Abstract
Background and objective
Hospitalized preterm infants experience reduced meaningful auditory exposures during a critical period of brain development. Music-based interventions (MBI) may be beneficial, though it remains unclear which stimuli optimally enhance infant stabilization. We investigated the relationship between three conceptually-different MBIs and short-term responses in hospitalized preterm infants.
Study design
This is a case-crossover pilot study including 21 preterm infants between 30 and 35 weeks postmenstrual age. Participants listened to three MBIs and ‘no music’; each condition was provided three times in random order. We monitored physiologic and behavioral parameters around each exposure and analyzed results using linear mixed models.
Results
Respiratory rates decreased after each MBI compared with ‘no music’ (p = 0.02). The most notable decrease occurred following exposure to a low, repetitive musical pattern resembling a lullaby (p = 0.01). We noted no significant changes for the remaining parameters.
Conclusion
Specific MBI characteristics may preferentially enhance physiologic stabilization in hospitalized preterm infants.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
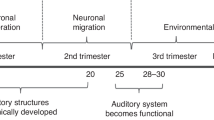
Infants born preterm undergo a critical period of brain development, including of the auditory cortex, while hospitalized in the Neonatal Intensive Care Unit (NICU) before term-equivalent age [1, 2]. During this period, preterm infants experience limited enriching auditory input, such as human voice, which increases risk for later adverse outcomes [3, 4]. Instead, the NICU auditory environment is often composed of loud equipment noises, excessive silence [4, 5]. In addition, preterm infants also experience significant medical morbidities, often requiring related cumulative atypical neurosensory experiences, all of which contribute to adverse neurological outcomes [6,7,8,9]. Emerging data suggest that optimizing the development of sensory functions in early infancy may enhance preterm brain maturation [10, 11] with resultant long-lasting benefits for cognitive and social-emotional processes [12].
Music-based interventions (MBIs) have been proposed as a strategy to reduce infant stress while enriching the auditory environment of hospitalized preterm infants [13]. The resultant stress reduction combined with auditory enrichment may have both an intendent and a multiplicative impact optimizing brain development in the NICU. Prior studies have assessed how music may help minimize infant stress in the NICU by examining the effects of MBIs on infants’ physiologic stability [14,15,16,17,18,19,20,21]. Small-size randomized trials in hospitalized preterm infants reported varying short-term benefits of music- and/or singing-based interventions on physiologic parameters, including increased oxygen saturation, reduced respiratory rate, and reduced heart rate [14,15,16,17,18]. MBIs using music and/or singing have also been shown to reduce observed symptoms of stress [19] and extremity activity levels [17] of preterm infants in the NICU. Moreover, data suggest that providing MBIs surrounding infant stressful procedures such as heel sticks, endotracheal suctioning, or routine oral cares may have a calming effect and facilitate return to baseline state [19, 22,23,24]. However, findings on the effects of MBIs on hospitalized preterm infants’ outcomes remain mixed [13], with some studies reporting lack of beneficial effects of music on infant physiologic parameters or behavioral state [20, 21]. In fact, a recent meta-analysis suggests that MBIs have a beneficial effect on reducing heart rate in preterm infants, but no further conclusions could be drawn regarding the effects on other physiologic parameters, overall efficacy, or the impact of different intervention types on infant and family outcomes [25]. One of the current limitations of the literature is that existing studies have employed a wide range of MBIs, especially in terms of the types of music stimuli used, limiting interpretation and applicability of findings. Specifically, it remains insufficiently understood which characteristics of MBIs might optimally modulate physiologic and neurologic stabilization after stressful experiences in preterm infants. In this study, we aimed to examine the relationship between exposure to three conceptually-different recorded MBIs provided after routine care times, and short-term physiologic and behavioral responses in hospitalized preterm infants.
Methods
Study design
This is a single center, case-crossover, controlled pilot study. We employed a within-subject, repeated measures approach to determine which musical characteristics of three conceptually-different MBIs was associated with optimal modulation of short-term physiologic and behavioral responses in hospitalized preterm infants. The study was approved by the Institutional Review Board at Mass General Brigham and families of all participants provided written informed consent.
Participants
A total of 21 preterm infants from the Brigham and Women’s Hospital NICU were enrolled, and 20 infants completed all study exposures. One patient had incomplete data (completed exposure to 7 out of 12 conditions) due to unanticipated transfer to another hospital. Infants were deemed eligible for the study if they were currently admitted in the level-III NICU where the study was conducted, had a postmenstrual age at enrollment between 30 weeks and 35 weeks 6 days, and were considered stable per their clinical care team. The exclusion criteria for the study included: major congenital anomaly, genetic or metabolic syndrome, high clinical suspicion of hearing impairment, and infants whose birth parent was less than 18 years old.
Study procedures
Conditions randomization and intervention timeline
Each participant was exposed to four audio conditions, consisting of three conceptually-different MBIs, and a “no music” condition. Each of the four conditions were provided to each patient three times, for a total of 12 exposures per participant, in a random order. To standardize administration of the audio conditions, 25 distinct playlists were created before enrollment began, each containing a predetermined, unique combination of the 12 conditions. Upon enrollment in the study, each patient was assigned an individual playlist which was uploaded on their designated speaker for the duration of their study participation. Research staff remained blinded to the order of conditions on each playlist until data collection was completed for all participants.
Interventions occurred on average three times per week until completion of the 12 exposures for each participant. The goal of the MBIs provided in this study was to assist with calming and soothing, hence study conditions were played immediately after a care or handling time (such as measurement of vital signs, physical examination, diaper/clothing changing, or drawing laboratory samples via heel stick or venipuncture) in coordination with the infant’s clinical care team. At each exposure time-point, infants listened to one of the four audio conditions from a BrightSign media player connected to a speaker (Bose SoundLink Revolve Bluetooth Speaker) at a preset volume.
Audio conditions
Three conceptually-different MBIs were created for the purpose of this study, each lasting approximately 15 min. A brief description of each MBI is as follows:
Condition 1 – ‘Glide Music’: This composition features a lead piano instrument, synthesized bass, drum pad, and string instruments providing harmonic accompaniment and a steady hand percussion providing rhythmic structure. The piece started at a moderate tempo, with several instruments playing, and no discernable pauses between the instruments. Over the course of the piece, the tempo noticeably slows down, the arrangement is reduced to 2–3 instruments, and pauses of silence are increasingly inserted between the motifs. We hypothesized this MBI will promote relaxation and sleep in infants by reducing the tempo and number of instruments playing in a piece of music over time.
Condition 2 – ‘Cloud Shapes’ Music: This composition features a lead piano and guitar instruments, synthesized pad, strings and guitar instruments providing harmonic accompaniment and a shaker or rattle percussion instrument. The piece embeds a simple and consistent rhythm that is played throughout the music segment, with piano alternating with guitar sounds. We hypothesized that this MBI will promote relaxation and sleep in infants by providing a slow, clear, repetitive and rhythmically consistent entrainment stimulus in the form of a melody within a conventional piece of music.
Condition 3 – ‘Womb Sounds’: This composition features synthesized rhythmic high frequency sound to simulate arterial blood flow, a steady background ambient low frequency sound and synthesized harmonic accompaniment. We hypothesized that this MBI will promote relaxation and sleep in infants by mimicking the acoustic environment of a womb within a conventional piece of music.
Condition 4 –‘No music’: This condition consisted of exposure to the NICU background auditory environment, with no additional audio element for the 15 min duration of the condition. We hypothesized that this condition would have no impact on infants’ physiologic or behavioral state.
Outcome measures and data collection
We measured outcome parameters around the time of each intervention, segmented into five time-intervals (Fig. 1). T0 designated a pre-intervention period of up to 15 min preceding the start of the intervention and served as the baseline interval, T1 occurred during the 15-min period of the intervention itself, while T2, T3, and T4 covered the 10, 30, and 60-min period respectively following the end of the intervention (i.e. a period of a total of 75 min following the start of the intervention was assessed). The measured physiologic parameters included the infant’s heart rate (HR), respiratory rate (RR), cerebral regional oxygen saturation (CrSO2), oxygen saturation (SpO2), and infant behavioral state scores. HR, RR, CrSO2, and SpO2 were captured from the infant’s bedside clinical care monitor using the CNS Envision device (Moberg Research, Inc.). CrSO2 was measured by near-infrared spectroscopy (NIRS, INVOSTM 5100 C Cerebral/Somatic Oximeter) via a small sensor positioned on the infant’s forehead and kept in place using either hydrogel and/or a standard infant hat.
The data collection for continuous measures was synchronized with the ‘time 0’ (i.e. start of exposure to a condition) noted in the study record. The data was then sectioned into five time-intervals, as [−15:0], [0:15], [15:25], [25:45], and [45:75] in minutes. Continuous outcome measures were averaged for each time-interval. To mitigate abrupt signal artifacts resulting from subject movements or clinical interventions, the time series data was downsampled to 1-min-rate signal medians. The physiological responses for each time interval were obtained by averaging using the median and then normalized against the [−15:0] pre-intervention time interval as the baseline for each exposure. For metrics without a specific clinical baseline and without an upper limit, such as RR, we considered their rate of change to be meaningful. For metrics with an expected clinical baseline and a clear upper bound, like SpO2, we considered their changes in the original units for clinical relevance. More specifically, we computed rMeasurement = Measurement/Measurement0, as HR and RR responses, and ΔMeasurement = Measurement-Measurement0 for SpO2 and CrSO2 responses, where Measurement was the signal median of [−15:0]. This yielded rHR, rRR, ΔSpO2, and ΔCrSO2 for each time interval of an exposure. The MATLAB program was used to process the time series data (ver. R2019b, Mathworks, Inc., Natick, MA).
Infant behavioral state was documented for each time-interval (T0 to T4) by a trained study staff member using the Anderson Behavioral State Scale (ABSS) [26, 27]. The scale evaluates an infant’s respirations, eye and body movements, and activity level to classify the sleep-wake state of preterm infants onto a 12-point scale, ranging from 1 (regular quiet sleep) to 12 (hard crying). The ABSS score was documented before the start of exposure, five minutes after the end of intervention (in order to maintain blinding of the examiner to the type of condition played at each timepoint), and again at the end of T2, T3 and T4 time periods.
We collected baseline characteristics of the study participants using medical record review, including demographic, clinical, and neuroimaging data where available. We also captured the background auditory environment of study participants around the time of exposures using the Language Environment Analysis (LENA) device [28], which was placed in the infant’s isolette or crib during the data collection period around each exposure. This allowed us to characterize the baseline auditory environment for each study patient, and categorize it in components including meaningful language, distant language, electronic noise, background noise, and silence.
Statistical analysis
We reported descriptive statistics of outcome measures collected as means (standard deviations [SD]), medians (ranges), and proportions. For each time interval, we utilized a mixed model to examine the effect of MBI on the pattern of infant physiology parameters (rHR, rRR, ΔSpO2, and ΔCrSO2) and behavioral state scores (ABSS) while accounting for repeated measures from three exposures of each of the audio conditions. These repeated measures were set as a ‘random’ effect and the different audio conditions were set as a ‘fixed’ effect in the model. When we found a significant fixed effect, we conducted Tukey post-hoc analysis to determine which music condition differed from others in terms of pattern of measured parameters, adjusting for multiple comparisons. We also tested for possible confounding factors and interactions related to sex and GA at birth. To ensure the normality of the variables, we employed Shapiro–Wilk tests and QQ-plots for each audio condition and further evaluated the normality of the model residual. We considered p < 0.05 as the threshold for statistical significance. All analyses were performed using JMP Pro v15 Software (SAS Institute Inc).
Results
We summarize the demographics and clinical characteristics for all study participants (n = 21) in Table 1. Among the 21 participants enrolled in the study, 10 (48%) were males and 4 (19%) were twins. The average GA at birth was 28 weeks, with a median birth weight (BW) of 1030 g and average BW z-score of 0.2. Intraventricular hemorrhage grade ≥3 was diagnosed in 4 (19%) participants, while any white matter injury was documented in 6 of the 17 (35%) participants who had a clinical or other research-related brain MRI. Eight participants required oxygen at 36 weeks postmenstrual age, and the median length of stay among the study population was 118 days (range 26–155).
With regards to the background auditory environment of study participants around the time of exposures, we note that this was primarily composed of silence (ranging between 35.0 and 59%). Baseline exposure to background noise (7.1–30.5%) and electronic noise (11.5–23.2%) was also high, while distant language (9.9–21.2%) and meaningful language (4.0–7.1%) accounted for the minority of auditory components, in keeping with prior research [4].
Physiological responses to MBI
Among the physiological responses examined during each time interval, we found a significant difference in rRR responses to MBIs specifically during the music period (T1 [0:15 min], p = 0.02, Table 2). Tukey post-hoc analysis revealed a significantly lower rRR during exposure to condition 2, as compared to the ‘no music’ condition 4 (p = 0.01, Fig. 2). This trend with respect to other audio conditions was consistent over time (Supplementary material). We found no evidence of confounding and interaction effects with sex or GA at birth. No concerns were documented or reported by clinical or research staff regarding adverse reactions experienced by any participants throughout the study.
aLeast squares means plot of RR responses during the exposure time interval (T1) over the baseline time-interval (T0). p values shown are after Tukey post-hoc analyses to adjust for multiple comparisons. The bars indicate 95% confidence interval of the mean after accounting for repeated measurements in each subject.
Infant behavioral states
The mixed model analysis showed a significant reduction in infant behavioral state scores after all conditions (End of T1, Fig. 3, also see Supplemental Fig. 1), meaning that infants reached a state of sleep after all exposures including condition 4–‘no music’. While not statistically significant, we observed the lowest infant states with condition 2 at end of T4 interval, with a p = 0.15 (p = 0.035 with condition 2 when compared to condition 4 ‘no music’ before adjusting for multiple comparisons, and p = 0.15 after Tukey post-hoc analysis accounting for multiple comparisons).
Discussion
While many studies have been conducted to measure the effects of music on a variety of infant outcomes, there are gaps in defining the specific MBI characteristics that may lead to optimal physiologic and behavioral responses in preterm infants. What this single center, case-crossover, controlled pilot study adds to existing literature is the description of the effects of three conceptually-different MBIs on short-term physiologic and behavioral patterns in hospitalized preterm infants. Our results indicate that there is a statistically significant effect (p = 0.02) on the respiratory rate in the desired (lower) direction following exposure to MBIs, with the strongest effect (p = 0.01) noted in post-hoc analysis during exposure to condition 2. Our finding that exposure to a recorded music intervention lowered hospitalized infants’ RR is consistent with several prior studies [15, 17, 18]. Specifically, when considering the three different MBI exposures, we found that the respiratory rate reduction was strongest during exposure to the MBI that consisted of a low, repetitive, and rhythmically consistent entrainment stimulus which most closely resembles a traditional lullaby. This finding is also consistent with limited other research available that has compared infant responses during exposure to lullaby-style music versus other types of recorded music [15, 29], and found that lullabies appear to have the most calming/desired effect on selected outcomes. In our study, this specific MBI (‘Cloud Shapes’) is an original piece of music written in a 4/4 meter with a central melody line with a consistent rhythm reproduced throughout the segment, played alternately by piano and guitar. Per our hypothesis, we speculate that the calm, simple, and repetitive pattern of this specific MBI are the key music stimulus characteristics that most likely mediated the desired effect observed on RR. Alternatively, the other two types of MBIs tested in this study may have been more activating (condition 1 with an initial moderate tempo with several instruments and no discernable pauses, condition 3 featuring a pulsing/ synthesized rhythmic high-frequency sound to simulate arterial blood flow on a background ambient low frequency sound), and were therefore associated with a less prominent effect on RR patterns. Our data appear to suggest that recorded MBIs with simple and repetitive elements are associated with a stabilizing effect on the RR pattern of hospitalized preterm infants, however we acknowledge that the small size and other limitations of this pilot study preclude us from drawing definitive conclusions.
Notably, the LENA data averages of the measures for all 12 interventions for each patient in this study suggested that nearly 60% of the auditory environment of the preterm infant is silence, and less than 10% is meaningful language. However, we also note that the LENA device was designed to quantify language exposures, and it is not known to differentiate recorded music from other types of electronic sound exposure. While these measurements were collected to simply characterize the environment surrounding hospitalized preterm infants, our results are in keeping with prior research [4] and support the need for further auditory enrichment for this population.
In our study, we did not observe a significant change from baseline in any of the other measured physiologic parameters (HR, SpO2, and. CrSO2). Behavioral state ratings were lower one hour after exposure to all conditions including condition 4 (no music), and remained most stable at the lowest rating after exposure to condition 2, however, this finding did not reach statistical significance. Importantly, no adverse effects were reported for any of the study patients enrolled.
When comparing our results with those of a recent meta-analysis [25], we note we did not find a significant change in HR pattern; instead, we found a significant change in the RR pattern, which was also observed in some but not all prior research included in this meta-analysis [15, 17, 18, 29, 30]. Overall, our findings are in keeping with recent literature that our understanding of effects of MBIs in this population is still emerging, and there may be a possible, albeit limited effect of music interventions on infant short-term outcomes. One possible reason for the lack of evidence of a more compelling calming effect of the MBIs may be that there are other competing interventions, therapies, and/or unpredictable events that often concurrently occur within a busy NICU environment that may interfere with preterm infants’ ability to ‘settle down’ and rest consistently after routine care times. In addition, preterm infants are known to often experience signs that are often attributed to gastrointestinal distress and gastroesophageal reflux (whether suspected or confirmed) during and after care and feeding times [31]. These signs often consist of changes in HR, RR, oxygen saturation, and behavioral changes similar to those assessed by the ABSS rating scale, all of which may have interfered with the post-intervention assessments collected in this study. Furthermore, we chose the physiologic and behavioral outcome measures for our study in keeping with prior research, however it is possible that the selected outcomes are in fact suboptimal indicators of infant stress. Future studies might consider more innovative and perhaps, more reliable methods of assessment of hospitalized infant stress, such as DNA methylation studies [32], assessment of infant hormonal status of cortisol and/or oxytocin [33], and/or brain white matter maturation of pathways involved in emotional processing as assessed by advanced neuroimaging techniques [34].
We would like to acknowledge several limitations of our study, including: (1) this was a pilot study with a small sample size which likely limited our power, as well as ability to explore other possible relationships for certain subpopulations at risk (i.e. responses in infants with advanced brain injury in subgroup analyses); (2) the change in RR we report on is statistically significant, however we recognize that the magnitude of the observed change might not be clinically significant; (3) our MBI lacked the inclusion of parent voice or another parent component due to feasibility (i.e. variability in family presence patterns, and to maintain blinding around exposures), (4) as discussed above, our study outcome measures are likely imperfect measures of infant stress, and (5) we only tested one aspect of the exposure (music type) in this study, and only had limited variations of the exposure. For all these reasons, our results remain preliminary and should be interpreted with caution. Further research should evaluate additional aspects of music exposures (‘dose’, duration, timing of exposure, with and without layered parental voice with careful consideration to avoid excessive stimulation particularly for infants with neurological injury [35]) to further define the optimal auditory experience for hospitalized preterm infants. Prospectively, large, well-powered studies employing MBIs and measuring clinically relevant outcomes remain needed to help establish whether and how MBIs may potentially make a statistically and clinically significant impact on hospitalized infants’ outcomes.
Data availability
The MATLAB program scripts as analyzed, along with deidentified data supporting our findings can be provided by the authors upon reasonable request.
References
Tierney AL, Nelson CA. Brain development and the role of experience in the early years. Zero Three. 2009;30:9–13.
Inder TE, Volpe JJ, Anderson PJ. Defining the neurologic consequences of preterm birth. N. Engl J Med. 2023;389:441–53.
Pineda RG, Neil J, Dierker D, Smyser CD, Wallendorf M, Kidokoro H, et al. Alterations in brain structure and neurodevelopmental outcome in preterm infants hospitalized in different neonatal intensive care unit environments. J Pediatr. 2014;164:52–60.e2.
Pineda R, Durant P, Mathur A, Inder T, Wallendorf M, Schlaggar BL. Auditory exposure in the neonatal intensive care unit: room type and other predictors. J Pediatr. 2017;183:56–66.e3.
Mayhew KJ, Lawrence SL, Squires JE, Harrison D. Elevated sound levels in the neonatal intensive care unit: what is causing the problem? Adv Neonatal Care. 2022;22:E207–16.
Smith GC, Gutovich J, Smyser C, Pineda R, Newnham C, Tjoeng TH, et al. Neonatal intensive care unit stress is associated with brain development in preterm infants. Ann Neurol. 2011;70:541–9.
Brummelte S, Grunau RE, Chau V, Poskitt KJ, Brant R, Vinall J, et al. Procedural pain and brain development in premature newborns. Ann Neurol. 2012;71:385–96.
Pineda RG, Tjoeng TH, Vavasseur C, Kidokoro H, Neil JJ, Inder T. Patterns of altered neurobehavior in preterm infants within the neonatal intensive care unit. J Pediatr. 2013;162:470–476.e1.
Kellner P, Kwon J, Smith J, Pineda R. Neurodevelopmental outcomes following preterm birth and the association with postmenstrual age at discharge. Am J Perinatol. 2022. https://doi.org/10.1055/a-1733-2690. Epub ahead of print.
Sa de Almeida J, Baud O, Fau S, Barcos-Munoz F, Courvoisier S, Lordier L, et al. Music impacts brain cortical microstructural maturation in very preterm infants: A longitudinal diffusion MR imaging study. Dev Cogn Neurosci. 2023;61:101254.
Lordier, Meskaldji DE L, Grouiller F, Pittet MP, Vollenweider A, Vasung L, et al. Music in premature infants enhances high-level cognitive brain networks. Proc Natl Acad Sci USA. 2019;116:12103–8.
Maitre NL, Key AP, Chorna OD, Slaughter JC, Matusz PJ, Wallace MT, et al. The dual nature of early-life experience on somatosensory processing in the human infant brain. Curr Biol CB. 2017;27:1048–54.
Mikulis N, Inder TE, Erdei C. Utilising recorded music to reduce stress and enhance infant neurodevelopment in neonatal intensive care units. Acta Paediatr Oslo Nor 1992. 2021;110:2921–36.
Jabraeili M, Sabet T, MustafaGharebaghi M, Asghari Jafarabadi M, Arshadi M. The effect of recorded mum’s lullaby and brahm’s lullaby on oxygen saturation in preterm infants: a randomized double-blind clinical trial. J Caring Sci. 2016;5:85–93.
Amini E, Rafiei P, Zarei K, Gohari M, Hamidi M. Effect of lullaby and classical music on physiologic stability of hospitalized preterm infants: a randomized trial. J Neonatal Perinat Med. 2013;6:295–301.
Taheri L, Jahromi MK, Abbasi M, Hojat M. Effect of recorded male lullaby on physiologic response of neonates in NICU. Appl Nurs Res ANR. 2017;33:127–30.
Wirth L, Dorn F, Wege M, Zemlin M, Lemmer B, Gorbey S, et al. Effects of standardized acoustic stimulation in premature infants: a randomized controlled trial. J Perinatol. 2016;36:486–92.
Caparros-Gonzalez RA, de la Torre-Luque A, Diaz-Piedra C, Vico FJ, Buela-Casal G. Listening to relaxing music improves physiological responses in premature infants: a randomized controlled trial. Adv Neonatal Care. 2018;18:58–69.
Aydin D, Yıldız S. Effect of classical music on stress among preterm infants in a neonatal intensive care unit. HealthMED. 2012;6:3162–8.
Blumenfeld H, Eisenfeld L. Does a mother singing to her premature baby affect feeding in the neonatal intensive care unit? Clin Pediatr. 2006;45:65–70.
Alipour Z, Eskandari N, Ahmari Tehran H, Eshagh Hossaini SK, Sangi S. Effects of music on physiological and behavioral responses of premature infants: a randomized controlled trial. Complement Ther Clin Pr. 2013;19:128–32.
Butt ML, Kisilevsky BS. Music modulates behaviour of premature infants following heel lance. Can J Nurs Res. 2000;31:17–39.
Chou LL, Wang RH, Chen SJ, Pai L. Effects of music therapy on oxygen saturation in premature infants receiving endotracheal suctioning. J Nurs Res JNR. 2003;11:209–16.
Anbalagan S, Velasquez JH, Staufert Gutierrez D, Devagiri S, Nieto D, Ankola P. Music for pain relief of minor procedures in term neonates. Pediatr Res. 2023;1–5. https://doi.org/10.1038/s41390-023-02746-4. Epub ahead of print. Erratum in: Pediatr Res 2023 Sep 29.
Haslbeck FB, Mueller K, Karen T, Loewy J, Meerpohl JJ, Bassler D. Musical and vocal interventions to improve neurodevelopmental outcomes for preterm infants. Cochrane Database Syst Rev. 2023;9:CD013472.
Gill NE, Behnke M, Conlon M, McNeely JB, Anderson GC. Effect of nonnutritive sucking on behavioral state in preterm infants before feeding. Nurs Res. 1988;37:347–50.
Gill NE, Behnke M, Conlon M, Anderson GC. Nonnutritive sucking modulates behavioral state for preterm infants before feeding. Scand J Caring Sci. 1992;6:3–7.
Caskey M, Vohr B. Assessing language and language environment of high-risk infants and children: a new approach. Acta Paediatr Oslo Nor 1992. 2013;102:451–61.
Loewy J, Stewart K, Dassler AM, Telsey A, Homel P. The effects of music therapy on vital signs, feeding, and sleep in premature infants. Pediatrics. 2013;131:902–18.
Tandoi F, Francescato G, Pagani A, Buzzetti G, Negri E, Agosti M. The Original Sound”: a new non-pharmacological approach to the postnatal stress management of preterm infants. J Matern Fetal Neonatal Med. 2015;28:1934–8.
Eichenwald EC, COMMITTEE ON FETUS AND NEWBORN. Diagnosis and management of gastroesophageal reflux in preterm infants. Pediatrics. 2018;142:e20181061.
Malin KJ, Gondwe KW, Fial AV, Moore R, Conley Y, White-Traut R, et al. Scoping review of early toxic stress and epigenetic alterations in the neonatal intensive care unit. Nurs Res. 2023;72:218–28.
Pavlyshyn H, Sarapuk I, Horishna I, Slyva V, Skubenko N. Skin-to-skin contact to support preterm infants and reduce NICU-related stress. Int J Dev Neurosci. 2022;82:639–45.
Sa de Almeida J, Lordier L, Zollinger B, Kunz N, Bastiani M, Gui L, et al. Music enhances structural maturation of emotional processing neural pathways in very preterm infants. NeuroImage. 2020;207:116391.
Epstein S, Bauer S, Levkovitz Stern O, Litmanovitz I, Elefant C, Yakobson D, et al. Preterm infants with severe brain injury demonstrate unstable physiological responses during maternal singing with music therapy: a randomized controlled study. Eur J Pediatr. 2021;180:1403–12.
Acknowledgements
We thank first and foremost our patients and their families, along with the Brigham Infant Brain Studies (BIBS) research laboratory colleagues for making this work possible.
Author information
Authors and Affiliations
Contributions
Authors’ contributions: CE and TI conceptualized the study design, intervention, and outcomes. CE contributed to leading and overseeing data collection, analyses, drafted the initial manuscript, and reviewed and revised the manuscript. JS performed data analyses, and contributed to writing and reviewing the manuscript. GCC contributed to data analyses, writing of the initial draft, and reviewing the manuscript. MF facilitated data collection, and contributed to drafting the manuscript. MED and TEI critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Mass General Brigham Institutional Review Board and all families of enrolled infants signed informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Erdei, C., Sunwoo, J., Corriveau, G.C. et al. Effect of music-based interventions on physiologic stability of hospitalized preterm infants. A pilot study. J Perinatol 44, 665–670 (2024). https://doi.org/10.1038/s41372-024-01907-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-024-01907-5
- Springer Nature America, Inc.