Abstract
Objective
Whole-body vibration (WBV) appears to modulate reflex hyperexcitability and spasticity. Due to common underlying neural mechanisms between spasticity and neuropathic pain, WBV may also reduce chronic pain after spinal cord injury (SCI). Our objective was to determine whether there are dose-related changes in pain following WBV and to examine the relationships between neuropathic pain and reflex excitability.
Study design
Secondary analysis of a sub-population (participants with neuropathic pain, n = 16) from a larger trial comparing the effects of two different doses of WBV on spasticity in persons with SCI.
Setting
Hospital/Rehabilitation Center in Atlanta, GA, USA.
Methods
Participants were randomized to 8-bout or 16-bout WBV groups. Both groups received ten sessions of sham intervention, followed by ten sessions of WBV. Primary measures included the Neuropathic Pain Symptom Inventory (NPSI) for pain symptom severity and H-reflex paired-pulse depression (PPD) for reflex excitability.
Results
Mean change in NPSI scores were not significantly different between the groups (7 ± 6; p = 0.29; ES = 0.57); however, 8-bouts of WBV were consistently beneficial for participants with high neuropathic pain symptom severity (NPSI total score >30), while 16-bouts of WBV appeared to increase pain in some individuals with high NPSI scores. A baseline NPSI cut score of 30 predicted PPD response (sensitivity = 1.0, specificity = 0.83), with higher NPSI scores associated with decreased PPD in response to WBV.
Conclusions
WBV in moderate doses appears to decrease neuropathic pain symptoms and improve reflex modulation. However, at higher doses neuropathic pain symptoms may be aggravated. Lower baseline NPSI scores were associated with improved reflex modulation.
Similar content being viewed by others
Introduction
Spasticity and chronic pain are frequent consequences of spinal cord injury (SCI), affecting more than two-thirds of persons with SCI [1]. Furthermore, spasticity and muscle spasms are significantly more common in individuals who experience chronic pain after their SCI than in those who do not [2], and the severity and impact of both chronic pain and spasticity seem to be closely related [3]. Systematic reviews have concluded that pharmacological approaches do not consistently relieve either spasticity [4] or neuropathic pain [5] and are often associated with an unfavorable risk/benefit ratio. Due to the limitations of pharmacological interventions, there is an interest in the use of non-pharmacological approaches including physical therapy to reduce spasticity and neuropathic pain.
Basic and clinical studies support a relationship between pain and spasticity after SCI [3, 6], and spasticity and neuropathic pain after SCI are both associated with central sensitization [7]. Following SCI, dysregulation of chloride homeostasis and upregulation of serotonin receptors in the spinal cord circuits leads to loss of inhibitory signaling by GABA. These pathological mechanisms result in an increased neuronal excitability that contributes to both spasticity and pain [8, 9]. Afferent input associated with movement, stimulation, and vibration reduces the excitability of segmental reflex circuits, presumably through activation of presynaptic inhibitory pathways [10, 11]. Likewise, stimulation of large-diameter afferents and their central pathways via dorsal column stimulation or peripheral stimulation (e.g., transcutaneous electrical nerve stimulation) has long been used to treat various chronic pain conditions [12].
Whole-body vibration (WBV) is a modality that offers an accessible approach for a generalized activation of sensory afferents. WBV activates presynaptic inhibitory mechanisms that modulate segmental reflex excitability [13] and has been shown to reduce spasticity in persons with chronic SCI [14, 15]. Research indicates that WBV may also be of value for the management of chronic pain conditions [16], with basic research demonstrating a reduction in both mechanical hyperalgesia and thermal hot pain perception thresholds after a series of WBV sessions [17].
The purpose of this study was to examine dose-related changes in neuropathic pain severity following a WBV intervention and to explore the relationship between measures of pain and reflex excitability. The present study compared dose-response effects for WBV applied at 50 Hz over 8 bouts/session versus over 16 bouts/session. We hypothesized that larger doses of WBV would be associated with greater reduction in neuropathic pain severity and that there would be a significant relationship between neuropathic pain and spasticity.
Methods
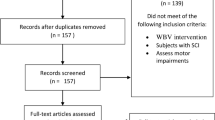
This study was a secondary analysis of a subset of participants (i.e., only those with chronic neuropathic pain) from a larger study (n = 35) on the dose-response effects of WBV on spasticity and walking function in persons with SCI. To be included in the study participants were required to: (1) demonstrate sufficient motor function to stand for at least 1 min using upper extremities only for balance, (2) while standing advance 1 leg at least a small amount (with or without an assistive device), (3) have at least mild spasticity affecting the lower extremity muscles (as indicated by an increased responsiveness to passive stretch), and (4) have the ability to rise from sit to stand with no more than moderate assistance of one person. Individuals were excluded from participation if they had a neurological level of injury below T12, progressive or potentially progressive spinal lesions, history of severe or chronic cardiovascular irregularities, difficulty following instructions, or orthopedic conditions that would prevent participation in WBV (e.g., recent fracture, lower extremity flexion contractures >10 degrees). The original study was conducted under the approval of the Shepherd Center Research Review Committee and registered with clinicaltrials.gov (NCT02340910).
Interventions
We used a wash-in control > intervention > wash-out study design (Fig. 1), where the wash-in phase constituted assessment timepoints T1–T2, the WBV intervention phase constituted assessment timepoints T2–T3, and the wash-out phase constituted assessment timepoints T3–T4.
Participants were randomized into two groups receiving either 8-bouts/session of WBV or 16-bouts/session of WBV. During the wash-in control phase participants performed the same sitting-standing movements performed during the WBV intervention phase, except that they received sham electrical stimulation to the scapular regions instead of vibration.
Each bout comprised of standing with either sham-stimulation (wash-in control phase) or WBV (intervention phase) for 45 s followed by 1 min of seated rest. To maintain equality of total participation time between the 8-bout WBV and 16-bout WBV groups, the sitting/standing bouts were counterbalanced between phases such that participants in the 8-bout WBV group received 16 bouts of the active-control intervention during the wash-in phase, and vice versa. The WBV doses were derived from an earlier study, which determined that WBV at 50 Hz over 8 bouts was associated with larger effects on spasticity than WBV applied at lower frequency and fewer bouts [14]. The study design allowed us to assess the effects of an active control (wash-in; repeated sitting > standing > sitting) versus WBV (intervention), and any persistent effects (wash-out) associated with the two different doses of WBV. The wash-in control was important as our prior studies have shown that repeated sitting-standing-sitting has itself affected spasticity [14]. During the wash-out period, no intervention was administered.
Outcomes assessment
Assessment of pain
The Neuropathic Pain Symptom Inventory (NPSI) was used to assess neuropathic pain symptom severity. The NPSI includes severity ratings of ten descriptive adjectives reflecting spontaneous ongoing or paroxysmal pain, evoked pain (i.e. mechanical and thermal allodynia/hyperalgesia), dysesthesia/paresthesia and two items regarding the duration of ongoing and paroxysmal pain. The NPSI has been shown to be both valid and reliable in a variety of populations with neuropathic pain [18], including SCI [19]. The International Spinal Cord Pain Basic dataset was used to classify pain type and to assess the pain intensity (numeric rating scale (NRS); 0–10) of up to three separate pains [20]. The NRS scores reported in this study are the average intensity of neuropathic pain symptoms over the 7 days preceding assessment for each measurement reported. The pain severity subscale of the West Haven-Yale Multidimensional Pain Inventory: SCI version (MPI-PS) was used to assess overall pain severity. The MPI-PS consists of three items which are answered on a seven-point Likert scale with a potential range of 0–6 [21].
Assessment of segmental reflex excitability and modulation
To examine reflex excitability, we used both biomechanical and electrophysiologic biomarkers of spasticity. The pendulum test was used to assess excitability in response to gravity-evoked stretch of the quadriceps muscle. This method has been described in detail elsewhere [22], and this test has been shown to be a reproducible, valid, and sensitive measure of spasticity [23]. Briefly, participants were positioned supine on a mat with the lower legs hanging over the edge, and the examiner released the heel allowing the lower leg to swing. The angle at which the swinging leg first reversed direction from flexion to extension represents the first swing excursion (FSE), and a smaller FSE angle indicates greater quadriceps excitability (i.e., spasticity). The knee angle during the pendulum test was collected via an inertial motion capture system (XSENS Technologies, the Netherlands).
Excitability of the soleus muscle was assessed based on modulation of the soleus H-reflex using procedures described in our prior studies [24]. Stimulating electrodes were placed over the tibial nerve in the popliteal fossa, and pulses of 1 ms duration (via a Digitimer DS7A constant current stimulator) were delivered with increasing intensity until a maximum H-reflex (Hmax) and M-wave (Mmax) were observed. Homosynaptic modulation of the soleus H-reflex was assessed based on pair-pulse post-activation depression (PPD; in µV) with stimulus intensities of 20–40% Mmax with interstimulus intervals of 1 s between stimulus pairs.
Previous work suggests that detailed data on pain symptom severity, such as that provided by the NPSI, may be useful for understanding neuropathic pain mechanisms and for phenotyping neuropathic pain [19]. Additionally, previous studies have identified PDD as a potential tool to assess the relative contribution of spinal inhibitory dysfunction and segregation of peripherally from centrally generated pain in diabetic neuropathy [25]. Thus, the NPSI and the PPD were the primary measures of interest for this study.
Statistical analysis
To assess the change between assessment timepoints, values from the earlier timepoint were subtracted from the later timepoint; accordingly, a decrease in pain scores between T1 and T2 would be indicated by a negative value. Tests for normality indicated that the primary measures of interest, NPSI and PPD, were normally distributed (Shapiro–Wilk test statistic = 0.915 and 0.921; p = 0.139 and 0.366, respectively); thus, parametric statistical tests were used. Due to the exploratory nature of this study, we followed published guidance from experts in clinical trial design defining statistical significance as p ≤ 0.10 to reduce the likelihood of Type II errors [26]. Pearson’s correlation coefficient was used to assess the relationship between baseline pain and physiological outcomes. Paired sample t-tests were used to assess change in measures across timepoints, and both chi-square tests and independent sample t-tests were used to compare differences between treatment groups. To assess baseline differences between groups we compared injury characteristics, age, gender, race, and walking capacity. Walking capacity was scored based on ratings in the Temporal/Distance domain of the Spinal Cord Injury Functional Ambulation Inventory [27]. Cohen’s d was used to determine effect sizes for WBV on pain and on reflex excitability. Because statistical tests have low power when sample sizes are small, and because effects sizes are more meaningful than p values in these situations [28], in the results we report the effect sizes for changes in pain and physiological measures.
To assess the relationship between the NPSI and PPD, the entire sample was dichotomized into responders (PPD change >0) and non-responders (PPD change ≤0) to WBV based on the difference between baseline (T1) and T3. Independent t-tests were used to examine differences between responders and non-responders. Receiver operator characteristic curve and chi-square analyses were used to determine the utility of baseline NPSI scores to correctly predict response to WBV, and Pearson’s correlation was used to quantify the relationship between baseline NPSI scores and PPD change.
Results
Baseline
Of the 35 participants in the full study sample, 16 experienced neuropathic pain and were included in the analyses. All participants had neuropathic pain symptoms below the level of injury, and none had neuropathic pain symptoms at the level of injury. Table 1 shows demographic and background information. Injury characteristics and demographic factors were not significantly different at baseline for the 8-bout and 16-bout groups (n = 8 for each group, p > 0.10). Regarding medication use, 63% of the 8-bout WBV group were using opioid medication versus 25% of the 16-bout WBV group (p = 0.31). Further, all members of the 8-bout WBV group were taking antispasmodics, while only 25% (n = 2) of the 16-bout WBV group were taking antispasmodics (p < 0.001).
The groups were not significantly different with respect to baseline pain or outcomes on the pendulum test. However, pain scores varied from mild pain to severe pain among participants, and the 8-bout WBV group had significantly higher average baseline PPD values (mean difference = 23µV ± 8µV; p = 0.02) (Table 1).
Table 2 shows the correlations between all measures of interest at baseline. As expected, the NPSI total score was strongly correlated with the 7-day-average NRS scores (r = 0.84, p < 0.001) and the MPI-PS (r = 0.70, p < 0.001). Similarly, baseline PPD and pendulum FSE were moderately correlated (r = 0.55, p = 0.08). However, the baseline pain measures were not significantly correlated to the baseline physiological measures (r values between −0.02 and 0.44, p > 0.10).
Effect of WBV on pain
Table 3 shows the change in pain scores for each phase of the study. Pain measures were not completed at T2 for one participant in the 8-bout WBV group; thus, pairwise analysis across timepoints was only conducted on seven participants in the group. Only the 8-bout WBV group exhibited a significant decrease in NRS scores between T1–T2. Analysis of the entire cohort combined (n = 15) found that both NPSI and MPI-PS decreased from T2 to T3 with WBV (−6.4 ± 2.7; p = 0.08; ES = 0.50 and 0.56 ± 0.20; p = 0.01; ES = 0.69, respectively). However, analysis of the dosage groups separately found that only the 8-bout WBV group demonstrated a significant decrease in NPSI and MPI-PS scores. Although the difference between groups for change in NSPI and MPI-PS between T2 and T3 was not significant, plots show that 8-bouts of WBV appeared to be more beneficial for participants with moderate to high levels of neuropathic pain (NPSI total score >30), while 16-bouts of WBV appeared to increase pain in some individuals with moderate to severe pain symptoms (Fig. 2). During the wash-out phase between T3 and T4, the 8-bout WBV group demonstrated a slight decrease in NPSI scores while the 16-bout WBV group demonstrated a slight increase; however, these changes were not significant in either group (mean difference = −3 ± 6 and 1 ± 9; p = 0.65 and 0.88, respectively).
Effect of WBV on reflex excitability
Change values for the measures of reflex excitability across timepoints are provided in Table 3. Participants with neuropathic pain, who are the focus of this secondary analysis study, demonstrated no significant changes in FSE across timepoints. For both the 8 and 16-bout groups, PPD could be elicited consistently across all timepoints in only 5 out of 8 participants in each of the two groups. The 8-bout WBV group demonstrated an increase in PPD between T2 and T3, while the 16-bout WBV group exhibited a decrease in PPD, but the changes were not significant for either group.
Given the small observed change between T2 and T3 and knowing that the active-control used during the wash-in is itself associated with an effect on spasticity, we also analyzed the relationship between change in PPD between T1 and T3 for the entire cohort (combined treatment groups, n = 11) to assess if baseline NPSI total scores influenced response to active physical therapeutic modalities. Baseline NPSI total scores were negatively correlated with PPD change between T1 and T3 (r = −0.62; p = 0.04), indicating that higher baseline pain symptom severity was associated with less modulation of H-reflex excitability in response to WBV. Baseline NPSI total scores successfully classified non-responders (PPD change ≤0) and responders (PPD change >0) with an area under the curve of 0.92, p = 0.02 (CI = 0.74–1.0). A baseline NPSI cut score of 30 predicted PPD response with sensitivity = 1.0 and specificity = 0.83, and it correctly classified all 5 (100%) non-responders and 5/6 (83%) of the responders. This analysis was repeated for the pendulum test using changes between T1 and T3 in FSE. However, baseline NPSI total scores were not significantly associated with change in FSE from T1 to T3.
Discussion
In this study, we examined pain and reflex excitability responses to two different doses of WBV in people with chronic neuropathic pain following SCI. In addition, we examined the relationship between baseline NPSI scores and change in reflex excitability after WBV. We found that lower dose WBV (8-bouts of 45 s) was associated with greater improvement in pain symptom severity than higher dose WBV (16-bouts of 45 s). The 8-bout WBV group demonstrated a significant decrease in MPI-PS and NPSI scores, while the 16-bout WBV group did not. Interestingly, baseline NPSI scores were predictive of PPD response to WBV. Although exploratory, these novel findings may shed light on potential relationships between pain symptomology and physiologic responses to WBV that may help to better tailor WBV interventions to individual patients.
We anticipated that a higher dose of WBV would have greater therapeutic effect on pain; however, the results were inverse to what we expected. The 8-bout group had greater decrease in pain compared to the 16-bout group, although the difference did not reach statistical significance. This was true during the wash-in phase (T1–T2) and during the intervention phase (T2–T3). The fact that the difference was observed in the wash-in phase suggests that the activity of standing up and sitting down repeatedly influenced pain, a finding that has also been noted for spasticity [29]. The different group responses appear to be driven by participants who experienced moderate to high paroxysmal and/or evoked pain (subscale scores >3), as 8-bouts of repeated sitting-to-standing (T1–T2) or WBV (T2–T3) was consistently beneficial for individuals who had moderate to high paroxysmal (4/4 participants) or evoked symptoms at T2 (2/2 participants), while 16-bouts caused exacerbation or had no effects for most (2/3 participants for paroxysmal symptoms and 3/4 for evoked symptoms) (Fig. 2D, E).
The present study suggests that prolonged intense afferent input (as in the 16-bout group) may have exacerbated neuropathic pain for some participants. In clinical experience, this is a common phenomenon noted for many active interventions for neuropathic pain (e.g. aerobic and strengthening exercises). Because participants with moderate to high paroxysmal and/or evoked pain exhibited the best responses to the 8-bout intervention, it is possible that specific neuropathic pain phenotypes are associated with different treatment responses similar to what has been observed in pharmacological studies [30]. Evoked pain after SCI may to some degree represent a different pain mechanism [31] and one that is less associated with the overall perception and appraisal of neuropathic pain severity by the participant. Moreover, the relationship between physical activity and evoked pain is poorly understood, and this lack of understanding is a noted barrier for both researchers and healthcare professionals in assessing and managing neuropathic pain [32]. These findings highlight the importance of assessing specific pain symptoms [19], as well as the need for additional studies on dose response to active interventions and pain symptom exacerbation.
The identification of an NSPI total score cutoff for predicting PPD response to WBV is a novel finding and potentially useful for clinical applications. PPD may be a particularly useful measure for improving understanding of pain in the SCI population, since PPD has also proven to be a valuable physiologic measure of spasticity [33], and spasticity and neuropathic pain are closely related in this population [3]. Our findings suggest that greater severity of neuropathic pain symptoms may adversely affect responsiveness of reflex modulation to WBV. Thus, using severity of neuropathic pain symptoms as inclusion/exclusion criteria for WBV may improve matching of patients to interventions to achieve improved outcomes. However, this is speculative and future studies are needed to determine if using NPSI cutoff scores to match people with chronic pain after SCI to specific interventions improves clinical care.
Further investigation of WBV intervention for chronic neuropathic pain in people with SCI is warranted, as many people with SCI prefer non-pharmacological interventions to manage their neuropathic pain [34]. WBV provides an effective form of afferent stimulation that can activate a variety of mechanoreceptors, and central pain inhibitory control systems [35]. WBV can be combined with other pain management strategies, and it has been found to relieve pain in heterogenous pain populations. For example, in elderly persons with osteoarthritis, WBV in combination with exercise reduced pain ratings and inflammatory biomarkers compared to a control group [36]. Moreover, in women with fibromyalgia the combination of WBV and exercise was more effective in reducing pain than exercise alone [37]. Epidural stimulation (i.e., dorsal column stimulators) have long been used for the management of intractable pain, with effects that are likely mediated by activation of the dorsal nerve roots which transmit afferent information to the spinal circuits [38]. As a robust form of afferent input, WBV provides an intriguing possibility for non-invasive and non-pharmacological pain management in people with chronic neuropathic pain after SCI.
Limitations
Findings from this study should be interpreted with caution due to several limitations. This exploratory study was a subcomponent of a larger study on WBV and spasticity, and the larger study was powered based on study sample characteristics related to spasticity rather than pain. Thus, these findings need to be replicated in larger samples of persons with neuropathic pain after SCI before drawing firm conclusions. Moreover, there were differences between the groups in terms of pain medication use, with more than twice as many participants in the 8-bout group taking opioid medications. It is possible that there is a synergistic effect between opioids and mechanoreceptor activation that accounts for the greater change in NPSI. Finally, the action of standing/sitting in each trial of WBV is known to have an influence on spasticity and reflex modulation [29]. During the wash-in control period, the action of sitting/standing also appears to have influenced the pain intensity ratings in the 8-bout WBV group but not in the 16-bout WBV group. Future studies are warranted to assess the influence of WBV on neuropathic pain, and they should be adequately powered on characteristics related to neuropathic pain. The effect sizes described in our results may be used to inform power analyses for determining sample size of future studies in the area.
Conclusions
WBV is a potentially promising non-pharmacological intervention for chronic neuropathic pain after SCI, as WBV in moderate doses appears to decrease neuropathic pain symptom severity and improve reflex modulation. However, higher doses of WBV may aggravate symptoms in some individuals. Moreover, the baseline neuropathic pain symptom severity appeared to predict the reflex modulation in response to WBV which suggests that more moderate levels of WBV should be applied to those who experience severe neuropathic pain after their SCI. Although novel and potentially important, these findings are preliminary and need to be replicated in larger studies.
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).
References
Skoog B, Jakobsson KE. Prevalence of spasticity and below-level neuropathic pain related to spinal cord injury level and damage to the lower spinal segments. J Rehabil Med Clin Commun. 2020;3:1000039.
Andresen SR, Biering-Sørensen F, Hagen EM, Nielsen JF, Bach FW, Finnerup NB, et al. Pain, spasticity and quality of life in individuals with traumatic spinal cord injury in Denmark. Spinal Cord. 2016;54:973–9.
Tibbett JA, Field-Fote EC, Thomas CK, Widerstrom-Noga EG. Spasticity and pain after spinal cord injury: impact on daily life and the influence of psychological factors. PM R 2020;12:119–29.
Taricco M, Pagliacci MC, Telaro E, Adone R. Pharmacological interventions for spasticity following spinal cord injury: results of a Cochrane systematic review. Eur Medicophysica. 2006;42:5–15.
Attal N, Mazaltarine G, Perrouin-Verbe B, Albert T. Medicine SFSfP, rehabilitation. Chronic neuropathic pain management in spinal cord injury patients. What is the efficacy of pharmacological treatments with a general mode of administration? (oral, transdermal, intravenous). Ann Phys Rehabil Med. 2009;52:124–41.
Nardone R, Holler Y, Thomschewski A, Holler P, Lochner P, Golaszewski S, et al. Serotonergic transmission after spinal cord injury. J Neural Transm. 2015;122:279–95.
Biurrun Manresa JA, Finnerup NSB, Johannesen IL, Biering-Sørensen F, Jensen TS, Arendt-Nielsen L, et al. Central sensitization in spinal cord injured humans assessed by reflex receptive fields. Clin Neurophysiol. 2014;125:352–62.
Boulenguez P, Liabeuf S, Bos R, Bras H, Jean-Xavier C, Brocard C, et al. Down-regulation of the potassium-chloride cotransporter KCC2 contributes to spasticity after spinal cord injury. Nat Med. 2010;16:302–7.
Kahle KT, Khanna A, Clapham DE, Woolf CJ. Therapeutic restoration of spinal inhibition via druggable enhancement of potassium-chloride cotransporter KCC2–mediated chloride extrusion in peripheral neuropathic pain. JAMA Neurol. 2014;71:640.
Gruber M, Taube W, Gollhofer A, Beck S, Amtage F, Schubert M. Training-specific adaptations of H- and stretch reflexes in human soleus muscle. J Mot Behav. 2007;39:68–78.
Morita H, Crone C, Christenhuis D, Petersen NT, Nielsen JB. Modulation of presynaptic inhibition and disynaptic reciprocal Ia inhibition during voluntary movement in spasticity. Brain. 2001;124:826–37.
Gibson W, Wand BM, O’Connell NE. Transcutaneous electrical nerve stimulation (TENS) for neuropathic pain in adults. Cochrane Database Syst Rev. 2017;9:CD011976.
Karacan I, Cidem M, Cidem M, Turker KS. Whole-body vibration induces distinct reflex patterns in human soleus muscle. J Electromyogr Kinesiol. 2017;34:93–101.
Estes S, Iddings JA, Ray S, Kirk-Sanchez NJ, Field-Fote EC. Comparison of single-session dose response effects of whole body vibration on spasticity and walking speed in persons with spinal cord injury. Neurotherapeutics. 2018;15:684–96.
Ness LL, Field-Fote EC. Effect of whole-body vibration on quadriceps spasticity in individuals with spastic hypertonia due to spinal cord injury. Restor Neurol Neurosci. 2009;27:621–31.
Mingorance JA, Montoya P, Vivas Miranda JG, Riquelme I. A comparison of the effect of two types of whole body vibration platforms on fibromyalgia. A randomized controlled trial. Int J Environ Res Public Health. 2021;18:1–14.
Sonza A, Sanada LS, Oliveira LR, Bernardo-Filho M, Sa-Caputo DDC, Zaro MA, et al. Whole-body vibration mediates mechanical hypersensitivity through Abeta-fiber and C-fiber thermal sensation in a chronic pain model. Exp Biol Med. 2021;10:1210–8.
Bouhassira D, Attal N, Fermanian J, Alchaar H, Gautron M, Masquelier E, et al. Development and validation of the Neuropathic Pain Symptom Inventory. Pain. 2004;108:248–57.
Wong ML, Fleming L, Robayo LE, Widerstrom-Noga E. Utility of the neuropathic pain symptom inventory in people with spinal cord injury. Spinal Cord. 2020;58:35–42.
Widerstrom-Noga E, Biering-Sorensen F, Bryce TN, Cardenas DD, Finnerup NB, Jensen MP, et al. The International Spinal Cord Injury Pain Basic Data Set (version 2.0). Spinal Cord. 2014;52:282–6.
Widerstrom-Noga EG, Cruz-Almeida Y, Martinez-Arizala A, Turk DC. Internal consistency, stability, and validity of the spinal cord injury version of the multidimensional pain inventory. Arch Phys Med Rehabil. 2006;87:516–23.
Ness LL, Field-Fote EC. Effect of whole-body vibration on quadriceps spasticity in individuals with spastic hypertonia due to spinal cord injury. Restor Neurol Neurosci. 2009;27:621–31.
Fowler EG, Nwigwe AI, Ho TW. Sensitivity of the pendulum test for assessing spasticity in persons with cerebral palsy. Devl Med Child Neurol. 2000;42:182–9.
Field-Fote EC, Brown KM, Lindley SD. Influence of posture and stimulus parameters on post-activation depression of the soleus H-reflex in individuals with chronic spinal cord injury. Neurosci Lett. 2006;410:37–41.
Lee-Kubli CA, Zhou X, Jolivalt CG, Calcutt NA. Pharmacological modulation of rate-dependent depression of the spinal H-reflex predicts therapeutic efficacy against painful diabetic neuropathy. Diagnostics. 2021;11:1–14.
Moore CG, Carter RE, Nietert PJ, Stewart PW. Recommendations for planning pilot studies in clinical and translational research. Clin Transl Sci. 2011;4:332–7.
Field-Fote EC, Fluet GG, Schafer SD, Schneider EM, Smith R, Downey PA, et al. The spinal cord injury functional ambulation inventory (SCI-FAI). J Rehabil Med. 2001;33:177–81.
Ottenbacher KJ. Why rehabilitation research does not work (as well as we think it should). Arch Phys Med Rehabil. 1995;76:123–9.
Estes S, Iddings JA, Ray S, Kirk-Sanchez NJ, Field-Fote EC. Comparison of single-session dose response effects of whole body vibration on spasticity and walking speed in persons with spinal cord injury. Neurotherapeutics. 2018;15:684–96.
Widerstrom-Noga E. Neuropathic pain and spinal cord injury: phenotypes and pharmacological management. Drugs. 2017;77:967–84.
Finnerup NB, Kuner R, Jensen TS. Neuropathic pain: from mechanisms to treatment. Physiol Rev. 2021;101:259–301.
Corbett DB, Simon CB, Manini TM, George SZ, Riley JL 3rd, Fillingim RB. Movement-evoked pain: transforming the way we understand and measure pain. Pain. 2019;160:757–61.
Bilchak JN, Yeakle K, Caron G, Malloy D, Cote MP. Enhancing KCC2 activity decreases hyperreflexia and spasticity after chronic spinal cord injury. Exp Neurol. 2021;338:113605.
Widerstrom-Noga E, Anderson KD, Perez S, Martinez-Arizala A, Calle-Coule L, Fleming L. Barriers and facilitators to optimal neuropathic pain management: SCI consumer, significant other, and health care provider perspectives. Pain Med. 2020;21:2913–24.
Lin T, Gargya A, Singh H, Sivanesan E, Gulati A. Mechanism of peripheral nerve stimulation in chronic pain. Pain Med. 2020;21(Suppl 1):S6–12.
Simao AP, Avelar NC, Tossige-Gomes R, Neves CD, Mendonca VA, Miranda AS, et al. Functional performance and inflammatory cytokines after squat exercises and whole-body vibration in elderly individuals with knee osteoarthritis. Arch Phys Med Rehabil. 2012;93:1692–700.
Alentorn-Geli E, Padilla J, Moras G, Lazaro Haro C, Fernandez-Sola J. Six weeks of whole-body vibration exercise improves pain and fatigue in women with fibromyalgia. J Alter Complement Med. 2008;14:975–81.
Danner SM, Hofstoetter US, Ladenbauer J, Rattay F, Minassian K. Can the Human Lumbar Posterior Columns Be Stimulated by Transcutaneous Spinal Cord Stimulation? A Modeling Study. Artificial Organs 2011;35:257–62.
Funding
This study was supported by the NIH, National Institute of Child Health and Human Development (Grant ID: R01 HD079009, Trial registration NCT02340910, EFF).
Author information
Authors and Affiliations
Contributions
MLW was responsible for data analysis and writing the report. EWN was responsible for protocol design, data analysis, and writing the report. As the senior author, EFF was responsible for designing the protocol, conducting the research, extracting the data, and writing the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wong, M.L., Widerstrom-Noga, E. & Field-Fote, E.C. Effects of whole-body vibration on neuropathic pain and the relationship between pain and spasticity in persons with spinal cord injury. Spinal Cord 60, 963–970 (2022). https://doi.org/10.1038/s41393-022-00806-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00806-w
- Springer Nature Limited
This article is cited by
-
A novel theta-controlled vibrotactile brain–computer interface to treat chronic pain: a pilot study
Scientific Reports (2024)