Abstract
Purpose
To assess the prevalence of sarcopenia and whether body composition parameters are associated with disease progression and overall survival (OS) in castration-resistant prostate cancer (CRPC) patients.
Materials and methods
This single-centre retrospective study evaluated data of 186 consecutive patients who underwent chemohormonal therapy between 2005 and 2016 as first-line systemic treatment for CRPC. Skeletal muscle and fat indices were determined using computerized tomography data before initiation of chemotherapy. Sarcopenia was defined as SMI of <55 cm2/m2. Visceral-to-subcutaneous fat ratio and skeletal muscle volume were calculated with body composition specific areas. Harrell’s concordance index was used for predictive accuracy.
Results
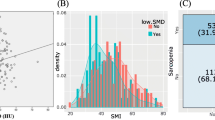
A total of 154 (82.8%) patients met the criteria for sarcopenia; 139 (74.7%) individuals completed at least six cycles of docetaxel. Within a median follow-up of 24.1 months, age (HR 1.03, 95% CI 1.01–1.06, p = 0.02), high PSA (1.55, 95% CI 1.07–2.25, p = 0.02) and low skeletal muscle volume (HR 1.61, 95% CI 1.10–2.35, p = 0.02) were the only independent prognostic factor for tumor progression. Overall, 93 (50%) patients died during the follow-up period. The established prognosticator, the prechemotherapy presence of liver metastases (HR 1.32, 95% CI 1.08–1.61, p < 0.01) was associated with shorter OS. Moreover, we noted that patients with an elevated visceral-to-subcutaneous fat ratio tended to have a shorter OS (p = 0.06).
Conclusion
The large majority of men with CRPC suffers from sarcopenia. In our cohort, low skeletal muscle volume was an independent adverse prognosticator for progression of disease. We could not detect a statistically significant body composition parameter for OS, although patients with a high proportion of visceral fat had a trend for shorter OS. However, we suggest that body composition parameters determined by CT data can provide useful objective prognostic factors that may support tailored treatment decision-making.
Similar content being viewed by others
Introduction
Prostate cancer accounts for 19% of the cancers diagnosed in men and therefore represents the most common solid male neoplasm [1]. Ten percent of men diagnosed with PCa eventually develop metastatic disease; with a 5-year overall survival (OS) of 30% [2]. Androgen deprivation therapy (ADT), the standard therapy for some patients with locally advanced and all patients with metastatic disease, [3] alters the body composition of patients such as a significant loss in skeletal muscle mass (SMM) and an increase in subcutaneous adipose tissue (SAT) [4,5,6]. Despite initial favorable oncologic response to ADT, eventually irreversible resistance to ADT will develop in almost all the patients with a median response duration of 2 years, resulting in castration-resistance prostate cancer (CRPC) [7].
Docetaxel based chemotherapy is one of the standard first-line agents used for the therapy of CRPC patients, specifically in those with increasing symptoms due to progressive disease such as bone pain and general fatigue [3]. However, there are concerns regarding its toxicity, particularly in men with age- and ADT-related low SMM or sarcopenia [8]. In addition to being linked to toxicity from chemotherapy, body composition parameters have been shown to be associated with the prognosis of CRPC patients [9]. For example, studies have reported that being overweight or obese is prognostically favorable when resistance to castration arises [10, 11]. Patients with a high SAT volume have longer OS than those with a low SAT volume [12, 13]. Conversely, sarcopenia has been shown to independently predict worse survival in PCa patients [13,14,15]. Despite these early small studies, the effect of body composition parameters on survival outcomes in CRPC patients remains unclear.
The objective of the current study was to determine the prevalence of sarcopenia in CRPC patients. In addition, we aimed to assess whether muscle, visceral, and SAT are correlated with tumor progression and/or OS in CRPC patients treated with docetaxel chemotherapy. We hypothesized that muscle and fat tissue would be independently associated with oncologic outcomes in CPRC patients, thereby offering additional information for counseling and guiding patients.
Materials and methods
Study aims
The primary aim was to assess the prevalence of sarcopenia in CRPC patients. The secondary aim was to evaluate whether body composition parameters are associated with tumor progression in CRPC patients treated with docetaxel chemotherapy. The tertiary aim was to study the value of body composition parameters in prognosticating OS after docetaxel chemotherapy in CRPC patients.
Study population
After institutional review board approval (2056/2016), we reviewed data from 191 consecutive patients who underwent chemohormonal therapy between 2005 and 2015 for CRPC at our center (Fig. 1). CRPC status was defined as cancer progression despite a serum testosterone level within the castrate level (<50 ng/dL) [3]. Patients were excluded from the analyses if they had insufficient imaging data (n = 2) and if they were lost to follow-up (n = 3). A total of 186 patients were included in the final analyses. All men underwent a treatment regimen of docetaxel [75 mg/m2] every 3 weeks in combination with 10 mg of prednisolone per day. Chemohormonal treatment was continued until the patient experienced radiographic or PSA progression, intolerable side-effects or death. Due to the retrospective design of the study, follow-up was not standardized. For most patients, serum PSA was evaluated every 3 months with whole-body imaging (i.e., thoracoabdominal CT, MRI, and bone scan) after every third chemotherapy cycle based on clinicopathologic features and at physician discretion [16].
Study design depicted in organigram form. Patients’ distribution and clinical pathway. Of 191 CRPC patients identified, 186 were eligible for final analysis. All patients continued androgen deprivation throughout the studied period. One hundred and thirty-nine men completed ≥6 cycles of chemotherapy
Data collection and definitions
Patients’ characteristics at the time of PCa diagnosis and initiation of chemotherapy were retrieved from the institutional electronic medical records database. Two trained investigators measured the cross-sectional areas of subcutaneous fat, visceral fat, and skeletal muscle from CT scans in the portal venous phase before initiation of chemotherapy at the level of the 3rd lumbar vertebra [17]. Through the image processing application OsiriX (version 6.0.2; Bernex, Switzerland), the areas of interest were measured based on their specific Hounsfield units (subcutaneous fat area [SFA] −190 to −30, visceral fat area [VFA] −150 to −50, and skeletal muscle area [SMA] −29 to 150). The patients’ body composition areas were normalized to the square of the height (m2) of the patient to calculate the indices: subcutaneous fat index (SFI), visceral fat index (VFI), and skeletal muscle index (SMI). Sarcopenia was defined according to international consensus definitions of an SMI < 55 cm2/m2 for men [18]. In order to assess sarcopenic obesity, we used the Martin et al. classification of SMI < 43 cm2/m2 for males with BMI < 25 kg/m2 and <53 cm2/m2 for males with BMI ≥ 25 kg/m2 [19]. The skeletal muscle volume (SMV) was calculated with the formula for SMV = 0.166 × skeletal muscle area + 4.142, and the adipose tissue volume (ATV) with 0.068 × (visceral fat area + subcutaneous fat area) + 2.142 [20]. For group comparison, median values were used as cutoffs. From the body composition values, we calculated visceral-to-subcutaneous fat area ratio (VSR) and visceral fat-to-muscle area ratio (VMR). Progression was defined as a consecutive rise of 25% in PSA and/or progression of tumor burden and/or occurrence of new metastases in imaging studies. When osseous metastases are present, there must appear ≥2 new bone lesions, to meet the criteria for progression. Ambiguous results needed to be confirmed by other imaging modalities (e.g., CT or MRI) [21]. OS was defined as death of any reason after chemohormonal therapy initiation [22].
Statistical analysis
Categorical variables were summarized by absolute numbers and percentages, continuous variables by the median and interquartile range. Chi-squared test and Mann–Whitney U-test were used to compare categorical and continuous variables. Cox proportional hazards regression analyses reporting hazard ratios (HR) were done to assess the risk for disease progression dependent on the calculated body composition parameters. Survival analyses were conducted to investigate the association of body composition indices, ratios and volumes with outcome, respectively. Cox’s proportional hazards model was used. Therein, following continuous variables were tested: age, BMI, VMR, VSR, and LDH. The ECOG performance status, the presence of sarcopenia, distant nodal, bone or liver metastases, and high PSA, defined as PSA over the median of 38.2 ng/mL, were tested as binary variables. The SMV, SFI, and VFI, adipose tissue index and ATV were dichotomized at their median for further testing. Multivariable analysis was performed to adjust for the effect of potential confounders. The presence of liver metastases, prechemotherapy PSA level, ECOG performance status, and SMV were included in the progression model. In the survival model, the presence of liver metastases and prechemotherapy PSA level, BMI and LDH were included as well as VSR. Harrell’s concordance index (C-index) was used for predictive accuracy. To report sensitivity and specificity, a receiver operating characteristic (ROC) curve analysis was performed. All tests were two-sided and a p value < 0.05 was considered as statistically significant. We performed statistical analysis with the software STATA v14 (StataCorp, College Station, TX, USA).
Results
Baseline characteristics of the population
The clinical and pathologic features of the analyzed men at the time of first diagnosis and at the time of initiation of chemotherapy with docetaxel are shown in Table 1. Overall, 154 (82.8%) patients met the criteria for sarcopenia and 118 (63.4%) for sarcopenic obesity. Sarcopenic patients were significantly older (p = 0.007) and had a lower BMI (p = 0.01) at chemotherapy initiation. The median time from the start of ADT therapy and the administration of the first chemotherapy cycle was 33.2 months (IQR 10.9–106.1). A median of six docetaxel cycles (IQR 5–8) was administered to both sarcopenic and nonsarcopenic CRPC patients.
Treatments for CRPC
Overall, 139 (74.7%) of 186 included patients completed at least six cycles of docetaxel chemotherapy, the remaining discontinued chemotherapy due to adverse events (n = 18) or withdraw treatment consent after initiation of docetaxel (n = 26) or died during the treatment period (n = 3). Within a median follow-up of 24.1 months (IQR 12.8–40.8), 156 patients (83.9%) experienced progression of their disease (median time to progression 7.8 months [IQR 4.4–16.3]). A total of 105 (56.5%) men received further treatment after disease progression.
Association of body composition parameters with progression-free survival
In univariable Cox regression analyses (Table 2), multiple muscle parameters such as ECOG performance status, age, high PSA, low SMV, and the presence of liver metastasis were associated with disease progression. Figure 2 depicts the time difference to progression after docetaxel chemotherapy in patients with low versus high SMV using the median SMV of 28.7 kg as cutoff (p = 0.02). In the multivariable model, the prognostic impact of ECOG performance status, prechemotherapy PSA level, presence of liver metastases was assessed. By including the variable low SMV, the accuracy for predicting association of body composition parameters with progression rose from a C-index of 0.628–0.638 (Table 3). The area under the ROC curve for the progression model was 71.2% (Supplementary Fig. 1).
Association of body composition parameters with OS
Overall 93 (50%) patients died during follow-up whereby median OS was 26.2 months (IQR 13.7–42.4). On univariable analyses, VSR, LDH, BMI, and presence of liver metastases were associated with shorter OS. Figure 1 shows Kaplan–Meier analyses stratifying the patients according to the median SMV of 28.7 kg. The median SMV did not differentiate the docetaxel treated CRPC patients regarding OS (p = 0.26). In multivariable analysis, which contained the presence of liver metastases, prechemotherapy BMI, LDH, and VSR; a high VSR (p = 0.06) showed a prognostic tendency for OS and the presence of liver metastases (p < 0.01) was associated with shorter OS (Table 3). The C-Index after including the high VSR variable in the multivariable model, the accuracy for predicting association of body composition parameters with OS was 0.633 with an area under the ROC curve of 58.7% (Supplementary fig. 1).
Discussion
Body composition is defined as the proportions and distribution of lean and fatty tissues in the human body [14]. The relationship between SMM, visceral, and SAT in CRPC patients treated with ADT and docetaxel remains largely unclear while it has developed into an emergent topic in urologic oncology. Androgens are known to activate anabolic pathways which result in the gain of lean muscle mass. Thus, castrate levels of testosterone will lead to reduced muscle mass and increased subcutaneous and visceral adipose tissue in men [4, 23, 24]. The influence exerted by androgens on body muscle and fat distribution suggests a relation and association between sarcopenia, obesity, and survival in CRPC. This is more important as docetaxel, a standard treatment for metastatic CRPC (mCRPC), has a high affinity for adipose tissue resulting in an increased accumulation in obese patients [13]. Several previous studies have suggested that higher body fat composition is associated with improved survival, possibly due to the better chemotherapeutic agent distribution and a tolerance to higher doses of cytotoxic chemotherapy [9, 10, 13].
In this study of CRPC patients treated with chemohormonal therapy, 82% and 63% of patients met the criteria for sarcopenia and sarcopenic obesity, respectively. This percentage is considerably higher than the reported average in previous studies [8, 12, 15]. We found that low SMV is an independent factor associated with tumor progression. In a retrospective study assessing muscle mass in 77 CRPC patients who underwent docetaxel treatment of which 34% were diagnosed with sarcopenia, Ohtaka et al. reported that survival time after docetaxel administration was significantly shorter in sarcopenic patients (p < 0.01). These authors further identified sarcopenia as an independent predictive factor for poor tolerance to docetaxel treatment [15]. Conversely, in a retrospective study by Cushen et al. including 63 mCRPC patients treated with docetaxel, of which 47% and 26.7% were sarcopenic and sarcopenic obese, respectively, the authors found no significant difference in survival between sarcopenic and nonsarcopenic patients (17.8 months vs. 15 months, p = 0.4) [8]. Also, the presence of liver metastases was an adverse prognosticator for OS in our study cohort, which goes in line with the findings of the recent meta-analysis of Halabi et al. [22].
On the other hand, there was reported that a high volume of visceral fat area was independently associated with reduced OS (p < 0.01). This suggests that patients with the same BMI may have different proportions of visceral and subcutaneous fat, and that the visceral fat area index is a body composition parameter that may provide information that is not captured by BMI [8]. We further found that a high VSR tends to be prognostic for OS (p = 0.06) and the presence of liver metastases is associated with a decreased OS (p < 0.01). Wu et al. conducted a retrospective review of 333 patients with mCRPC treated with docetaxel of which only three (0.9%) patients were sarcopenic when using the BMI-adjusted definition for sarcopenia [25]. Their analyses of body composition parameters revealed that patients with high VSR ratio had a “near-significant” (p = 0.06) association with decreased survival time as compared with the low VSR group. When stratified by BMI categories, high VSR was associated with shorter survival (median: 9.9 months) as compared with the low VSR group (median: 21.3 months) in patients with normal BMI (p < 0.01) [12]. These results suggest that despite the absence of sarcopenia, high VSR is a significant predictor of shorter survival in CRPC patients treated with chemohormonal therapy.
Antoun et al. analyzed whether body composition parameters exerted a prognostic role in 120 mCRPC patients treated with next-generation androgen receptor axis inhibitors abiraterone and enzalutamide in a postdocetaxel setting. OS was associated with the SAT index: median survival was 15 months for patients with a SAT index < median value and 18 months for patients with SAT index above (p < 0.01). Furthermore, the occurrence of visceral metastasis was a statistically significant predictor of OS compared with that of patients without visceral disease (HR = 2.8; p < 0.01) [10]. Our results are in accordance with the accumulating evidence that SMM, visceral metastasis, and a high visceral-to-subcutaneous fat ratio are independent predictors of survival in CRPC patients. Moreover, it contributes to the narrative that BMI is an inaccurate measure of sarcopenia and obesity, based on its inability to distinguish between lean muscle mass, subcutaneous fat, and visceral fat. Therefore, a combination of various body composition parameters, which are not expressed by BMI alone, may be useful for understanding the metabolic implications and help enlightening on CRPC development and progression. In addition, sarcopenia has been independently associated with higher mortality and higher complication rates in patients treated either with systemic or surgical treatments across multiple cancer sites [8, 14]. The mechanisms responsible for this association have not been fully elucidated; however, it has been proposed that adipose tissue provides a drug reservoir in BMI based-treatments causing an increased rate of dose-limiting toxicity. Pharmacokinetic data are required to support or refute this hypothesis based on lipophilicity of each compound [14]. Assessing individual patients sarcopenia status can provide custom-made strategies so that systemic therapy can be tailored accordingly especially for unfit patients [13, 15]. This would also allow better patient stratification for future clinical trials and provide invaluable information to the clinician in order to facilitate risk-stratified treatment selection and dosage [13]. In order to provide patient-individual treatment, based on body composition, clinicopharmacological trials are needed to formally test for differences in oncological outcomes in patients with reduced, normal and high muscle mass.
Our study is not devoid of limitations which are worth mentioning. First, its retrospective nature may be associated with a risk of selection bias since physician and patient preferences may have affected treatment selection. Second, we were unable to determine the precise duration of ADT therapy prior to initiation of docetaxel. This is of particular importance since the duration of hormonal treatment has a direct role in lean mass and adipose tissue distribution. Thirdly, owing to the small sample size of the study cohort, the prevalence of sarcopenia observed is not necessarily generalizable to a broader group of CRPC patients. Also, body composition parameters may differ between race and thus results can only be applied to the investigated populations. The study is only hypothesis generating as there is no control arm. Further studies are warranted to determine docetaxel pharmacokinetics according to specific body composition parameters in racially diverse populations.
Conclusion
More than 80% of our patients met the criteria for sarcopenia. Low SMV in CRPC patients treated with docetaxel was an independent prognostic factor for progression of disease. The established prognosticator and the presence of liver metastases were independently associated with OS; patients with a high proportion of visceral fat had a trend for shorter OS. In conclusion, we suggest that body composition parameters determined by CT data are useful objective prognostic factors that may support tailored treatment decision-making.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34.
American Cancer Society’s (ACS). Cancer facts and figures 2018. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2018.html. Accessed on 20.08.2019.
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017;71:618–29.
Saylor PJ, Smith MR. Metabolic complications of androgen deprivation therapy for prostate cancer. J Urol. 2013;189:S34–42.
Smith MR, Saad F, Egerdie B, Sieber PR, Tammela TL, Ke C, et al. Sarcopenia during androgen-deprivation therapy for prostate cancer. J Clin Oncol. 2012;30:3271–6.
Hamilton EJ, Gianatti E, Strauss BJ, Wentworth J, Lim-Joon D, Bolton D, et al. Increase in visceral and subcutaneous abdominal fat in men with prostate cancer treated with androgen deprivation therapy. Clin Endocrinol. 2011;74:377–83.
Sharifi N, Dahut WL, Steinberg SM, Figg WD, Tarassoff C, Arlen P, et al. A retrospective study of the time to clinical endpoints for advanced prostate cancer. BJU Int. 2005;96:985–9.
Cushen SJ, Power DG, Murphy KP, McDermott R, Griffin BT, Lim M, et al. Impact of body composition parameters on clinical outcomes in patients with metastatic castrate-resistant prostate cancer treated with docetaxel. Clin Nutr ESPEN. 2016;13:e39–e45.
Antoun S, Bayar A, Ileana E, Laplanche A, Fizazi K, di Palma M, et al. High subcutaneous adipose tissue predicts the prognosis in metastatic castration-resistant prostate cancer patients in post chemotherapy setting. Eur J Cancer. 2015;51:2570–7.
Halabi S, Ou SS, Vogelzang NJ, Small EJ. Inverse correlation between body mass index and clinical outcomes in men with advanced castration–recurrent prostate. Cancer Cancer. 2007;110:1478–84.
Vidal AC, Howard LE, de Hoedt A, Kane CJ, Terris MK, Aronson WJ, et al. Obese patients with castration-resistant prostate cancer may be at a lower risk of all-cause mortality: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) database. BJU Int 2018;122:76–82.
Wu W, Liu X, Chaftari P, Cruz Carreras MT, Gonzalez C, Viets-Upchurch J, et al. Association of body composition with outcome of docetaxel chemotherapy in metastatic prostate cancer: a retrospective review. PLoS One. 2015;10:e0122047.
Lee JS, Lee HS, Ha JS, Han KS, Rha KH, Hong SJ, et al. Subcutaneous fat distribution is a prognostic biomarker for men with castration resistant prostate cancer. J Urol. 2018;200:114–20.
Baracos VE, Arribas L. Sarcopenic obesity: hidden muscle wasting and its impact for survival and complications of cancer therapy. Ann Oncol. 2018;29:ii1–ii9.
Ohtaka A, Aoki H, Nagata M, Kanayamaa M, Shimizu F, Ide H, et al. Sarcopenia is a poor prognostic factor of castration-resistant prostate cancer treated with docetaxel therapy. Prostate Int. 2019;7:9–14.
Shariat SF, Semjonow A, Lilja H, Savage C, Vickers AJ, Bjartell A. Tumor markers in prostate cancer I: blood-based markers. Acta Oncol Stock Swed. 2011;50:61–75.
Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab. 2008;33:997–1006.
Fearon K, Strasser F, Anker SD. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12:489–95.
Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol. 2013;31:1539–47.
Shen W, Punyanitya M, Wang Z, Gallagher D, St-Onge MP, Albu J, et al. Total body skeletal muscle and adipose tissue volumes: estimation from a single abdominal cross-sectional image. J Appl Physiol. 2004;97:2333–8.
Scher HI, Halabi S, Tannock I, Morris M, Sternberg CN, Carducci MA, et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol J Am Soc Clin Oncol. 2008;26:1148–59.
Halabi S, Kelly WK, Ma H, Zhou H, Solomon NC, Fizazi K, et al. Meta-analysis evaluating the impact of site of metastasis on overall survival in men with castration-resistant prostate cancer. J Clin Oncol J Am Soc Clin Oncol. 2016;34:1652–9.
Foulkes SJ, Daly RM, Fraser SF. The clinical importance of quantifying body fat distribution during androgen deprivation therapy for prostate cancer. Endocr Relat Cancer. 2017;24:R35–R48.
Mitsuzuka K, Arai Y. Metabolic changes in patients with prostate cancer during androgen deprivation therapy. Int J Urol. 2018;25:45–53.
Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol J Am Soc Clin Oncol. 2013;31:1539–47.
Acknowledgements
We would like to thank G. Poglitsch for assistance with the collection of the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SFS: advisory board of and/or speaker for Astellas, Astra Zeneca, Bayer, BMS, Cepheid, Ferring, Ipsen, Jansen, Lissy, MSD, Olympus, Pfizer, Pierre Fabre, Roche, Sanochemia, Sanofi, and Wolff. GK: advisory board of and/or speaker for Astellas, Bayer AG, BMS, Ipsen, Janssen, MSD, Roche, Takeda, and Sanofi. All other authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Stangl-Kremser, J., Suarez‐Ibarrola, R., Andrea, D.D. et al. Assessment of body composition in the advanced stage of castration-resistant prostate cancer: special focus on sarcopenia. Prostate Cancer Prostatic Dis 23, 309–315 (2020). https://doi.org/10.1038/s41391-019-0186-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-019-0186-6
- Springer Nature Limited
This article is cited by
-
Creatine supplementation and resistance training to preserve muscle mass and attenuate cancer progression (CREATINE-52): a protocol for a double-blind randomized controlled trial
BMC Cancer (2024)
-
Associations of fat and muscle mass with overall survival in men with prostate cancer: a systematic review with meta-analysis
Prostate Cancer and Prostatic Diseases (2022)
-
Adiposity and cancer survival: a systematic review and meta-analysis
Cancer Causes & Control (2022)
-
Opportunistic skeletal muscle metrics as prognostic tools in metastatic castration-resistant prostate cancer patients candidates to receive Radium-223
Annals of Nuclear Medicine (2022)