Abstract
Background
Neutrophil–lymphocyte ratio (NLR) is a widely used, representative marker of systemic inflammatory response within the body. NLR can be calculated from simple, inexpensive peripheral blood samples. High NLR is a negative prognostic factor in a variety of malignancies including urological tumors. In this study, we aim to assess the prognostic value of preoperative neutrophil- lymphocyte ratio (NLR) in patients treated with radical prostatectomy (RP) for localized prostate cancer (PCa).
Materials and methods
Records of 7426 patients were retrospectively analyzed from prospectively collected datasets. A cut-off point of 3 was taken for NLR based on ROC analyses and previous literature.
Results
23% (n = 1707) of patients had an NLR of ≥3. Patients with NLR ≥3 were more likely to harbor unfavorable pathological features such as higher biopsy Gleason score (GS), higher RP GS, higher rates of extra capsular extension, nodal involvement (all p < 0.001) and positive surgical margins (p = 0.002). On multivariable analyses, NLR ≥ 3 was associated with higher RP GS (OR 2.32; p < 0.001), seminal vesicle invasion (OR 1.60; p < 0.001) and nodal involvement (OR 1.43; p < 0.001). On multivariable analyses, NLR ≥ 3 was significantly associated with GS upgrading at RP (OR 1.39 p < 0.001). During a median follow up of 45 months, NLR ≥ 3 was associated with higher risk of BCR (p = 0.001). However, on multivariable Cox regression analysis such association was not shown (HR 0.86; p = 0.4).
Conclusion
Preoperative NLR ≥ 3 was associated with aggressive PCa, such as upgrading at RP. Even though its effect on clinical-decision making seems to be limited when all clinical and pathological confounders are taken into account, preoperative NLR may still be useful in selected patients to identify aggressive PCa helping patient selection for active surveillance protocols. Conversely, it does not predict BCR when adjusted for the effect of pathological features.
Similar content being viewed by others
Introduction
Prostate cancer (PCa) alone accounts for 27% of newly diagnosed cancers in men each year in the United States and it is the second most common cause of male deaths [1]. Inflammation plays a key role in the initiation and progression of various cancers [2]. Indeed, markers of systemic inflammation is associated with poor prognosis in urological and other malignancies [3,4,5]. In the tumor microenvironment, tumor infiltrating inflammatory cells produce mediators and cytokines that can induce or promote angiogenesis, tumor growth, invasion and metastasis [2, 6, 7]. In concert with these processes, various systemic inflammation markers such as serum white blood cells, neutrophils, lymphocytes, platelets and acute-phase proteins have been shown to predict prognosis and response to therapy in various malignancies [4, 8, 9].
Neutrophil–lymphocyte ratio (NLR) is a widely used, representative marker of systemic inflammatory response within the body. NLR can be calculated from simple, inexpensive peripheral blood samples. High NLR is a negative prognostic factor in a variety of malignancies including urological tumors [10,11,12,13]. Previous studies have shown possible clinical use of NLR at various PCa disease states. For example NLR predicts PCa presence in men who underwent prostate needle biopsy [14] as well as worse prognosis in patients with advanced metastatic castration resistant PCa [15, 16]. Further studies assessed the prognostic value of NLR in patients with localized PCa, a disease stage that needs biomarkers to improve risk stratification to help with clinical decision-making. In two recent, relatively small cohort studies (n = 1367 and n = 175), high NLR was associated with unfavorable outcomes such as biochemical recurrence (BCR) after RP [10, 17]. In a recent meta-analysis, high pretreatment NLR was found to have significant prognostic value with regards to patients with advanced PCa but not in patients with localized PCa [12].
We hypothesized that preoperative NLR is associated with unfavorable outcomes for localized PCa and assessed its prognostic effect in a large contemporary multicenter cohort of men treated with RP for clinically non-metastatic PCa. We focused on its value in improving our predictive accuracy for identifying low risk patients who are safe to undergo active surveillance.
Materials and methods
Records of all patients who were treated with RP between 2000 and 2010 were retrospectively analyzed from prospectively collected data after receiving approval from the Institutional Review Board of the Weill Cornell Medical College. Preoperative complete blood cell count with differential were collected and NLR was calculated as the neutrophil count divided by the lymphocyte count. In patients where multiple measurements were taken, the mean value was taken into account. To minimize confounding effects blood test were obtained earliest 3 weeks after prostate biopsy and within 30 days prior to RP. As standard procedure, urine dipstick examinations as well as urine cultures were performed prior to surgery. Hundred forty-three patients with a history of chronic inflammatory disease or on chronic steroid medication were excluded. None of the patients had adjuvant therapy for PCa. Preoperative and postoperative clinico-pathological characteristics and BCR outcomes were collected from our database. A rise in the PSA level ≥0.2 ng/mL on two consecutive occasions was defined as BCR [18]. The date of the first rise was considered as the date of BCR. Dedicated uro-pathologists processed the RP specimens were processed according to international standards [19]. Staging and grading was reported according to the 2009 American Joint Committee on Cancer TNM staging system and the International Society of Urological Pathology 2005. All specimens were re-reviewed locally to standardize reporting. Follow-up consisted of PSA measurements that were generally carried out quarterly in the first year, semiannually in years 2–5 and annually thereafter.
Statistics
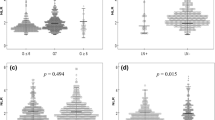
A cut-off point of 3 was taken for NLR based on visual best correlation of the ROC analyses focusing on BCR; this was in line with the previous literature [12]. Means, medians, and Interquartile ranges (IQR) were reported for continuously coded variables. Chi-square and Mann-Whitney-U tests were used to compare the statistical significance of differences in proportions and medians, respectively. Logistic regression analyses were performed to assess the association of NLR with adverse pathological features and Gleason score upgrading. Kaplan Meier and Cox regression analyses were performed to assess the association of NLR with BCR. The area under the curve (AUC) for each variable was estimated and compared according to DeLong et al. [20]. Bonferroni corrections were carried out for multivariable logistic regression analysis. Subgroup analyses were also performed by stratifying the patients into D’Amico risk groups [21]. SPSS software package (version 21.0; SPSS, Chicago, IL, USA) and Stata v.12 (Stata Corp LP, College Station, TX, USA) were used for statistical analysis. All p values were two-sided and those <0.05 were considered statistically significant.
Results
A total of 7426 patients who underwent RP for PCa were included in the final analysis. Median age was 61 years [IQR: 57–66]. 23% (n = 1707) of patients had a NLR of ≥3. The patients with NLR ≥ 3 were more likely to harbor unfavorable pathological features such as higher biopsy Gleason score (GS) (p < 0.001), higher RP GS (p < 0.001), extra capsular extension (p < 0.001), nodal involvement (p < 0.001) and positive surgical margins (p = 0.002). Clinico-pathological characteristics of all patients and their association with NLR stratified by the cut-off of 3 are summarized in Table 1.
In multivariable logistic regression analysis that adjusted for the effects of age, preoperative PSA, preoperative biopsy GS and clinical stage, NLR ≥ 3 was associated with higher RP GS (OR 2.32; p < 0.001), seminal vesicle invasion (OR 1.60; p < 0.001) and nodal involvement (OR 1.43; p < 0.001) even after performing Bonferroni corrections (Table 2). Similarly, after stratifying the patients according D’Amico risk groups, preoperative NLR ≥ 3 remained associated with adverse pathological results for low and intermediate, but not high D’Amico risk groups in multivariable analyses ([OR 2.07; p < 0.001] and (OR 1.73; p < 0.001), for low and intermediate groups respectively) (Table 3).
A preoperative model predicting higher RP GS including biopsy GS, age, clinical stage and preoperative PSA had an AUC of 0.80. Addition of preoperative NLR increased the discrimination of the model to 0.82. However, addition of preoperative NLR did not increase the discrimination of this model build on standard preoperative features to predict positive surgical margin status, seminal vesicle invasion or nodal involvement (data not shown).
Overall 2983 (40.2%) patients had GS upgrading from biopsy to RP specimens. In multivariable logistic regression analysis that adjusted for the effects of age, year of surgery, preoperative PSA, and clinical stage, NLR ≥ 3 was significantly associated with GS upgrading (OR 1.39 p < 0.001). In the subgroups analyses 2126 of the 4023 (52.8%) patients who had GS 6 and 736 of the 2013 (36%) patients who had GS7 (3+4) at the initial biopsy had GS upgrading at RP. Similarly, in multivariable logistic regression analysis that adjusted for the effects of age, year of surgery, preoperative PSA, and clinical stage, NLR ≥ 3 was significantly associated with GS upgrading at RP for both subgroups ((OR 1.84 p < 0.001) and (OR 2.30 p < 0.001), respectively). A preoperative model predicting GS upgrading at RP in the overall population including age, year of surgery, preoperative PSA and clinical stage had an AUC of 0.62. Addition of preoperative NLR increased the discrimination of the model to 0.65.
During a median follow up of 45 months (IQR 29.7–55.0), 815 (11%) patients experienced BCR. On Kaplan Meier analysis, patients with NLR ≥ 3 had a significantly higher risk of experiencing BCR (p = 0.001). However, on multivariable Cox regression analysis that adjusted for the effects of standard clinical and pathological features, NLR did not retain its association with BCR (HR 0.86; p = 0.4) Stratifying patients according to D’Amico risk groups did not affect the lack of significance of the associations between NLR and BCR. (p ≥ 0.2)
Discussion
We found that preoperative NLR ≥ 3 is associated with adverse pathological features such as higher RP GS, seminal vesicle invasion and nodal involvement. Knowledge of preoperative NLR helped most with prediction of GS upgrading from biopsy to RP, specifically in patients who could be considered for active surveillance. Considering the strong prognostic power of biopsy GS for the prediction of clinical behavior and treatment response at almost each disease stage [22] knowledge of preoperative NLR seems to add information to improve clinical decision-making.
Similar to our findings, a high NLR was associated with adverse pathological features in a recent publication by Lee et al. [10]. In this study patients with NLR ≥ 2.5 had a higher biopsy GS (p < 0.001), pathological GS (p < 0.001), and pathological stage (p < 0.001) than patients with NLR < 2.5. Multivariable analysis revealed high NLR to be significantly correlated with adverse pathological outcomes such as higher pathological stage (HR 1.688; p = 0.009) and extra-prostatic disease (HR 1.698; p = 0.008).
On the other hand, Maeda et al. was unable to demonstrate a relationship between NLR and adverse pathologic features after RP [23]. However conclusions from this study are limited because of its small cohort size (n = 73). Similar to their findings, Minardi et al. found no association between NLR ≥ 3 and baseline total PSA, GS or pathological stage [24]. Another study where NLR was unable to predicting adverse pathologic outcomes in PCa was published by Young et al. [25]. Their patient cohort consisted of 217 low-risk PCa patients who had undergone robot-assisted RP. A high NLR was not associated with disease upstaging, GS upgrading or with BCR [25]. These last results are in contradiction with our findings. We could show a significant association between preoperative NLR ≥ 3 and adverse pathological features such as upstaging and upgrading. In our study, 40.2% of patients in the overall population showed GS upgrading at RP and NLR ≥ 3 was a strong predictor for GS upgrading. In addition, the subgroup of patients with preoperative NLR ≥ 3 who had biopsy GS 6 or biopsy GS 7 (3+4) had significantly higher risk of having GS upgrading at RP. Furthermore, in our multivariable analysis, patients with preoperative NLR ≥ 3 in the D’Amico low risk and intermediate risk groups had significantly more pathological features of biologically and clinically aggressive disease compared to patients with NLR < 3.
D’Amico risk classification is used to predict prognosis and decide management strategies. Patients belonging to D’Amico low-risk group can for example be counseled to undergo active surveillance protocols depending on their prostate biopsy results. In the past, some studies even offered active surveillance to patients belonging to intermediate-risk group [26, 27].
To increase the accuracy of patient selection to ensure the identification of right patient with the right tumor for active surveillance, various tests have been proposed such as Decipher™, Oncotype DX®, Prolaris® and ProMark®. Even though these biomarkers can be helpful for post-biopsy decision-making for low risk patients and post-radical prostatectomy for patient selection, they are very expensive and not widely available [28]. On the other hand NLR is a simple and inexpensive tool.
The impact of high NLR on predicting BCR seems to be limited when all clinical and pathological confounders are taken into account. Even though patients with NLR ≥ 3 had a significantly higher risk of experiencing BCR after RP in univariable analysis, in multivariable analysis that adjusted for the effects of standard clinical and pathological features, it did not retain its association with BCR. Similarly, in a study with 731 patients treated with RP for clinically localized PCa, patients with a NLR ≥ 3 had a higher likelihood to experience recurrence than those patients with a NLR < 3. But in multivariable analyses that adjusted for total neutrophil and lymphocyte count, age, total PSA, Gleason grading, stage, and surgical margin status, NLR was not anymore associated with BCR [24].
Most of the studies published to date that investigated the relationship of NLR with PCa had relatively smaller patient cohorts. In order to overcome this limitation, Tang et al. conducted a systematic review and meta-analysis assessing the prognostic value of NLR in localized and advanced PCa [12]. A total of 9418 patients from 18 studies were included in their meta-analysis; 10 studies included locally advanced or metastatic castration resistant PCa patients, and the other 8 included patients with localized PCa. Dichotomized cut-off values for NLR varied from 2 to 5 in the included studies. However, the subgroup analysis showed NLR ≥ 3 to have the most significant prognostic value. In 4819 patients from 10 studies, higher NLR was associated with an increased risk of disease recurrence (HR 1.367) but the studies suffered from significant heterogeneity (I2 = 57.1, P = 0.013). Sub-group analysis revealed this effect to be more significant in patients with advanced PCa manifested as clinical recurrence (HR 1.840), than in patients with localized PCa manifested as BCR (HR 1.208). NLR was positively related to lymph node involvement (OR 1.616) but unlike our study the meta-analysis showed no impact of NLR on pathological stage (OR 0.827) or GS (OR 0.761) [12].
The contradictory data regarding the predictive value of preoperative NLR in localized PCa stems from the heterogeneity and differences in patient cohorts. Despite the retrospective nature of our study, its large size and multicenter nature could be considered as strength. Limitations of our study are, utilization of different laboratories for NLR measurements and the relatively short follow-up time. Choosing the optimal cut-off point is also another challenge and even though there are various calculations in the literature, most large studies agree at the cut-off value of NLR ≥ 3 [12]. Our database lacked detailed biopsy results such as number of positive cores or percentage of positive cores but even if their biopsy results would be suitable for active surveillance, patients with NLR ≥ 3 are probably not the best candidates for deferred treatment strategies.
Conclusions
Preoperative NLR ≥ 3 was associated with pathological features of biologically and clinically aggressive PCa, such as upgrading at RP. Even though its effect on clinical-decision making seems to be limited when all clinical and pathological confounders are taken into account, preoperative NLR may be still be useful in selected patients to identify aggressive PCa helping patient selection for active surveillance protocols. Conversely, it does not predict BCR when adjusted for the effect of pathological features.
Author contributions
MÖ: Project development, Data Management, Manuscript writing. MM: Data Management, Data analysis. HF: Manuscript writing. FS: Data analysis. CS: Manuscript editing. TK: Data analysis, Manuscript editing. KG: Data management. AB: project development, Manuscript editing. PIK: Data collection, Manuscript editing. MR: Manuscript editing, project development. GK: Data management. SFS: Protocol/project development, Data collection, Manuscript writing/editing.
References
Siegel, RL, Miller, KD, Jemal, A Cancer statistics, 2016. CA Cancer J Clin. 2016 Jan [cited 2017 Jul 4];66:7–30. http://www.ncbi.nlm.nih.gov/pubmed/26742998.
Mantovani A, Allavena P, Sica A, Balkwill F, Cancer-related inflammation. Nature. 2008;454:436–44. http://www.nature.com/doifinder/10.1038/nature07205.
De Martino, M et al. Validation of serum C-reactive protein (CRP) as an independent prognostic factor for disease-free survival in patients with localised renal cell carcinoma (RCC). BJU Int. 2013;111:E348–53.
Zhou L, Cai X, Liu Q, Jian Z-Y, Li H, Wang K-J. Prognostic role of C-reactive protein in urological cancers: a meta-analysis. Sci Rep. 2015;5:12733 https://doi.org/10.1038/srep12733.
Macciò A, Madeddu C. Inflammation and ovarian cancer. Cytokine. 2012;58:133–47.
Lu H, Ouyang W, Huang C. Inflammation, a key event in cancer development. Mol Cancer Res. 2006;4:221–33. http://mcr.aacrjournals.org/content/4/4/221.full.html%5Cnhttp://mcr.aacrjournals.org/content/4/4/221.full
Kusumanto YH, Dam WA, Hospers GAP, Meijer C, Mulder NH. Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis. 2003;6:283–7.
Sevcenco S, Mathieu R, Baltzer P, Klatte T, Fajkovic H, Seitz C, et al. The prognostic role of preoperative serum C-reactive protein in predicting the biochemical recurrence in patients treated with radical prostatectomy. Prostate Cancer Prostatic Dis. 2016;19:163–7.
Koike Y, Miki C, Okugawa Y, Yokoe T, Toiyama Y, Tanaka K, et al. Preoperative C-reactive protein as a prognostic and therapeutic marker for colorectal cancer. J Surg Oncol. 2008;98:540–4.
Lee H, Jeong SJ, Hong SK, Byun S-S, Lee SE, Oh JJ. High preoperative neutrophil-lymphocyte ratio predicts biochemical recurrence in patients with localized prostate cancer after radical prostatectomy. World J Urol. 2016;34:821–7. http://www.ncbi.nlm.nih.gov/pubmed/26449784.
De Martino M, Pantuck AJ, Hofbauer S, Waldert M, Shariat SF, Belldegrun AS, et al. Prognostic impact of preoperative neutrophil-to-lymphocyte ratio in localized nonclear cell renal cell carcinoma. J Urol. 2013;190:1999–2004.
Tang L, Li X, Wang B, Luo G, Gu L, Chen L, et al. Prognostic value of neutrophil-to-lymphocyte ratio in localized and advanced prostate cancer: a systematic review and meta-analysis. PLoS One. 2016;11:e0153981. http://dx.plos.org/10.1371/journal.pone.0153981
Templeton, AJ et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106:dju124.
Kawahara T, Fukui S, Sakamaki K, Ito Y, Ito H, Kobayashi N, et al. Neutrophil-to-lymphocyte ratio predicts prostatic carcinoma in men undergoing needle biopsy. Oncotarget. 2015;6:32169–76.
Nuhn P, Vaghasia AM, Goyal J, Zhou XC, Carducci MA, Eisenberger MA, et al. Association of pretreatment neutrophil-to-lymphocyte ratio (NLR) and overall survival (OS) in patients with metastatic castration-resistant prostate cancer (mCRPC) treated with first-line docetaxel. BJU Int. 2014;114:E11–7.
Leibowitz-Amit R, Templeton AJ, Omlin A, Pezaro C, Atenafu EG, Keizman D, et al. Clinical variables associated with PSA response to abiraterone acetate in patients with metastatic castration-resistant prostate cancer. Ann Oncol. 2014;25:657–62. http://annonc.oxfordjournals.org/content/25/3/657.short
Gazel E, Tastemur S, Acikgoz O, Yigman M, Olcucuoglu E, Camtosun A, et al. Importance of neutrophil/lymphocyte ratio in prediction of PSA recurrence after radical prostatectomy. Asian Pacific J Cancer Prev. 2015;16:1813–6.
Cookson MS, et al. Variation in the definition of biochemical recurrence in patients treated for localized prostate cancer: the American Urological Association Prostate Guidelines for Localized Prostate CancerUpdate Panel report and recommendations for a standard in the reporting of surgical outcomes. Urol. 2007;177:540–5.
Wheeler TM, Lebovitz RM. Fresh tissue harvest for research from prostatectomy specimens. Prostate. 1994;25:274–9. [cited 2016 Nov 27]. http://doi.wiley.com/10.1002/pros.2990250507.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988 [cited 2017 Jul 12];44:837–45. http://www.ncbi.nlm.nih.gov/pubmed/3203132.
D’Amico AV, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. J Am Med Assoc 1998;280:969–74.
Partin AW, Mangold LA, Lamm DM, Walsh PC, Epstein JI, Pearson JD. Contemporary update of prostate cancer staging nomograms (Partin Tables) for the new millennium. Urology. 2001;58:843–8.
Maeda Y, Kawahara T, Koizumi M, Ito H, Kumano Y, Ohtaka M, et al. Lack of an association between neutrophil-to-lymphocyte ratio and PSA failure of prostate cancer patients who underwent radical prostatectomy. Biomed Res Int. 2016;2016:6197353.
Minardi D, Scartozzi M, Montesi L, Santoni M, Burattini L, Bianconi M, et al. Neutrophil-to-lymphocyte ratio may be associated with the outcome in patients with prostate cancer. Springerplus. 2015;4:255. http://www.springerplus.com/content/4/1/255.
Kwon YS, Han CS, Yu JW, Kim S, Modi P, Davis R, et al. Neutrophil and lymphocyte counts as clinical markers for stratifying low-risk prostate cancer. Clin Genitourin Cancer. 2016;14:e1–8. http://linkinghub.elsevier.com/retrieve/pii/S1558767315001913.
Montironi R, Hammond EH, Lin DW, Gore JL, Srigley JR, Samaratunga H, et al. Consensus statement with recommendations on active surveillance inclusion criteria and definition of progression in men with localized prostate cancer: the critical role of the pathologist. Virchows Archiv. 2014;465:623–8.
Ploussard G, Isbarn H, Briganti A, Sooriakumaran P, Surcel CI, Salomon L, et al. Can we expand active surveillance criteria to include biopsy Gleason 3+4 prostate cancer? A multi-institutional study of 2,323 patients. Urol Oncol Semin Orig Investig. 2015;33:71e1–9.
Moschini M, Spahn M, Mattei A, Cheville J, Karnes RJ. Incorporation of tissue-based genomic biomarkers into localized prostate cancer clinics. BMC Med. 2016;14:67. http://www.ncbi.nlm.nih.gov/pubmed/27044421%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4820857.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with Ethical Standards
All data were collected after receiving approval from local ethical committee.
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Özsoy, M., Moschini, M., Fajkovic, H. et al. Elevated preoperative neutrophil–lymphocyte ratio predicts upgrading at radical prostatectomy. Prostate Cancer Prostatic Dis 21, 100–105 (2018). https://doi.org/10.1038/s41391-017-0015-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-017-0015-8
- Springer Nature Limited
This article is cited by
-
A high high-density lipoprotein level is associated with Gleason score upgrade in Chinese patients diagnosed with high-grade prostate carcinoma
BMC Urology (2023)
-
Neutrophil-to-lymphocyte ratio predicts nodal involvement in unfavourable, clinically nonmetastatic prostate cancer patients and overall survival in pN1 patients
Scientific Reports (2023)