Abstract
Purpose
Metastasis-free survival (MFS) is a surrogate for overall survival (OS) in men with non-metastatic castration-resistant prostate cancer (CRPC), but this endpoint may take years to develop in men with non-metastatic castrate-sensitive disease. The study objective was to examine whether progression to CRPC is a potential intermediate endpoint for developing metastatic disease in patients with biochemical recurrence (BCR) after radical prostatectomy (RP).
Materials and methods
Men with BCR following RP who had PSA doubling times (PSADT) < 9 months and no metastasis at the time of initiating androgen deprivation therapy (ADT) (n = 210) were included. The primary objective was to assess the correlation between CRPC-free survival (CRPC-FS) and MFS, and the secondary objective was to assess the correlation between time to metastasis and time to CRPC. Kendall’s Tau was used to test the correlation for the primary and secondary outcomes.
Results
The median MFS was 104 months (95% CI: 83–114) and median CRPC-FS was 100 months (95% CI: 80–114). Based on the Kaplan–Meier curve, the greatest difference in time to MFS and CRPC-FS was around 70% free survival, which was reached at 61.2 months for MFS and 49.6 months for CRPC-FS. Kendall’s Tau for the correlation between CRPC-FS and MFS and between time to CRPC and time to metastasis was 0.867 (95% CI: 0.765–0.968) and 0.764 (95% CI: 0.644–0.884), respectively.
Conclusions
Given the high correlation between CRPC-FS and MFS, after validation, CRPC-FS may serve as a potential intermediate endpoint in trials for men with BCR initiating ADT following local therapy.
Similar content being viewed by others
Introduction
Due to recent developments in the treatment of advanced prostate cancer, men may live for several years following the diagnosis of metastatic castration-resistant prostate cancer (CRPC) [1]. As a result, though overall survival (OS) remains the most robust endpoint for clinical trial design, these data may take years to mature, especially in men with non-metastatic hormone-sensitive disease. Appropriate evidence-based intermediate endpoints are necessary for clinical trial design and expediting the evaluation of new therapies [2,3,4].
The ICECaP Working Group demonstrated that among 19 predominantly radiotherapy-based trials, metastasis-free survival (MFS) is a strong surrogate of OS among men with localized prostate cancer [2]. Using this outcome, three novel anti-androgen inhibitors (enzalutamide, apalutamide, and darolutamide) have gained FDA approval in the non-metastatic CRPC disease space given their benefits in delaying MFS [5,6,7]. However, in the active treatment arm of these trials, median MFS was long, ranging from 36.6–40.5 months. More recently, Gharzai and colleagues assessed aggregative trial-level performance of commonly reported intermediate clinical endpoints (biochemical failure, local failure, distant metastases, biochemical failure-free survival, progression-free survival (PFS), and MFS) among 75 trials across all randomized trials in localized prostate cancer [4]. Although endpoints early in the disease process correlated poorly with OS, PFS (R2 0.46) showed moderate correlation and MFS (R2 0.78) showed strong correlation with OS.
In patients with recurrent disease following local therapy, androgen deprivation therapy (ADT) is typically given prior to metastasis. As such, many men will develop CRPC prior to metastasis. Time to CRPC may take years, followed by the addition of novel antiandrogen agents further delaying metastasis [5,6,7], thus making trial design in this disease space difficult. We therefore hypothesized that CRPC-free survival (CRPC-FS) while on ADT may also be a reasonable intermediate endpoint for MFS among men previously treated with radical prostatectomy (RP) who are initiating ADT for biochemical recurrence (BCR).
Materials and methods
Study population
After receiving institutional review board approval, data from patients undergoing RP at eight Veteran Affairs Medical Centers (West Los Angeles, San Diego, San Francisco, Palo Alto, CA; Augusta, GA; Durham and Asheville, NC; and Portland, OR) between 1988–2017 were combined into the Shared Equal Access Regional Cancer Hospital (SEARCH) database [8]. Among 7811 men undergoing RP, 2689 experienced BCR (Fig. 1). We excluded men with missing data on PSA doubling time (PSADT; n = 1208), those with PSADT ≥ 9 months (n = 1095), those who did not receive ADT (n = 128), and those who had metastases at initiation of ADT (n = 48), resulting in a study population of 210 men. A comparison between men that had PSADT data versus those men excluded for missing PSADT data demonstrated several differences between these cohorts (Supplementary Table 1). PSADT < 9 months was chosen to a select cohort at high-risk of metastasis [8,9,10]. Taken together, men with BCR following RP who had PSA doubling time (PSADT) < 9 months and no metastasis at the time of initiating ADT (n = 210) were included.
Objectives and covariates
The primary objective was to assess the correlation between CRPC-FS and MFS. The secondary objective was to assess the correlation between time to CRPC and time to metastasis. An exploratory objective was to assess the correlation between CRPC-FS and overall survival (OS). MFS, CRPC-FS and OS were defined as time from initiation of ADT to metastasis or any cause of death, CRPC or any cause of death, and any cause of death, respectively. CRPC was defined using the Prostate Cancer Clinical Trials Working Group 2 definition [11]. Covariates included age at ADT (continuous), year of ADT (continuous), race (non-black, black), surgical center (categorical), clinical stage (T1, T2-T4), pathologic grade group (1, 2, 3, 4, 5), positive surgical margins (no, yes), extracapsular extension (ECE; no, yes), seminal vesicle invasion (SVI; no, yes), lymph node involvement (no, yes, not assessed), and PSA at ADT initiation (continuous, log-transformed).
Statistical analysis
Multivariable Cox proportional hazards models, adjusted for variables a priori, were fit to examine which clinical characteristics were associated with time to CRPC, time to metastasis, and time to death. Kendall’s Tau was used to test the correlation between CRPC-FS and MFS, between time to CRPC and time to metastasis [12]. Kaplan-Meier curves were created for each outcome. Kendall’s Tau was also used to test the correlation between CRPC-FS and OS. The Kendall’s Tau was calculated using the formula by Weier et al. [13] or Kim et al. [14], which is similar to the Pearson’s correlation between two variables, using the Kaplan–Meier estimates to address censoring. Moreover, this Kendall’s Tau estimate is purely non-parametric and the copula model is not assumed. To identify men most likely to develop metastasis and not die of other causes who would be subjects of future clinical trials (thus benefiting the most from an intermediate endpoint), we performed a subgroup analysis for patients with PSA at ADT initiation >1 ng/ml and patients with Charlson-Deyo Comorbidity Index (CCI) ≤ 2. Additionally, we performed a subgroup analysis excluding men that developed mCSPC.
Results
In this cohort of 210 men, the median age at ADT was 67 years (IQR 62, 72), most men were non-black (71%), the most common pathologic grade group was 2–3 (54%), 46% had positive margins, 30% had SVI, 44% had ECE, and 8% had N + disease (Table 1). The median pre-ADT PSA was 3.8 ng/mL (IQR 1.2, 8.1), and median follow-up after ADT was 79.4 months (IQR 38.1, 127.7; MFS: 132 events, CRPC-FS: 131 events).
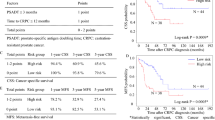
The median MFS was 104 months (95% CI: 83–114) and median CRPC-FS was 100 months (95% CI: 80–114) (Fig. 2). Based on the Kaplan–Meier curve of all men, the greatest difference in time to MFS and CRPC-FS was around 70% event-free survival, which was reached at 61.2 months for MFS and 49.6 months for CRPC-FS. Kendall’s Tau for the correlation between CRPC-FS and MFS was 0.867 (95% CI: 0.765–0.968), with comparable correlation when limited to men with PSA at ADT > 1 ng/mL (0.846; 95% CI: 0.726–0.966) and CCI ≤ 2 (0.875; 95% CI 0.728–1.000) (Table 2a). Similarly, Kendall’s Tau for the correlation between time to CRPC and time to metastasis was 0.764 (95% CI 0.644–0.884), with comparable correlation when limited to men with PSA at ADT > 1 ng/mL (0.763; 95% CI: 0.624–0.902) and CCI ≤ 2 (0.739; 95% CI: 0.568–0.910). The overall similar time to events occurred because some men were treated with intermittent ADT and thus developed castrate-sensitive metastases prior to developing CRPC (n = 7). While this reflects real-world practice patterns, in a clinical trial design wherein ADT is intermittent but then reinitiated at a modest PSA level and thus prior to metastases, development of castrate-sensitive metastases would be unlikely. To model this, we repeated the analyses excluding these seven men and found that Kendall’s Tau for the correlation between CRPC-FS and MFS was 0.888 (95% CI: 0.783–0.993), with comparable correlation when limited to men with PSA at ADT > 1 ng/mL (0.862; 95% CI: 0.741–0.983) and CCI ≤ 2 (0.906; 95% CI: 0.755–1.057) (Table 2b). In an exploratory analysis, similar results were found for the Kendall’s Tau correlation between CRPC-FS and OS (Supplementary Table 2).
The predictors of time from ADT to CRPC-FS and MFS were similar with N + disease and higher PSA at ADT associated with worse outcomes with similar hazard ratios for both outcomes (all p ≤ 0.003; Table 3). While black race predicted lower risk of CRPC-FS (HR 0.56, 95% CI: 0.33–0.96) and MFS (HR 0.63, 95% CI: 0.37–1.08) compared to white race with similar hazards, the association with MFS was not statistically significant. Similar results were also found when assessing predictors of time from ADT to OS (Supplementary Table 3).
Discussion
In a cohort of high-risk men without metastasis at the time of initiating ADT after RP, we found a strong correlation between CRPC-FS and MFS, in addition to time to CRPC and time to metastasis. Specifically, the greatest difference in time to MFS and CRPC-FS was 61.2 months for MFS and 49.6 months for CRPC-FS at an event free survival of 70%, suggesting a 12-month earlier time to event for CRPC. These results were also robust in subsets of men with PSA at ADT > 1 ng/mL and CCI ≤ 2, men that are most likely to develop metastasis and not die of other causes, and who would be most likely subjects of future clinical trials. Furthermore, predictors of time from ADT to CRPC-FS and MFS were similar (including in a subset analysis excluding patients that developed mCSPC), supporting the similarity between these two end-points providing further evidence that if confirmed, CRPC-FS may be a reasonable intermediate end-point for men with BCR after RP initiating ADT.
Intermediate clinical endpoints have emerged with great interest over the last several years. These surrogate endpoints are necessary for clinical trial design and expediting the evaluation of new therapies given that these data may take years to mature to the ultimate endpoint of OS. MFS has emerged as a viable intermediate clinical endpoint for OS, first based on work from the ICECaP group in radiotherapy trials [2] and more recently in all localized prostate cancer clinical trials [4]. MFS as an endpoint was used to approve apalutamide [6], enzalutamide [5], and darolutamide [7] in the non-metastatic CRPC disease space, based on a significant MFS benefit for these agents compared to standard of care. The legitimacy of intermediate clinical endpoints, specifically MFS, was further justified when all three non-metastatic CRPC trials published data in 2020 demonstrating an OS benefit for the intervention group with longer follow-up [15,16,17].
The results of our study have several implications and should be taken into context with the existing literature. Since time to CRPC correlates with time to metastasis, aggressive, upfront therapy among men with high-risk localized disease in order to delay CRPC should also delay metastasis. Historically, adjuvant systemic therapy trials for high-risk patients after RP have had difficulty accruing patients. For example, in TAX-3501, the primary outcome was PFS for high-risk men with undetectable PSA after RP who were treated with immediate versus deferred ADT + /− docetaxel [18]. This trial was terminated early, secondary to enrollment challenges, which were attributed to lack of consensus regarding patient selection, need for long follow-up, and non-validated intermediate endpoints (i.e., PFS).
Our results also suggest CRPC-FS may be a valuable intermediate endpoint for future clinical trials. Several on-going phase III trials are testing novel hormonal agents in earlier stage non-metastatic prostate cancer with an MFS primary outcome (EMBARK [NCT02319837], ATLAS [NCT02531516], PROTEUS [NCT03767244]). If our results are validated, in the future it may be possible for studies to use CRPC-FS as a primary outcome rather than MFS, potentially saving ~12 months (or more) of follow-up waiting for MFS events to mature. Changing imaging tests, such as next generation imaging studies such as PSMA, make for a moving target in the definition of metastasis as well as challenges for global studies with variable use of next generation imaging around the world. In contrast, CRPC is a simple and robust definition without confusion [19]. This would dramatically expedite drug development and not only encourage more trials in this disease space, but ensure that patients have more rapid access to novel agents with significant clinical benefit.
There are several limitations of the current study. First, we did not have a validation dataset to enable testing the correlations from this study in a similar population of patients with hormone sensitive prostate cancer. Second, there was a relatively small sample size, however the event rate in our study is >60% and follow-up is >6 years, thus providing a significant event rate to allow meaningful analyses. Third, all of the men in this study underwent RP and thus the results may not be generalizable to all men without metastasis initiating ADT, for example after radiotherapy or other local therapies. Fourth, even if CRPC-FS is validated as an intermediate end-point for time to metastasis, this end-point may be limited by the small difference between CRPC-FS and MFS, and the more limited association of time to metastasis and time to CRPC. Fifth, there were 1208 men with BCR that were excluded from the study secondary to missing data for PSADT (Supplementary Table 1), which may have led to a potential bias in patient selection. Finally, we did not formally test for surrogacy between the outcomes. Thus, our findings are purely correlative and ideally should be assessed for surrogacy in a controlled dataset with OS as the primary outcome.
Conclusions
Among men with BCR after RP and PSADT < 9 months at high-risk of metastases, but no metastasis prior to initiating ADT, we found that CRPC-FS and MFS were highly correlated. Intermediate clinical endpoints are of interest considering that an OS endpoint may take years to develop in men with non-metastatic castrate-sensitive disease. If validated, these results may have important clinical trial ramifications, including CRPC-FS as a relevant intermediate endpoint for early stage clinical trials, potentially saving up to ~12 months (or more) of follow-up time.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Moreira DM, Howard LE, Sourbeer KN, Amarasekara HS, Chow LC, Cockrell DC, et al. Predicting time from metastasis to overall survival in castration-resistant prostate cancer: results from SEARCH. Clin Genitourin Cancer. 2017;15:60–66.
Xie W, Regan MM, Buyse M, Halabi S, Kantoff PW, Sartor O, et al. Metastasis-free survival is a strong surrogate of overall survival in localized prostate cancer. J Clin Oncol. 2017;35:3097–104.
Xie W, Regan MM, Buyse M, Halabi, Kantoff PW, Sartor O, et al. Event-free survival, a prostate-specific antigen-based composite end point, is not a surrogate for overall survival in men with localized prostate cancer treated with radiation. J Clin Oncol. 2020;38:3032–41.
Gharzai LA, Jiang R, Wallington D, Jones G, Birer S, Jairath N, et al. Intermediate clinical endpoints for surrogacy in localised prostate cancer: an aggregate meta-analysis. Lancet Oncol. 2021;22:402–10.
Hussain M, Fizazi K, Saad F, Rathenborg P, Shore N, Ferreira U, et al. Enzalutamide in men with nonmetastatic, castration-resistant prostate cancer. N. Engl J Med. 2018;378:2465–74.
Smith MR, Saad F, Chowdhury S, Oudard S, Hadaschik BA, Graff JN, et al. Apalutamide treatment and metastasis-free survival in prostate cancer. N. Engl J Med. 2018;378:1408–18.
Fizazi K, Shore N, Tammela TL, Ulys A, Vjaters E, Polyakov S, et al. Darolutamide in nonmetastatic, castration-resistant prostate cancer. N Engl J Med. 2019;380:1235–46.
Whitney CA, Howard LE, Freedland SJ, De Hoedt AM, Amling CL, Aronson WJ, et al. Impact of age, comorbidity, and PSA doubling time on long-term competing risks for mortality among men with non-metastatic castration-resistant prostate cancer. Prostate Cancer Prostatic Dis. 2019;22:252–60.
Freedland SJ, Humphreys EB, Mangold LA, Eisenberger M, Dorey FJ, Walsh PC, et al. Risk of prostate cancer-specific mortality following biochemical recurrence after radical prostatectomy. JAMA. 2005;294:433–9.
Freedland SJ, Humphreys EB, Mangold LA, Eisenberger M, Dorey FJ, Walsh PC, et al. Death in patients with recurrent prostate cancer after radical prostatectomy: prostate-specific antigen doubling time subgroups and their associated contributions to all-cause mortality. J Clin Oncol. 2007;25:1765–71.
Scher HI, Halabi S, Tannock I, Morris M, Sternberg CN, Carducci MA, et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol. 2008;26:1148–59.
Akoglu H. User’s guide to correlation coefficients. Turk J Emerg Med. 2018;18:91–93.
Weier DR, Basu AP. An investigation of Kendall’s tau modified for censered data with applications. J Stat Plan Inference. 1980;4:381–90.
Kim Y, Lim J, Park D. Testing independence of bivariate interval-censored data using modified Kendall’s tau statistic. Biometrical J. 2015;57:1131–45.
Smith MR, Saad F, Chowdhury S, Oudard S, Hadaschik BA, Graff JN, et al. Apalutamide and overall survival in prostate cancer. Eur Urol. 2021;79:150–8.
Sternberg CN, Fizazi K, Saad F, Shore ND, De Giorgi U, Penson DF, et al. Enzalutamide and survival in nonmetastatic, castration-resistant prostate cancer. N. Engl J Med. 2020;382:2197–206.
Fizazi K, Shore N, Tammela TL, Ulys A, Fjaters E, Polyakov S, et al. Nonmetastatic, castration-resistant prostate cancer and survival with darolutamide. N. Engl J Med. 2020;383:1040–9.
Schweizer MT, Huang P, Kattan MW, Kibel AS, de Wit R, Sternberg CN, et al. Adjuvant leuprolide with or without docetaxel in patients with high-risk prostate cancer after radical prostatectomy (TAX-3501): important lessons for future trials. Cancer. 2013;119:3610–8.
Hofman MS, Lawrentschuk N, Francis RJ, Tang C, Vela I, Thomas P, et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multi-centre study. Lancet. 2020;395:1208–16.
Funding
This work was supported by funding from Pfizer. Furthermore, additional support included NIH R01CA231219 (WJA), and the Georgia Cancer Coalition (MKT). Views and opinions of, and endorsements by the author(s), do not reflect those of the US Army or the Dept. of Defense.
Author information
Authors and Affiliations
Contributions
ZK: study concept and design, acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, technical or material support. LEH: acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis. CJDW: analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content. JL: acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis. AH: study concept and design, acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, technical or material support. WA: acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, technical or material support. TJP: acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, technical or material support. CA: acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, technical or material support. CK: acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, technical or material support. MC: acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, technical or material support. MT: acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, technical or material support. YW: acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis. SF: study concept and design, acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, technical or material support.
Corresponding author
Ethics declarations
Competing interests
ZK: Pfizer/Astellas, Bayer; SJF: Pfizer, Astellas, Janssen, Bayer, Astra Zeneca, Merck, Myovant, Clovis, Sanofi, Exact Sciences, Decipher Biosciences, Tempus, Exosome, Boston Scientific. The rest of the authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Klaassen, Z., Howard, L., Wallis, C.J.D. et al. Is time to castration resistant prostate cancer a potential intermediate end-point for time to metastasis among men initiating androgen deprivation therapy for non-metastatic prostate cancer with rapid PSA doubling time (<9 months)?. Prostate Cancer Prostatic Dis 26, 151–155 (2023). https://doi.org/10.1038/s41391-022-00585-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00585-8
- Springer Nature Limited
This article is cited by
-
Predictive significance of inflammatory markers and mGPS in metastatic castration-resistant prostate cancer treated with abiraterone or enzalutamide
Cancer Chemotherapy and Pharmacology (2024)