Abstract
The effective treatment of acute myeloid leukemia (AML) is very challenging. Due to the immense heterogeneity of this disease, treating it using a “one size fits all” approach is ineffective and only benefits a subset of patients. Instead, there is a shift towards more personalized treatment based on the patients’ genomic signature. This shift has facilitated the increased revelation of novel insights into pathways that lead to the survival and propagation of AML cells. These AML survival pathways are involved in drug resistance, evasion of the immune system, reprogramming metabolism, and impairing differentiation. In addition, based on the reports of enhanced clinical efficiencies when combining drugs or treatments, deeper investigation into possible pathways, which can be targeted together to increase treatment response in a wider group of patients, is warranted. In this review, not only is a comprehensive summary of targets involved in these pathways provided, but also insights into the potential of targeting these molecules in combination therapy will be discussed.
Similar content being viewed by others
Introduction
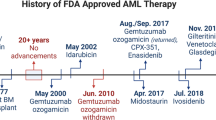
Acute myeloid leukemia (AML) is a blood cancer characterized by an abnormal proliferation and differentiation arrest of myeloid progenitor cells. It primarily affects elderly individuals with 68 years being the median age of diagnosis in the U.S. [1]. Only 24% of individuals with AML survive five years after diagnosis, and no notable improvements in overall survival of individuals over 65 years of age have been observed since 1968 [1]. One reason for the lack of therapy success over the last decades is the mostly unchanged “7 + 3” standard induction scheme, consisting of treatment with the chemotherapeutics cytarabine (Ara-C) and daunorubicin [2]. The limited success of this treatment, especially in the older population, can be attributed not only to the fact that these drugs are highly toxic, but also to the heterogeneity of the disease, where considerable variability both among and within individual patients exist [3, 4].
The extent of this heterogeneity is becoming more apparent as new insights into the biology of AML are revealed [5]. Consequently, there is a shift from the “one size fits all” approach towards more targeted individualized therapy [5]. In 2017 and 2018, a wave of newly approved drugs provided fresh hope for some AML patients and presented a stepping stone into a new era of precision treatment [6]. These include a new liposomal formulation of cytarabine and daunorubicin (CPX-351), and a B-cell lymphoma 2 (BCL-2) inhibitor in combination with hypomethylating agents (Venetoclax and azacitidine or decitabine), among others (for review see [7]). Besides, the Beat AML® Master Clinical Trial launched in 2016 also aims to improve treatment response by categorizing patients based on their genomic signature and assigning them to specific treatment arms (Identifier: NCT02927106). The program has also launched an open-access database consisting of genomic, clinical, and functional information from 562 patient specimens to facilitate further discovery and development of novel targets for AML treatment [8].
The rewards of the increased knowledge of AML biology can already be seen in the discovery of novel targets within the last decade. These targets are involved in multiple pathways that are essential for AML survival, including anti-apoptotic pathways, pro-survival pathways, and epigenetic modification pathways [9]. These new insights into the disease can be beneficial for two reasons. Firstly, it can provide new avenues to treat AML. Secondly, inhibitors of these targets can be used in different combinations with existing drugs to increase the treatment efficiency depending on the molecular landscape of individual AML patients, and thereby serve a broader population of AML patients [10]. A recent example is the FDA approval of combining BCL-2 inhibitor venetoclax with hypomethylating agent (HMA) azacitidine or low dose cytarabine for the treatment of newly diagnosed AML patients, which showed significant synergistic effects [11].
In this review, some promising novel targets, which have shown preclinical potencies against AML and focus on several new directions in the field, will be discussed. It must be noted that this list is not meant to be exhaustive since a recent review has covered many candidates for targeted therapy, involved in pro-apoptotic pathways, cell cycle checkpoint pathways, and epigenetic regulatory pathways, which have shown promising clinical efficiencies [12]. This review instead focuses on novel targets and pathways that are primarily in preclinical testing, but which have nevertheless shown potential to join the battle against AML. These targets are involved in pathways that contribute to the survival of AML cells by modulating (see Fig. 1):
-
Resistance to chemotherapeutics (via SAMHD1 or sphingolipid metabolism)
-
Immune evasion (via LILRB4 or PARP1)
-
Metabolic reprogramming (via NOX or PFKFB3)
-
Differentiation impairment (via DHODH)
Immune evasion, drug resistance, impaired differentiation, and metabolic reprogramming are all strategies used by AML cells to ensure their survival. Targets 1 (PARP1) and 2 (LILRB4) are involved in the immune evasion strategy of AML cells by counteracting anti-tumor responses by NK cells. Targets 3 (SAMHD1) and 4 (AC and SK – part of the sphingolipid metabolic pathway) contribute to drug resistance by either preventing activation of prodrugs or impairing drug-induced cytotoxicity. Target 5 (DHODH) uses different pathways to interfere with the differentiation of leukemic blasts and contribute to their self-renewal properties. Targets 6 (PFKFB3) and 7 (NOX) facilitate the survival of AML cells by reprogramming their metabolism to satisfy their increased energy requirements.
The clinical impact of these targets, in terms of their expression in cells of AML patients and their influence on patient survival, is summarized in Table 1. In addition to reviewing how these targets contribute to AML progression and the preclinical efficiencies of targeting them, insights into the benefits of combining treatments targeting multiple pathways will also be provided [13,14,15,16].
Targeting drug resistance
Drug resistance of AML cells is a primary reason for treatment failure in patients, particularly those over 60 years of age, resulting in disease relapse where treatment is less successful [13]. This is because the cells that survived initial treatment can make up the major population of minimal residual disease (MRD) at relapse. Therefore, understanding pathways taken by the cell to reduce chemotherapeutic-induced damage is pivotal to combating the disease. Cancer cells can develop drug resistance using two strategies: (1) the inability of the drug to perform its task in the cell or (2) modifying the pathways that lead to drug-induced cytotoxicity [17]. There have been several studies elucidating resistance mechanisms of AML cells to current chemotherapeutics (for review see [13]). Although going through all these pathways is beyond the scope of this review, an example for each of the two strategies mentioned above will be discussed below.
SAMHD1
In 2017, sterile alpha motif and HD-domain-containing protein 1 (SAMHD1) was identified as a biomarker for treatment unresponsiveness in AML patients [18, 19]. SAMDH1 is a triphosphonucleoside hydrolase that converts dNTPs to dNs, thereby lowering the dNTP pool in cells. SAMHD1 expression is elevated in myeloid cells, such as macrophages and monocytes, and lymphoid cells, such as resting CD4 + T cells. In cancer, SAMHD1 has been portrayed as a tumor suppressor by limiting the dNTP pool needed for tumor cells to replicate [20]. Contrastingly, SAMHD1 has also been described as a drug resistance factor towards nucleoside analogs, which are frequently used in cancer treatment [21].
In AML, SAMHD1 recognizes the active forms of prodrugs Ara-C (Cytarabine), Ara-CTP, as well as decitabine, DAC-TP, as substrates and converts them back to the inactive prodrug forms, thereby reducing their efficiency [18, 22]. Retrospective analysis based on data from The Cancer Genome Atlas (TCGA) revealed that low SAMHD1 expression in AML patients significantly correlated with better relapse-free survival rates and event-free survival rates [18]. An inverse correlation was also observed between complete remission (CR) and SAMHD1 levels in AML patients treated with Ara-C and decitabine [18, 22]. Reducing SAMHD1 protein levels or knocking out the gene resulted in increased Ara-C and decitabine sensitivity of AML cell lines and primary cells, which was also observed in vivo [18, 22]. Furthermore, Mlcochova et al. have reported that topoisomerase inhibitors, such as daunorubicin, activate SAMHD1 through the induction of DNA damage [23]. Since daunorubicin is administered together with Ara-C during standard treatment, it could contribute to the resistance of the SAMHD1-expressing AML cells to Ara-C, providing further support for targeting SAMHD1 in combination with standard therapy. These results suggest that SAMHD1 is a suitable biomarker to predict a patient’s response to standard induction therapy and could be integrated into patient risk assessment before treatment.
SAMHD1 inhibitors could be combined with nucleoside analogs to help increase their efficiency in high SAMHD1-expressing AML patient subgroups. In the studies by Schneider et al. and Oellerich et al., the administration of virus-like particles (VLPs) packaged with lentiviral accessory protein Vpx reduced SAMHD1 protein levels and increased treatment efficiency in AML cell lines and primary cells [18, 22]. Vpx has a well-established role in recruiting SAMHD1 for degradation by the proteasomal complex [24]. An earlier approach for targeting chemotherapy resistance employed ribonucleotide reductase inhibitors (RRi), which is involved in the synthesis of deoxyribonucleotides. But considering the limited efficacy of the RRi hydroxyurea in AML [25], and since some RRi, such as clofarabine and fludarabine, are recognized as substrates by SAMHD1 [21], directly targeting SAMHD1 holds great potential for AML treatment. Moreover, a recent study has shown that RRi restore the cytotoxicity of Ara-C by indirectly suppressing SAMHD1 [26], further reinforcing the idea of directly inhibiting or degrading SAMHD1. Therefore, the development of small-molecule inhibitors of SAMHD1 or Vpx delivery systems would be beneficial to be used in combination with standard therapy for AML patients who highly express SAMHD1.
Sphingolipid metabolism
The sphingolipid metabolism pathway is involved in several vital cellular processes, including survival, apoptosis, cell cycle progression, and maintenance of membrane integrity [27]. Two critical metabolites of the pathway are ceramide and sphingosine-1-phosphate (S1P), which play opposing roles of pro-death and pro-survival, respectively [28] (see Supplementary Fig. 1). Cellular levels of these two metabolites are tightly regulated by the enzymes ceramidase and sphingosine kinases (SK or SPHK) [29]. Ceramide is converted to sphingosine by ceramidases and then converted to S1P by SK [29] (see Supplementary Fig. 1). This regulation is often hampered in certain cancers, leading to tumor progression and drug resistance via the disruption of drug-induced cytotoxicity.
In AML, analysis of patient data obtained from the TCGA database, mRNA microarray, as well as acid ceramidase (AC) enzyme activity conducted by Tan et al. revealed an increase of both mRNA expression as well as activity of AC in AML samples compared to healthy bone marrow samples [30]. This upregulation consequently reduced cellular levels of pro-apoptotic ceramide [30]. AC overexpression also led to an increase in the expression of P-glycoprotein (P-gp, or MDR1), a well-studied drug resistance factor in AML involved in drug efflux, as well as anti-apoptotic agent myeloid cell leukemia 1 (Mcl-1) [30]. In drug-sensitive cells, the increase in ceramide levels, which leads to cell death, could be caused by drug-induced DNA damage [31]. Tan et al. reported an increase in sensitivity of AML cells to Ara-C and anthracyclines, daunorubicin, and mitoxantrone, upon targeting AC using the ceramide analog LCL204 [32]. A study by Dany et al. described the use of another ceramide analog LCL461 in increasing sensitivity of cells transformed by FLT3 internal tandem duplications (FLT3-ITD), a common mutation in AML, towards FLT3 inhibitors [33]. In both studies, ceramide levels were increased upon treatment with the ceramide analogs. In drug-resistant AML cells, an increase in expression of ceramide synthase (CerS1), AC, and SK was observed, all resulting in reduced ceramide levels [33, 34]. These observations not only reiterate the role of ceramide in drug-induced cytotoxicity, but also provide evidence of induction of drug resistance in AML cells after chemotherapy, in addition to inherent drug resistance of AML cells that already highly express AC, CerS1, or SK before therapy [33, 34]. In addition to AC, SK inhibitors have also shown attractive anti-leukemic activity in preclinical studies [35]. The authors showed that manipulating SK using both inhibitor, such as MP-A08, and genetic knockdowns, could restore the sensitivity of primary AML cells to cytarabine and reduce tumor burden in xenografted mice [35].
Another interesting finding by Tan et al. was the upregulation of the pro-survival factor Mcl-1 upon AC overexpression [32]. Mcl-1, as well as BCL-XL, were also reported to be involved in resistance towards BCL-2 inhibitor venetoclax [36]. In the study by Powell et al., the postulated mechanism by which SK inhibition induced AML cell death was via the inhibition of Mcl-1 [35]. Perhaps it might be beneficial to combine venetoclax treatment with SK or AC inhibitors to counteract resistance mechanisms by Mcl-1 and, at the same time, enhance apoptotic signaling by increasing ceramide levels [35]. Taking these findings together, the role of the members of the sphingolipid metabolism pathway in promoting the survival of AML cells has become even more apparent. Kao et al., in addition, looked further into the effects of targeting members of the sphingolipid metabolic pathway in daunorubicin and cytarabine sensitive and resistant HL-60 cell lines [34]. Inhibitors of AC and SK were able to induce cell death in both sensitive and resistant HL-60 AML cells, suggesting that they could be used after chemotherapy to target cells that might have escaped initial drug-induced cell death [34].
AML cells with high levels of AC or SK are protected from drug-induced cytotoxicity by preventing the accumulation of pro-apoptotic ceramide, which is an important factor involved in apoptotic pathways induced by chemotherapeutics [37]. Inhibitors of AC, ceramide analogs, or SK inhibitors combined with current chemotherapeutics may reverse this protection mechanism by increasing ceramide levels and facilitating drug-induced cytotoxicity, thereby enhancing the anti-leukemic effects of the chemotherapeutics via synergy. An additional benefit of targeting these members of the sphingolipid metabolic pathway is that they are also effective as monotherapy, since targeting them reduces levels of pro-survival signaling through S1P and trigger apoptotic signaling through ceramide (see Supplementary Fig. 1), thereby even benefiting patients who are ineligible for current chemotherapeutic therapies.
Targeting immune evasion
Evading the immune system is a well-developed strategy used by many tumors to thrive in the tumor microenvironment. In AML, leukemic blasts can also avoid being recognized and eliminated by cytotoxic lymphocytes. The success of graft-versus-leukemia response in selected patients who received allogeneic stem cell transplantation shows the potential of immunotherapy in AML. Nevertheless, relapse after transplantation can occur, caused by immune escape mechanisms of AML [38]. Two such mechanisms are (1) preventing activation and proliferation of anti-tumor immune cells and (2) by making themselves “invisible” to anti-tumor immune cells. The use of immune checkpoint inhibitors, for example, anti programmed death-ligand 1 (PD-L1) antibodies, seemed to show promise in early clinical trials [39]. These observations provide the rationale for digging deeper into immune evasion pathways exploited by AML cells. Besides immune checkpoint inhibitors, LILRB4 and PARP are two such candidates involved in AML immune evasion, which will be discussed further below. A comprehensive review of the use of checkpoint inhibitors in AML treatment is provided by Winer and Stone [12].
LILRB4
Leukocyte immunoglobulin-like receptor B (LILRB4, or ILT3) is an immune receptor expressed on cells of the myeloid lineage and is involved in the suppression of T cell activation and proliferation through immune receptor tyrosine-based inhibitory motif (ITIM) signaling. In AML, Deng et al. reported an increase in LILRB4 expression, specifically in the monocytic subtype of AML cells compared to other subtypes and healthy myeloid cells upon analysis of the TCGA database [40]. LILRB4 contributes to immune evasion of AML cells by inactivating anti-tumor natural killer (NK) T cells [40]. This involves the binding of glycoprotein apolipoprotein E (apoE) to LILRB4. apoE is reported to be an inducer of anti-inflammatory response by facilitating the conversion of pro-inflammatory macrophages to anti-inflammatory ones [41]. In monocytic AML cells, upon binding of the apoE, the Src homology region 2 (SHP2) domain of the LILRB4 ITIM activates NF-kB via a phosphorylation cascade, leading to the expression of urokinase receptor (uPAR) and arginase 1 (ARG1) [40]. These two effectors are released from AML cells and consequently prevent activation and proliferation of T cells and the migration of leukemic cells. Usage of anti-LILRB4 antibodies resulted in the reversal of T cell suppression by disrupting the interaction of LILRB4 with apoE, allowing for the hindrance of AML development and migration of AML cells [42]. In vivo efficacy was also reported when tumor burden was significantly reduced in xenografted mice treated with an anti-LILBR4 antibody [42]. In addition, chimeric antigen receptor (CAR) T cells against the receptor have been evaluated for their efficiency in vitro and in vivo. John et al. reported that LILRB4-directed CAR T cells specifically target monocytic AML cells and leave healthy hematopoietic cells unharmed both in vitro and in xenografted mouse models, reducing tumor burden [43].
There has been some evidence showing that immune checkpoint inhibitors enhance the efficiency of HMA. Since HMA treatment could induce the expression of immune inhibitory receptors caused by the reduced methylation of their promoters, co-treatment with immune checkpoint inhibitors could counteract this immune evasive effect [44, 45]. Although so far, there is no evidence to show an increase in LILRB4 expression upon hypomethylation, it might be worthy to test the combination of LILRB4 with HMAs in preclinical settings to look for synergistic effects. These studies shed some light on the possibility of using LILRB4 not only as a target for intervention to reverse immune evasion by AML cells, but also a possible homing molecule for CAR T cell therapy. Combining LILRB4 inhibition with adoptive cell therapy might also be beneficial to boost anti-tumor immunity by providing a favorable environment for immune activation, particularly in monocytic AML. In addition, other ITIM-containing receptors, such as leukocyte associated immunoglobulin-like receptor 1 (LAIR1), have also been reported to be involved in AML development via an alternative pathway [46]. Therefore, further investigation into ITIM-containing receptors and their role in AML could facilitate the discovery of better immune modulators that can perhaps widen the patient group, which can be benefited.
PARP1
Poly[ADP-ribose] polymerase 1 (PARP1) plays a role in DNA damage repair by mobilizing proteins involved in double-stranded and single-stranded DNA break repair. The use of PARP inhibitors to induce synthetic lethality has been explored in FLT3-ITD AML, where FLT3 inhibitors and PARP inhibitors showed synergistic anti-leukemic effects [47]. It was shown that FLT3 inhibition led to a downregulation of repair via homologous recombination in these cells, thereby mimicking the effect of repair-deficient cells, which are more sensitive to PARP inhibition [47]. Besides synthetic lethality in repair-deficient cancers, more evidence seems to indicate alternative pathways of PARP1 that lead to tumor progression other than through DNA damage response, showing potencies in repair-competent cancers as well [48]. One of these pathways include modulating the immune environment in tumors [49]. In AML cells, PARP can contribute to immune evasion via two reported mechanisms: (1) PARP-dependent apoptosis of anti-tumor immune cells through increased reactive oxygen species (ROS) levels, and (2) PARP-mediated downregulation of NK-cell activating receptor-ligand (NKG2DL) expression on AML cells.
The first mechanism was reported in the monocytic subtype of AML [50]. PARP-mediated apoptosis of killer lymphocytes was already described in 2006 and was shown to be induced by ROS [51]. ROS production via the catalytic activity of NADPH oxidases (NOX) was increased in specifically monocytic AML cells, which induced PARP-dependent apoptosis in anti-tumor immune cells such as NK cells and T cells [50]. Using either PARP inhibitor PJ34 or NOX inhibitor DPI, they demonstrated that apoptosis induction of NK cells and T cells was significantly reduced in vitro [50]. Although this efficacy has not been described in vivo so far, inhibiting PARP to reverse the ROS-induced apoptosis of NK and T cells might be worth considering for AML treatment. Support for this comes from the recent approval of ROS-suppressing histamine dihydrochloride (HDC) in combination with IL-2 to induce immune intervention of AML cells [52]. Following the same mechanism, PARP inhibitors could also be used to prevent ROS-induced apoptosis of NK and T cells.
The second mechanism of immune modulation is the involvement of PARP in the regulation of NKG2DL [53, 54]. NKG2D receptors are found on NK cells and can be activated via NKG2DLs found on tumor cells or cells under stress [55]. High expression of PARP was shown to be associated with poor clinical outcome of AML patients [54, 56]. Paczulla et al. reported that the PARP1-dependent downregulation of NKG2DL in leukemic stem cells leads to their immune evasion by making themselves unrecognizable by NK cells and T cells that express the receptors on their surface [54]. In their study, they described synergistic anti-leukemic effects of combination therapy with PARP inhibitor AG-14361 and polyclonal NK cells in vivo [54].
The usage of PARP inhibitors has been extensively described in combination with other drugs for AML [56]. Not only was it reported to be efficacious in combination with FLT3 inhibitors, PARP inhibitors have also shown synergistic potencies when combined with DNA damaging chemotherapeutic agents such as daunorubicin in IDH1/2-mutant AML cells [57, 58]. Preclinical studies also revealed that PARP inhibition enhanced the cytotoxic effects of the DNA damaging agent temozolomide by preventing DNA damage repair and thereby inducing synthetic lethality in relapsed or refractory AML patients [59]. Usage of PARP inhibitors combined with glycogen synthase kinase-3 (GSK3) inhibitors was also efficacious against PARP inhibitor-resistant MLL-rearranged acute leukemia in vivo [60]. All these studies show evidence for the multi-pronged effects of PARP inhibition. PARP inhibitors also have already established tolerances in patients from many clinical trials. Considering the preclinical potential of combination therapy of PARP inhibitors, their efficiencies should also be explored in the clinical setting.
Targeting metabolic reprogramming
Deregulated metabolism is a major hallmark of cancer. Due to their immense growth requirements, cancer cells often need to reprogram their metabolism to provide themselves with enough energy to supply all the upregulated cellular processes needed for survival and proliferation [61]. Cancer cells obtain energy primarily by metabolizing glucose using different pathways, such as glycolysis and the pentose phosphate pathway (PPP) [62]. Targeting deregulated metabolism has proven to be effective based on the success of IDH1/2 inhibition in IDH1/2-mutated AML patients, and the clinical efficiency of IDH1/2 inhibitors has already been extensively reviewed [12]. Another factor that is important for survival signaling of cancer cells is the ROS level. The role of ROS in cancer is bifunctional and heavily dependent on the levels of these radicals, the ability of the cell to cope with them, and the downstream pathways that are involved [63]. Nevertheless, evidence exists describing the tumor-promoting role of ROS in the AML context. In the following subsections, the role of ROS and glucose metabolism in the AML setting and novel potential targets of these pathways will be discussed.
NOX
NOX are transmembrane proteins, which catalyze ROS production, such as the superoxide anion, using NADPH as an electron donor. NADPH can also function as scavengers for ROS by facilitating the regeneration of reduced glutathione (GSH) to serve as an anti-oxidant by donating electrons to hydrogen peroxide (H2O2) [64]. The opposing roles of NADPH underscores the importance of redox homeostasis in the survival of cells. In the context of AML, Hole and colleagues reported that in over 60% of AML cells, ROS levels are elevated and mainly produced by NOX rather than mitochondrial respiration, which is another major source of ROS [65]. This NOX-derived increase in ROS level induced cell proliferation of AML blasts in a p38 MAPK-suppressed environment [65]. This might have caused a reduction in levels of anti-oxidant Prx-1, weakening the cell’s ability to counteract the increased ROS levels [65]. In an earlier study, Hole et al. reported in Ras-activated myeloid progenitor cells an increase in NOX-derived ROS, which resulted in cell proliferation caused by an activation of D cyclins [66].
Several studies have described further roles of NOX on AML development. In FLT3-ITD AML cells, NOX-derived ROS were shown to be involved in pro-survival signaling [67]. Leukemia propagation after transplantation was also reduced in cells deficient for Rac2, considering that Rac is an important activator of NOX [68, 69]. Another study from 2018 reported that NOX2 inhibition in the proto-oncogene KRAS-activated murine leukemia model resulted in improved survival of mice due to delayed onset of myeloproliferative disease [70]. NOX2 is a member of the NOX family, which is a major source of ROS and is predominantly expressed in myeloid cells [71]. A similar phenotype was also observed by Adane et al., where mice engrafted with NOX2-knockout leukemia cells survived longer and had lower disease burden compared to wildtype leukemia cells [71]. In addition, the authors also reported the reprogramming of metabolic pathway towards fatty acid metabolism from glucose metabolism upon NOX2 inhibition [71]. This might provide some rationale for investigating the combination of NOX2 inhibitors with fatty acid metabolism inhibitors to induce synthetic lethality.
NOX-derived ROS also positively affects glucose uptake by leukemic cells. Prata et al. reported that increased ROS levels derived from NOX2 and NOX4 caused an increase in glucose transporter 1 (GLUT1) expression, thereby linking ROS generation to NOX and glucose metabolism [72]. Although the mechanism for ROS-induced GLUT1 expression was not described, it might be due to the activation of HIF1 alpha (HIF1a) by ROS, which then promotes the expression of GLUT1 [73, 74]. Another interesting observation of metabolic reprogramming by NOX-derived ROS is the increased transfer of mitochondria from bone marrow stromal cells (BMSC) to AML blasts [75]. It has been described that AML blasts have a higher mitochondrial mass than normal hematopoietic cells, which accounts for their increased dependence on mitochondrial ATP production for survival [76]. An increase in mitochondrial transfer was also reported to provide post-chemotherapeutic advantage of AML blasts by protecting them against therapy-induced mitochondrial damage [76]. Marlein and colleagues reported that the pathway used by AML blasts to acquire mitochondria from the BMSC was mediated by NOX-generated ROS, which facilitated the formation of tunneling nanotubes between AML blasts and BMSCs [75]. These findings further strengthen the link between ROS production by NOX and AML metabolism.
While NOX-derived ROS seems to rather promote survival of ROShigh AML blasts, induction of mitochondrial ROS is an important feature of venetoclax and HMA-induced cytotoxicity of leukemic stem cells (LSCs) [77]. This is because LSCs are characterized by high BCL-2 expression, low ROS levels, and an increased dependence on oxidative phosphorylation as a source of energy compared to AML blasts [77]. Therefore, it must be noted that targeting just NOX might not be sufficient to fully eradicate all leukemic cells. Instead, combining therapies, where both blasts and LSCs are targeted, could be more beneficial.
Taking all these findings together, the multifaceted role of NOX-derived ROS in the development of AML is evident. NOX-derived ROS are involved in enhancing pro-survival pathways, metabolic reprogramming as well as immune evasion mechanisms. In addition, the interplay of NOX-derived ROS with other factors involved in AML development, such as PARP, as mentioned in subsection “PARP”, encourages the investigation of several combination therapies depending on the expression profile of AML cells from individual patients.
PFKFB3
PFKFB3, or 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase 3, is an isoenzyme that has two opposing enzyme activities. It is known to have a much stronger kinase activity than phosphatase activity compared to other PFKFB family members, such as PFKFB4, which has a stronger phosphatase activity [78]. PFKFB3 plays an important role in the regulation of glycolysis and pentose phosphate pathway (PPP), both of which are pathways of glucose metabolism [78] (see Supplementary Fig. 2). The kinase activity of PFKFB3 is involved in activating the glycolysis pathway rather than the PPP by producing fructose-2,6-bisphosphate (F2,6P2) from fructose-6-phosphate (F6P), which is an activator of 6-phosphofructo-1-kinase (PFK1), an essential enzyme in the rate-limiting step of glycolysis [78] (see Supplementary Fig. 2).
In AML, Feng and Wu reported that in mTOR-activated AML cells, the expression of PFKFB3 is upregulated [79]. They showed that the expression of PFKFB3 is regulated by HIF1, which is stabilized by mTORC1 [79]. mTOR has been shown to induce the expression of not only PFKFB3, but also GLUT1, via the action of HIF1, reiterating its pivotal role in modulating glycolysis [80]. Interestingly, ROS have also been described to activate the kinase function of PFKFB3 [81]. Robinson et al. observed an AMPK-induced activation of PFKFB3 caused by an increase in NOX-derived ROS, which led to the proliferation and survival of Ras-activated AML cells [81]. When they treated the ROShigh AML cell line THP-1 with the NOX inhibitor DPI, they observed a significant reduction in PFKFB3 expression [81]. This phenotype was reversed when cells were treated with glucose oxidase to produce H2O2 and was not observed in the ROSlow Mv4;11 cell line [81]. Furthermore, treatment of ROShigh THP-1 cells with PFKFB3 inhibitors 3PO and PFK158 resulted in reduced glucose uptake and proliferation, reiterating the crosstalk between ROS and PFKFB3 in AML survival and proliferation [81].
Another study also revealed the role of TP53-induced glycolysis and apoptosis regulator (TIGAR) during PFKFB3 activation [82]. TIGAR was reported to be overexpressed in cytogenetically normal AML patients, which correlated with their reduced survival [82]. Mechanistically, TIGAR overexpression led to the inactivation of PFKFB3, activation of PPP, and subsequent decrease in ROS levels by increasing GSH (anti-oxidant) levels [82]. Consequently, leukemic survival was boosted, and apoptosis was hemmed. The authors also reported that a combination of TIGAR knockdown with glycolysis inhibition showed synergy in inducing leukemic cell death [82]. Although 2-deoxy-D-glucose (2-DG) was used as a glycolysis inhibitor, which inhibits the production of fructose-6-phosphate, TIGAR knockdown also sensitized cells to PFKFB3 inhibition [82]. This is because TIGAR activation leads to the use of PPP for energy production, and through its knockdown, PPP is inactivated, and the cells become heavily dependent on glycolysis [82]. The studies above provide evidence that both PPP and glycolysis pathways are exploited by AML cells for energy production and survival. PFKFB3 is an essential element of this switch between PPP and glycolysis and thereby serves as an attractive target of metabolic reprogramming and adaptation by leukemic cells, especially when combined with inhibitors of other metabolic pathways such as PPP. Furthermore, increasing evidence of the interplay between ROS and glucose metabolism warrants investigation into combination therapies targeting both pathways, which could prove effective against leukemic cells.
Targeting impaired differentiation
AML is characterized by the impaired differentiation of immature myeloid progenitor cells. Therapy to induce differentiation of AML cells became very attractive since the success of all-trans retinoic acid (ATRA) differentiation therapy in acute promyelocytic leukemia (APL) [16, 83]. Differentiation therapy is also attractive for AML treatment because it can restore the population of normal immune cells within the patients rather than eliminate blasts cells, which could possibly lead to tumor lysis syndrome (TLS) caused by cellular debris [16, 84]. Recently, IDH1/2 inhibitors have gained popularity as inducers of differentiation in relapsed or refractory AML patients with IDH1/2 mutations. These inhibitors have even gained FDA approval to treat older patients with IDH1/2 mutations having relapsed or refractory AML. Since inhibition of IDH1/2 has been reviewed extensively [12], this section focuses on new targets, which could also benefit AML patients who do not belong to the IDH1/2 mutant group.
Differentiation can be induced in two ways: (1) counteracting genes linked to self-renewal and stem cell-like properties, and (2) inducing genes involved in differentiation. In this section, a target involved in both pathways will be further discussed.
DHODH
Dihydroorate dehydrogenase (DHODH) catalyzes dihydroorotate conversion into orotate, which is part of the pathway of de novo pyrimidine synthesis [85]. This pathway is essential for cell growth and metabolism, since it provides the cells with pyrimidine bases not only for nucleotide synthesis and recycling, but also for glycoprotein and phospholipid synthesis [86]. The involvement of DHODH in AML survival was first revealed by Sykes et al. [87]. An inverse correlation between DHODH expression and survival of AML patients was also observed in a panel of cytogenetically normal AML patients [88]. Since this report, several DHODH inhibitors have been tested for efficiency against AML both in vitro and in vivo [88,89,90,91].
Compounds inhibiting DHODH have only showed mild effects in AML, which might be caused by the fact that they are only weak inhibitors of DHODH [87]. After several decades of inactivity, DHODH inhibitors are being investigated for their efficiency in treating myeloid malignancies [92], namely BAY 2402234 and ASLAN003, from Bayer and Aslan Pharmaceuticals, respectively. BAY 2404434 recently entered Phase 1 clinical trials after highly promising preclinical results showing the efficiency of monotherapy and induction of differentiation among different subtypes of AML [89]. ASLAN003 has entered Phase 2a clinical trials for its use in AML patients after showing tolerance in healthy patients in the Phase 1 trial, as well as high efficiency in vitro, ex vivo, and in vivo [90].
Despite the success of targeting DHODH in AML, the exact mechanism of how DHODH inhibition leads to differentiation induction is not fully understood. Since DHODH is an essential enzyme of the pyrimidine biosynthesis pathway and has close relationships with other metabolic pathways such as oxidative phosphorylation, DHODH could prevent differentiation by modulating these pathways [93]. O-GlcNAcylation (O-GlcNAc) is an important post-translational modification that regulates many proteins essential for proliferation and metabolism, such as Myc and AKT [94]. Inhibition of DHODH leads to a reduction in O-GlcNAc marks, which might explain the observed suppression of Myc protein and the consequent stabilization of p21, an essential regulator of cell cycle, observed in the studies by Wu et al. [88, 89, 95]. GSK3 alpha (GSK3a), whose inhibition induced differentiation of AML cells [96], was also inactivated in response to DHODH inhibitor BAY2404434 [89]. DHODH inhibition also leads to reduced O-GlcNAcylation of key factors involved in metabolism, such as AKT, which is an essential part of the P13K/AKT/mTOR pathway also involved in activating PFKFB3 (see subsection “PFKFB3”) [94].
The inhibition of DHODH has proven to be an invaluable strategy to induce AML differentiation. Not only that, the interplay of the pyrimidine synthesis pathway with multiple other pathways involved in metabolism and cell proliferation makes it an attractive target for use in combination therapy. While highly speculative, DHODH inhibitors could have synergistic activities with PFKFB3 inhibitors or mTOR inhibitors, considering the crosstalk between those two pathways as mentioned above, and could be worth investigating in a preclinical setting. Furthermore, recent findings linking the FLT3 pathway to DHODH dependency also provides a platform for exploring combination therapy of FLT3 inhibitors with DHODH inhibitors, which is currently underway [97]. Taken together, these studies open up the stage to DHODH inhibitors as a therapeutic strategy with high potential to go from bench to bedside.
Concluding remarks
This review goes in-depth into the current knowledge on the mechanisms of development of resistance to chemotherapeutic drugs, evasion of the immune system, adaptation of metabolism for survival, and impairment of differentiation by AML cells (Fig. 1). The search for novel targets and therapeutics for AML has accelerated in parallel with the efforts to better understand the biology behind initiation and progression of AML, as well as response to therapy. Although there are many details yet to be unraveled, the broad knowledge available has led to the identification of potential targets, like the ones mentioned here, which have shown considerable preclinical efficiencies in treating AML both in vitro and in vivo. Bringing therapies against these targets into clinical trials could benefit a broader population of AML patients, rather than just specific subgroups.
Another important point is the need to introduce more clinical studies which combine compounds against several targets, as emphasized by Estey et al. [98]. The presence of crosstalks between the pathways further supports the need for investigators to look into combination therapy to improve the effects of what might otherwise be inefficacious monotherapies (Fig. 1). The benefits of using FLT3 inhibitors together with ceramide analogs or the combination of SAMHD1 inhibitors with Ara-C or decitabine, among others, is proof that such a strategy should be pursued. The recent successes of combinations of several novel drugs with existing chemotherapeutics, such as venetoclax with hypomethylating agents or low dose cytarabine [99, 100], will hopefully increase the number of combination therapies being tested in clinical trials and provide more options for personalized therapy in current and future AML patients.
References
Shallis RM, Wang R, Davidoff A, Ma X, Zeidan AM. Epidemiology of acute myeloid leukemia: Recent progress and enduring challenges. Blood Rev. 2019;36:70–87.
Döhner H, Weisdorf DJ, Bloomfield CD. Acute myeloid leukemia. N Engl J Med. 2015;373:1136–52.
Eleni LD, Nicholas ZC, Alexandros S. Challenges in treating older patients with acute Myeloid Leukemia. J Oncol. 2010;2010:11.
Hassan C, Afshinnekoo E, Li S, Wu S, Mason CE. Genetic and epigenetic heterogeneity and the impact on cancer relapse. Exp Hematol. 2017;54:26–30.
Lohse I, Statz-Geary K, Brothers SP, Wahlestedt C. Precision medicine in the treatment stratification of AML patients: challenges and progress. Oncotarget. 2018;9:37790–7.
Tiong IS, Wei AH. New drugs creating new challenges in acute myeloid leukemia. Genes Chromosom Cancer. 2019;58:903–14.
Lai C, Doucette K, Norsworthy K. Recent drug approvals for acute myeloid leukemia. J Hematol Oncol. 2019;12:100.
Tyner JW, Tognon CE, Bottomly D, Wilmot B, Kurtz SE, Savage SL, et al. Functional genomic landscape of acute myeloid leukemia. Nature. 2018;562:526.
Cerrano M, Itzykson R. New treatment options for acute myeloid leukemia in 2019. Curr Oncol Rep. 2019;21:16.
Kang Y, Tran T, Zhang L, Ball ED, Piermarocchi C, Paternostro G. Personalized drug combinations for the treatment of acute myeloid leukemia (AML) patients. Blood 2014;124:3616.
Pollyea DA, Amaya M, Strati P, Konopleva MY. Venetoclax for AML: changing the treatment paradigm. Blood Adv. 2019;3:4326–35.
Winer ES, Stone RM. Novel therapy in Acute myeloid leukemia (AML): moving toward targeted approaches. Ther Adv Hematol. 2019;10:204062071986064.
Zhang J, Gu Y, Chen B. Mechanisms of drug resistance in acute myeloid leukemia. Onco Targets Ther. 2019;12:1937–45.
Teague RM, Kline J. Immune evasion in acute myeloid leukemia: Current concepts and future directions. J Immunother cancer. 2013;1:13.
Chapuis N, Poulain L, Birsen R, Tamburini J, Bouscary D. Rationale for targeting deregulated metabolic pathways as a therapeutic strategy in acute myeloid leukemia. Front Oncol. 2019;9:405.
Gocek E, Marcinkowska E. Differentiation therapy of acute myeloid leukemia. Cancers (Basel). 2011;3:2402–20.
Ross DD. Novel mechanisms of drug resistance in leukemia. Leukemia. 2000;14:467–73.
Schneider C, Oellerich T, Baldauf HM, Schwarz SM, Thomas D, Flick R, et al. SAMHD1 is a biomarker for cytarabine response and a therapeutic target in acute myeloid leukemia. Nat Med. 2017;23:250–5.
Herold N, Rudd SG, Ljungblad L, Sanjiv K, Myrberg IH, Paulin CBJ, et al. Targeting SAMHD1 with the Vpx protein to improve cytarabine therapy for hematological malignancies. Nat Med. 2017;23:256–63.
Kohnken R, Kodigepalli KM, Wu L. Regulation of deoxynucleotide metabolism in cancer: Novel mechanisms and therapeutic implications. Mol Cancer. 2015;14:176.
Knecht KM, Buzovetsky O, Schneider C, Thomas D, Srikanth V, Kaderali L, et al. The structural basis for cancer drug interactions with the catalytic and allosteric sites of SAMHD1. Proc Natl Acad Sci USA 2018;115:E10022–31.
Oellerich T, Schneider C, Thomas D, Knecht KM, Buzovetsky O, Kaderali L, et al. Selective inactivation of hypomethylating agents by SAMHD1 provides a rationale for therapeutic stratification in AML. Nat Commun. 2019;10:3475.
Mlcochova P, Caswell SJ, Taylor IA, Towers GJ, Gupta RK. DNA damage induced by topoisomerase inhibitors activates SAMHD 1 and blocks HIV -1 infection of macrophages. EMBO J. 2018;37:50–62.
Hofmann H, Logue EC, Bloch N, Daddacha W, Polsky SB, Schultz ML, et al. The Vpx lentiviral accessory protein targets SAMHD1 for degradation in the nucleus. J Virol. 2012;86:12552–60.
Burnett AK, Milligan D, Prentice AG, Goldstone AH, McMullin MF, Hills RK, et al. A comparison of low-dose cytarabine and hydroxyurea with or without all-trans retinoic acid for acute myeloid leukemia and high-risk myelodysplastic syndrome in patients not considered fit for intensive treatment. Cancer. 2007;109:1114–24.
Rudd SG, Tsesmetzis N, Sanjiv K, Paulin CB, Sandhow L, Kutzner J, et al. Ribonucleotide reductase inhibitors suppress SAMHD 1 ara‐ CTP ase activity enhancing cytarabine efficacy. EMBO Mol Med. 2020;12.
Matsuura K, Canfield K, Feng W, Kurokawa M. Metabolic regulation of apoptosis in cancer. Int Rev Cell Mol Biol. 2016;327:43–87.
Van Brocklyn JR, Williams JB. The control of the balance between ceramide and sphingosine-1-phosphate by sphingosine kinase: Oxidative stress and the seesaw of cell survival and death. Comp Biochem Physiol - B Biochem Mol Biol. 2012;163:26–36.
Gault CR, Obeid LM, Hannun YA. An overview of sphingolipid metabolism: from synthesis to breakdown. Adv Exp Med Biol. 2010;688:1–23.
Tan SF, Liu X, Fox TE, Barth BM, Sharma A, Turner SD, et al. Acid ceramidase is upregulated in AML and represents a novel therapeutic target. Oncotarget. 2016;7:83208–22.
Fordham SE, Matheson EC, Scott K, Irving JAE, Allan JM. DNA mismatch repair status affects cellular response to Ara-C and other anti-leukemic nucleoside analogs. Leukemia. 2011;25:1046–9.
Tan S-F, Dunton W, Liu X, Fox TE, Morad SAF, Desai D, et al. Acid ceramidase promotes drug resistance in acute myeloid leukemia through NF-κB-dependent P-glycoprotein upregulation. J Lipid Res. 2019;60:1078–86.
Dany M, Gencer S, Nganga R, Thomas RJ, Oleinik N, Baron KD, et al. Targeting FLT3-ITD signaling mediates ceramide-dependent mitophagy and attenuates drug resistance in AML. Blood. 2016;128:1944–58.
Kao L-P, Morad SAF, Davis TS, MacDougall MR, Kassai M, Abdelmageed N, et al. Chemotherapy selection pressure alters sphingolipid composition and mitochondrial bioenergetics in resistant HL-60 cells. J Lipid Res. 2019;60:1590–602.
Powell JA, Lewis AC, Zhu W, Toubia J, Pitman MR, Wallington-Beddoe CT, et al. Targeting sphingosine kinase 1 induces MCL1-dependent cell death in acute myeloid leukemia. Blood. 2017;129:771–82.
Ramsey HE, Fischer MA, Lee T, Gorska AE, Arrate MP, Fuller L, et al. A novel MCL1 inhibitor combined with venetoclax rescues venetoclax-resistant acute myelogenous Leukemia. Cancer Discov. 2018;8:1566–81.
Senchenkov A, Litvak DA, Cabot MC. Targeting ceramide metabolism—a strategy for overcoming drug resistance. J Natl Cancer Inst. 2001;93:347–57.
Toffalori C, Zito L, Gambacorta V, Riba M, Oliveira G, Bucci G, et al. Immune signature drives leukemia escape and relapse after hematopoietic cell transplantation. Nat Med Nat Publ Group. 2019;25:603–11.
Liao D, Wang M, Liao Y, Li J, Niu T. A review of efficacy and safety of checkpoint inhibitor for the treatment of acute myeloid leukemia. Frontiers in Pharmacology. Frontiers Media S.A.; 2019. vol. 10.
Deng M, Gui X, Kim J, Xie L, Chen W, Li Z, et al. LILRB4 signalling in leukaemia cells mediates T cell suppression and tumour infiltration. Nature. 2018;562:605–9.
Baitsch D, Bock HH, Engel T, Telgmann R, Müller-Tidow C, Varga G, et al. Apolipoprotein e induces antiinflammatory phenotype in macrophages. Arterioscler Thromb Vasc Biol. 2011;31:1160–8.
Gui X, Deng M, Song H, Chen Y, Xie J, Li Z, et al. Disrupting LILRB4/APOE interaction by an efficacious humanized antibody reverses T-cell suppression and blocks AML development. Cancer Immunol Res. 2019;7:1244–57.
John S, Chen H, Deng M, Gui X, Wu G, Chen W, et al. A novel anti-LILRB4 CAR-T cell for the treatment of monocytic AML. Mol Ther. 2018;26:2487–95.
Yang H, Bueso-Ramos C, Dinardo C, Estecio MR, Davanlou M, Geng QR, et al. Expression of PD-L1, PD-L2, PD-1 and CTLA4 in myelodysplastic syndromes is enhanced by treatment with hypomethylating agents. Leukemia. 2014;28:1280–8.
Daver N, Boddu P, Garcia-Manero G, Yadav SS, Sharma P, Allison J, et al. Hypomethylating agents in combination with immune checkpoint inhibitors in acute myeloid leukemia and myelodysplastic syndromes. Leukemia. 2018;32:1094–105.
Kang X, Lu Z, Cui C, Deng M, Fan Y, Dong B, et al. The ITIM-containing receptor LAIR1 is essential for acute myeloid leukaemia development. Nat Cell Biol. 2015;17:665–77.
Maifrede S, Nieborowska-Skorska M, Sullivan-Reed K, Dasgupta Y, Podszywalow-Bartnicka P, Le BV, et al. Tyrosine kinase inhibitor–induced defects in DNA repair sensitize FLT3(ITD)-positive leukemia cells to PARP1 inhibitors. Blood. 2018;132:67–77.
Weaver AN, Yang ES. Beyond DNA repair: additional functions of PARP-1 in cancer. Front Oncol. 2013;3:290.
Yélamos J, Moreno-Lama L, Jimeno J, Ali SO. Immunomodulatory roles of PARP-1 and PARP-2: impact on PARP-centered cancer therapies. Cancers. 2020;12:392.
Aurelius J, Thorén FB, Akhiani AA, Brune M, Palmqvist L, Hansson M, et al. Monocytic AML cells inactivate antileukemic lymphocytes: Role of NADPH oxidase/gp91 phox expression and the PARP-1/PAR pathway of apoptosis. Blood 2012;119:5832–7.
Thorén FB, Romero AI, Hellstrand K. Oxygen radicals induce Poly(ADP-Ribose) polymerase-dependent cell death in cytotoxic lymphocytes. J Immunol. 2006;176:7301–7.
Nilsson MS, Hallner A, Brune M, Nilsson S, Thorén FB, Martner A, et al. Immunotherapy with HDC/IL-2 may be clinically efficacious in acute myeloid leukemia of normal karyotype. Hum Vaccines Immunother. 2020;16:109–11.
Gasser S, Orsulic S, Brown EJ, Raulet DH. The DNA damage pathway regulates innate immune system ligands of the NKG2D receptor. Nature 2005;436:1186–90.
Paczulla AM, Rothfelder K, Raffel S, Konantz M, Steinbacher J, Wang H, et al. Absence of NKG2D ligands defines leukaemia stem cells and mediates their immune evasion. Nature. 2019;572:254–9.
Carlsten M, Järås M. Natural killer cells in myeloid malignancies: immune surveillance, nk cell dysfunction, and pharmacological opportunities to bolster the endogenous NK cells. Front Immunol. 2019;10:2357.
Li X, Li C, Jin J, Wang J, Huang J, Ma Z, et al. High PARP-1 expression predicts poor survival in acute myeloid leukemia and PARP-1 inhibitor and SAHA-bendamustine hybrid inhibitor combination treatment synergistically enhances anti-tumor effects. EBioMed. 2018;38:47–56.
Molenaar RJ, Radivoyevitch T, Nagata Y, Khurshed M, Przychodzen B, Makishima H, et al. Idh1/2 mutations sensitize acute myeloid leukemia to parp inhibition and this is reversed by idh1/2-mutant inhibitors. Clin Cancer Res. 2018;24:1705–15.
Dellomo AJ, Baer MR, Rassool FV. Partnering with PARP inhibitors in acute myeloid leukemia with FLT3-ITD. Cancer Lett. 2019;454:171–8.
Gojo I, Beumer JH, Pratz KW, McDevitt MA, Baer MR, Blackford AL, et al. A phase 1 study of the PARP inhibitor veliparib in combination with temozolomide in acute myeloid leukemia. Clin Cancer Res. 2017;23:697–706.
Esposito MT, Zhao L, Fung TK, Rane JK, Wilson A, Martin N, et al. Synthetic lethal targeting of oncogenic transcription factors in acute leukemia by PARP inhibitors. Nat Med. 2015;21:1481–90.
Phan LM, Yeung SCJ, Lee MH. Cancer metabolic reprogramming: importance, main features, and potentials for precise targeted anti-cancer therapies. Cancer Biol Med. 2014;11:1–19.
Patra KC, Hay N. The pentose phosphate pathway and cancer. Trends Biochem Sci. 2014;39:347–54.
Reczek CR, Chandel NS. The Two Faces of Reactive Oxygen Species in Cancer. Annu Rev Cancer Biol. 2017;1:79–98.
Ribas V, García-Ruiz C, Fernández-Checa JC. Glutathione and mitochondria. Front Pharmacol. 2014;5:151.
Hole PS, Zabkiewicz J, Munje C, Newton Z, Pearn L, White P, et al. Overproduction of NOX-derived ROS in AML promotes proliferation and is associated with defective oxidative stress signaling. Blood. 2013;122:3322–30.
Hole PS, Pearn L, Tonks AJ, James PE, Burnett AK, Darley RL, et al. Ras-induced reactive oxygen species promote growth factor - Independent proliferation in human CD34+ hematopoietic progenitor cells. Blood. 2010;115:1238–46.
Jayavelu AK, Moloney JN, Böhmer FD, Cotter TG. NOX-driven ROS formation in cell transformation of FLT3-ITD-positive AML. Exp Hematol. 2016;44:1113–22.
Sengupta A, Arnett J, Dunn S, Williams DA, Cancelas JA. Rac2 GTPase deficiency depletes BCR-ABL+ leukemic stem cells and progenitors in vivo. Blood. 2010;116:81–4.
Pick E. Role of the Rho GTPase Rac in the activation of the phagocyte NADPH oxidase: outsourcing a key task. Small GTPases. 2014;5:e27952.
Aydin E, Hallner A, Grauers Wiktorin H, Staffas A, Hellstrand K, Martner A. NOX2 inhibition reduces oxidative stress and prolongs survival in murine KRAS-induced myeloproliferative disease. Oncogene. 2019;38:1534–43.
Adane B, Ye H, Khan N, Pei S, Minhajuddin M, Stevens BM, et al. The hematopoietic oxidase NOX2 regulates self-renewal of leukemic stem cells. Cell Rep. 2019;27:238–254.e6.
Prata C, Maraldi T, Fiorentini D, Zambonin L, Hakim G, Landi L. Nox-generated ROS modulate glucose uptake in a leukaemic cell line. Free Radic Res. 2008;42:405–14.
Bonello S, Zähringer C, BelAiba RS, Djordjevic T, Hess J, Michiels C, et al. Reactive oxygen species activate the HIF-1α promoter via a functional NFκB site. Arterioscler Thromb Vasc Biol. 2007;27:755–61.
Mucaj V, Shay JES, Simon MC. Effects of hypoxia and HIFs on cancer metabolism. Int J Hematol. 2012;95:464–70.
Marlein CR, Zaitseva L, Piddock RE, Robinson SD, Edwards DR, Shafat MS, et al. NADPH oxidase-2 derived superoxide drives mitochondrial transfer from bone marrow stromal cells to leukemic blasts. Blood. 2017;130:1649–60.
Moschoi R, Imbert V, Nebout M, Chiche J, Mary D, Prebet T, et al. Protective mitochondrial transfer from bone marrow stromal cells to acute myeloid leukemic cells during chemotherapy. Blood. 2016;128:253–64.
Pollyea DA, Stevens BM, Jones CL, Winters A, Pei S, Minhajuddin M, et al. Venetoclax with azacitidine disrupts energy metabolism and targets leukemia stem cells in patients with acute myeloid leukemia. Nat Med. 2018;24:1859–66.
Shi L, Pan H, Liu Z, Xie J, Han W. Roles of PFKFB3 in cancer. Signal Transduct Target Ther. 2017;2:17044.
Feng Y, Wu L. mTOR up-regulation of PFKFB3 is essential for acute myeloid leukemia cell survival. Biochem Biophys Res Commun. 2017;483:897–903.
Masoud GN, Li W. HIF-1α pathway: role, regulation and intervention for cancer therapy. Acta Pharma Sinica B. 2015;5:378–89.
Robinson AJ, Hopkins GL, Rastogi N, Hodges M, Doyle M, Davies S, et al. Reactive oxygen species drive proliferation in acute myeloid leukemia via the glycolytic regulator PFKFB3. Cancer Res. 2020;80:937–49.
Qian S, Li J, Hong M, Zhu Y, Zhao H, Xie Y, et al. TIGAR cooperated with glycolysis to inhibit the apoptosis of leukemia cells and associated with poor prognosis in patients with cytogenetically normal acute myeloid leukemia. J Hematol Oncol. 2016;9:128.
Degos L, Wang ZY. All trans retinoic acid in acute promyelocytic leukemia. Oncogene. 2001;20:7140–5.
Mughal TI, Ejaz AA, Foringer JR, Coiffier B. An integrated clinical approach for the identification, prevention, and treatment of tumor lysis syndrome. Cancer Treat Rev. 2010;36:164–76.
Löffler M, Jöckel J, Schuster G, Becker C. Dihydroorotat-ubiquinone oxidoreductase links mitochondria in the biosynthesis of pyrimidine nucleotides. Mol Cell Biochem. 1997;174:125–9.
Levine RL, Hoogenraad NJ, Kretchmer N. A review: Biological and clinical aspects of pyrimidine metabolism. Pediatr Res. 1974;8:724–34.
Sykes DB, Kfoury YS, Mercier FE, Wawer MJ, Law JM, Haynes MK, et al. Inhibition of dihydroorotate dehydrogenase overcomes differentiation blockade in acute myeloid leukemia. Cell. 2016;167:171–86.e15.
Wu D, Wang W, Chen W, Lian F, Lang L, Huang Y, et al. Pharmacological inhibition of dihydroorotate dehydrogenase induces apoptosis and differentiation in acute myeloid leukemia cells. Haematologica. 2018;103:1472–83.
Christian S, Merz C, Evans L, Gradl S, Seidel H, Friberg A, et al. The novel dihydroorotate dehydrogenase (DHODH) inhibitor BAY 2402234 triggers differentiation and is effective in the treatment of myeloid malignancies. Leukemia. 2019;33:2403–15.
Zhou J, Quah JY, Ng Y, Chooi J-Y, Toh SH-M, Lin B, et al. ASLAN003, a potent dihydroorotate dehydrogenase inhibitor for differentiation of acute myeloid leukemia. Haematologica. 2019. https://doi.org/10.3324/haematol.2019.230482.
Cao L, Weetall M, Trotta C, Cintron K, Ma J, Kim MJ, et al. Targeting of hematologic malignancies with PTC299, a novel potent inhibitor of dihydroorotate dehydrogenase with favorable pharmaceutical properties. Mol Cancer Ther. 2019;18:3–16.
Sykes DB. The emergence of dihydroorotate dehydrogenase (DHODH) as a therapeutic target in acute myeloid leukemia. Expert Opinion Ther Targets. 2018;22:893–8.
Vélez J, Hail N, Konopleva M, Zeng Z, Kojima K, Samudio I, et al. Mitochondrial uncoupling and the reprograming of intermediary metabolism in leukemia cells. Front Oncol. 2013;3:67.
Jóźwiak P, Forma E, Bryś M, Krześlak A. O-GlcNAcylation and metabolic reprograming in cancer. Front Endocrinol (Lausanne). 2014;5:145.
Itkonen HM, Mills IG. N-linked glycosylation supports cross-talk between receptor tyrosine kinases and androgen receptor. PLoS ONE. 2013;8:e65016.
Wagner FF, Benajiba L, Campbell AJ, Weïwer M, Sacher JR, Gale JP, et al. Exploiting an asp-glu “switch” in glycogen synthase kinase 3 to design paralog-selective inhibitors for use in acute myeloid leukemia. Sci Transl Med. 2018;10:eaam8460.
Sexauer AN, Do B, Sykes DB. Loss of FLT3 sensitizes myeloid cells to differentiation Via DHODH inhibition. Blood. 2019;134(Supplement_1):2712–2712.
Estey E, Levine RL, Löwenberg B. Current challenges in clinical development of “targeted therapies”: the case of acute myeloid leukemia. Blood. 2015;125:2461–6.
Wei AH, Strickland SA, Hou JZ, Fiedler W, Lin TL, Walter RB, et al. Venetoclax combined with low-dose cytarabine for previously untreated patients with acute myeloid leukemia: Results from a phase Ib/II study. J Clin Oncol. 2019;37:1277–84.
DiNardo CD, Pratz K, Pullarkat V, Jonas BA, Arellano M, Becker PS, et al. Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Blood. 2019;133:7–17.
Acknowledgements
We apologize to colleagues whose work could not be cited due to space constraints. We thank Dr. Oliver T. Keppler for continuous support and Dr. Constanze Schneider for critical reading of the manuscript. HMB acknowledges funding from the Wilhelm-Sander Stiftung (2017.122.1). RN is supported by the graduate program Infection Research on Human Pathogens@MvPI at Max von Pettenkofer Institute, LMU. AS-I is supported by the Max Weber-Program of the State of Bavaria. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41375_2020_1069_MOESM1_ESM.pdf
Ceramide and sphingosine-1-phosphate (S1P) are involved in pro-apoptotic and pro-survival signaling of AML cells, respectively, as well as drug sensitivity.
Rights and permissions
About this article
Cite this article
Nair, R., Salinas-Illarena, A. & Baldauf, HM. New strategies to treat AML: novel insights into AML survival pathways and combination therapies. Leukemia 35, 299–311 (2021). https://doi.org/10.1038/s41375-020-01069-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-020-01069-1
- Springer Nature Limited
This article is cited by
-
A novel immunogenic cell death-related classification indicates the immune landscape and predicts clinical outcome and treatment response in acute myeloid leukemia
Cancer Cell International (2024)
-
Uncovering expression signatures of synergistic drug responses via ensembles of explainable machine-learning models
Nature Biomedical Engineering (2023)
-
Deletion of Mettl3 in mesenchymal stem cells promotes acute myeloid leukemia resistance to chemotherapy
Cell Death & Disease (2023)
-
Curcumin combined with arsenic trioxide in the treatment of acute myeloid leukemia: network pharmacology analysis and experimental validation
Journal of Cancer Research and Clinical Oncology (2023)
-
ILC1s control leukemia stem cell fate and limit development of AML
Nature Immunology (2022)