Abstract
Mitochondrial pyruvate carrier 1 (MPC-1) appears to be a tumor suppressor. In this study, we determined the regulation of MPC-1 expression by Lysine demethylase 5A (KDM5A) and critical impact of this novel KDM5A/MPC-1 signaling on PDA progression. TCGA database, paired PDA and adjacent normal pancreatic tissues, PDA tissue array and cell lines were used to determine the levels of MPC-1 and KDM5A expression, and their relationship with the clinicopathologic characteristics and overall survival (OS) of PDA patients. Both in vitro and in vivo models were used to determine biologic impacts of MPC-1 and KDM5A on PDA and mitochondrial pyruvate metabolism, and the mechanism underling reduced MPC-1 expression in PDA. The expression of MPC-1 was decreased in PDA cell lines and tissues, and negatively associated with tumor poorer differentiation, lymph nodes metastasis, higher TNM stages, and patients’ overall survival (OS). Functional analysis revealed that restored expression of MPC-1 suppressed the growth, invasion, migration, stemness and tumorigenicity. Re-expression of MPC-1 stimulated the mitochondrial pyruvate metabolism and inhibited glycolysis, while MPC-1-specific inhibitor UK5099 attenuated these effects. Furthermore, KDM5A bound directly to MPC-1 promoter region and transcriptionally suppressed the expression of MPC-1 via demethylation H3K4. Consistently, KDM5A expression was elevated in PDA and promoted PDA cell proliferation in vitro and tumor growth in vivo via suppressing the expression of MPC-1. The expression of KDM5A was inversely correlated with that of MPC-1 in PDA. KDM5A/MPC-1 signaling promoted PDA growth, invasion, migration, and stemness via inhibiting mitochondrial pyruvate metabolism. Targeting KDM5A/MPC-1 signaling may be an effective therapeutic strategy for PDA.
Similar content being viewed by others
Introduction
Pancreatic ductal adenocarcinoma (PDA), the most common type of pancreatic malignancy, is a deadly disease and its 5-year survival rate is about 8% [1, 2]. Alarmingly, the incidence and death in PDA is a consistent rise and it has been estimated that PDA would be the second leading cause of cancer-related death by 2030 [3]. It has been reported that activating KRAS mutation and loss of function of CDKN2A, TP53, and SMAD4 tumor suppressors play critical roles in PDA development and progression [4]. Although recently, many studies have tried to identify the subtypes of PDA, the result could hardly be used in clinic and few readily “druggable” targets has been identified in PDA [5, 6]. Thus, there is an urgent need to study the molecular mechanism of PDA development and progression, and identify new targets for the treatment of PDA.
“Warburg effect”, the root of cancer development and progression, has been first reported almost 100 years ago that cancer cells tends to glycolysis, but not fully oxidize the pyruvate [7]. This was originally proposed to be the result of absent or dysfunctional mitochondria. However, it has been increasingly clear that mitochondria remain functional and crucial in most cancer cells, as essential steps in the biosynthesis of nucleotide, amino acids, and lipid occur therein [8,9,10,11]. The critical step of oxidative phosphorylation is import of pyruvate into the mitochondrial matrix. However, the mechanism of decreased pyruvate in mitochondrion was difficult to demonstrate until recently two groups discovered the mitochondrial pyruvate carrier (MPC), which was assembled with the two proteins MPC1 and MPC2 [12, 13]. This complex is necessary and sufficient for pyruvate import into mitochondrion and serves as the junction between cytoplasmic glycolysis and mitochondrial oxidative phosphorylation. Rutter, J’s group has showed that the expression of MPC1 was decreased in many types of cancers, which led to decreased expression and activity of the MPC and promoted colon cancer cells to form colonies in vitro and tumors in vivo [14]. Furthermore, their group reported that decreased expression of MPC1 controlled the intestinal stem cell function and proliferation via mitochondrial pyruvate metabolism [15]. Recently, a series of studies have published to demonstrate the roles of MPC1 in prostate cancer, esophageal squamous cell carcinomas, and liver cancer [16, 17]. However, the roles and mechanisms of MPC-1 expression in PDA development and progression are unknown.
Histone methylation is one of the important histone modifications that play key roles in controlling gene expression via methyltransferases and demethylases. A number of histone lysine demethylases (KDMs) has been identified recently and were reported to have critical roles in PDA [18,19,20]. Lysine demethylase 5A (KDM5A), also known as JARID1A or RBP2, is a newly found jumonji domain-containing demethylase for H3 lysine 4 (H3K4) trimethylation and demethylation [21]. KDM5A has been reported to control differentiation and mitochondrial metabolism [22,23,24]. Moreover, in study from Bardeesy group, KDM5A was overexpressed in PDA by meta-analysis of SAGE data and formed a complex with KDM2B, which was required for the maintenance of a metabolic gene signature [19]. However, the mechanism of KDM5A in promoting PDA development and progression still needs elucidating.
In the present study, we showed that the expression of MPC-1 decreased in PDA, and restored expression of MPC-1 suppressed PDA progression via increasing mitochondrial pyruvate metabolism. Furthermore, KDM5A transcriptionally suppressed the expression of MPC-1 by H3K4me3 demethylation in PDA. Thus, this novel KDM5A/MPC-1 signaling pathway critically regulates the PDA progression.
Results
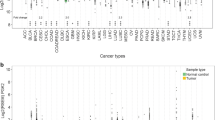
Reduced expression of MPC-1 directly associated with pathologic features in PDA
To determine the role of MPC expression in PDA pathogenesis, we first investigated the messenger RNA (mRNA) expression level of MPC-1 and MPC-2 in TCGA database on the website of SurvExpress [1]. As shown in Supplementary Fig. S1B, D, the gene expression levels of MPC-1 and MPC-2 were significantly higher in low-risk groups as grouped prognostic index (P = 5.91e-36 and P = 2.61e-36, respectively). Survival analysis showed that elevated expression of MPC-1 on low-risk group had longer survival time (P = 0.02754, Log-rank test, Supplementary Fig. S1A). However, elevated expression of MPC-2 on low-risk group didnot significantly associate with longer survival time (P = 0.1131, Log-rank test, Supplementary Fig. S1C). We then tested the mRNA levels of MPC-1 and MPC-2 in 14 paired PDA and adjacent normal pancreatic tissues using real-time PCR. The mRNA levels of MPC-1 were significantly lower in PDA tissues in 12 of 14 cases (Fig. 1a, *P < 0.05), however, the levels of MPC-2 were lower in PDA samples in 4 of 14 cases (Fig. 1b, *P < 0.05). The result was consistent with Jared Rutter group’s study that the expression of MPC-1 might be more important in MPC, and the expression of MPC-2 was greatly varied in differently types of cancer [14]. We then focused our study on MPC-1 and analyzed the protein levels of MPC-1 in PDA tissue array via IHC. With a specific anti-MPC-1 antibody, we observed MPC-1-positive staining in the cytoplasm of adjacent normal pancreatic tissue and some cancer tissues, and it showed a decreasingly positive staining activity of MPC-1 among cancer tissues (Fig. 1c, d). The decreased expression of MPC-1 was positively associated with tumor poorer differentiation (Fig. 1e, f and Supplementary Table S1), lymph nodes metastasis (Supplementary Table S1), and higher TNM stages (Fig. 1g, h and Supplementary Table S1). Kaplan–Meier analysis and log-rank test were used to investigate the prognostic value of MPC-1 expression and classic clinicopathologic characteristics on patient survival. In univariate analysis, MPC-1 was closely associated with overall survival (OS) of PDA patients (P < 0.001; Fig.1i and Supplementary Tables S2 and S3). Univariate analysis also indicated that tumor differentiation, lymph nodes metastasis and clinical stages correlated with patient OS (P = 0.033, P = 0.002, and P = 0.001, respectively. Supplementary Table S3). Multivariate analysis showed that MPC-1, tumor differentiation, lymph nodes metastasis, and clinical stages were independent prognostic factors for PDA patients (Supplementary Table S3).
Expression of MPC-1 in and its association with clinicopathologic features of PDA. a, b mRNA was extracted from 14 paired PDA and adjacent normal pancreatic tissues for quantitative PCR analysis (*P < 0.05). TMA PDA specimens were immunostained with a specific anti-MPC-1 antibody. c Representative images of MPC-1 expression in PDA specimens and adjacent normal pancreatic tissue specimens were shown. Shown was markedly high MPC-1 expression in adjacent normal (Normal, left panel), high MPC-1 expression in tumor tissue (Tumor-1, middle panel) and low MPC-1 expression in tumor tissue (Tumor-2, right panel). d The expression of MPC-1 was significantly lower in tumors (TT) than in adjacent normal tissue (TN) (left panel, P = 0.002, χ2 test), and the percentage of high and low expression of MPC-1 in TT and TN were also provided (right panel). e Representative images of high MPC-1 expression in well and moderate differentiation tissues (upper panel) and low MPC-1 expression in poor differentiation tissues. f Negative association of the expression of MPC-1 with tumor differentiation (upper panel, P < 0.001, χ2 test), and the percentage of high and low expression of MPC-1 in well and poor differentiation were also provided (lower panel). g Representative images of high MPC-1 expression in early stages of PDA tissues (upper panel) and low MPC-1 expression in late stages of PDA tissues (lower panels). h Negative association of the expression of MPC-1 with tumor clinical stages (upper panel, P < 0.001, χ2 test), and the percentage of high and low expression of MPC-1 in early and advanced stages were also provided (lower panel). i the expression of MPC-1 was positively associated with OS of PDA patients. j, k verification of the expression of MPC-1 protein in PDA cell lines and paired normal pancreas tissues and PDA tissues by western blot
We then confirmed the protein levels of MPC-1 in three-paired PDA and adjacent normal pancreatic tissues, and cancer cell lines via western blot. The levels of MPC-1 were obviously lower in PDA tissues and cancer cell lines (Fig. 1j, k). These findings indicated that lost expression of MPC-1 played critical roles in PDA and might be a valuable biomarker for this disease.
Impact of MPC-1 expression on PDA cancer cell biology
To assess the impact of MPC-1 expression on PDA cancer cell biology, we infected PANC-1, BxPC-3, and AsPC-1 cells, which have very low or intermediate levels of endogenous MPC-1 expression, with retroviruses containing MPC-1 (PANC-1/BxPC-3/AsPC-1-pMPC-1) and empty retroviral expression vectors used as controls (PANC-1/BxPC-3/AsPC-1-pControl). After selection of the infected cells with puromycin, we found the pooled drug-resistant cells to had elevated levels of MPC-1 expression (Fig. 2a). Moreover, re-expression of MPC-1 also led to increased expression of MPC-2, which was also consistent with Jared Rutter group’s study, as MPC-1 and MPC-2 generated MPC complex, which was much more stable (Fig. 2a) [14]. We then tested the effect of re-repression of MPC-1 on PDA cell proliferation in vitro. As shown in Fig. 2b, restored expression of MPC-1 had limited effect on the proliferation of PANC-1 and BxPC-3 cells via colony formation assay, which was also consistent with Jared Rutter group’s study. We then tested the role of MPC-1 in PDA cell spheroid formation. The re-expression of MPC-1 significantly decreased the number and size of the first and second generations of spheroids in both PANC-1 and BxPC-3 cell lines (Fig. 2c, d). We then further determined the effect of re-expressed MPC-1 on PDA growth in vivo. We found that restored expression of MPC-1 markedly suppressed tumor growth (Fig. 2e–g). It has been reported that MPC-1 expression controls cancer epithelial–mesenchymal transition (EMT), and also MPC-1 could interact with signal transducer and activator of transcription 3 (STAT3) pathway, and lead to a decreased expression of SOX2, and inhibit cancer proliferation and invasion [25, 26]. We then further confirmed the expression of MPC-1, the proliferative marker Ki-67 positivity, and SOX2 with xenograft tumors. As revealed by western blot analyses, overexpression of MPC-1 led to an increased expression of MPC-1, but decreased expression of Ki-67 and SOX2 in vivo (Supplementary Fig. S2).
Impact of MPC-1 expression on PDA cancer cell biology. a PANC-1, BxPC-3, and AsPC-1 cells were infected with retroviruses and stably overexpressed MPC-1 (Mock, pControl = pBABEpuro, pMPC-1 = pBABE-MPC-1). b Colony formation assay was performed with PANC-1 and BxPC-3 cells in 24-well plates, and numbers of colonies were counted 14 days after. c, d Spheroid colony formation assay were performed with PANC-1 and BxPC-3 cells, and restored expression of MPC-1 decreased the number and size of the first and second generations of spheroids (*P < 0.05). PANC-1 cells with restored expression of MPC-1 were injected subcutaneously (1 × 106 per mouse, n = 5) into the right and left scapular region of the nude mice. The tumor-bearing mice were sacrificed when they became moribund or on day 35. e Shown was the representative photo of mouse and gross tumors in the mice. f The tumor volume of resulting tumors in each group was measured once a week (*P < 0.05). g The weight of the tumors was measured
It has been reported that during impaired mitochondrial pyruvate transport, the glutamine oxidation maintains the cell survival. Furthermore, also the in vivo tumors were lack of oxygen. Thus, we further tested the roles of MPC-1 in PDA cell biology under hypoxia and without glutamine supplementary in vitro [27]. As shown in Fig. 3a, b, re-expressed MPC-1 significantly suppressed the growth and colony formation of PANC-1 and BxPC-3 cells (*P < 0.05). Similarly, restored MPC-1 expression suppressed the migration and invasion of PANC-1 and BxPC-3 cells (*P < 0.05) (Fig. 3c, d). Collectively, these data clearly demonstrated that MPC-1 suppressed the growth, migration, invasion, stemness, and tumorigenicy of PDA, and supporting that MPC-1 might function as a tumor suppressor for PDA.
Impact of MPC-1 on PDA proliferation, invasion, and migration under hypoxia and without glutamine supplementary. PANC-1 and BxPC-3 cells with restored expression of MPC-1 were cultured under hypoxia (1% oxygen) condition without glutamine supplement. a Cell growth was assessed via cell counting at the indicated time points (*P < 0.05). b Colony formation assay was performed in 24-well plates (mean ± SD; *P < 0.05). c, d The migration and invasion of PANC-1 and BxPC-3 cells were determined as described in Supplementary Materials and Methods. Representative tumor cell migrated or invaded were photographed, data represent mean ± SD of triplicates (*P < 0.05)
Restored expression of MPC-1 stimulated the mitochondrial pyruvate metabolism and inhibited glycolysis
MPC-1 is the key subunit of MPC, thus, we sought to assess the metabolic effects of MPC-1 re-expression by focusing on PANC-1 and BxPC-3 cell lines. As shown in Fig. 4a, b, re-expression of MPC-1 significantly increased the pyruvate concentration in mitochondria and reduced the lactic secretion in media. Furthermore, treated cells with MPC-1-specific inhibitor UK5099 significantly attenuated the stimulated effect of MPC-1 in mitochondrial pyruvate concentration and inhibitory effect of MPC-1 in lactate production. To further demonstrate the effect of MPC-1 on glycolysis, we test the utilization of glucose in different MPC-1 expression level and activity. As shown in Fig. 4c, re-expressed MPC-1 decreased the consumption of glucose, meanwhile UK5099 increased the glucose consumption of PDA cells and attenuated the inhibitory effect of MPC-1 on glucose consumption. As mitochondrial pyruvate carrier, MPC plays critical roles in transporting and promoting the oxidative phosphorylation of pyruvate. Thus, we further analyzed the effect of re-expressing MPC-1 on the expression of enzymes that were relevant to pyruvate metabolism. We implemented these experiments on both cancer cell lines and subcutaneous tumors in xenograft assays in nude mice. Both in PANC-1 and BxPC-3 cells and xenograft tumors, restored expression of MPC-1 had limited effect on the abundance of LDHA, PKM1, PDK, and PDH, but led to decreased expression PKM2, which was important for the promotion of aerobic glycolysis (Fig. 4d). Collectively, this data demonstrated that re-expression of MPC-1 altered mitochondrial pyruvate metabolism.
Effect of MPC-1 on the mitochondrial pyruvate metabolism and glycolysis. PANC-1 and BxPC-3 cells with restored expression of MPC-1 were cultured under hypoxia (1% oxygen) condition without glutamine supplement. MPC-1-specific inhibitor UK5099 (40 µM) treated the cells as indicated. a–c The mitochondrial pyruvate concentration, lactate levels in the extracellular media, and glucose consumption in each group were tested as described in Materials and Methods. d Western blots analyzed the expression of MPC-1, MPC-2, LDHA, PKM1, PKM2, PDK, and PDH in control and MPC-1 restored expression groups in cells and subcutaneous tumors in the mice (β-actin as internal control)
KDM5A demethylates H3K4 and transcriptionally suppressed the expression of MPC-1
We further study the mechanism of decreased expression of MPC-1 in PDA. We analyzed the MPC-1 gene in TCGA database and found that the mutation of MPC-1 was rare in PDA (data not show). We then analyzed the promoter region of MPC-1 gene and found that the promoter of MPC-1 was rich in CpG islands (Supplementary Fig. S3A). Methylation-specific PCR was further performed to test whether PDA cells were exhibited DNA hypermethylation in the promoter region of MPC-1. However, the DNA of the promoter region of MPC-1 was not hypermethylation in most PDA cell lines, except for MiaPaca-2 cells (Supplementary Fig. S3B). Therefore, promoter DNA hypermethylation might only contribute to suppressed MPC-1 expression in a small subset of PDA cases.
In a study from Bardeesy group [19], the ChiP-seq result revealed that MPC-1 was a downstream target of KDM2B and EZH2, but not KDM5A. However, in the study from Benevolenskaya group [28], the ChiP-seq result showed that MPC-1 was the downstream target of KDM5A. We then knocked down KDM2B and EZH2 in PANC-1 and BxPC-3 cell lines. Decreased expression of KDM2B resulted in increased expression of MPC-1, while suppressed expression of EZH2 had little effect on MPC-1 (Fig. 5a). Furthermore, knocked down of KDM5A also led to increased expression of MPC-1 in both mRNA and protein levels (Fig. 5c, d). It has been reported that KDM2B regulated the levels of KDM5A [19]. We then tested the effect of KDM2B and KDM5A on the expression of MPC-1 in PDA. As shown in Fig. 5e, knocked down both of KDM2B and KDM5A resulted in further increased expression of MPC-1, while overexpression of KDM5A attenuated the effect of knockdown of KDM2B on MPC-1 and even further decreased MPC-1. These results revealed that the effect of KDM2B on MPC-1 might via KDM5A. Furthermore, the result of ChIP assay revealed that KDM5A but not KDM2B directly bound to the promoter region of MPC-1 (Fig. 5b). KDM5A is a newly found demethylase for H3K4 trimethylation and dimethylation, and H3K4me3 is often the sign of activation of genes [29]. In our study, H3K4me3 and H3K4me2 were both existed in MPC-1 promoter region, and knocked down of KDM5A indeed led to increased levels of H3K4me3, which activated the transcription of MPC-1 (Fig. 5b, d). It has been reported that KDM5A contained an AT-rich interaction domain usually binding to the 5ʹ-CCGCCC-3ʹ motif of genes’ promoter [30]. We then analyzed the promoter region of MPC-1 and found that several 5ʹ-CCGCCC-3ʹ motifs were existed (Fig. 5f). We then generated MPC-1 promoter reporter pMPC-1-773 and two deletion mutants pMPC-1-604 and pMPC-1-332 (Fig. 5f, left panel). To determine if KDM5A regulates MPC-1 expression at the transcriptional level, we co-transfected the prompter reporters with or without shKDM5A into PANC-1 and BxPC-3 cells. As shown in Fig. 5f, middle and right panel, shKDM5A increased the transcriptional activity of all reporters. These results demonstrated that MPC-1 was a direct downstream target of KDM5A, which regulated the expression of MPC-1 at the transcriptional level via demethylating H3K4 for trimethylation.
KDM5A transcriptionally regulated the expression of MPC-1. a KDM2B and EZH2 shRNAs and control vectors were transfected into PANC-1 and BxPC-3 cells. Western blots analyzed the expression of KDM2B, EZH2, and MPC-1 (β-actin as internal control). b Chromatins were isolated from PANC-1 and BxPC-3 cells and binding of KDM2B (2B), H3K4me2 (m2), H3K4me3 (me3), KDM5A (5A), and negative control water (W) to the MPC-1 promoter was determined using ChIP assay as described in Materials and Methods. PDA cells lines were transfected with KDM5A shRNA and control vectors, and the cultures were incubated for 120 h. c Total RNA was harvested for the determination of the levels MPC-1 via quantitative real-time PCR (normalized to β-actin). d PANC-1 and BxPC-3 cell protein lysates were harvested, and western blot was used to test the levels of KDM5A, MPC-1, H3K4me3, H3K4me2, and total H3 (β-actin as internal control). e shRNAs of KDM2B and KDM5A, KDM5A overexpression vector (pKDM5A) and control vectors were transfected into PANC-1 cells alone or combining as indicated. The protein levels of KDM2B, KDM5A, and MPC-1 were analyzed using western blot (β-actin as internal control). f Constructions of MPC-1 promoter reporter and its deletion mutants (pLuc-MPC-1-773, pLuc-MPC-1-604, and pLuc-MPC-1-332). PANC-1 and BxPC-3 cells were co-transfected with 0.2 µg of the MPC-1 promoter luciferase constructs pLuc-MPC-1 and 0.2 µg of KDM5A shRNA or control vector. Promoter activity was examined using a dual luciferase assay kit (*P < 0.05)
The elevated expression of KDM5A directly correlated with PDA progression and negatively associated with MPC-1 expression
We have provided evidence that KDM5A transcriptionally suppressed MPC-1 expression. To further confirm our hypothesis, we also investigated the mRNA level of KDM5A in TCGA database on the website of SurvExpress. We found that KDM5A level was significantly higher in high-risk group as grouped prognostic index (P = 8.05e-31, Supplementary Fig. S4A). Survival analysis showed that increased expression of KDM5A in high-risk group has shorter survival time (P = 0.02962, Log-rank test, Supplementary Fig. S4B). We then analyzed the protein level of KDM5A in the serial PDA tissue array of MPC-1 using IHC. We observed KDM5A mainly positive staining in the nucleus of cancer tissues, but negative or weak expression in the adjacent normal tissues (Fig. 6a, b). Furthermore, the increased expression of KDM5A was positively associated with tumor poorer differentiation, lymph nodes metastasis, and higher TNM stages (Supplementary Table S2). Kaplan–Meier analysis and log-rank test were used to investigate the prognostic value of KDM5A expression on PDA patient survival. In univariate analysis, KDM5A was closely associated with OS of PDA patients (P < 0.001; Fig. 6c and Supplementary Table S3). Multivariate analysis showed that KDM5A was also an independent prognostic factor for PDA patients (Supplementary Table S3).
The expressions of KDM5A related to PDA progression and MPC-1. TMA PDA specimens were immunostained with a specific anti-KDM5A antibody. a Representative images of KDM5A expression in PDA specimens and adjacent normal pancreatic tissue specimens were shown. Shown was markedly low KDM5A expression in adjacent normal (Normal, left panel), low KDM5A expression in tumor tissue (Tumor-1, middle panel) and high KDM5A expression in tumor tissue (Tumor-2, right panel). b The expression of KDM5A was significantly higher in tumors (TT) than in adjacent normal tissue (TN). c The expression of KDM5A was negatively associated with the OS of PDA patients. PANC-1 and BxPC-3 cells were infected with retroviruses and stably knocked of KDM5A (shKDM5A and shControl). Colony formation assay was performed with PANC-1 and BxPC-3 cells in 24-well plates (mean ± SD; *P < 0.05). PANC-1 cells with shControl or shKDM5A were injected subcutaneously (1 × 106 per mouse, n = 5) into the right and left scapular region of the nude mice. The tumor-bearing mice were sacrificed when they became moribund or on day 35. e Shown was representative photo of gross tumors in the mice (the magnification of the control group was 10:1, and the magnification of the shKDM5A group was 14:1). f The weight of the tumors was measured. g Western blot was used to test the levels of KDM5A and MPC-1 in gross tumors (C = shControl, K = shKDM5A, and β-actin as internal control). h, i KDM5A and MPC-1 protein expression TMA tissue sections were represented from the cohort described in Figs. 1c and 6a. Negative correlation of KDM5A with MPC-1 expression was assessed using Pearson correlation coefficient analysis (n = 100; r = −0.391, P < 0.001)
Although there were a series of studies about KDM5A, the roles of KDM5A in PDA biology was not fully demonstrated. We knocked down KDM5A in PANC-1 and BxPC-3 cell lines. The results of colony formation assay and mice subcutaneous transplanted model revealed that decreased expression of KDM5A inhibited PDA cells proliferation in vitro and growth in vivo (Fig. 6d–f). We further confirmed the regulatory effect of KDM5A on MPC-1 in vivo with the subcutaneous tumors. As the result of western bolt, knocked down of KDM5A led to increased expression of MPC-1 in vivo (Fig. 6g). We then tested whether KDM5A had any effect on PDA biology and mitochondrial pyruvate metabolism via regulating MPC-1. As shown in Supplementary Fig. S5, under hypoxia and without glutamine supplementary in vitro, knockdown of KDM5A inhibited PANC-1 proliferation, invasion and migration. However, MPC-1 inhibitor UK5099 significantly attenuated the effect of knocking down KDM5A on PANC-1. Furthermore, knocked down of KDM5A significantly increased the pyruvate concentration in mitochondria, reduced the lactic secretion in media, and decreased consumption of glucose. Combining restored expression of MPC-1 with suppressed expression of KDM5A could not further promote mitochondrial pyruvate metabolism and inhibited glycolysis than knocking down KDM5A, but MPC-1 inhibitor UK5099 significantly attenuated the effect of knocking down KDM5A on metabolism (Supplementary Fig. S6A–S6D, S6F, and S6G). These data demonstrated that KDM5A regulated metabolism at least partly through transcriptionally inhibiting MPC-1 expression. We then further analyzed the correlated expression of MPC-1 and KDM5A with the same cohort. As shown in Fig. 6h, i, direct negative correlation between KDM5A and MPC-1 expression was found in PDA tissues (r = −0.391, P < 0.001).
Discussion
In the present study, we provided six lines of evidence to define the critical roles of the KDM5A/MPC-1 signaling in PDA mitochondrial pyruvate metabolism and progression. First, we revealed that the expression of MPC-1 was decreased in PDA cell lines and tissues, and negatively associated with tumor poorer differentiation, lymph nodes metastasis, higher TNM stages, and patients’ OS. MPC-1 was an independent prognostic factor for PDA patients. These results indicated that MPC-1 might be a valuable biomarker for PDA. Second, restored expression of MPC-1 suppressed the growth, invasion, migration, and cell spheroid formation of PDA in vitro and tumor growth in vivo. Third, restored expression of MPC-1 stimulated the mitochondrial pyruvate metabolism and inhibited glycolysis via increasing mitochondrial pyruvate concentration and decreasing lactate levels in the extracellular media and glucose consumption. Furthermore, MPC-1-specific inhibitor UK5099 attenuated the effect. Forth, the promoter region of MPC-1 contains CpG islands. However, the main mechanism of decreased expression of MPC-1 in PDA was not DNA methylation, but the demethylation of H3K4 of MPC-1 promoter by KDM5A. Fifth, KDM5A directly bound to the promoter of MPC-1, suppressed the promoter activity of MPC-1 and transcriptionally inhibited the MPC-1 expression. Sixth, elevated expression of KDM5A was investigated in PDA and promoted PDA cell proliferation in vitro and tumor growth in vivo via suppressing the expression of MPC-1. Additionally, the expression of KDM5A was inversely correlated with that of MPC-1 in PDA specimens. Collectively, these findings demonstrated a novel KDM5A/MPC-1 signaling controlled pancreatic cancer progression via mitochondrial pyruvate metabolism.
About 50 years ago, a study made a hypothesis that cells contained mitochondrial pyruvate carriers that assisted pyruvate entry the mitochondrial matrix [31]. However, the carrier was not identified till 2012. Two groups reported that two paralogous subunits, MPC1 and MPC2, were expressed in mammals and formed multimeric MPC complex mounting in the inner mitochondrial membrane and controlled pyruvate transportation [12, 13]. Studies revealed that MPC-1 was the key subunit in the MPC complex and mutations or lack expression of MPC-1 caused illness, including hyperpyruvatemia, lactic acidosis, and other severe diseases in humans [12, 32]. Recently, it has been reported that the decreased expression of MPC-1 played critical roles in colon cancer, ovarian cancer, esophageal squamous cell carcinomas, and prostate cancer development and progression via regulating mitochondrial pyruvate metabolism and glycolysis [15,16,17, 33]. Furthermore, MPC-1 was crucial for cancer stem cell maintenance [15, 16]. However, the roles of MPC-1 in PDA development and mechanism of regulating MPC-1 expression have not been studied.
In our study, we focused on the key MPC subunit MPC-1 and tested the expression of MPC-1 in both mRNA and protein levels with multiple methods, including TCGA database, paired PDA and adjacent normal pancreatic tissues, PDA tissue array and cell lines, and demonstrated that MPC-1 was decreased expression in and an independent prognostic factor for PDA. This result was consistent with Jared Rutter’s study that analyzed the expression of MPC-1 in Oncomine database. All these data indicated a valuable biomarker of MPC-1 for PDA. Furthermore, Jared Rutter’s study revealed that restored expression of MPC-1 did not change the proliferation, apoptosis, or necrosis of colon cancer cells in vitro, but inhibited colony formation and tumor growth in vivo [15]. Our study found that the expression levels of MPC-2 were also slightly increased in the MPC-1 restored groups, which might due to the stability of MPC complex [14]. Furthermore, the proliferation of PDA in vitro was not affected but the sphere formation and xenograft growth in vivo was suppressed. In another research, it has been demonstrated that glutamine oxidation could maintain the TCA cycle and cell survival with MPC deficiency and furthermore the in vivo tumors grew in a hypoxia condition [27]. We then further found that restored expression of MPC-1 in PDA inhibited cell proliferation, invasion and migration in vitro under the condition of hypoxia (1% oxygen) and without glutamine supplement. These results revealed that re-expression of MPC-1 suppressed PDA progression via inhibiting growth, metastasis, and stemness of PDA cells. Ki-67 is a typical biomarker of cell proliferation. We tested the effect of MPC-1 expression on Ki-67 positivity in xenograft tumors. The results showed that overexpression of MPC-1 led to a decreased expression of Ki-67. These results further confirmed that restored expression of MPC-1 inhibited PDA cell proliferation. Indeed, knockdown of MPC-1 expression promoted colon cancer EMT; and MPC-1 interacted with mito-STAT3, and disrupted STAT3 pathway, and further led to decreased expression of SOX2, and inhibited lung cancer proliferation and invasion [25, 26]. We then further tested, investigated the effect of restored expression of MPC-1 on SOX2 in xenograft tumors. The results showed that overexpression of MPC-1 led to a decreased expression of SOX2. These data consistently indicated that the suppression effect of MPC-1 on PDA progression be at least in part through regulating SOX2 expression and function. The molecular mechanisms of suppressive effect of MPC-1 on PDA progression warrant further investigations.
The import of pyruvate into the mitochondrial matrix is the critical step of pyruvate oxidative phosphorylation. We then investigated the metabolic effects of MPC-1 re-expression. We revealed that restored expression of MPC-1 significantly increased the pyruvate concentration in mitochondria, reduced the lactic secretion in media, and consumption of glucose. Moreover, MPC-1-specific inhibitor UK5099 significantly attenuated the effect of MPC-1. Meanwhile, we tested the effect of re-expressing MPC-1 on the expression of enzymes that were relevant to pyruvate metabolism, and found that re-expression of MPC-1 had limited effect on the levels of LDHA, PKM1, PDK, and PDH, but decreased the expression of PKM2 in vitro and in vivo, which might reflect adaptation to the enhanced metabolic demand with MPC-1 re-expression [15]. These data demonstrated that re-expression of MPC-1 promoted the mitochondrial pyruvate metabolism, which might be the mechanism of MPC-1 in inhibiting PDA progression.
The roles of MPC-1 in PDA progression have been revealed, however, the mechanism of decreased expression of MPC-1 in PDA has not been demonstrated. The data of TCGA showed that the mutation of MPC-1 was rare in PDA, and we found that the promoter region of MPC-1 gene was rich in CpG islands. However, the result of Methylation-specific PCR revealed that the promoter region DNA of MPC-1 in most PDA cells were not hypermethylation. In the study from Bardeesy group, they reported that the binding pattern of KDM2B was shifted depending on the EZH2 or KDM5A, and KDM2B-EZH2 cobound genes were mostly involved in developmental and pluripotency networks, meanwhile, the KDM2B-KDM5A cobound genes mainly participated in metabolic processes [19]. Furthermore, methylation pattern revealed that the promoters bound by KDM2B-EZH2 were DNA methylated regardless of the presence of CpG islands. However, the promoters bound by KDM2B-KDM5A were unmethylated. The ChiP-seq result of this study revealed that MPC-1 was a downstream target of KDM2B-EZH2, but not KDM2B-KDM5A. In another study, Benevolenskaya and coworkers [24] have shown that MPC-1 was the downstream target of KDM5A via ChiP-seq [34]. Our results showed that the promoter region of MPC-1 was unmethylated. We then tested the roles of KDM2B, EZH2, and KDM5A on MPC-1 expression in PDA and showed that decreased expression of KDM2B and KDM5A led to increased levels of MPC-1. However, EZH2 did not show any effect on MPC-1 expression. KDM5A was regulated by KDM2B in PDA, so we tested the effect of KDM2B and KDM5A on MPC-1, and revealed that knocked down both of KDM2B and KDM5A further increased MPC-1, while overexpression of KDM5A attenuated the effect of KDM2B on MPC-1 and even further decreased MPC-1. These results revealed that MPC-1 was a downstream target of KDM5A and the effect of KDM2B on MPC-1 might be via KDM5A. Further ChIP assay revealed that KDM5A but not KDM2B directly bound to the promoter region of MPC-1, and H3K4me3 and H3K4me2, the products of KDM5A, both existed in MPC-1 promoter region. KDM5A usually binds to the 5ʹ-CCGCCC-3ʹ motif of genes’ promoter and several of these motifs were found in MPC-1 promoter. The result of lucifrease assay is that KDM5A regulates MPC-1 expression at the transcriptional level. We then further analyzed the correlated expression of KDM5A and MPC-1 in PDA array with the same cohort. The result further confirmed a direct correlation between KDM5A and MPC-1 expression. These data demonstrated that KDM5A transcriptionally regulated the expression of MPC-1 via directly binding to the promoter region of MPC-1, and demethylasing H3K4 for trimethylation.
KDM5A was originally identified as a retinoblastoma-binding protein and reported to play critical roles in multiple types of cancer [35,36,37,38,39]. It has been reported that KDM5A induced histone demethylation and regulated the expression of genes involved in cancer metabolism and cell cycle [28, 36]. However, the roles of KDM5A had not been reported in PDA. In our study, we showed that the expression of KDM5A was elevated in PDA via TCGA database and PDA tissue array, and KDM5A was also an independent prognostic factor for PDA patients. Furthermore, knocking down of KDM5A let to inhibited PDA growth. As MPC-1 was a directly downstream target of KDM5A. We then further demonstrated that the effect of KDM5A on PDA was at least partly through regulating MPC-1. Our results revealed that suppressed expression of KDM5A increased MPC-1 expression, elevated pyruvate concentration in mitochondria, and reduced lactic secretion in media and consumption of glucose. Furthermore, restored expression of MPC-1 with knocking of KDM5A could not further enhance the effect of KDM5A, but MPC-1 inhibitor UK5099 significantly attenuated the effect of knocking down KDM5A. These data demonstrated that KDM5A also played critical roles in PDA progression and the effect at least partly through transcriptionally inhibiting MPC-1 expression.
In summary, this study for the first time provided both clinical and mechanistic evidence supporting that KDM5A transcriptionally regulates MPC-1 expression and that KMD5A/MPC-1 signaling has a critical role in PDA mitochondrial pyruvate metabolism and promotes PDA progression. Therefore, we have not only identified a novel molecular mechanism underling a decreased expression of MPC-1 in PDA, but also revealed a promising molecular target for potentially new therapeutic strategies for controlling PDA progression.
Materials and methods
Mouse model of pancreatic tumor growth
Pathogen-free female athymic nude mice were purchased from the National Cancer Institute (Bethesda, MD). The animals were maintained in facilities approved by the Association for Assessment and Accreditation of Laboratory Animal Care International in accordance with the current regulations and standards of the U.S. Department of Agriculture and Department of Health and Human Services. Tumor cells (1 × 106) in 0.1 mL of Hank’s balanced salt solution were injected subcutaneously of nude mice. The tumor size was measured every week. The tumor-bearing mice were sacrificed on day 35 after inoculation and the tumors were removed and weighed.
Mitochondrial pyruvate, lactate production, and glucose utilization assay
Tumor cells were transfected with different plasmids, and the mitochondria of 1 × 106 cells were isolated using the Mitochondria/Cytosol Fractionation Kit (BioVision, K256-25, California, USA) as the instructions. Mitochondrial pyruvate concentration was determined by pyruvate assay kit (BioVision, K609-100, California, USA) according to the instructions.
Tumor cells were transfected with different plasmids, 1 × 106 cells were prepared for lactate production assay with Lactate Assay Kit (Sigma, Louis, MO, US) according to the manufacturer’s protocol.
For glucose utilization assay, tumor cells were transfected with different plasmids, and the cultures were incubated for 24 h. The media were replaced with phenol-red free RPMI with 1% FBS to continuous culture for 2 days. Glucose concentrations in media were measured using a colorimetric glucose assay kit (Biovision, US) and normalized with cell number.
References
Aguirre-Gamboa R, Gomez-Rueda H, Martinez-Ledesma E, Martinez-Torteya A, Chacolla-Huaringa R, Rodriguez-Barrientos A, et al. SurvExpress: an online biomarker validation tool and database for cancer gene expression data using survival analysis. PLoS ONE. 2013;8:e74250.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7–30.
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74:2913–21.
Jones S, Zhang X, Parsons DW, Lin JC, Leary RJ, Angenendt P, et al. Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science. 2008;321:1801–6.
Bailey P, Chang DK, Nones K, Johns AL, Patch AM, Gingras MC, et al. Genomic analyses identify molecular subtypes of pancreatic cancer. Nature. 2016;531:47–52.
Collisson EA, Sadanandam A, Olson P, Gibb WJ, Truitt M, Gu S, et al. Subtypes of pancreatic ductal adenocarcinoma and their differing responses to therapy. Nat Med. 2011;17:500–3.
Warburg O. On respiratory impairment in cancer cells. Science. 1956;124:269–70.
Birsoy K, Wang T, Chen WW, Freinkman E, Abu-Remaileh M, Sabatini DM. An essential role of the mitochondrial electron transport chain in cell proliferation is to enable aspartate synthesis. Cell. 2015;162:540–51.
Flavell RB. Mitochondrion as a multifunctional organelle. Nature. 1971;230:504–6.
Martinez-Reyes I, Diebold LP, Kong H, Schieber M, Huang H, Hensley CT, et al. TCA cycle and mitochondrial membrane potential are necessary for diverse biological functions. Mol Cell. 2016;61:199–209.
Sullivan LB, Gui DY, Hosios AM, Bush LN, Freinkman E, Vander Heiden MG. Supporting aspartate biosynthesis is an essential function of respiration in proliferating cells. Cell. 2015;162:552–63.
Bricker DK, Taylor EB, Schell JC, Orsak T, Boutron A, Chen YC, et al. A mitochondrial pyruvate carrier required for pyruvate uptake in yeast, Drosophila, and humans. Science. 2012;337:96–100.
Herzig S, Raemy E, Montessuit S, Veuthey JL, Zamboni N, Westermann B, et al. Identification and functional expression of the mitochondrial pyruvate carrier. Science. 2012;337:93–6.
Schell JC, Olson KA, Jiang L, Hawkins AJ, Van Vranken JG, Xie J, et al. A role for the mitochondrial pyruvate carrier as a repressor of the Warburg effect and colon cancer cell growth. Mol Cell. 2014;56:400–13.
Schell JC, Wisidagama DR, Bensard C, Zhao H, Wei P, Tanner J, et al. Control of intestinal stem cell function and proliferation by mitochondrial pyruvate metabolism. Nat Cell Biol. 2017;19:1027–36.
Li Y, Li X, Kan Q, Zhang M, Xu R, Wang J, et al. Mitochondrial pyruvate carrier function is negatively linked to Warburg phenotype in vitro and malignant features in esophageal squamous cell carcinomas. Oncotarget. 2017;8:1058–73.
Shannon CE, Daniele G, Galindo C, Abdul-Ghani MA, DeFronzo RA, Norton L. Pioglitazone inhibits mitochondrial pyruvate metabolism and glucose production in hepatocytes. FEBS J. 2017;284:451–65.
Mair B, Kubicek S, Nijman SM. Exploiting epigenetic vulnerabilities for cancer therapeutics. Trends Pharm Sci. 2014;35:136–45.
Tzatsos A, Paskaleva P, Ferrari F, Deshpande V, Stoykova S, Contino G, et al. KDM2B promotes pancreatic cancer via Polycomb-dependent and -independent transcriptional programs. J Clin Invest. 2013;123:727–39.
Yamamoto K, Tateishi K, Kudo Y, Sato T, Yamamoto S, Miyabayashi K, et al. Loss of histone demethylase KDM6B enhances aggressiveness of pancreatic cancer through downregulation of C/EBPalpha. Carcinogenesis. 2014;35:2404–14.
Blair LP, Cao J, Zou MR, Sayegh J, Yan Q. Epigenetic regulation by lysine demethylase 5 (KDM5) enzymes in cancer. Cancers (Basel). 2011;3:1383–404.
Lopez-Bigas N, Kisiel TA, Dewaal DC, Holmes KB, Volkert TL, Gupta S, et al. Genome-wide analysis of the H3K4 histone demethylase RBP2 reveals a transcriptional program controlling differentiation. Mol Cell. 2008;31:520–30.
Peng JC, Valouev A, Swigut T, Zhang J, Zhao Y, Sidow A, et al. Jarid2/Jumonji coordinates control of PRC2 enzymatic activity and target gene occupancy in pluripotent cells. Cell. 2009;139:1290–302.
Varaljai R, Islam AB, Beshiri ML, Rehman J, Lopez-Bigas N, Benevolenskaya EV. Increased mitochondrial function downstream from KDM5A histone demethylase rescues differentiation in pRB-deficient cells. Genes Dev. 2015;29:1817–34.
Takaoka Y, Konno M, Koseki J, Colvin H, Asai A, Tamari K, et al. Mitochondrial pyruvate carrier 1 expression controls cancer epithelial-mesenchymal transition and radioresistance. Cancer Sci. 2019;110:1331–9.
Zou H, Chen Q, Zhang A, Wang S, Wu H, Yuan Y, et al. MPC1 deficiency accelerates lung adenocarcinoma progression through the STAT3 pathway. Cell Death Dis. 2019;10:148.
Yang C, Ko B, Hensley CT, Jiang L, Wasti AT, Kim J, et al. Glutamine oxidation maintains the TCA cycle and cell survival during impaired mitochondrial pyruvate transport. Mol Cell. 2014;56:414–24.
Beshiri ML, Holmes KB, Richter WF, Hess S, Islam AB, Yan Q, et al. Coordinated repression of cell cycle genes by KDM5A and E2F4 during differentiation. Proc Natl Acad Sci USA. 2012;109:18499–504.
Howe FS, Fischl H, Murray SC, Mellor J. Is H3K4me3 instructive for transcription activation? Bioessays. 2017;39:1–12.
Tu S, Teng YC, Yuan C, Wu YT, Chan MY, Cheng AN, et al. The ARID domain of the H3K4 demethylase RBP2 binds to a DNA CCGCCC motif. Nat Struct Mol Biol. 2008;15:419–21.
Lofrumento NE, Papa S, Zanotti F, Kanduc D, Quagliariello E. [Properties of systems of transport of anionic substrates in mitochondria]. Boll Soc Ital Biol Sper. 1971;47:676–80.
Brivet M, Garcia-Cazorla A, Lyonnet S, Dumez Y, Nassogne MC, Slama A, et al. Impaired mitochondrial pyruvate importation in a patient and a fetus at risk. Mol Genet Metab. 2003;78:186–92.
Li X, Ji Y, Han G, Fan Z, Li Y, Zhong Y, et al. MPC1 and MPC2 expressions are associated with favorable clinical outcomes in prostate cancer. BMC Cancer. 2016;16:894.
Pasini D, Hansen KH, Christensen J, Agger K, Cloos PA, Helin K. Coordinated regulation of transcriptional repression by the RBP2 H3K4 demethylase and polycomb-repressive complex 2. Genes Dev. 2008;22:1345–55.
Defeo-Jones D, Huang PS, Jones RE, Haskell KM, Vuocolo GA, Hanobik MG, et al. Cloning of cDNAs for cellular proteins that bind to the retinoblastoma gene product. Nature. 1991;352:251–4.
Gong F, Clouaire T, Aguirrebengoa M, Legube G, Miller KM. Histone demethylase KDM5A regulates the ZMYND8-NuRD chromatin remodeler to promote DNA repair. J Cell Biol. 2017;216:1959–74.
Klose RJ, Yan Q, Tothova Z, Yamane K, Erdjument-Bromage H, Tempst P, et al. The retinoblastoma binding protein RBP2 is an H3K4 demethylase. Cell. 2007;128:889–900.
Wang C, Wang J, Li J, Hu G, Shan S, Li Q, et al. KDM5A controls bone morphogenic protein 2-induced osteogenic differentiation of bone mesenchymal stem cells during osteoporosis. Cell Death Dis. 2016;7:e2335.
Zhao D, Zhang Q, Liu Y, Li X, Zhao K, Ding Y, et al. H3K4me3 demethylase Kdm5a is required for NK cell activation by associating with p50 to suppress SOCS1. Cell Rep. 2016;15:288–99.
Funding
This work was supported by grants 81502018 (to JC), 81502043 (to MQ) and 81602051 (to DX) from National Natural Science Foundation of China; grant [2019]72 (to JC) from Shanghai “Rising Stars of Medical Talent” Youth Development Program, Youth Medical Talents-Specialist Program; Fundamental Research Funds for the Central Universities 22120180029 (to MQ); The Outstanding Clinical Discipline Project of Shanghai Pudong (Grant No. PWYgy2018-02).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cui, J., Quan, M., Xie, D. et al. A novel KDM5A/MPC-1 signaling pathway promotes pancreatic cancer progression via redirecting mitochondrial pyruvate metabolism. Oncogene 39, 1140–1151 (2020). https://doi.org/10.1038/s41388-019-1051-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41388-019-1051-8
- Springer Nature Limited
This article is cited by
-
Hypoxia promotes metastasis by relieving miR-598-3p-restricted glycolysis in gastric cancer
Journal of Translational Medicine (2024)
-
Deubiquitinase USP7 stabilizes KDM5B and promotes tumor progression and cisplatin resistance in nasopharyngeal carcinoma through the ZBTB16/TOP2A axis
Cell Death & Differentiation (2024)
-
Identification of subgroups and development of prognostic risk models along the glycolysis–cholesterol synthesis axis in lung adenocarcinoma
Scientific Reports (2024)
-
The Molecular Twin artificial-intelligence platform integrates multi-omic data to predict outcomes for pancreatic adenocarcinoma patients
Nature Cancer (2024)
-
MARCH5 promotes aerobic glycolysis to facilitate ovarian cancer progression via ubiquitinating MPC1
Apoptosis (2024)