Abstract
Low sleep duration in adults is correlated with psychiatric and cognitive problems. We performed for the first time a large-scale analysis of sleep duration in children, and how this relates to psychiatric problems including depression, to cognition, and to brain structure. Structural MRI was analyzed in relation to sleep duration, and psychiatric and cognitive measures in 11,067 9–11-year-old children from the Adolescent Brain Cognitive Development (ABCD) Study, using a linear mixed model, mediation analysis, and structural equation methods in a longitudinal analysis. Dimensional psychopathology (including depression, anxiety, impulsive behavior) in the children was negatively correlated with sleep duration. Dimensional psychopathology in the parents was also correlated with short sleep duration in their children. The brain areas in which higher volume was correlated with longer sleep duration included the orbitofrontal cortex, prefrontal and temporal cortex, precuneus, and supramarginal gyrus. Longitudinal data analysis showed that the psychiatric problems, especially the depressive problems, were significantly associated with short sleep duration 1 year later. Further, mediation analysis showed that depressive problems significantly mediate the effect of these brain regions on sleep. Higher cognitive scores were associated with higher volume of the prefrontal cortex, temporal cortex, and medial orbitofrontal cortex. Public health implications are that psychopathology in the parents should be considered in relation to sleep problems in children. Moreover, we show that brain structure is associated with sleep problems in children, and that this is related to whether or not the child has depressive problems.
Similar content being viewed by others
Introduction
Sleep is necessary for maintaining cognitive and emotional abilities. Lack of sleep has been associated with health-related and cognitive consequences [1,2,3,4]. Population-based studies show that individuals with short sleep duration or insomnia are at significantly greater risk for cerebrovascular diseases [5], mental disorders [6, 7], and metabolic disorders [8, 9]. A meta-analysis of 91 studies found that sleep alterations, such as sleep depth and altered rapid eye movement sleep, were present in many mental disorders including schizophrenia, anxiety, affective, eating, and autistic disorders [10]. A previous study in adults revealed a high association between sleep quality and the depressive problems score that was mediated by functional connectivities involving the lateral orbitofrontal cortex, anterior cingulate cortices, hippocampus, and precuneus [7]. Moreover, the impact of sleep and insomnia on brain structure and function is striking. For example, the functional connectivity in the resting state of the default mode, dorsal attention, and hippocampal networks was different after sleep deprivation. [11]. In adults aged ≥55 years, self-reported short sleep duration was associated with faster expansion of the ventricles and faster decline in cognitive performance in the following 2 years [12]. However, most studies on the relation between sleep and brain structure and function have used relatively small numbers of participants (e.g., 1972 participants in 24 studies in a recent meta-analysis [13]), indicating the need for a robust large-scale study such as the present one that included 11,067 participants.
Sleep states are active processes that may function to support reorganization of brain circuitry [14], which makes sleep especially important for children at this stage of brain development. A recent meta-analysis showed a high correlation between sleep and cognitive functioning and behavioral problems in school-age children. Shorter sleep duration was associated with poorer cognitive functioning and worse school performance, and also was related to behavioral problems [15]. Although many studies have identified associations between sleep and cognitive performance and adverse mental health outcomes in children, only a few imaging studies have examined the association between low sleep duration and brain structure [16] and development [17, 18], and the neural mechanisms underlying the association between sleep and cognition and mental health in children are still unknown.
A large-scale multimodal neuroimaging study tracking over 11,000 children in the Adolescent Brain Cognitive Development (ABCD) cohort provides an unprecedented opportunity to investigate the neural differences in children with short sleep duration, and the possible neural mechanisms underlying the association between sleep and various mental health disorders and cognitive performance [19]. The ABCD dataset has been shown useful in investigating the relationship between children’s behavior and brain structure [20, 21]. In the present investigation, we analyzed in the ABCD cohort the relation between brain structure and sleep duration, cognitive performance and mental health by measuring brain morphometric information of different brain regions, and then using a mediation analysis to assess the underlying mechanisms. The main hypothesis that we investigate is that the relation between brain structure and sleep is mediated by psychiatric problems related to brain structure. The second hypothesis that we investigate in another mediation analysis is the extent to which the relation between brain structure and cognition is mediated by sleep duration. Strengths of the present investigation are the longitudinal data with a large number of child participants (baseline 11,067; 1-year follow-up 4696) leading to robust findings; the mediation analysis; linking the findings to recent advances in understanding brain mechanisms related to mental disorders, cognition, and sleep; and the inherent interest of the relation between sleep, cognition, and psychiatric problems to a wide readership.
Materials and methods
Participants and data preprocessing
The dataset used for this investigation was selected from the Annual Curated Data Release 2.01 from the ABCD consortium (https://abcdstudy.org/index.html) which contains over 11,000 children aged 9–11 years recruited from 21 centers throughout the United States with a diverse range of geographic, socioeconomic, ethnic, and health backgrounds [19, 22]. The 21 centers obtained parents’ full written informed consent and the childrens' assent, and research procedures and ethical guidelines were followed in accordance with the Institutional Review Boards (IRB). Our sample includes 11,067 subjects (ages 9–11 years, 5301 females) scanned with three 3 Tesla (T) scanner platforms: Siemens Prisma, General Electric 750 and Phillips. More details of the subjects, and the collection and preprocessing parameters of the data are provided at the ABCD website (https://abcdstudy.org/scientists/protocols/) and also are described elsewhere [19, 22].
We obtained preprocessed structural imaging data (T1 and T2) using the ABCD pipeline, with all the data preprocessing procedures performed by the ABCD team as described in their image processing paper [22] and in the Supplementary Material. Morphometric measures consisting of the cortical area, volume, and thickness of 68 cortical regions [23] and 40 subcortical regions [24] from the ABCD preprocessing were used in the following analyses. The imaging data were only available for baseline (11,067 participants).
The quality control of the processed images was done by the ABCD team and 481 participants who failed to pass the quality control of the ABCD team were removed from subsequent analysis. In addition, three participants who did not contain the full information of both the sleep behavior measures and the structural images were excluded. Finally, 11,067 participants were left for this study and the demographic characteristics of these participants are summarized in Table 1.
Behavioral measures
Sleep assessments
The sleep disturbances scale for children is based on the ABCD Parent Sleep Disturbance Scale for Children (abcd_sds01) which is useful for assessing the sleep–wake rhythm of a child and of any problems in his/her sleep behavior [25]. In the current study, we focus on an important measure of sleep, sleep duration, which is question 1 of the above scale, namely "How many hours of sleep does your child get on most nights" (with further details in the Supplementary Material). We note that a high sleep duration score in this measurement system indicates short sleep duration. In this paper, we use “sleep duration” as the descriptor, where a high sleep duration indicates a large number of hours of sleep. The data were available for baseline (11,067 participants) and 1-year follow-up (4696 participants).
Cognitive assessments
To investigate the relationship between sleep duration and cognitive performance, the NIH Cognition Battery Toolbox (abcd_tbss01) was used to evaluate the cognitive performance of children [26]. The summary score of the NIH Cognition Battery Toolbox contains seven components: language vocabulary knowledge, attention, cognitive control, working memory, executive function, episodic memory, and language. These data were only available for baseline (11,067 participants).
Mental health assessments
We also investigated the relationship between sleep duration and psychiatric problems. The Parent Child Behavior Checklist Scores (abcd_cbcls01) were used to assess the dimensional psychopathology and adaptive functioning in children [27]. It contains ten empirically-based syndrome scales related to psychiatric problems: anxious/depressed, withdrawn/depressed, somatic complaints, social problems, thought problems, attention problems, rule-breaking behavior, aggressive behavior, internalizing broad band score and externalizing broad band score; and a psychiatric problems total score. Six DSM-Oriented Scales were also calculated based on the questionnaire. A high score indicates dimensional psychopathology. The data were available for baseline (11,067 participants) and 1-year follow-up (4696 participants).
More details of these behavior assessments are provided in the Supplementary Material (Table S1) and also can be found at the ABCD website (https://abcdstudy.org/scientists-protocol.html).
Statistical analysis
Association analysis
A linear mixed-effect model (LMM) was used to test the associations of the sleep duration with the brain morphometric measures and with the children’s cognitive scores from the NIH Cognitive Toolbox and the psychiatric problems scores from the Child Behavior Checklist noted above that are provided by ABCD. As recommended by the ABCD and used in many studies [21, 28], a LMM was used to take account of the correlated observations within families due to twins and siblings and at sites. In this way, the LMM was specified to model family nested within site. The LMM was implemented using the MATLAB function fitlme. A morphometry measurement or behavioral score was modeled as the dependent variable, and the sleep duration and the nuisance covariates were modeled as fixed effects, while the family structures nested within sites were modeled as random effects. To ensure that the following variables did not influence the results, they were used in the LMM as covariates of no interest: children’s age, sex, body mass index, puberty score, race (coded as 3-column dummy variables), and parents’ income and number of years of education. A t-statistic and the effect size Cohen's d were obtained for each LMM model to reflect the association between sleep duration and the dependent variable. Finally, false discovery rate (FDR) and Bonferroni corrections to correct the results for multiple comparisons were performed [29]. All brain measurements and behavioral variables used in the association analysis were collected at the ABCD baseline time when the average age was 119 months.
Mediation analysis
A standard mediation analysis was performed using the Mediation Toolbox developed by Tor Wager’s group (https://github.com/canlab/MediationToolbox), which has been widely used in neuroimaging studies [30, 31]. A standard three-variable path model was used here [32], with the detailed methodology described in the supplementary material of [30]. Briefly, mediation analysis tests whether the covariance between two variables can be explained by a third variable (the mediator). The two hypotheses investigated the relation of cortical morphometry with psychiatric and cognitive problems and sleep duration. For the first hypothesis, the independent (predictor) variable was a morphometry measure and the dependent (predicted) variable was sleep duration. The proposed mediator (in the indirect path) was the depressive score. (The proposed mediator in another test in the Supplementary Material was the psychiatric problems total score.) For the second hypothesis, the independent (predictor) variable was a morphometric measure and the dependent (predicted) variable was the Cognition Total Composite Score. The proposed mediator was sleep duration. Confounding variables as in the association analysis were regressed out in the mediation model. The significance of the mediation was estimated by the bias-corrected bootstrap approach (with 10,000 random samplings). All brain measurements and behavioral variables used in the mediation analysis were collected at the ABCD baseline time. We note that significant mediation effects show how much of the correlation between independent and dependent variables is related to another variable termed the mediator, and is strictly a measure of association, which does not prove causality.
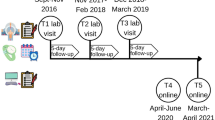
Longitudinal data analysis
For the above-mentioned measurements, it was possible to perform a longitudinal analysis for approximately half the participants (4696) using the sleep duration and psychiatric problems scores which were obtained in the follow-up, 1 year after the baseline time. The neuroimaging was available only at the baseline time. A classic two-wave cross-lagged panel model (CLPM, implemented by Mplus (version 7.4) [33]) based on structural equation modeling was implemented to investigate the longitudinal associations between sleep duration and each of the psychiatric problems scores, using the longitudinal panel data in ABCD [34, 35]. Specifically, let xt and yt be the demeaned baseline sleep duration score and a psychiatric problem score of a subject, and xt+1 and yt+1 be their 1-year follow-up. The CLPM models them as
where αt, βt, δt, γt, η1, and η2 are the coefficients of the model, zt is the confounding variable, and ε1 and ε2 are the error term. The model was estimated by using maximum likelihood estimation with robust standard errors that also take clustering of cases into account. The standardized regression coefficients and their standard errors of variables of interest (namely αt, βt, δt, γt) are reported throughout. Confounding variables, as in the association analysis, were regressed out in the CLPM analysis.
Results
The correlation between sleep duration and other measures in the ABCD dataset
The dimensional psychopathology measures (abcd_cbcl01, abcd_ksad501, abcd_ksad01) were significantly negatively correlated with the sleep duration (that is, pathology was positively associated with short sleep durations) (Fig. 1 and Table 2). 82 out of 119 individual items (119 questions in the CBCL questionnaire, abcd_cbcl01) were significant after Bonferroni correction (p < 0.05). Indeed, all the psychiatry problems scores (abcd_cbcls01) were negatively correlated with the sleep duration with r values ranging from −0.062 to −0.208 (Bonferroni corrected, p < 0.05, Table 2 and Fig. 1c). The depressive problems score was the score most significantly negatively correlated with the sleep duration (r = −0.208, Cohen's d = −0.425, p < 1 × 10−10). Thus the children with shorter sleep duration tended to have higher psychiatric problems scores. What is also interesting is that many parent dimensional psychopathology measures (including abcd_asrs01 and pasr01) were significantly negatively correlated with the sleep duration of the child. As shown in Fig. 1a, the screen time utilization (e.g., the use of mobile phones, TV, internet, and video games, abcd_stq01) was negatively correlated with sleep duration, which is consistent with previous studies [36, 37]. Interestingly, the environmental risk (abcd_rhds01) related measures were also correlated with sleep duration, suggesting that a sense of safety (low risk) may be associated with children’s sleep duration. These, and also the other sleep component scores (abcd_sds01), were negatively correlated with sleep duration with r values ranging from −0.07 to −0.21 (Bonferroni corrected, p < 0.05). In addition, subsyndromal mania (abcd_pgbi01); school, family, and social relations (dibf01); monitoring of children's functioning (abcd_ssbpmtf01); and cultural values (macv01) were negatively correlated with sleep duration in the children (Fig. 1a).
a The correlation between sleep duration and a wide variety of measurements including physical and mental health, neurocognition, substance use, culture, environment and mobile technology, etc. Here we highlight the 17 measurements that are significantly correlated with sleep duration. For example, the positive r value for the cognition scores indicates that long sleep duration is positively correlated with good cognition. The full names for these measurements are shown below and the details for each item are provided in Table S1. b A histogram showing the relation between the number of hours of sleep and cognitive measures. The Y axis is the cognitive score and the error bar is the standard error of the mean (SEM). There was a significant correlation between the cognitive score and the number of hours of sleep (Bonferroni corrected, p < 0.05). The children with long sleep duration tended to have good cognitive performance. c A histogram showing the relation between the number of hours of sleep and the psychiatric problems scores. The Y axis is the psychiatric problems score and the error bar is the SEM. There was a significant negative correlation between the psychiatric problems scores and the number of hours of sleep (Bonferroni corrected, p < 0.05). The children with short sleep duration tended to have high psychiatric problems scores. abcd_saiq02 ABCD Parent Sports and Activities Involvement Questionnaire (SAIQ), abcd_sds01 ABCD Parent Sleep Disturbance Scale for Children, abcd_ssphp01 ABCD Sum Scores Physical Health Parent, abcd_tbss01 ABCD Youth NIH TB Summary Scores, abcd_asrs01 Adult Self Report summary scores, abcd_cbcl01 ABCD Parent Child Behavior Checklist Raw Scores Aseba (CBCL), abcd_cbcls01 Child Behavior Check List summary scores, abcd_ksad01 ABCD Parent Diagnostic Interview for DSM−5 Full, abcd_ksad01 ABCD Parent Diagnostic Interview for DSM−5 Full (KSADS-5), abcd_ksad501 ABCD Youth Diagnostic Interview for DSM-5 (KSADS-5), abcd_pgbi01 ABCD Parent Parent General Behavior Inventory-Mania, abcd_ssbpmtf01 ABCD Summary Scores Brief Problem Monitor-Teacher Form for Ages 6–18, dibf01 ABCD Parent Diagnostic Interview for DSM-5 Background Items Full, pasr01 ABCD Parent Adult Self Report Raw Scores Aseba, abcd_rhds01 Residential History Derived Scores, fes02 ABCD Parent Family Environment Scale-Family Conflict Subscale Modified from PhenX, macv01 ABCD Parent Mexican American Cultural Values Scale Modified, abcd_stq01 ABCD Youth Screen Time Survey.
Eight out of ten of the cognitive summary scores (abcd_tbss01) were positively correlated with the sleep duration (Bonferroni corrected, p < 0.05, Fig. 1b). The range of r values between the sleep duration and cognitive measurements was between 0.032 and 0.069, and these were highly significant (Table 2 and Fig. 1b). Further, 15 out of 49 individual items within neurocognition (abcd_tbss01) were positively correlated with long sleep durations (Bonferroni corrected, p < 0.05, Fig. 1a and Table 2). Thus children with long sleep duration have better cognitive performance.
Short sleep duration, poor cognition, and psychiatric problems are associated with low cortical area and volume
Both cortical area and volume of the whole brain were significantly positively correlated with sleep duration (r = 0.046, Cohen's d = 0.093, p = 1.0 × 10−6 and r = 0.047, d = 0.095, p = 6.2 × 10−7, respectively). Specifically, in children with short sleep, the cortical areas/volumes were lower of the lateral and medial orbitofrontal cortex, superior and middle frontal gyrus and medial superior frontal, inferior and middle temporal gyrus, precuneus and posterior cingulate cortex, ventromedial prefrontal cortex, supramarginal gyrus, and some motor cortical areas (FDR corrected, p < 0.005, Figs. 2a and S1A), and volumes were lower of the thalamus, caudate, and the pallidum (FDR corrected, p < 0.005, Table S2). (Cortical thickness was not associated with sleep duration or with most of the other measures, and for brevity is not described further.) Given the significant association between sleep duration, and cognition and the other sleep component scores, we also performed a complementary analysis with these variables (cognitive total score and all five sleep component scores) as covariates, and found a high correlation between the associated brain patterns with and without these variables regressed out in the analysis of the association between cortical area (or volume) and sleep duration (r > 0.95, p < 1 × 10−10). This shows that the results are robust and consistent and do not depend on these other variables.
a Brain regions with their cortical area significantly associated with sleep duration (FDR corrected, p < 0.005). The red color indicates brain regions with high area positively associated with longer sleep duration. b Brain regions with their area significantly associated with the cognitive total score (FDR corrected, p < 0.005). The red color indicates brain regions where high area is positively correlated with a higher cognitive score. Here, we only show the regions with Cohen’s d larger than 0.15. c Brain regions with their area significantly associated with the depressive problems’ score (FDR corrected, p < 0.005). Blue indicates brain regions with a negative correlation between area and the depressive problems score (i.e., a low cortical area is associated with depressive problems). The brain regions shown here were confirmed using a nonparametric approach that utilized a permutation test (with 5000 random samplings). d Brain regions with their area associated with both sleep duration and the cognitive total score. The regions shown are the overlap of what is shown in a and b. e Brain regions with their area associated with both sleep duration and the depressive problems score. The regions shown are the overlap of what is shown in a and c.
Total cortical area and volume were significantly positively correlated with the cognition total composite score (r = 0.13, d = 0.27, p < 1 × 10−10 and r = 0.11, d = 0.23, p < 1 × 10−10, respectively). The brain areas with significant correlations with the cognition score included the prefrontal and anterior cingulate cortex, medial orbitofrontal cortex, temporal cortex, insula, inferior parietal gyrus, thalamus, caudate, and putamen (FDR corrected, p < 0.005, Figs. 2b, S1B and Table S2).
Total cortical area and volume were significantly negatively correlated with the psychiatric problems total score (r = −0.07, d = −0.15, p = 1.3 × 10−14 and r = −0.07, d = −0.14, p = 2.9 × 10−14, respectively). The significant brain regions after FDR correction (p < 0.005) are shown in Fig. S2. Given the high correlation between depression and sleep problems, we next focus on the depressive problems score. We found that both cortical area and volume were significantly negatively correlated with the depressive problems score (r = −0.05, d = −0.09, p = 8.1 × 10−7 and r = −0.05, d = −0.09, p = 6.4 × 10−7, respectively). Fig. 2c shows that the brain areas with lower area in participants with high depressive problems’ scores included the lateral and medial orbital frontal cortex, temporal cortex, precuneus, superior and middle frontal gyrus and superior medial frontal cortex, angular and supramarginal gyrus, hippocampus, thalamus, caudate, and motor areas (FDR corrected, p < 0.005, Figs. 2c, S1C and Table S2).
The brain areas with correlations with both sleep duration and cognitive performance are shown in Figs. 2d and S1D; and with both sleep duration and depressive problems in Figs. 2e and S1E.
Next, we performed two complementary analyses to determine whether the present brain structure findings were regionally specific. Firstly, we included the intracranial volume as a covariate, which is a useful normalization procedure used in morphometric analyses [38]. As shown in Fig. S3, the association patterns with brain regions were similar between the cases with and without regression of the intracranial volume for all behavioral measures including sleep duration, depressive score, and cognitive score. The regions associated with sleep duration included the orbitofrontal cortex, superior, middle and medial superior frontal gyrus, inferior and middle temporal gyrus, precuneus, and posterior cingulate cortex, all of which remained significant after regressing out the effect of the intracranial volume (FDR p < 0.05). Secondly, we also performed the same analysis using the total cortical volume or area as covariates. Although no region was significant in this case, the association patterns with and without regression of the total cortical volume or area were highly correlated (r ranging from 0.66 to 0.85, all p < 1.0 × 10−5).
The longitudinal association between sleep duration and the psychiatric problems scores
The structural equation modeling path estimates were used to analyze the changes that occurred between the baseline ages of around 10 and 1 year later. These showed that psychiatric problems at the baseline age including the depressive problems and total psychiatric problems’ scores were significantly associated with decreased sleep duration at the 1-year follow-up (Figs. 3a and S4). The reverse was not found. It should be noted that the depressive problems’ score is the top contribution from the different psychiatric measures to the association with decreased sleep duration (β = −0.081, SE = 0.016, p < 1 × 10−4); and the reverse was not found (β = −0.018, SE = 0.013, p = 0.17). The model accounted for 23.8% of the variance in sleep duration, and 40.1% of the variance in the depressive problems’ score in children aged around 11, by taking into account the measures of sleep and depressive problems 1 year earlier.
a The longitudinal association between the depressive problems score and the sleep duration revealed by structural equation modeling (using a two-wave cross-lagged panel model). The depressive problems score was significantly associated with lower sleep duration measured 1 year later (β = −0.081, SE = 0.016, p < 1 × 10−4); and the reverse (dashed line) was not true (β = −0.018, SE = 0.013, p = 0.174). b Mediation analysis: the mediation implemented by depressive problems from the cortical area on sleep duration was significant (β = 0.015, p = 2.5 × 10−10). The indirect path (A, AB, and B) shows that the depressive problems’ score mediates part of the effect of cortical area on sleep duration. Path A: effect of the independent variable, the mean cortical area of the brain regions shown in Fig. 2e which are associated with both sleep duration and the depressive score, on the mediator, the depressive problems’ score; Path B: the effect of the mediator (depressive problems score) on the outcome (sleep duration); Path C shows that the regression coefficient (beta value) of the cortical area on the sleep duration was high when the sleep duration was not taken into account. The beta values show the regression coefficient of the effect of the independent variable (cortical area) on the dependent variable (sleep duration). Path Cʹ indicates the direct effect of the cortical area on the outcome (sleep duration) controlling for the mediator (the depressive problems score). Path Cʹ shows some reduction in the regression coefficient when the effect of the depressive problems score was taken into account. Path AB indicates the extent to which taking the depressive problems score into account can explain the 25.9% effect of the cortical area on sleep duration, which is significant as noted above at p = 2.5 × 10−10. c Mediation analysis: the mediation implemented by sleep duration from the cortical area on cognition was significant (β = 0.032, p = 1.5 × 10−4). SE standard error.
Mediation analysis
The two main hypotheses are defined above. First, the depressive problems significantly mediated the relationship between the mean cortical area of the significant brain regions shown in Fig. 2e and sleep duration (Fig. 3b, path AB, 25.9% of the total effect size, β = 0.015, p = 2.5 × 10−10; 95% CI, 0.011–0.020, FDR corrected, p < 0.005). The brain regions with areas related to both sleep and depressive problems, and involved in the mediation analysis just described, are shown in Fig. 2e and include the medial and lateral orbitofrontal cortex, dorsolateral prefrontal cortex, precuneus, and angular gyrus. The interpretation is that depressive problems significantly mediate the effect of brain structure on sleep. (Similar findings for brain volume are provided in Fig. S5A.)
Similar results were also found for the total psychiatric problems score (Fig. S5B and C). The interpretation is that psychiatric problems taken together significantly mediate the effect of brain structure on sleep.
The second hypothesis investigated is the extent to which the relation between brain structure and cognition is mediated by sleep duration. Fig. 3c shows that the relation between brain structure (the mean cortical area of the significant brain regions shown in Fig. 2d) and cognition was significantly mediated by sleep duration (path AB, 2% of the total effect size, β = 0.032, p = 1.5 × 10−4; 95% CI, 0.018–0.053, FDR corrected, p < 0.005). (The result for brain volume was similar as shown in Fig. S5D.)
Third, in addition, we showed that brain structure mediated some of the effects found. For example, the mediation implemented by cortical area from depressive problems on sleep duration was significant (β = −0.0009, p = 7.8 × 10−4; 95% CI, −0.0014 to −0.0004, FDR corrected, p < 0.005) (Fig. S6). In addition, the mediation implemented by cortical area from sleep duration on cognition was significant (β = 0.065, p = 1.5 × 10−6; 95% CI, 0.04–0.092, FDR corrected, p < 0.005) (Fig. S6). These analyses provide evidence that the brain structure differences described here that are associated with sleep duration are closely related to the cognitive and depressive problems present in the children. We note that these analyses show partial mediation effects. Further, we note that the brain is a significant mediator in all these models, and that the brain in all these models also has a significant effect as an independent variable.
Discussion
We found that dimensional psychopathology (including depression, anxiety, impulsive behavior) in the children aged 9–11 was negatively correlated with sleep duration (Fig. 1 and Table 2). Very interestingly, dimensional psychopathology in the parents was also correlated with short sleep duration in their children (Fig. 1). The brain areas in which higher volume was correlated with longer sleep duration included the superior and middle frontal gyri and superior medial frontal areas, inferior and middle temporal gyrus, precuneus, supramarginal gyrus, thalamus, caudate, and the lateral and medial orbital frontal cortex. Longitudinal data analysis showed that the psychiatric problems, especially the depressive problems, were associated with lower sleep duration measured 1 year later. The reverse association was not significant. Further, mediation analysis showed that depressive problems mediate considerably the effect of brain structure (Fig. 2e) on sleep. The areas we suggest include the orbitofrontal cortex because of its functions in depression and other psychiatric problems [39, 40], and the dorsolateral prefrontal cortex, because of their importance in cognitive functions such as episodic memory and working memory [41].
The mediation analyses showing that depressive problems mediate considerably the effect of low brain area or volume on low sleep duration implicated the lateral orbitofrontal cortex. Part of what was found was that low volume in the orbitofrontal cortex was associated with a high depressive problems’ score (Fig. 2c). This is of interest, for the lateral orbitofrontal cortex is implicated in depression [39, 42]. A possible hypothesis is that reduced volume of the medial orbitofrontal cortex related to reward processing, and of the lateral orbitofrontal cortex related to nonreward processing, is related to depression [42]. Further, if the orbitofrontal cortex is not yet well developed as reflected in its volume, then problems related to depression and thereby poor sleep may occur (as shown by the mediation analysis in Fig. 3b). Many of the other brain areas with structure related to sleep duration and psychiatric problems especially depression including other frontal cortical areas, and the precuneus, are also implicated by functional connectivity analyses in depression and have different connectivity with the orbitofrontal cortex [39, 42,43,44]. There is also evidence for a role of the thalamus, especially the “nonspecific” intralaminar and midline thalamic nuclei, and the reticular nuclei, in sleep [45, 46].
The brain areas in which higher cognitive scores were associated with higher volume included the prefrontal cortex (involved in working memory), the temporal cortex (involved in perception and semantic representation), the medial orbitofrontal cortex, and the pregenual cingulate cortex (involved in reward [42, 47]) (Fig. 2b), and it was of interest that high sleep duration was also associated with high volume of similar areas (Fig. 2d). Sleep had a small effect in mediating the relationship between brain structure and cognition (Fig. 3c).
One of the interesting possibilities raised by this research is that children who are developmentally advanced for their age may have more brain volume in some of the areas identified in this investigation including the orbitofrontal cortex and precuneus, and may thereby be developing cognitive and behavioral capacities that enable them to perform better. Another point is the finding that dimensional psychopathology in the parents was positively correlated with short sleep durations in their children (and with the children's brain volumes and problems). This could be due to inherited characteristics, or could be due to the influences of the environment produced by the parents, or an interaction between the two. Further research will be of interest to address these issues, including genetic mediation analyses.
Research on the role of brain development in children as a factor to help understand the links between sleep, psychiatric problems, and brain structure has not provided clear answers yet. One study showed that sleep disturbances in the first 6 years are associated with smaller gray matter volumes and thinner dorsolateral prefrontal cortex at age 7 [48]. A recent study also showed that sleep problems in children at 1.5, 2, and 6 years of age were associated with lower fractional anisotropy values at 10 years [49]. Although these studies with sleep measures at different times in children potentially reflect the effect of sleep problems on neurodevelopment, the long-term effect of sleep on brain development remains unknown, partly due to the lack of longitudinal neuroimaging studies. A recent systematic review concluded that "Although the research presented supports and offers more insight into the importance of sleep for the developing brain of children and adolescents, no firm conclusions that apply broadly may be drawn" [13]. The present study involved more than a magnitude more participants than these previous studies, and a much wider range of measures. It will be useful to explore the causal relationship between sleep and brain structure and function when the follow-up brain imaging data are available in the ABCD dataset in the future.
Several strengths of the research described here are (1) the very large sample size (11,067) with many behavioral measures of children of almost the same age thereby controlling for age effects; (2) the longitudinal design of the study that enabled us to analyze the relation between psychiatric problems, and sleep duration measured 1 year later; (3) the mediation analysis providing evidence that the psychiatric problems mediated the relationship between brain structure and sleep.
In summary, we show that dimensional psychopathology (including depression, anxiety, and impulsive behavior) is negatively correlated with sleep duration in a large cohort of 11,067 children. Importantly, dimensional psychopathology in the parents was also correlated with short sleep duration in their children. Further, this is the first large-scale investigation of how brain regions contribute to sleep problems in children. We show that psychiatric problems mediate these effects to a considerable extent, via brain regions that include the orbitofrontal cortex, frontal including medial cortical areas, inferior and middle temporal gyrus, precuneus, and supramarginal gyrus (Fig. 2e). We also show that sleep duration mediates a small part of the relation between high brain volume and good cognition.
References
Freeman D, Sheaves B, Goodwin GM, Yu LM, Nickless A, Harrison PJ, et al. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry. 2017;4:749–58.
Yaffe K, Falvey CM, Hoang T. Connections between sleep and cognition in older adults. Lancet Neurol. 2014;13:1017–28.
de Bruin EJ, van Run C, Staaks J, Meijer AM. Effects of sleep manipulation on cognitive functioning of adolescents: a systematic review. Sleep Med Rev. 2017;32:45–57.
St-Onge MP, Grandner MA, Brown D, Conroy MB, Jean-Louis G, Coons M, et al. Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American Heart Association. Circulation. 2016;134:e367–86.
Canivet C, Nilsson PM, Lindeberg SI, Karasek R, Ostergren PO. Insomnia increases risk for cardiovascular events in women and in men with low socioeconomic status: a longitudinal, register-based study. J Psychosom Res. 2014;76:292–9.
Chan MS, Chung KF, Yung KP, Yeung WF. Sleep in schizophrenia: a systematic review and meta-analysis of polysomnographic findings in case-control studies. Sleep Med Rev. 2017;32:69–84.
Cheng W, Rolls ET, Ruan H, Feng J. Functional connectivities in the brain that mediate the association between depressive problems and sleep quality. JAMA Psychiatry. 2018;75:1052–61.
Deng HB, Tam T, Zee BC, Chung RY, Su X, Jin L et al. Short sleep duration increases metabolic impact in healthy adults: a population-based cohort study. Sleep. 2017;40:zsx130.
Gileles-Hillel A, Kheirandish-Gozal L, Gozal D. Biological plausibility linking sleep apnoea and metabolic dysfunction. Nat Rev Endocrinol. 2016;12:290–8.
Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, et al. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. 2016;142:969–90.
Kaufmann T, Elvsashagen T, Alnaes D, Zak N, Pedersen PO, Norbom LB, et al. The brain functional connectome is robustly altered by lack of sleep. Neuroimage. 2016;127:324–32.
Lo JC, Loh KK, Zheng H, Sim SK, Chee MW. Sleep duration and age-related changes in brain structure and cognitive performance. Sleep. 2014;37:1171–8.
Dutil C, Walsh JJ, Featherstone RB, Gunnell KE, Tremblay MS, Gruber R, et al. Influence of sleep on developing brain functions and structures in children and adolescents: a systematic review. Sleep Med Rev. 2018;42:184–201.
Tononi G, Cirelli C. Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration. Neuron. 2014;81:12–34.
Astill RG, Van der Heijden KB, Van Ijzendoorn MH, Van Someren EJ. Sleep, cognition, and behavioral problems in school-age children: a century of research meta-analyzed. Psychol Bull. 2012;138:1109–38.
Yaffe K, Nasrallah I, Hoang TD, Lauderdale DS, Knutson KL, Carnethon MR, et al. Sleep duration and white matter quality in middle-aged adults. Sleep. 2016;39:1743–7.
Telzer EH, Goldenberg D, Fuligni AJ, Lieberman MD, Galvan A. Sleep variability in adolescence is associated with altered brain development. Dev Cogn Neurosci. 2015;14:16–22.
Tarokh L, Saletin JM, Carskadon MA. Sleep in adolescence: physiology, cognition and mental health. Neurosci Biobehav Rev. 2016;70:182–8.
Casey BJ, Cannonier T, Conley MI, Cohen AO, Barch DM, Heitzeg MM, et al. The Adolescent Brain Cognitive Development (ABCD) study: imaging acquisition across 21 sites. Dev Cogn Neurosci. 2018;32:43–54.
Gorham LS, Jernigan T, Hudziak J, Barch DM. Involvement in sports, hippocampal volume, and depressive symptoms in children. Biol Psychiatry Cogn Neurosci Neuroimaging. 2019;4:484–92.
Paulus MP, Squeglia LM, Bagot K, Jacobus J, Kuplicki R, Breslin FJ, et al. Screen media activity and brain structure in youth: evidence for diverse structural correlation networks from the ABCD study. Neuroimage. 2019;185:140–53.
Hagler DJ, Jr., Hatton S, Cornejo MD, Makowski C, Fair DA, Dick AS et al. Image processing and analysis methods for the Adolescent Brain Cognitive Development Study. Neuroimage. 2019;202:116091.
Desikan RS, Ségonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D, et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage. 2006;31:968–80.
Fischl B, Salat DH, Busa E, Albert M, Dieterich M, Haselgrove C, et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron. 2002;33:341–55.
Bruni O, Ottaviano S, Guidetti V, Romoli M, Innocenzi M, Cortesi F, et al. The Sleep Disturbance Scale for Children (SDSC). Construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res. 1996;5:251–61.
Luciana M, Bjork JM, Nagel BJ, Barch DM, Gonzalez R, Nixon SJ, et al. Adolescent neurocognitive development and impacts of substance use: Overview of the adolescent brain cognitive development (ABCD) baseline neurocognition battery. Dev Cogn Neurosci. 2018;32:67–79.
Achenbach TM, Rescorla LA, Maruish ME. The Achenbach system of empirically based assessment (ASEBA) for ages 1.5 to 18 years. In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment, 3rd ed. Mahwah, N.J.: Erlbaum; 2004. p. 179–213. vol. 2.
Dick AS, Garcia NL, Pruden SM, Thompson WK, Hawes SW, Sutherland MT, et al. No evidence for a bilingual executive function advantage in the nationally representative ABCD study. Nat Hum Behav. 2019;3:692–701.
Benjamini Y, Hochberg Y. Controlling the false discovery rate—a practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57:289–300.
Wager TD, Davidson ML, Hughes BL, Lindquist MA, Ochsner KN. Prefrontal-subcortical pathways mediating successful emotion regulation. Neuron. 2008;59:1037–50.
Lim SL, Padmala S, Pessoa L. Segregating the significant from the mundane on a moment-to-moment basis via direct and indirect amygdala contributions. Proc Natl Acad Sci USA. 2009;106:16841–6.
Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82.
Muthén LK, Muthén BO. The comprehensive modeling program for applied researchers user guide. 7th ed. Los Angeles, CA; 2015. https://www.statmodel.com.
Quach JL, Nguyen CD, Williams KE, Sciberras E. Bidirectional associations between child sleep problems and internalizing and externalizing difficulties from preschool to early adolescence. JAMA Pediatr. 2018;172:e174363.
Kessler RC. Linear panel analysis: models of quantitative change. Amsterdam: Elsevier; 2014.
Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. 2015;21:50–58.
Carter B, Rees P, Hale L, Bhattacharjee D, Paradkar MS. Association between portable screen-based media device access or use and sleep outcomes: a systematic review and meta-analysis. JAMA Pediatrics. 2016;170:1202–8.
Hibar D, Westlye LT, Doan NT, Jahanshad N, Cheung J, Ching CR, et al. Cortical abnormalities in bipolar disorder: an MRI analysis of 6503 individuals from the ENIGMA Bipolar Disorder Working Group. Mol Psychiatry. 2018;23:932.
Cheng W, Rolls ET, Qiu J, Liu W, Tang Y, Huang CC, et al. Medial reward and lateral non-reward orbitofrontal cortex circuits change in opposite directions in depression. Brain. 2016;139:3296–309.
Rolls ET. The orbitofrontal cortex and emotion in health and disease, including depression. Neuropsychologia. 2019;128:14–43.
Rolls ET, Wirth S. Spatial representations in the primate hippocampus, and their functions in memory and navigation. Prog Neurobiol. 2018;171:90–113.
Rolls ET. The orbitofrontal cortex. Oxford: Oxford University Press; 2019.
Cheng W, Rolls ET, Qiu J, Yang D, Ruan H, Wei D, et al. Functional connectivity of the precuneus in unmedicated patients with depression. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3:1040–9.
Rolls ET. The brain, emotion, and depression. Oxford: Oxford University Press; 2018.
Gent TC, Bassetti C, Adamantidis AR. Sleep-wake control and the thalamus. Curr Opin Neurobiol. 2018;52:188–97.
Brown RE, Basheer R, McKenna JT, Strecker RE, McCarley RW. Control of sleep and wakefulness. Physiol Rev. 2012;92:1087–187.
Rolls ET. The cingulate cortex and limbic systems for emotion, action, and memory. Brain Struct Funct. 2019;224:3001–18.
Kocevska D, Muetzel RL, Luik AI, Luijk MP, Jaddoe VW, Verhulst FC et al. The developmental course of sleep disturbances across childhood relates to brain morphology at age 7: the Generation R Study. Sleep. 2017;40:zsw022.
Mulder TA, Kocevska D, Muetzel RL, Koopman‐Verhoeff ME, Hillegers MH, White T, et al. Childhood sleep disturbances and white matter microstructure in preadolescence. J Child Psychol Psychiatry. 2019;60:1242–50.
Acknowledgements
Use of the ABCD (https://abcdstudy.org/) dataset is acknowledged. A full list of supporters of ABCD project is available at https://abcdstudy.org/nih-collaborators. JF is supported by the 111 Project (No. B18015), the key project of Shanghai Science and Technology (No. 16JC1420402), National Key R&D Program of China (No. 2018YFC1312900), National Natural Science Foundation of China (NSFC 91630314), Shanghai Municipal Science and Technology Major Project (No. 2018SHZDZX01), and ZJLab. WC is supported by grants from the National Natural Sciences Foundation of China (No. 81701773, 11771010), sponsored by Shanghai Sailing Program (No. 17YF1426200). WC is also sponsored by Natural Science Foundation of Shanghai (No. 18ZR1404400). JZ is supported by grants from the National Natural Science Foundation of China (No. 61573107), and also sponsored by Natural Science Foundation of Shanghai (No. 17ZR1444200). XYZ is supported by grants from the National Natural Science Foundation of China (No. 81873893). FL is supported by funding from the National Natural Science Foundation of China (No. 81571031, No. 81761128035, No. 81930095, and No. 81701334), Shanghai Municipal Commission of Health and Family Planning (No. 2017ZZ02026, No. 2018BR33, No. 2017EKHWYX−02, and No. GDEK201709), Shanghai Shenkang Hospital Development Center (No. 16CR2025B), Shanghai Municipal Education Commission (No. 20152234), Shanghai Committee of Science and Technology (No. 17XD1403200, No. 19410713500, and No. 18DZ2313505), Shanghai Municipal Science and Technology Major Project (No. 2018SHZDZX01), Guangdong Key Project in "Development of new tools for diagnosis and treatment of Autism" (2018B030335001), Xinhua Hospital of Shanghai Jiao Tong University School of Medicine (2018YJRC03, Talent introduction−014, Top talent−201603).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Cheng, W., Rolls, E., Gong, W. et al. Sleep duration, brain structure, and psychiatric and cognitive problems in children. Mol Psychiatry 26, 3992–4003 (2021). https://doi.org/10.1038/s41380-020-0663-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-020-0663-2
- Springer Nature Limited
This article is cited by
-
Sleep and mental health among Chinese adolescents: the chain-mediating role of physical health perception and school adjustment
BMC Psychology (2024)
-
Accuracy of parent-reported sleep duration among adolescents assessed using accelerometry
Pediatric Research (2024)
-
Roles of the medial and lateral orbitofrontal cortex in major depression and its treatment
Molecular Psychiatry (2024)
-
Cognitive and psychiatric relevance of dynamic functional connectivity states in a large (N > 10,000) children population
Molecular Psychiatry (2024)
-
Association between sleep problems and impulsivity mediated through regional homogeneity abnormalities in male methamphetamine abstainers
Brain Imaging and Behavior (2024)