Abstract
Objective
To understand the characteristics of infants admitted to US NICUs.
Study design
2006–2014 linked birth certificate and hospital discharge data for potentially viable deliveries in Pennsylvania and South Carolina were used. NICU admissions were identified using revenue codes. NICU-admitted infants were categorized by gestational age (GA), birthweight, and condition severity (for GA 35+ weeks). We also assessed total patient days and trends over time.
Results
12% of infants were admitted to a NICU; 13.6% were GA < 32 weeks (45.3% of total days); 36.1% were GA 32–36 weeks (31.2% of total days); and 50.4% were GA 37+ weeks (23.5% of total days). 20% of admissions were for infants with GA 35+ weeks and mild conditions. Admissions increased numerically from 11.2% (2006) to 13.0% (2014), with increases among infants 35+ weeks.
Conclusion
Most NICU admissions are for infants 35+ weeks GA, many with mild conditions who may be accommodated in well-baby units.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
NICU admission rates have increased in the past several decades [1], with at least 10% of all infants receiving some level of NICU care [1,2,3,4]. Such care is essential and life-saving for many infants, especially those born preterm or with serious complications [5,6,7]. However, term infants with minor conditions may be admitted unnecessarily [1, 6], and studies have shown a high level of variation in NICU admission rates between facilities, particularly among lower acuity infants [1, 4, 8,9,10,11,12,13].
Understanding the characteristics of infants admitted to NICUs and their contributions to total NICU utilization may help contextualize trends in NICU admissions, further identify potential areas of variability in NICU admissions, and inform resource planning. However, NICU admissions have not been studied longitudinally at the population level (i.e., longitudinally within a discrete population) [3]. Further, many existing studies of NICU admissions rely only on birth certificate data, which substantially undercount NICU admissions and omit important clinical details [14, 15]. Additionally, most other studies explore NICU admissions in subgroups of infants, for example, focusing on specific gestational ages, birthweights, or condition severities in isolation [10, 12, 13, 16] without examining the overall population-based trends in such admissions.
Our study aims to describe population-level NICU admissions among all live births in Pennsylvania and South Carolina from 2006 to 2014. We use linked birth certificates and hospital discharge records to identify infants admitted to a NICU during initial admission to the hospital for delivery using revenue codes for neonatal intensive care services from the hospital discharge records, and divided such admissions by the severity of illness of the infants. We describe the characteristics of individuals (infants and their mothers), the general disposition of newborns (gestational age [GA], birthweight [BW]), the conditions leading to NICU admission and relative contribution of these conditions to total number of patient hospital days for the delivery admission, and potential trends over time.
Materials and methods
Data source and study sample
We used data from linked birth certificate and hospital discharge records for all births in Pennsylvania and South Carolina from 2006-2014. The process of linking birth certificates to discharge records has been shown to have a linkage rate of roughly 95% or higher [7, 16, 17].
Our analysis included potentially viable, liveborn infants (GA ≥ 22 weeks and BW ≥ 400 g) for in-hospital deliveries with birth certificates that could be linked to hospital discharge records. Infants were excluded if: their GA was <22 weeks, BW was <400 g, or GA and BW were missing and could not be accounted for using ICD-9 codes (n = 4738); their unique birth certificate identifier had an exact duplicate (in which case one record was retained and one was deleted) or non-exact duplicate with another record (in which case both records were deleted) (n = 330); or their birth certificate could not be linked to a hospital discharge record (n = 11,512). In total, 0.9% (16,580/1,751,277) of infant records were excluded based on these criteria, for a final sample of 1,734,697 infants. See Supplemental Fig. 1 for study flow.
Where possible, infant records were also linked to maternal hospital discharge records; however, since the goal of our analysis was to describe the infant population, babies whose records could not be linked to maternal discharge records were not excluded.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. It was approved by the Institutional Review Boards at Stanford University (protocol 38429), the Children’s Hospital of Philadelphia (protocol 16-013134), and the data agencies for Pennsylvania and South Carolina, with waivers of the need for informed consent for use of secondary data with no patient contact.
Measures
For each infant, we assessed NICU admission status and hospital length of stay (LOS, including both NICU and non-NICU days) for the delivery hospitalization using the hospital revenue codes for neonatal intensive care from hospital discharge records. These codes should be present for all NICU admissions as they are required for hospitals to receive the higher NICU payments. We defined NICU admission as any of the revenue codes associated with NICU care (identified by revenue codes 172, 173, or 174) during delivery hospitalization. Infants who were transferred (linked and unlinked) from their initial birth/delivery facility to another facility were also categorized as having a NICU admission, regardless of revenue code, under the assumption that any transfer was for care not available at the delivery hospital. Most transfers were linked and had a NICU revenue code.
We used information from birth certificates for the following newborn, delivery, and maternal characteristics: GA (weeks); BW (g); sex; plurality and mode of delivery; and mother’s age, race/ethnicity, education, and insurance type. Due to differences in birth certificate reporting over time, some characteristics (eg, mother’s education and insurance type) were frequently missing; we categorized infants with missing maternal data as missing/unknown and did not exclude them from our analysis. Missing (n = 5967) or implausible (>7500 g, n = 11) BW from birth certificates was supplemented using ICD-9 codes where available (n = 1621). Missing GA (n = 11,848) was supplemented using Kotelchuck imputation (using BW and sex, n = 11,634) where available, and using ICD-9 codes where BW was also missing (n = 214).
To understand the reasons leading to NICU admission for infants GA 35+ weeks, we categorized their condition acuity—based on ICD-9 codes in hospital discharge data—as mild/minor, moderate, or severe. Condition acuity definitions are described below and were based in part on those used in previous studies [12, 18]; the California Maternal Quality of Care (CMQCC), National Quality Forum, and The Joint Commission, definitions of unexpected moderate and severe complications in term newborns [19, 20]; and a review of ICD-9 codes and associated conditions in our dataset. We then further categorized infants into mutually exclusive groups based on highest level of condition acuity; for example, an infant with one mild condition and one moderate condition would be categorized in the “moderate is highest” group.
Minor/mild acuity was defined as: mild hyperbilirubinemia, mild hypoglycemia, neonatal abstinence syndrome (drug NAS), observation for suspected infection, mild respiratory condition, or LOS < 6 days (except for neonatal jaundice) for infants who did not have conditions that met criteria for moderate or severe. Moderate acuity was defined as: less serious but significant birth trauma, moderate respiratory complications, moderate neurological complications, or LOS > 5 days (except for those with jaundice or social problems) for infants who did not have conditions that met criteria for severe. Severe acuity was defined as: any anomaly with measurable mortality risk from prior work [18], use of extracorporeal membrane oxygenation (ECMO), pulmonary hypertension, aspiration syndrome, mechanical ventilation, intraventricular hemorrhage grade 3 or 4, major surgery, severe hypoxia/asphyxia, severe respiratory complications, severe neurological complications, serious infection, shock, or in-hospital death. See Supplementary Table 1 for detailed acuity definitions and their specific conditions (including ICD-9 codes).
In our analysis, we used descriptive statistics to understand relative proportions of NICU admissions and total patient days by GA and BW. We also assessed total patient days, transfer status, and survival for very preterm infants (GA 22-31 weeks) who did not have a documented NICU admission by revenue code, since it is generally standard practice to admit to a NICU all very preterm liveborn infants.
We further assessed the contribution of mild, moderate, and severe condition acuity among infants with GA 35+ weeks to overall NICU admissions and total patient days. To understand whether NICU admission rates have changed over time, we tabulated NICU admissions from 2006 to 2014 by GA; BW; condition acuity among infants with GA 35+ weeks; and for specific newborn conditions leading to NICU admission among infants with GA 35+ weeks.
We performed our analysis using Stata version 17.1 (Stata Statistical Software: Release 17. College Station, TX: StataCorp LP). Code available upon reasonable request.
Results
Of 1,734,697 infants meeting eligibility criteria, 12.0% (n = 207,645) were admitted to a NICU in Pennsylvania and South Carolina during the analysis period. Slightly less than half of infants (49.6%) admitted to a NICU were preterm (GA < 37 weeks), and less than half (42.8%) had low BW (BW < 2500 g). NICU-admitted infants accounted for more than 3.4 million hospital days, with a mean LOS of 16 days (vs 3 days for non-admitted infants). Table 1 provides additional characteristics of infants in our analysis.
Overall, a higher proportion of infants born to Black mothers were admitted to a NICU compared to infants born to mothers of other races and ethnicities (15.4% for infants born to Black mothers vs ~11% for infants of other races and ethnicities). NICU admissions generally decreased with increasing maternal educational attainment (13.2% for infants born to mothers with less than a high school education, vs 10.3% for infants born to mothers with a 4-year college degree or more), and those with government insurance had a higher admission rate than other insurance/payment types (Table 1). Nearly all extremely or very preterm and low BW infants were admitted to a NICU (>92%); most (91.6%) extremely preterm infants who were not admitted to a NICU died shortly after delivery.
In terms of NICU care utilization by GA, infants who were 22-31 weeks GA made up 13.6% of NICU admissions and 45.3% of total patient days. Infants 32–36 weeks GA accounted for 36.1% of NICU admissions and 31.2% of patient days. Infants 37+ weeks GA were 50.4% of the admitted population and had 23.5% of patient days. Admissions and total patient days followed similar trends by birthweight. Figure 1 provides proportions of NICU admissions and total patient days by GA and BW.
Admissions, total patient days, and condition acuity in infants 35+ weeks GA
Infants GA 35+ weeks made up 66.2% of the overall NICU-admitted population and accounted for 33.1% of total patient days (1,124,480/3,393,518 days) (Table 2). Those with only minor/mild conditions were 20% of all NICU admissions (19.9%; 41,393/137,458), but accounted for only 4.0% of total patient days (134,046 days). More than 25% of infants admitted to NICUs were 35+ weeks GA with moderate condition acuity (25.6%), and 20.7% were 35+ weeks GA with severe condition acuity. Table 2 provides additional details on condition acuity among infants 35 + GA admitted to NICUs.
Nearly 9% (8.9%) of all NICU admissions were for infants 35+ weeks with only one of the 5 specified mild/minor conditions—most commonly hyperbilirubinemia and observation for suspected infection. Nearly 6% (5.9%, 12,247/207,521) of all NICU admissions were in infants with GA 35+ weeks who had hyperbilirubinemia and mild acuity; most of these infants (66.6%; 8,151/12,247) had only hyperbilirubinemia and no other specified conditions (Table 2).
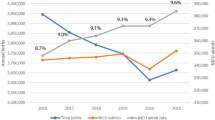
Secular trends in NICU admissions from 2006 to 2014
Over time, the number of deliveries in Pennsylvania and South Carolina decreased slightly from 200,003 infants in 2006 to 188,585 in 2014; and the proportion of infants born preterm (GA < 37 weeks) also decreased from 11.2% in 2006 to 9.9% in 2014 (See Supplemental Table 2). Conversely, the absolute number and percentage of newborns admitted to a NICU increased numerically from 11.2% (22,242/200,003) in 2006 to 13.0% (24,580/188,587) in 2014.
The observed numeric increase in absolute number of NICU admissions was among infants born 35+ weeks across all condition acuities. The proportion of NICU-admitted infants with mild condition acuity increased by 20% (2.1% to 2.5%), those with moderate condition acuity increased by 37% (2.7% to 3.7%), and infants with severe condition acuity increased by 22% (2.3% to 2.8%). See Fig. 2 for trends in admissions over time.
Definitions of severity: Mild only: one or more of mild hyperbilirubinemia, mild hypoglycemia, mild drug NAS (neonatal abstinence syndrome), observation for suspected infection, mild respiratory condition, LOS < 6 days (except jaundice or social problems), and conditions that did not meet criteria for moderate or severe. Moderate is highest: less serious but significant birth trauma, respiratory complications, and neurological complications, as well as LOS > 5 days (except for those with jaundice) and the absence of conditions defined as severe, as defined by CMQCC. Severe is highest: any serious anomaly with measurable mortality risk, ECMO, pulmonary hypertension, aspiration syndrome, mechanical ventilation, intraventricular hemorrhage grade 3 or 4, major surgery, severe hypoxia/asphyxia, shock/resuscitation, serious infection or septicemia, severe birth trauma, severe neurological complications, severe respiratory complications, or in-hospital death. NAS neonatal abstinence syndrome.
Among infants with mild condition acuity, the absolute proportion admitted to a NICU with hyperbilirubinemia as the sole specified condition varied during the observation period, with a high of 4.6% in 2008 and then generally decreased to 3.3% in 2014. The proportion of NICU-admitted infants with GA 35+ weeks and only mild suspected infection generally increased numerically. See Supplemental Table 2 for additional details regarding trends in time among the NICU-admitted population.
Discussion
In our analysis, we found that 12% of infants born during the analysis period in Pennsylvania and South Carolina were admitted to a NICU. The majority of admissions were in near-term or term infants (GA 35+ weeks), and one-fifth of all NICU admissions were for infants with mild condition acuity. While infants with higher GA and BW made up a large proportion of admissions, they accounted for a much lower relative proportion of hospital days. Importantly, we found that over time, the overall percentage of infants admitted to a NICU increased numerically from 2006 to 2014, with increases occurring among infants with GA 35+ weeks.
Our analysis helps to address a relative dearth of information regarding NICU admissions at the population level, and it expands the understanding of these conditions by documenting their prevalence and estimating care utilization among newborns with these conditions longitudinally in two discrete states. Information regarding NICU admissions—and particularly the characteristics of NICU-admitted newborns and conditions leading to admission—is critical to future policies and guidelines regarding maternal and newborn care and resource allocation. Our findings may useful in the implementation of initiatives to help improve outcomes, as term NICU admissions are a potential target for quality improvement programming, may be markers of value of care, or may indicate potential NICU overutilization [3, 21, 22].
Lower-acuity infants may receive care through well-baby units, which can improve healthcare experiences and reduce healthcare costs, without increasing risks to newborns [4, 23, 24]. This issue should not be taken lightly, since NICU admissions (when not clearly indicated) may increase the risk of unnecessary intervention, medication errors, and infection—particularly among infants GA 35+ weeks with minor conditions [25, 26]. Further, NICU admission can cause distress for parents and are associated with an increased risk of maternal mental illness; it may also interfere with parental-infant bonding and breastfeeding [27, 28]. Such risks may have both short- and long-term implications for infants and their families. Accommodating lower-acuity infants in well-baby units may also help focus NICU care on preterm newborns and those with moderate and severe conditions. That said, delays in NICU admission among infants whose conditions warrant additional care may also lead to longer lengths of stay and hospital readmissions. Additionally, while recent changes to guidelines and management protocols (for example, higher thresholds for phototherapy to treat jaundice in otherwise healthy newborns, and the availability of phototherapy in well-baby nurseries [29,30,31]) may further enable care for low-acuity infants GA 35+ weeks in well-baby units, other changes to hospital-based care for newborns (for example, increased rooming-in practices) may make non-NICU care for marginal newborns more challenging (like those with meconium exposure or suspected infection who may require more frequent monitoring).
Further, several studies have shown a high level of variation in NICU admission rates between facilities [1, 4, 8, 9]—variation that is not fully explained by variation in the severity of conditions for which infants are admitted [9,10,11,12,13]. This has raised substantial concerns that supply-side factors, like NICU bed availability and financial incentives, may influence NICU admissions in term infants with mild conditions [11, 32]. While our study does not specifically explore variability in or modifiability of NICU admissions, our expanded definition of condition acuity and use of a robust and population-level dataset may help inform future studies. Factors affecting facility-level variability in NICU admissions within levels of condition acuity, including potential differences in clinical practices (i.e., provider habits), care organization (i.e., care available in well-baby units), and other health system factors (e.g., bed availability and payment structures), should be explored further.
Our findings are consistent with other studies of NICU admissions, which found similar proportions of NICU admissions overall [3], and substantial proportions of admissions that were among infants with relatively high gestational ages and birthweights but low condition acuity [1, 2, 9, 12]. Differences in relative proportions of NICU admissions by mother’s race, ethnicity, and education level in our analysis compared to other studies are likely due to demographic differences in study populations; for example, our study includes all linked infants born in Pennsylvania and South Carolina, while other recent studies of NICU admissions were among cohorts born in California [2, 3, 12] or among US birth cohorts [1, 33].
We found a higher overall rate of admissions than what was found in several other studies [1, 33], which is to be expected, given our use of hospital revenue codes as opposed to birth certificate data [15, 17, 34]. However, our finding of a numeric increase in overall NICU admissions (from 11.2% in 2006 to 13.0% in 2014) is similar in magnitude and direction to that of Harrison and Goodman (from 6.4% in 2007 to 7.8% in 2012) and Kim (6.6% in 2008 to 9.1% in 2018) [1, 33]. An analysis by Braun et al., conducted in a large, integrated healthcare system in California found a similar overall rate of admissions (12.2% overall from 2010 to 2018), but a decrease in NICU admissions over time, especially among larger infants with lower condition acuity [3]. However, as the authors note, several “systemwide quality improvement initiatives” were implemented during the study period (such as risk calculators and strategies affecting timing and mode of delivery), each of which has been found to reduce NICU admissions in other studies [3].
The observed yearly increases in NICU admissions for infants GA 35+ weeks with moderate or severe condition acuity may be due to changes over time in how more severe conditions are identified and managed (e.g., technology to aid in the identification of serious anomalies) [35]. It may also be due to other factors, like changes in the maternal population (increases in maternal age, use of assisted reproductive technologies, metabolic conditions) [36,37,38,39], increases in the use of interventions during delivery [40,41,42], or other factors, such as changes in the way conditions are diagnosed or coded [33, 43]. Future studies should further assess the potential statistical significance of differences among groups and over time, along with drivers of increases in conditions leading to admissions.
Our study has some limitations, including differences in ICD coding between health facilities and between states, and missingness of data, especially for mothers, due to inconsistent tracking of some demographic data in birth certificates. However, we did not exclude infants based on missingness of maternal data, and our use of hospital discharge data—including revenue codes and ICD codes—is a major strength versus using birth certificate data alone. While our use of hospital discharge data may still result in some missed or misclassified NICU admissions or newborn conditions, the prevalence of such errors is lower than that of birth certificates, as described below. Second, among infants admitted to a NICU and sent back to a newborn nursery or vice versa, determining the number of days spent in the NICU cannot be obtained from our data. Also, infants who spend a few hours in a NICU are billed and coded the same amount as infants spending a complete day in the NICU, with differences in resources used between the patients. Lastly, due to the highly detailed and granular nature of billing data and the numerous potential conditions that may arise in newborns, our definitions of condition acuity may differ from those in other studies. For example, our moderate condition acuity group includes infants with a length of stay longer than 5 days for conditions not specified as severe; some infants in this group may have conditions that, if assessed at the individual level, may be considered severe by clinicians.
Our study has several strengths, most notably our use of hospital revenue codes to identify NICU admissions, as compared to studies relying on birth certificate data alone, which can miss as many as 40% of NICU admissions, have low sensitivity for some conditions, and are sometimes completed before clinical conditions arise during admission [17, 34]. Given that NICU revenue codes must be included in the discharge record for the hospital to receive the higher payment for infants cared for in the NICU, it is reasonable to assume that the revenue codes are included for all infants who were actually admitted to a NICU. We also used ICD-9 codes to better understand and appropriately define condition acuity within our study. Another strength is the size and duration of the analytic sample, covering the vast majority of liveborn infants in all birth facilities over nearly 10 years in 2 states in the US. However, NICU admissions and conditions leading to admission may differ in other states.
While our study provides descriptive details regarding infants admitted to NICUs—given the paucity of recent representative data on the subject—further studies should explore variability in NICU admissions among infants 35+ weeks GA (especially in those with lower condition acuity) to understand potential drivers of admissions, including maternal factors and facility factors. Future studies should also assess differences in admissions within and among groups and changes over time.
Conclusion
Of the 12% of infants admitted to NICUs during our study period, 20% were considered to be low acuity based on gestational age and condition severity. These infants make up a substantial portion of the NICU population; understanding this population and its contribution to NICU utilization may help inform reorganization of care. Low-acuity infants may benefit from non-NICU care in well-baby (or similar) nurseries. This may help focus NICU care on higher acuity infants, reduce risks and improve experiences among low-risk infants and their families, and reduce costs. Future studies should assess variability in NICU admissions between hospitals, resource utilization for NICU-admitted infants by varying condition severities, and changes in the NICU-admitted population over time.
Data availability
Data used in this analysis contain identifiable personal health information and were obtained through data use agreements with each state that prohibit any sharing of these data. Others wanting access to these data would need to obtain their own data use agreements with the individual state departments of health.
References
Harrison W, Goodman D. Epidemiologic trends in neonatal intensive care, 2007–2012. JAMA Pediatr. 2015;169:855–62.
Schulman J, Braun D, Lee HC, Profit J, Duenas G, Bennett MV, et al. Association between neonatal intensive care unit admission rates and illness acuity. JAMA Pediatr. 2018;172:17–23.
Braun D, Braun E, Chiu V, Burgos AE, Gupta M, Volodarskiy M, et al. Trends in neonatal intensive care unit utilization in a large integrated health care system. JAMA Netw Open. 2020;3:e205239.
Tex NICU Project. Improving the identification of quality and value in newborn care in Texas. 2019. https://www.ncbi.nlm.nih.gov/books/NBK584999/bin/Texas_NICU_Project_Final_Report_Appendix_20190402.pdf.
Williams RL, Chen PM. Identifying the sources of the recent decline in perinatal mortality rates in California. N Engl J Med. 1982;306:207–14.
Horbar JD, Badger GJ, Carpenter JH, Fanaroff AA, Kilpatrick S, LaCorte M, et al. Trends in mortality and morbidity for very low birth weight infants, 1991-1999. Pediatrics. 2002;110:143–51.
Lorch SA, Baiocchi M, Ahlberg CE, Small DS. The differential impact of delivery hospital on the outcomes of premature infants. Pediatrics. 2012;130:270–8.
Harrison WN, Wasserman JR, Goodman DC. Regional variation in neonatal intensive care admissions and the relationship to bed supply. J Pediatr. 2018;192:73–9.e4.
Edwards EM, Horbar JD. Variation in use by NICU types in the United States. Pediatrics. 2018;142:e20180457.
Ziegler KA, Paul DA, Hoffman M, Locke R. Variation in NICU admission rates without identifiable cause. Hosp Pediatr. 2016;6:255–60.
Freedman S. Capacity and utilization in health care: the effect of empty beds on neonatal intensive care admission. Am Econ J Econ Policy. 2016;8:154–85.
Haidari ES, Lee HC, Illuzzi JL, Phibbs CS, Lin H, Xu X. Hospital variation in admissions to neonatal intensive care units by diagnosis severity and category. J Perinatol. 2021;41:468–77.
Mahendra M, Steurer-Muller M, Hohmann SF, Keller RL, Aswani A, Dudley RA. Predicting NICU admissions in near-term and term infants with low illness acuity. J Perinatol. 2021;41:478–85.
Northam S, Knapp TR. The reliability and validity of birth certificates. J Obstet Gynecol Neonatal Nurs. 2006;35:3–12.
Haidari ES, Lee HC, Illuzzi JL, Lin H, Xu X. Utility of birth certificate data for evaluating hospital variation in admissions to NICUs. Hosp Pediatr. 2020;10:190–4.
Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH. Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med. 2007;356:2165–75.
Herrchen B, Gould JB, Nesbitt TS. Vital statistics linked birth/infant death and hospital discharge record linkage for epidemiological studies. Comput Biomed Res Int J. 1997;30:290–305.
Phibbs CS, Passarella M, Schmitt SK, Rogowski JA, Lorch SA. Understanding the relative contributions of prematurity and congenital anomalies to neonatal mortality. J Perinatol. 2022;42:569–73.
NQF: Quality Positioning SystemTM Unexpected Newborn Complications in Term Infants [Internet]. [cited 19 Oct 2022]. Available from: https://www.qualityforum.org/QPS/QPSTool.aspx?m=53#qpsPageState=%7B%22TabType%22%3A1,%22TabContentType%22%3A2,%22ItemsToCompare%22%3A%5B%5D,%22StandardID%22%3A53,%22EntityTypeID%22%3A1%7D.
Specifications Manual for Joint Commission National Quality Measures (v2019A) [Internet]. 2019 [cited 19 Oct 2022]. Available from: https://manual.jointcommission.org/releases/TJC2019A/MIF0393.html.
Clapp MA, James KE, Bates SV, Kaimal AJ. Unexpected term NICU admissions: a marker of obstetrical care quality? Am J Obstet Gynecol. 2019;220:395.e1–395.e12.
Pursley DM, Zupancic JAF. Using neonatal intensive care units more wisely for at-risk newborns and their families. JAMA Netw Open. 2020;3:e205693.
Goodman DC, Wasserman JR, Mowitz ME, Gilbert J, Stukel TA, Ganduglia-Cazaban C. Neonatal intensive care utilization and postdischarge newborn outcomes: a population-based study of Texas Medicaid insured infants. J Pediatr. 2021;236:62–9.e3.
Clemans-Cope L, Holla N, Lee HC, Cong AS, Castro R, Chyi L, et al. Neonatal abstinence syndrome management in California birth hospitals: results of a statewide survey. J Perinatol. 2020;40:463–72.
Polin RA, Denson S, Brady MT, Papile LA, Baley JE, Carlo WA, et al. Epidemiology and diagnosis of health care–associated infections in the NICU. Pediatrics. 2012;129:e1104–9.
Sharek PJ, Horbar JD, Mason W, Bisarya H, Thurm CW, Suresh G, et al. Adverse events in the neonatal intensive care unit: development, testing, and findings of an NICU-focused trigger tool to identify harm in North American NICUs. Pediatrics. 2006;118:1332–40.
Wyatt T, Shreffler KM, Ciciolla L. Neonatal intensive care unit admission and maternal postpartum depression. J Reprod Infant Psychol. 2019;37:267–76.
Affleck G, Tennen H. The effect of newborn intensive care on parents’ psychological well-being. Child Health Care J Assoc Care Child Health. 1991;20:6–14.
Beverstock AM, Rubin L, Akerman M, Noyola E. Reducing the time to action on bilirubin results overnight in a newborn nursery. Pediatr Qual Saf. 2023;8:e707.
Cahill C, Jegatheesan P, Song D, Cortes M, Adams M, Narasimhan SR, et al. Implementing higher phototherapy thresholds for jaundice in healthy infants 35 plus weeks. Hosp Pediatr. 2023;13:857–64.
Sukkar S, Lorusso G, Jananeh S, Harrison R, Martin MA, Grabois E, et al. Decreasing bilirubin serum tests in healthy newborns during birth hospitalization. Pediatrics. 2023;151:e2022059474.
Carroll AE. The concern for supply-sensitive neonatal intensive care unit care: if you build them, they will come. JAMA Pediatr. 2015;169:812–3.
Kim Y, Ganduglia-Cazaban C, Chan W, Lee M, Goodman DC. Trends in neonatal intensive care unit admissions by race/ethnicity in the United States, 2008–2018. Sci Rep. 2021;11:23795.
Phibbs CS. Identifying NICU admissions from secondary data: Differences between birth certificates and discharge abstracts. Poster presented at: Pediatric Academic Societies 2019 Meeting; 24 May 2019; Baltimore, MD.
Straub L, Huybrechts KF, Bateman BT, Mogun H, Gray KJ, Holmes LB, et al. The impact of technology on the diagnosis of congenital malformations. Am J Epidemiol. 2019;188:1892–901.
Addicott K, Nudelman M, Putty K, Prasher P, Preston D, Yoost JL, et al. Adverse perinatal outcomes associated with increasing maternal obesity. Am J Perinatol. 2024;41:1275–281.
Venkatesh KK, Huang X, Cameron NA, Petito LC, Joseph J, Landon MB, et al. Rural–urban disparities in pregestational and gestational diabetes in pregnancy: serial, cross-sectional analysis of over 12 million pregnancies. BJOG Int J Obstet Gynaecol. [cited 12 Sept 2023]. https://onlinelibrary.wiley.com/doi/abs/10.1111/1471-0528.17587.
Mauser S, Berghella V, Oliver EA. Birthweight is increasing in the United States. Am J Obstet Gynecol. 2023;5:100947.
Cameron NA, Everitt I, Seegmiller LE, Yee LM, Grobman WA, Khan SS. Trends in the incidence of new-onset hypertensive disorders of pregnancy among rural and Urban Areas in the United States, 2007 to 2019. J Am Heart Assoc. 2022;11:e023791.
Ashton DM. Elective delivery at less than 39 weeks. Curr Opin Obstet Gynecol. 2010;22:506–10.
Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial/ethnic disparities in obstetric outcomes and care: prevalence and determinants. Am J Obstet Gynecol. 2010;202:335–43.
Clark SL, Miller DD, Belfort MA, Dildy GA, Frye DK, Meyers JA. Neonatal and maternal outcomes associated with elective term delivery. Am J Obstet Gynecol. 2009;200:156.e1–4.
Blackmon LR, Barfield WD, Stark AR. Hospital neonatal services in the United States: variation in definitions, criteria, and regulatory status, 2008. J Perinatol. 2009;29:788–94.
Acknowledgements
Pennsylvania data: The Pennsylvania Health Care Cost Containment Council (PHC4) is an independent state agency responsible for addressing the problem of escalating health costs, ensuring the quality of health care, and increasing access to health care for all citizens regardless of ability to pay. PHC4 has provided data to this entity in an effort to further PHC4’s mission of educating the public and containing health care costs in Pennsylvania. PHC4, its agents, and staff, have made no representation, guarantee, or warranty, express or implied, that the data — financial, patient, payor, and physician specific information—provided to this entity, are errorfree, or that the use of the data will avoid differences of opinion or interpretation. This analysis was not prepared by PHC4. This analysis was done by the research team, including CSH, SS, MP, SAL, and CSP. PHC4, its agents and staff, bear no responsibility or liability for the results of the analysis, which are solely the opinion of this entity.
South Carolina data: This information is from the records of the Revenue and Fiscal Affairs Office, Health and Demographics Section, South Carolina. Our authorization to release this information does not imply endorsement of this study or its findings by either the revenue and fiscal affairs office or the data oversight council.
The views expressed are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Funding
This study was supported by the National Institute for Child Health and Human Development (grant nos. R01 HD08481901 and R01 HD099197). The funding sources had no role in the study design; collection, analysis, and interpretation of data; the writing of the report; and decision to submit the manuscript for publication. The authors have no financial relationships related to this article to disclose.
Author information
Authors and Affiliations
Contributions
Carolyn Smith Hughes contributed to data cleaning, performed the initial analyses, drafted the initial manuscript, and critically reviewed and revised the manuscript. Susan Schmitt provided support for data collection, extraction, cleaning, and analysis; and critically reviewed and revised the manuscript. Molly Passarella collected and extracted data, provided support for data cleaning and analysis, and critically reviewed and revised the manuscript. Scott Lorch obtained the funding; conceptualized and designed the study; coordinated and supervised data collection and interpretation; and critically reviewed and revised the manuscript. Ciaran Phibbs obtained the funding; conceptualized and designed the study; coordinated and supervised data collection, cleaning, analysis, and interpretation; and critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hughes, C.S., Schmitt, S., Passarella, M. et al. Who’s in the NICU? A population-level analysis. J Perinatol (2024). https://doi.org/10.1038/s41372-024-02039-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-024-02039-6
- Springer Nature America, Inc.