Abstract
Background
Acute kidney injury (AKI) is common but not often recognized. Early recognition and management may improve patient outcomes.
Methods
This is a prospective, nonrandomized study of clinical decision support (CDS) system [combining electronic alert and standardized care pathway (SCP)] to evaluate AKI detection and progression in hospitalized children. The study was done in three phases: pre-, intervention (CDS) and post. During CDS, text-page with AKI stage and link to SCP was sent to patient’s contact provider at diagnosis of AKI using creatinine. The SCP provided guidelines on AKI management [AEIOU: Assess cause of AKI, Evaluate drug doses, Intake-Output charting, Optimize volume status, Urine dipstick].
Results
In all, 239 episodes of AKI in 225 patients (97 females, 43.1%) were analyzed. Proportion of patients with decrease in the stage of AKI after onset was 71.4% for CDS vs. 64.4% for pre- and 55% for post-CDS phases (p = 0.3). Documentation of AKI was higher during CDS (74.3% CDS vs. 47.5% pre- and 57.5% post-, p < 0.001). Significantly greater proportion of patients had nephrotoxic medications adjusted, or fluid plan changed during CDS. Patients from CDS phase had higher eGFR at discharge and at follow-up.
Conclusions
AKI remains under-recognized. CDS (electronic alerts and SCP) improve recognition and allow early intervention. This may improve long-term outcomes, but larger studies are needed.
Impact
-
Acute kidney injury can cause significant morbidity and mortality. It is under-recognized in children.
-
Clinical decision support can be used to leverage existing data in the electronic health record to improve AKI recognition.
-
This study demonstrates the use of a novel, electronic health record-linked, clinical decision support tool to improve the recognition of AKI and guideline-adherent clinical care.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is a common clinical event in hospitalized children. In recent years, large epidemiologic studies have provided significant information on the incidence of AKI in the pediatric and neonatal intensive care units (ICU).1,2 Limited data are available regarding pediatric AKI outside the ICU. Using International Classification of Diseases, Ninth Revision, Clinical Modification codes, Sutherland et al.3 found an AKI incidence of 3.9/1000 pediatric admissions. Another study using retrospective data from the electronic health records (EHR) reported that only 17% of non-ICU admissions had two or more creatinine measurements allowing for AKI evaluation.4 AKI was observed in 30% of these patients who had at least two creatinine measurements. By extrapolating to all pediatric in-patients, they estimated that AKI occurred a minimum of 5% of all noncritically ill hospitalized children. However, given that 83% of the patients had insufficient creatinine measurements to diagnose AKI, their true incidence was likely higher than 5%.4 This study showed how AKI was underdiagnosed because creatinine was not checked. On the other hand, the almost tenfold difference in estimates between these two studies (0.39 vs. 5%) showed that there is significant under-reporting of AKI.3,4 This under-reporting can result from a lack of diagnosis (due to inadequate testing) or a lack of documentation.
Acute kidney injury is independently associated with prolonged hospital stays, increased risk of in-hospital death, and future risk of hypertension and progression to chronic kidney disease (CKD).1,5,6 Hypertension and CKD are modifiable cardiovascular risk factors, which, if present in childhood, may lead to long-term increased morbidity.6 In the acute phase, management of AKI focuses on supportive care, which includes monitoring fluid balance, avoidance of nephrotoxic medications, and appropriate diagnostic investigations.7 In the long term, patients need to be monitored for hypertension and CKD.6 Hence, both diagnosis and documentation of AKI is important for appropriate management. Even in patients where creatinine is checked, small changes are not easily recognized by providers, especially in pediatrics where the baseline creatinine may be low to begin with.3 Studies have shown that even a small rise in creatinine may be associated with poor outcomes.8 Another reason why AKI may not be recognized in a timely manner by providers is the absence of a known baseline creatinine.9
According to the Acute Disease Quality Initiative (ADQI), AKI is well suited to prediction and risk stratification.10 It has a standard consensus definition that relies on discrete markers like creatinine and urine output, which can be extracted from the EHR.10,11 In recent years various clinical decision support (CDS) systems, which include automated real-time electronic alerts (e-alert), have been developed to improve the detection and management of AKI.9,12,13 E-alerts are based on the idea that early identification of AKI may improve the standard of care and patient outcomes. Using an e-alert, Holmes et al.9 looked at the population-based incidence of AKI in neonates and children using a standardized electronic detection algorithm. Based on the number of AKI episodes and census data, they reported an incidence of 1.37 cases/1000 person-years. This incidence is higher than the 3.3 cases per 100,000 children reported from a previous population-based study out of Norway using ICD-10 codes.9 The discrepancy between the two suggests that the recognition and diagnosis of AKI is improved with an e-alert.
While the recognition of AKI has improved, the impact of e-alerts on the outcome of AKI is debatable.14 The inconsistent results seen from them could be secondary to an absence of clear directions to follow once AKI is identified. E-alerts work better when combined with a process that directs clinicians how to use the information they receive regarding the development of AKI has to be implemented.15 These actionable interventions can be in various formats. One such intervention was used in the Nephrotoxic Injury Negated by Just-in-time Action (NINJA) study.16 They used an automated daily EHR trigger to identify patients with high nephrotoxic medication exposure. Once patients were identified, pharmacists would recommend daily SCr measurement, dose adjustment, or use of less nephrotoxic regimens.16 Other studies have used an AKI care bundle as part of their CDS. These care bundles often contain simple guidelines to manage AKI.17
We designed a prospective, single-center, nonrandomized study, in three phases, to study the hypothesis that the use of a CDS system will improve both the detection of AKI and renal outcomes of children with AKI. This was a pilot study with the primary objective to evaluate if a targeted intervention that combined an e-alert with a standardized care pathway could reduce the increase in AKI stage after diagnosis in children.
Methods
The study was approved by the Institutional Review Board at Seattle Children’s Hospital (SCH) with waiver of the need for informed consent. Study procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. This study was conducted between January 2018 and October 2018. At SCH, patients are admitted to a specialty service (including nephrology) as primary or to the general pediatric service based on the reason for admission. All patients between 6 months and 18 years who were admitted with or developed AKI in all non-ICU inpatient units of the hospital were included. Patients were excluded if they had a history of CKD ≥ stage 4 (i.e., patients with an estimated glomerular filtration rate < 30 mL/min/1.73 m2), had a renal transplantation or nephrectomy within the last 3 months, were admitted to the nephrology service from the emergency department after the alert, or were receiving palliative care.
AKI “sniffer” and electronic alert
The electronic AKI surveillance tool (AKI “sniffer”) was developed on our EHR platform and was configured according to the KDIGO AKI classification. Baseline serum creatinine (SCr) was established as the lowest creatinine up to 6 months before admission. If no baseline SCr was available in the EHR, a reference estimated creatinine clearance of 120 mL/min/m2 was used and a baseline creatinine was calculated using the modified Schwartz equation and patient’s height in centimeters, as has been previously validated.18 AKI was defined as a 50% rise from baseline over 7 days or a 0.3 mg/dL rise over 48 h.7 For patients with a baseline SCr value of <0.5 mg/dL, the algorithm was configured to generate an AKI alert if they met the above criteria and SCr increased to values to ≥0.5 mg/dL. This was done to prevent over-diagnosis of AKI, particularly in the younger patients based on the potential error or variations in laboratory measurements.19 A patient was considered as having a repeat episode of AKI during the admission if SCr increased after having returned to baseline for a period of ≥7 days. AKI was staged for severity according to the rise in SCr per KDIGO criteria.7 The “sniffer” was triggered in real time when AKI was detected based on the change in SCr.
Community-acquired AKI was defined as an episode of AKI when the initial event occurred outside of the hospital setting and the patient was admitted with a diagnosis of AKI, or developed it within 24 h of admission. Hospital-acquired AKI was defined as an episode of AKI in patients who were admitted with a normal SCr and developed de novo AKI during their hospital stay.
Study design
A before-after-post design was chosen comparing three study phases. During a 2-month pre-alert control phase, the AKI sniffer sent AKI events by e-mail to the principal investigator (PI). This was followed by a 6-month alert phase during which AKI e-alerts were sent to the primary in-house provider. In our health system, each patient is electronically assigned a primary in-house provider (such as an intern, senior resident or nurse practitioner) who acts as the clinical contact point for that patient. The hospital uses a secure paging system that is compliant with patient privacy standards. We chose to use a short messaging system-based text-page to send the e-alert to the contact provider listed for each patient. The text-page read: “Patient [Initials], [Room Number], has been identified as having acute kidney injury (AKI) Stage [_] based upon the latest creatinine value. Please follow the AKI Care Pathway”. The third phase consisted of a 2-month control period (post-alert control phase), when no AKI alerts were sent to providers, but an e-mail was sent to the PI.
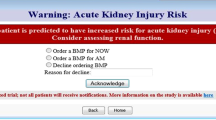
AKI care pathway
The AKI care pathway was derived from KDIGO guidelines and best practice recommendations.7 It was in the form of a guideline and consisted of five simple steps (“AEIOU,” Fig. 1). Prior to the start of the alert phase, information on recognition and management of AKI and the care pathway was disseminated among providers via lectures, emails, and posters. It was also posted in team work rooms and online on the hospital intranet. Providers were informed about the e-alert and the page that they might receive. There was no provision to opt-out of receiving the pages, but the components of the AKI care pathway were optional.
Outcome measures
We had two primary outcome measures: First, AKI progression, defined as AKI that increases by at least one stage from the AKI-stage at time of first detection; and second, a decrease in stage of AKI within 48 h after onset. For secondary outcomes, we looked at processes followed, including adjustment of drug doses, monitoring of fluid balance, documentation of AKI in the progress notes, peak AKI stage, and creatinine at discharge and follow-up.
Data collection included demographic, laboratory parameters, and clinical characteristics. Information was also collected on the history of AKI based on chart review and clinical adjudication in the previous 6 months prior to the study.
Statistical analysis
Socio-demographic, laboratory, and clinical features of study participants were summarized and compared between the intervention phases. Continuous variables were summarized using mean (and standard deviation) and compared between phases using ANOVA. Categorical variables were summarized using counts and proportions and compared using Pearson’s chi-square or Fisher’s Exact Tests as appropriate. Log-binomial regression was used to compare AKI documentation, charting of input/output monitoring, dose adjustments, nephrotoxic medications stopped, and renal consults between the study phases. Results were reported as relative risk and 95% confidence intervals. A p value of 0.05 was considered statistically significant. Adjustments for multiple comparisons were not performed. SAS 9.4 (Cary, NC) was used for all analyses.
Results
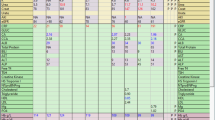
There were 375 alerts during the study period. Of these, 39 (10.4%) were adjudicated by the investigators to be false-positive due to an incorrect baseline. These patients had at least one SCr value during a previous prolonged hospitalization that was much lower than what would be appropriate for their age and size, which resulted in a false alert. Another 72 met the exclusion criteria, and 25 were repeat alerts on the patient due to an increase in the stage of AKI (Fig. 2). Thus, 239 unique episodes of AKI were recorded during the study period in 225 patients (97 females, 43.1%). Baseline SCr was available for 185 (82.3%) patients and calculated for the remaining 40 (17.8%). Sixty-five patients (28.9%) had a history of transplant, most commonly hematopoietic stem cell transplant, and 89 (39.5%) had a history of AKI in the previous 6 months. The characteristics of patients based on their study phases are described in Table 1.
Details of the AKI episode and management of AKI are shown in Table 2. Overall, 68.6% alerts (n = 164) were for AKI stage 1 and 47% of the episodes of AKI were deemed to be hospital-acquired (n = 112). Between the three phases, the frequency of severe AKI (AKI stage 2–3 by KDIGO) varied from 25 to 37% (Table 2). For our primary outcome measures, AKI progression was seen in 13.8% patients in the CDS phase, compared to 15.2% in the pre- and 8.7% in the post-CDS phases (p = 0.8). The proportion of patients showing a decrease in the stage of AKI after onset was slightly higher in the CDS phase but this was not statistically significant (71.4% for the CDS vs. 64.4% for the pre- and 55% for the post-CDS control phases, p = 0.3).
Documentation of AKI in progress notes was less than 50% at baseline, and there was a significant improvement in the CDS phase (74.3% for the CDS vs. 47.5% for the pre- and 57.5% for the post-CDS control phases, p < 0.001) (Table 2, Fig. 3). A significantly higher percentage of patients had intake and output charting ordered and their fluid management changed in the CDS phase, with most receiving a fluid bolus or having the rate of fluid increased (Table 2). Of the patients who were on kidney eliminated and nephrotoxic drugs (KEND), a greater proportion had their medications discontinued or doses adjusted (78.8% for the CDS group vs. 51.6% for the pre- and 56.5% for the post-CDS control groups, p = 0.007). There was a slight increase in the number of consults to the nephrology service for all AKI stages 1–3, though this was not significant. Consults for severe AKI remained fairly consistent at 33–38% across the three phases.
Characteristics at the time of discharge are shown in Table 3. More patients in the CDS phase had their creatinine checked. They also had a higher eGFR than those in the pre- and post-CDS phases, though these were not statistically significant. A greater proportion of patients had complete recovery by discharge and had follow-up labs planned in the alert phase.
Overall, 197 patients (87.5%) were seen in follow-up at the hospital, and of those, 61 (31%) were seen by a nephrologist. The proportion of patients seen by nephrology increased over the three phases (Table 4).
Significant improvements were seen between the baseline phase and CDS phase in AKI documentation (RR = 1.57, 95% CI = 1.18, 2.08), input and output charting (RR = 1.19, 95% CI = 1.03, 1.37), doses adjusted (RR = 2.10, 95% CI = 1.29, 3.41), and nephrotoxic medications stopped (RR = 2.74, 95% CI = 1.30, 5.77). Renal consults did not differ by study phase. The relative risk of AKI documentation, input and output charting, doses adjusted, and nephrotoxic medications stopped did not differ significantly between the pre-and-post-CDS periods (Table 5).
Discussion
This is the first pediatric study in the United States to evaluate the impact of implementation of a CDS system on the progression of AKI in children. This was a small pilot study where we used the existing paging technology within our hospital and paired it with a simple care pathway for the management of AKI. Our study shows that more patients had an improvement in their AKI stage after the alert. This is mediated by a significant increase in the number of interventions including more diligent monitoring of the volume status, change in the amount or type of intravenous fluids, and adjustment of kidney eliminated and nephrotoxic drugs.
In recent years, multiple studies have investigated the potential of information-technology-based interventions to improve outcomes in AKI.12,13,20 Some of the initial studies utilized real-time electronic AKI alerts alone. In one prospective intervention study in the medical and surgical ICU, Colpaert et al.12 looked at the impact of an AKI e-alert on therapeutic interventions and AKI progression. They reported that a higher percentage of patients in the alert group received therapeutic intervention within 60 min after the alert compared to the pre- and post-alert control groups. The interventions included fluid therapy, diuretics, or vasopressors. In another parallel-group, randomized controlled trial, patients were randomly assigned to receive an AKI alert (sent to the covering provider and unit pharmacist) or usual care.13 There was no difference in the primary outcome (a composite of relative maximum change in creatinine, dialysis, and death at 7 days after randomization) between the two groups.
The lack of clear guidelines or actionable interventions has been cited as a reason for the limited success seen with the e-alerts alone. Consequently, studies have tried to incorporate targeted education and standardized care pathways with the e-alert.17,21 Since AKI in the non-ICU setting is often seen and managed by non-nephrologists, having a CDS system that combines the e-alert with a care pathway might improve the management of these patients. In a propensity score-matched cohort of multifactorial AKI, Kolhe et al.17 looked at the impact of compliance with an AKI care bundle on in-hospital case–fatality and AKI progression. In their study, the care bundle was completed in 25.6% of patients within 24 h, and completion of the bundle was associated with lower odds for in-hospital death and lower progression of AKI. Another study by Al-Jaghbeer et al.21 used a CDSS which alerted the clinicians of “possible AKI” based on the changes in SCr. In addition to the alert, it also provided information on the stage of AKI and had a prompt to consult nephrology or intensive care (with corresponding pager numbers provided). They showed a sustained improvement in hospital mortality, dialysis use, and length of stay with the use of this system.21
There are limited data on the use of CDS systems, including e-alerts in children. Using the Welsh National electronic AKI reporting system, Holmes et al.9 reported data on all cases of pediatric AKI over a 30-month period. This study utilized an automated real-time e-alert system for AKI using the KDIGO SCr criteria. Over a 30-month period, there were 1343 incident AKI alerts, with an incidence rate of 1.37 cases per 1000 person-years for those under the age of 18 years. This incident rate was higher than has been previously reported.3,9
To our knowledge, we report the first study to use a CDS system that incorporates an e-alert with a standard care pathway for pediatric AKI. While our primary outcomes did not reach statistical significance, we did see a trend towards decrease in the stage of AKI after onset. In addition, there was better recognition of AKI, and there were more interventions, recommended by the “AEIOU” care pathway, performed for patients with AKI in the alert group. More children in the alert group had their creatinine checked prior to discharge and had a better eGFR at discharge and follow-up. Patients in the pre-alert control group had lower eGFRs at follow-up compared to baseline, suggesting lack of recovery. Additionally, almost 40% of our patients had history of AKI in the previous 6 months. Better recognition and documentation of AKI can lead to improved identification of these patients, which can improve risk stratification on an individual patient basis and personalized approaches for AKI management and follow-up.
We limited our study to a relatively short duration due to the concern of alert fatigue. A longer duration might have provided us more statistical power, and this is certainly a limitation. We were concerned that generating too many or irrelevant alerts could cause fatigue and result in nonacceptance as has been previously reported.22 In a follow-up survey at our center, the providers reported their satisfaction with the alert. This was likely related to the fact that providers only received alerts for patients they were responsible, and hence received only 1–2 during a shift. The alert, as well as the care pathway, was easy to handle and understand.
Our study has several limitations. First, this was a single-center, nonrandomized study. Our study period was spread over 10 months, which can lead to variation in the study population due to seasonal changes in admission patterns. Second, the AKI diagnosis based on SCr and baseline serum creatinine concentration is not always available, particularly in pediatric patients. Serum creatinine was calculated in 17% patients from an eGFR of 120 mL/min/1.73 m2. This can be a source of error but we used this method as it has been commonly used in studies of pediatric AKI.1,18,23 Holmes et al.9 used normative midpoint SCr values for age and sex and compared it with a baseline SCr back-calculated from eGFR of 120 mL/min/1.73 m2. They found that the normative values provided a more accurate reflection of the true baseline value. This method, however, needs to be validated in additional studies. In addition, we used the lowest SCr in the previous 6 months as baseline as has been previously described. We had a 10% false-positive rate due to an incorrectly low baseline in patients who had a history of complicated medical issues and multiple admissions. It is likely that the use of age- and sex-based normative values would mitigate this problem. Third, our center is a part of the Nephrotoxic Injury Negated by Just-in time Action (NINJA) quality improvement program, which is a multicenter collaborative to reduce the rates of nephrotoxic medication-associated AKI in the non-ICU population.24 However, we do not think there would have been significant interaction between the two projects as the NINJA study focused on patients receiving 3+ nephrotoxic medications simultaneously or an IV aminoglycoside for 3+ consecutive days, and recommends daily SCr monitoring for those patients. This study recognized all patients with AKI, irrespective of cause.
Going forward, to keep this system sustainable, we would need an ongoing AKI education program for pediatric residents. We believe our “AEIOU” method is simple to remember and a good place to start. We saw in our study that the improvements seen in AKI documentation, medication adjustments, and follow-up go away with the discontinuation of the e-alert system. Ongoing attention to AKI on the floor will require a careful, ongoing AKI program. The AKI alert system would also require periodic random sampling and adjudication by 1–2 physicians involved in the program. One of the keys to avoiding alert fatigue is to minimize false-positive alerts. The alerts are currently set to be interruptive (pager based). As AKI awareness and education improves, it may be possible to switch to a noninterruptive alert (as a notification in the patient’s EHR).
In conclusion, we show that the use of a CDS system that incorporates an e-alert with a standard care pathway improves the recognition of AKI and interventions performed for it. While we did not see a significant improvement in the progression of AKI in our pilot study, we believe this is an important step in improving the outcomes of children with AKI. With refinement of our e-alert in the future and with more education of providers, we may be able to initiate earlier management of children with AKI. While there are no proven therapies for AKI yet, better identification and risk stratification will allow us to personalize care for patients with AKI.
Data availability
The study was registered at ClinicalTrials.gov under the name “AKI Management Using Electronic Alerts”, number NCT03538769.
References
Kaddourah, A., Basu, R. K., Bagshaw, S. M., Goldstein, S. L. & AWARE Investigators. Epidemiology of acute kidney injury in critically ill children and young adults. N. Engl. J. Med. 376, 11–20 (2017).
Jetton, J. G. et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc. Health 1, 184–194 (2017).
Sutherland, S. M. et al. AKI in hospitalized children: epidemiology and clinical associations in a national cohort. Clin. J. Am. Soc. Nephrol. 8, 1661–1669 (2013).
McGregor, T. L. et al. Acute kidney injury incidence in noncritically ill hospitalized children, adolescents, and young adults: a retrospective observational study. Am. J. Kidney Dis. 67, 384–390 (2016).
Hessey, E. et al. Healthcare utilization after acute kidney injury in the pediatric intensive care unit. Clin. J. Am. Soc. Nephrol. 13, 685–692 (2018).
Hessey, E., Perreault, S., Dorais, M., Roy, L. & Zappitelli, M. Acute kidney injury in critically ill children and subsequent chronic kidney disease. Can. J. Kidney Health Dis. 6, 2054358119880188 (2019).
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. 2, (Suppl) 1−138 (2012).
Chertow, G. M., Burdick, E., Honour, M., Bonventre, J. V. & Bates, D. W. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J. Am. Soc. Nephrol. 16, 3365–3370 (2005).
Holmes, J. et al. The incidence of pediatric acute kidney injury is increased when identified by a change in a creatinine-based electronic alert. Kidney Int. 92, 432–439 (2017).
Sutherland, S. M. et al. Utilizing electronic health records to predict acute kidney injury risk and outcomes: workgroup statements from the 15(th) ADQI Consensus Conference. Can. J. Kidney Health Dis. 3, 11-016-0099-4 (2016). eCollection 2016.
Hoste, E. A. et al. Impact of electronic-alerting of acute kidney injury: workgroup statements from the 15(th) ADQI Consensus Conference. Can. J. Kidney Health Dis. 3, 10-016-0101-1 (2016). eCollection 2016.
Colpaert, K. et al. Impact of real-time electronic alerting of acute kidney injury on therapeutic intervention and progression of RIFLE class. Crit. Care Med. 40, 1164–1170 (2012).
Wilson, F. P. et al. Automated, electronic alerts for acute kidney injury: a single-blind, parallel-group, randomised controlled trial. Lancet 385, 1966–1974 (2015).
Wilson, F. P. & Greenberg, J. H. Acute kidney injury in real time: prediction, alerts, and clinical decision support. Nephron 140, 116–119 (2018).
Goldstein, S. L. Automated/integrated real-time clinical decision support in acute kidney injury. Curr. Opin. Crit. Care 21, 485–489 (2015).
Goldstein, S. L. et al. Electronic health record identification of nephrotoxin exposure and associated acute kidney injury. Pediatrics 132, e756–e767 (2013).
Kolhe, N. V. et al. A simple care bundle for use in acute kidney injury: a propensity score-matched cohort study. Nephrol. Dial. Transpl. 31, 1846–1854 (2016).
Zappitelli, M. et al. Ascertainment and epidemiology of acute kidney injury varies with definition interpretation. Clin. J. Am. Soc. Nephrol. 3, 948–954 (2008).
Kirkendall, E. S. et al. Development and performance of electronic acute kidney injury triggers to identify pediatric patients at risk for nephrotoxic medication-associated harm. Appl. Clin. Inf. 5, 313–333 (2014).
Holmes, J. et al. Utility of electronic AKI alerts in intensive care: a national multicentre cohort study. J. Crit. Care 44, 185–190 (2018).
Al-Jaghbeer, M., Dealmeida, D., Bilderback, A., Ambrosino, R. & Kellum, J. A. Clinical decision support for in-hospital AKI. J. Am. Soc. Nephrol. 29, 654–660 (2018).
Wilson, F. P. Information technology and acute kidney injury: alerts, alarms, bells, and whistles. Adv. Chronic Kidney Dis. 24, 241–245 (2017).
Menon, S. et al. Urinary biomarker incorporation into the renal angina index early in intensive care unit admission optimizes acute kidney injury prediction in critically ill children: a prospective cohort study. Nephrol. Dial. Transpl. 31, 586–594 (2016).
Goldstein, S. L. et al. A prospective multi-center quality improvement initiative (NINJA) indicates a reduction in nephrotoxic acute kidney injury in hospitalized children. Kidney Int. 97, 580–588 (2020).
Acknowledgements
There was no external funding for this project. Internal funding was provided by the Division of Nephrology, Seattle Children’s Hospital.
Author information
Authors and Affiliations
Contributions
S.M. and K.Y. conceptualized and designed the study, collected the data, drafted the initial manuscript, and reviewed and revised the manuscript. K.C. designed the data collection instruments, carried out the initial analyses, and reviewed and revised the manuscript. H.W. designed the study, created the clinical decision support tool (e-alert), designed data collection tools, reviewed and revised the manuscript. R.T. conceptualized and designed the study, and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent
The study was approved by the Seattle Children’s Hospital Institutional Review Board with waiver of informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Menon, S., Tarrago, R., Carlin, K. et al. Impact of integrated clinical decision support systems in the management of pediatric acute kidney injury: a pilot study. Pediatr Res 89, 1164–1170 (2021). https://doi.org/10.1038/s41390-020-1046-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-1046-8
- Springer Nature America, Inc.
This article is cited by
-
Utilizing electronic medical records alert to improve documentation of neonatal acute kidney injury
Pediatric Nephrology (2024)
-
A proposed framework for advancing acute kidney injury risk stratification and diagnosis in children: a report from the 26th Acute Disease Quality Initiative (ADQI) conference
Pediatric Nephrology (2024)
-
Pediatric AKI in the real world: changing outcomes through education and advocacy—a report from the 26th Acute Disease Quality Initiative (ADQI) consensus conference
Pediatric Nephrology (2024)
-
Patient level factors increase risk of acute kidney disease in hospitalized children with acute kidney injury
Pediatric Nephrology (2023)
-
Integrated care for children living with complex care needs: an evolutionary concept analysis
European Journal of Pediatrics (2023)