received Baltimore conditioning, PTCy, cyclosporin, and mycophenolate mofetil (MMF) as GvHD prophylaxis. He engrafted with full donor chimaerism, and was alive and GvHD-free at last follow-up (15.9 months).
Hematological recovery and engraftment
The cumulative incidence of neutrophil engraftment was 67% (CI95%: 51–83) at D +28 and 79% (65–93) at D +100 (Fig. 1). The median time for neutrophil engraftment was 22 days (CI95%: 18–26, range 11–98). Age group, stem cell source, conditioning regimen, and ATG use did not affect engraftment by day +28 (Table 3).
The cumulative incidences of platelet engraftment 20 × 109/L (Fig. 2a) and 50 × 109/L were 42% (26–59) and 14% (1–26) at D +28, 64% (47–80%) and 45% (27–63) at D +100, respectively. In univariate analysis, PB grafts yielded a higher 50 × 109/L engraftment (75% (51–99)) than BM grafts (25% (4–46%) p = 0.011) by D +100 (Fig. 2b), but no significant difference was seen for 20 × 109/L. Five patients were excluded from the former comparison: two because of combined marrow and PB grafts and three because of missing data on platelet 50 × 109/L engraftment.
a Stacked cumulative incidence of platelet engraftment 20 × 109/L. The area between the curves indicates the probability of having one of the corresponding events; the dark gray area indicates platelet engraftment and the light gray area the competing events. b The cumulative incidence of platelet engraftment 50 × 109/L stratified by stem cell source. The shaded areas indicate the corresponding 95% confidence intervals. The competing events were no engraftment, graft loss, relapse, second transplant, and death.
Information about chimaerism was available for 24 patients: 15 full donor, four mixed, two graft losses after successful engraftment, two autologous reconstitutions without significant hematological improvement, and one aplasia. From the entire cohort, seven patients failed to engraft (Table 3); four died and three were salvaged with another transplant. Four patients lost the graft—all before 5 months after transplantation—and one subsequently died.
Graft-versus-host disease
The cumulative incidence of aGvHD grades II–III was 23% at D +100 (Fig. 3); there were no reported cases of grade IV and grading was missing for two patients. The two-year cumulative incidence of limited cGvHD was 10% (0–20); there were no reported cases of extensive cGvHD. All cGvHD events reported here occurred before 2 years.
One- and 2-year GFS were 62% (45–79) and 58% (40–76), respectively. In univariate analysis, age group, stem cell source, or Baltimore conditioning results were comparable by 2 years (Table 3). By 1 year, ATG use also had no significant effect on GFS: ATG 40% (10–70), no ATG, 73% (54–92), p = 0.09.
GRFS was 63% (46–81) at 1 and 2 years. In univariate analysis, age group, stem cell source, or Baltimore conditioning regimen did not affect GRFS (Table 3). By 1 year, ATG use had no effect on GRFS: ATG 57% (20–94), no ATG 65% (46–85), p = 0.75.
OS and mortality
With a median follow-up of 35.9 (24.6–43.0) months, 1 and 2-year OS were 82% (68–95) and 78% (64–93), respectively (Fig. 4a). When stratified by conditioning regimen, Baltimore yielded a higher 2-year OS (93% (81–100)) when compared with nonBaltimore regimens (64% (41–87), p = 0.03) in univariate analysis (Fig. 4b). Age group, stem cell source, or ATG use did not affect 2-year OS (Table 3). In total, seven patients died within the first 2 years after haploidentical transplantation: five of infection, one of PTLD, and the other of transplant-related toxicity. Another patient died of infection 39 months after transplantation.
Discussion
This is the largest multicentric cohort reporting the outcomes of haploidentical transplantation using unmanipulated graft and PTCy for refractory SAA patients. We report good neutrophil engraftment and survival, low incidence of acute and cGvHD without any severe cases, and an acceptable GRFS.
The prognosis of refractory SAA patients has improved in the last decades. Five-year OS increased from 23% in the 90 s to 57% (p < 0.001) in 2000. This improvement is due to the progress in antifungal therapy [17], and better HLA matching for transplantation from MUD [18, 19]. The best treatment for transplant-eligible refractory patients aged 30 years or less for whom a MUD is available is transplantation [2, 3, 18]. In the absence of a MUD, the best option is not consensual [2]. Still, patients receiving nontransplant treatments face the risks of clonal evolution and chronic transfusions [10, 20]. Alternative donor transplantation might cure and provide a good quality of life; however, nonengraftment, GvHD and infections are concerns.
We report a 2-year OS of 78% in a population with a median age of 20.4 years. By 2 years, pediatric patients presented a 92% OS compared with 69% for adults, but this difference was not significant (p = 0.12). Our results compare favorably with the best supportive care and previous retrospective studies using cord blood, mismatched unrelated donors, or haploidentical donors. Unrelated cord blood transplantation provided a 3-year OS of 38% [21]. Using the best predictive factors of the previous report, a phase 2 study found a 1-year OS of 88.5% but nonnegligible GvHD in young patients [22], emphasizing the need of prospective studies. One-antigen mismatched unrelated donors provided a 5-year OS of 57% to 72.7% in retrospective studies [23, 24], and prognosis was worse if more than one mismatch were present [25]; the CI of cGvHD was about than 25% in these cohorts. Haploidentical donors seems an acceptable strategy according to other retrospective studies: ex-vivo T-cell depletion provided excellent OS and low GvHD incidence in refractory SAA of pediatric patients, but at the expense of delayed immune reconstitution and considerable viral reactivation [26, 27]; ATG, posttransplant intensified immunosuppression and combined PB and BM grafts provided adequate engraftment and survival [28,29,30,31,32,33,34], but nonnegligible GvHD. One multicentric prospective study using the GIAC strategy found a 3-year OS of 89% with a CI of extensive cGvHD of 10% [35].
We do not report any cases of acute grade IV or extensive cGvHD, nor any deaths related to GvHD. Our results are in alignment with previous reports of unmanipulated haploidentical transplantation with PTCy: one study with 16 patients reported a 1-year OS of 67.1% with three patients presenting grade II–IV aGvHD [36]; another study with eight patients reported six engraftments and no severe aGvHD [37]. In both, all patients received the Baltimore conditioning regimen. Adding ATG to this regimen, a phase 2 study reported all 16 patients receiving alternative transplantation—13 haploidentical—alive and off immunosuppression by 21 months [38].
In our study, patients conditioned with the Baltimore regimen presented a better OS than the heterogeneous group of nonBaltimore regimens (2-year OS of 93% vs. 64%, respectively, p = 0.03) that comprised 41% of myeloablative conditioning. Deaths occurred mostly early after transplantation in the nonBaltimore group, likely because of toxicity. The combination of fludarabine and cyclophosphamide is currently the backbone for conditioning alternative donor transplantations in SAA patients [22, 39]. The inclusion of low-dose TBI seems to reduce the risk of rejection without prohibitive toxicity [40, 41].
We did not identify the benefit of ATG in reducing GvHD and improving survival reported in sibling or unrelated donor transplants [41, 42]. We saw less engraftment among patients treated with ATG; although suggestive, this difference was not significant.
We did not confirm the expected lower incidence of GvHD with BM grafts in SAA patients [43, 44]; we found no stem cell source effect on GvHD or survival. The use of PB grafts was associated with better platelet engraftment. Though missing data on cellularity precludes firm conclusions, we speculate that the number of infused cells might have influenced. No patients transplanted with a PB graft received a dose inferior to recommendations, whereas about 30% (5/17) of BM did [45, 46].
We acknowledge that the sample size precluded multivariate analyses and reduced power. Other limitations were the lack of data concerning donor-specific antibodies, ABO matching, and chimaerism, and the retrospective nature of this study.
In conclusion, we confirm the encouraging initial results of unmanipulated haploidentical transplantation using the Baltimore conditioning regimen and PTCy for refractory SAA patients. We found that 63% of the overall patients and 73% of those treated with the Baltimore regimen were alive, transfusion-independent, and without severe GvHD 2 years later. We could not find any stem cell source effect on survival in this cohort; the impact of ATG and patient’s age in haploidentical transplantation with PTCy for SAA needs to be measured in a larger population. We plan to conduct a prospective phase two trial using the Baltimore conditioning to confirm the safety and efficacy of haploidentical transplantation with PTCy for treating relapsed or refractory SAA patients.
References
Young NS. Aplastic anemia. N. Engl J Med. 2018;379:1643–56.
Bacigalupo A. How I treat acquired aplastic anemia. Blood. 2017;129:1428–36.
Peffault de Latour R. Transplantation for bone marrow failure: current issues. Hematology. 2016;90–8.
Scheinberg P, Cooper JN, Sloand EM, Wu CO, Calado RT, Young NS. Association of telomere length of peripheral blood leukocytes with hematopoietic relapse, malignant transformation, and survival in severe aplastic anemia. JAMA. 2010;304:1358–64.
Olnes MJ, Scheinberg P, Calvo KR, Desmond R, Tang Y, Dumitriu B, et al. Eltrombopag and improved hematopoiesis in refractory aplastic anemia. N. Engl J Med. 2012;367:11–9.
Townsley DM, Olnes MJ, Broder K, Scheinberg P, Desmond R, Bevans M, et al. Eltrombopag restores trilineage hematopoiesis in refractory severe aplastic anemia that can be sustained on discontinuation of drug. Blood. 2013;123:1818–25.
Lengline E, Drenou B, Peterlin P, Tournilhac O, Abraham J, Berceanu A, et al. Nationwide survey on the use of eltrombopag in patients with severe aplastic anemia: a report on behalf of the french reference center for aplastic anemia. Haematologica. 2018;103:212–20.
Cle DV, Atta EH, Dias DSP, Lima CBL, Bonduel M, Sciuccati G, et al. Repeat course of rabbit antithymocyte globulin as salvage following initial therapy with rabbit antithymocyte globulin in acquired aplastic anemia. Haematologica. 2015;100:e345–7.
Trcuelu A, Passweg J, Nissen C, Bargetzi M, Hoffmann T, Signer E, et al. Repeated treatment with horse antilymphocyte globulin for severe aplastic anaemia. Br J Haematol. 1998;100:393–400.
Yoshizato T, Dumitriu B, Hosokawa K, Makishima H, Yoshida K, Townsley D, et al. Somatic mutations and clonal hematopoiesis in aplastic anemia. N. Engl J Med. 2015;373:35–47.
Scheinberg P, Young NS. How I treat acquired aplastic anemia. Blood. 2014;120:1185–96.
Bacigalupo A. Alternative donor transplants for severe aplastic anemia. Hematology. 2018;467–73.
Luznik L, Donnell PVO, Symons HJ, Chen AR, Susan M, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transpl. 2008;14:641–50.
European Society for Blood and Marrow Transplantation. MED-AB forms manual a guide to the completion of the EBMT HSCT Med-AB forms [Internet]. 2018. p. 1–152. https://www.ebmt.org/sites/default/files/2018-03/MED-AB Forms Manual.pdf.
Battipaglia G, Ruggeri A, Labopin M, Volin L, Blaise D, Socie G, et al. Refined graft-versus-host disease/relapse-free survival in transplant from HLA-identical related or unrelated donors in acute myeloid leukemia. Bone Marrow Transpl. 2018;53:1295–303.
Iacobelli S. Suggestions on the use of statistical methodologies in studies of the European Group for Blood and Marrow Transplantation. Bone Marrow Transpl. 2013;48:S1–37.
Valdez JM, Scheinberg P, Nunez O, Wu CO, Young NS, Walsh TJ. Decreased infection-related mortality and improved survival in severe aplastic anemia in the past two decades. Clin Infect Dis. 2011;52:726–35.
Devillier R, Dalle J-HH, Kulasekararaj A, D’aveni M, Clément L, Chybicka A, et al. Unrelated alternative donor transplantation for severe acquired aplastic anemia: a study from the french society of bone marrow transplantation and cell therapies and the EBMT severe aplastic anemia working party. Haematologica. 2016;101:884–90.
Maury S, Chir Z, Boiron J, Galambrun C, Yakouben K, Bordigoni P, et al. Unrelated stem cell transplantation for severe acquired aplastic anemia: improved outcome in the era of high-resolution HLA matching between donor and recipient. Haematologica. 2007;92:589–96.
Socie G, Henry-Amar M, Bacigalupo A, Hows J, Tichelli A, Ljungman P, et al. Malignant tumors occurring after treatment of aplastic anemia. European Bone Marrow Transplantation-Severe Aplastic Anaemia Working Party. N. Engl J Med. 1993;329:1152–7.
Peffault de Latour R, Purtill D, Ruggeri A, Sanz G, Michel G, Gandemer V, et al. Influence of nucleated cell dose on overall survival of unrelated cord blood transplantation for patients with severe acquired aplastic anemia: a study by eurocord and the aplastic anemia working party of the european group for blood and marrow transplant. Biol Blood Marrow Transpl. 2011;17:78–85.
Peffault de Latour R, Chevret S, Jubert C, Sirvent A, Galambrun C, Ruggeri A, et al. Unrelated cord blood transplantation in patients with idiopathic refractory severe aplastic anemia: a nationwide phase 2 study. Blood. 2018;132:750–4.
Horan J, Wang T, Haagenson M, Ayas M, Baxter-Lowe LA, Bielorai B, et al. Evaluation of HLA matching requirements in unrelated hematopoietic stem cell transplantation for nonmalignant disorders. Blood. 2012;120:2918–24.
Yagasaki H, Kojima S, Yabe H, Kato K, Kigasawa H, Sakamaki H, et al. Acceptable HLA-mismatching in unrelated donor bone marrow transplantation for patients with acquired severe aplastic anemia. Blood. 2011;118:3186–90.
Passweg JR, Përez WS, Eapen M, Camitta BM, Gluckman E, Hinterberger W, et al. Bone marrow transplants from mismatched related and unrelated donors for severe aplastic anemia. Bone Marrow Transpl. 2006;37:641–9.
Kim H, Im HJ, Koh K-N, Kang SH, Yoo JW, Choi ES, et al. Comparable outcome with a faster engraftment of optimized haploidentical hematopoietic stem cell transplantation compared with transplantations from other donor types in pediatric acquired aplastic anemia. Biol Blood Marrow Transpl. 2019;25:965–74.
Im HJ, Koh KN, Seo JJ, Choi ES, Jang S, Kwon SW, et al. Excellent outcome of haploidentical hematopoietic stem cell transplantation in children and adolescents with acquired severe aplastic anemia. Biol Blood Marrow Transpl. 2013;19:754–9.
Gao L, Li Y, Zhang Y, Chen X, Gao L, Zhang C, et al. Long-term outcome of HLA-haploidentical hematopoietic SCT without in vitro T-cell depletion for adult severe aplastic anemia after modified conditioning and supportive therapy. Bone Marrow Transpl. 2014;49:519–24.
Li XH, Gao CJ, Da WM, Bin CaoY, Wang ZH, Xu LX, et al. Reduced intensity conditioning, combined transplantation of haploidentical hematopoietic stem cells and mesenchymal stem cells in patients with severe aplastic anemia. PLoS ONE. 2014;9:1–7.
Yamei W, Rongmu L, Yongbin C, Yingjian S, Xiaohong L. Improved outcome of haploidentical transplantation in severe aplastic anemia using reduced-intensity fludarabine-based conditioning. Oncotarget. 2017;8:83817–30.
Xu ZL, Zhou M, Jia JS, Mo WJ, Zhang XH, Zhang YP, et al. Immunosuppressive therapy versus haploidentical transplantation in adults with acquired severe aplastic anemia. Bone Marrow Transpl. 2019;54:1319–26.
Zhu H, Luo RM, Luan Z, Lee V, Zhu YP, Luo CJ, et al. Unmanipulated haploidentical haematopoietic stem cell transplantation for children with severe aplastic anaemia. Br J Haematol. 2016;174:799–805.
Yang S, Yuan X, Ma R, Jiang L, Guo J, Zang Y, et al. Comparison of outcomes of frontline immunosuppressive therapy and frontline haploidentical hematopoietic stem cell transplantation for children with severe aplastic anemia who lack an HLA-matched sibling donor. Biol Blood Marrow Transpl. 2019;25:975–80.
Xu LP, Jin S, Wang SQ, Xia LH, Bai H, Gao SJ, et al. Upfront haploidentical transplant for acquired severe aplastic anemia: registry-based comparison with matched related transplant. J Hematol Oncol. 2017;10:1–10.
Xu L-PP, Wang S-QQ, Wu D-PP, Wang J-MM, Gao S-JJ, Jiang M, et al. Haplo-identical transplantation for acquired severe aplastic anaemia in a multicentre prospective study. Br J Haematol. 2016;175:265–74.
Esteves I, Bonfim C, Pasquini R, Funke V, NF P, Rocha V, et al. Haploidentical BMT and post-transplant Cy for severe aplastic anemia: a multicenter retrospective study. Bone Marrow Transpl. 2015;50:685–9.
Clay J, Kulasekararaj AG, Potter V, Grimaldi F, McLornan D, Raj K, et al. Nonmyeloablative peripheral blood haploidentical stem cell transplantation for refractory severe aplastic anemia. Biol Blood Marrow Transpl. 2014;20:1711–6.
DeZern AE, Zahurak M, Symons H, Cooke K, Jones RJ, Brodsky RA. Alternative donor transplantation with high-dose post-transplantation cyclophosphamide for refractory severe aplastic anemia. Biol Blood Marrow Transpl. 2017;23:498–504.
Anderlini P, Wu J, Gersten I, Ewell M, Tolar J, Antin JH, et al. Cyclophosphamide conditioning in patients with severe aplastic anaemia given unrelated marrow transplantation: a phase 1–2 dose de-escalation study. Lancet Haematol. 2015;2:e367–75.
Deeg HJ, Amylon ID, Harris RE, Collins R, Beatty PG, Feig S, et al. Marrow transplants from unrelated donors for patients with aplastic anemia: minimum effective dose of total body irradiation. Biol Blood Marrow Transpl. 2001;7:208–15.
Bacigalupo A, Socie G, Hamladji RM, Aljurf M, Maschan A, Kyrcz-Krzemien S, et al. Current outcome of HLA identical sibling versus unrelated donor transplants in severe aplastic anemia: An EBMT analysis. Haematologica. 2015;100:696–702.
Giammarco S, Peffault de Latour R, Sica S, Dufour C, Socie G, Passweg J, et al. Transplant outcome for patients with acquired aplastic anemia over the age of 40: has the outcome improved? Blood. 2018;131:blood-2018-01-826495.
Bacigalupo A, Socié G, Schrezenmeier H, Tichelli A, Locasciulli A, Fuehrer M, et al. Bone marrow versus peripheral blood as the stem cell source for sibling transplants in acquired aplastic anemia: Survival advantage for bone marrow in all age groups. Haematologica. 2012;97:1142–8.
Schrezenmeier H, Passweg JR, Marsh JCW, Bacigalupo A, Bredeson CN, Bullorsky E, et al. Worse outcome and more chronic GVHD with peripheral blood progenitor cells than bone marrow in HLA-matched sibling donor transplants for young patients with severe acquired aplastic anemia. Blood. 2007;110:1397–400.
Gorin C. Bone marrow harvesting for HSCT. In: Carreras E, Dufour C, Mohty M, Kröger N, editors. The EBMT handbook. Cham, Switzerland: Springer Open; 2019. p. 109–16.
Hübel K. Mobilization and collection of HSC. In: Carreras E, Dufour C, Mohty M, Kröger N, editors. The EBMT handbook. Cham, Switzerland: Springer Open; 2019. p. 117–24.
Acknowledgements
The authors are grateful to the Fondation HPN France—Aplasie Médullaire (Paroxysmal Nocturnal Hemoglobinuria—Aplastic Anemia Foundation in France) for helping fund this study.
Author information
Authors and Affiliations
Consortia
Contributions
PHP, RPL, CD and AR planned this study. PHP, DJE and RPL wrote the paper with support of GS. PB was responsible for data collection and processing. DJE performed statistical analyses. All authors provided critical feedback and helped shape the research, analyses, and paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Prata, P.H., Eikema, DJ., Afansyev, B. et al. Haploidentical transplantation and posttransplant cyclophosphamide for treating aplastic anemia patients: a report from the EBMT Severe Aplastic Anemia Working Party. Bone Marrow Transplant 55, 1050–1058 (2020). https://doi.org/10.1038/s41409-019-0773-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-019-0773-0
- Springer Nature Limited
This article is cited by
-
Second haploidentical bone marrow transplantation with antithymocyte antibody-containing conditioning regimen for graft failure in eight patients with severe aplastic anemia
Scientific Reports (2024)
-
Addition of ruxolitinib to standard graft-versus-host disease prophylaxis for allogeneic stem cell transplantation in aplastic anemia patients
Bone Marrow Transplantation (2024)
-
Recent advances in the diagnosis and treatment of pediatric acquired aplastic anemia
International Journal of Hematology (2024)
-
Allogeneic bone marrow transplantation for aplastic anemia
International Journal of Hematology (2024)
-
Thiotepa-based reduced toxicity conditioning in combination with post-transplant cyclophosphamide and mTOR inhibitor for heavily transfused acquired severe aplastic anemia in children and young adults: encouraging outcomes of a pilot study
Bone Marrow Transplantation (2023)