Abstract
Objective
Determine effect of at least 60 s delayed cord clamping (DCC) on postpartum hemorrhage and maternal estimated blood loss (EBL) in very low birth weight (VLBW) cesarean deliveries when compared to early cord clamping (ECC).
Study design
Retrospective study of VLBW infants at birth. Maternal pre- and post-operative hemoglobin, EBL, and neonatal outcomes were collected.
Results
In total, 620 VLBW infants (DCC = 166, ECC = 454) born to 545 mothers (DCC = 155, ECC = 390) were included. Maternal PPH between DCC was 8% versus ECC was 10% p = 0.52. There were no differences in estimated blood loss or rate of maternal blood transfusion between groups. The post-operative hemoglobin was lower in infants receiving ECC compared to DCC (10.4 [9.4–11.5] versus 10.8 [10.1–11.9] g/dl, p = 0.01). In comparing pre-operative to post-operative hemoglobin there was no difference between DCC and ECC (−1.2 [−2.0 to −0.3] versus −1.2 [−2.1 to −0.6] g/dl, p = 0.46).
Conclusion
DCC of at least 60 s did not increase maternal bleeding complications during VLBW cesarean delivery. To our knowledge, this retrospective study is the largest sample size to date of preterm cesarean deliveries to support maternal safety regarding bleeding complications after delayed cord clamping.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
American College of Obstetricians and Gynecologists (ACOG) recommends delaying umbilical cord clamping by at least 30–60 s regardless of delivery mode for preterm and term births rather than clamping the umbilical cord right away [1]. The benefits of delayed cord clamping in preterm and term neonates are well supported and include better transitional circulation and establishment of red blood cell volume, decreased need for blood transfusion, and lower incidence of necrotizing enterocolitis and intraventricular hemorrhage (IVH) [1]. The World Health Organization (WHO) defines delayed cord clamping (DCC) as occurring 60 s or more after birth and early or immediate cord clamping (ECC) as less than 60 s [2]. Despite the neonatal benefits of delayed umbilical cord clamping, research on maternal safety associated with umbilical cord treatments at delivery is lacking. For women delivering by cesarean section where blood loss is expected to be greater than a vaginal delivery, evidence is limited for both term and preterm babies born via unscheduled and urgent cesarean sections. Postpartum hemorrhage (PPH) is the leading cause of maternal mortality globally [3] and is defined as blood loss ≥1000 ml or any blood loss with signs or symptoms of hypovolemia within 24 h of birth [4].
In an ACOG cited review of five trials of term vaginal births, delayed cord clamping was not associated with a higher risk of postpartum hemorrhage, need for blood transfusion, or lower post-operative hemoglobin [5]. In a randomized controlled trial of 113 term infants born by cesarean section comparing maternal blood loss in immediate cord clamping with delayed cord clamping of 60 s, there was no significant difference in maternal hemoglobin levels from pre-operative to post-operative day 1 [6].
Data on maternal safety of delayed cord clamping in preterm deliveries is limited. A meta-analysis of preterm umbilical cord interventions cited insufficient data on maternal blood loss greater than 500 ml when comparing delayed cord clamping to early/immediate cord clamping or umbilical cord milking [7]. Since the majority of preterm births occur via cesarean section, an evaluation of maternal outcomes is critical.
We sought to determine whether delayed cord clamping of at least 60 s compared to early cord clamping (0–59 s) increased maternal blood loss in cesarean deliveries in very low birthweight infants (under 1500 grams). The primary objective of this study was to identify whether delayed cord clamping increases the risk of maternal blood loss evidenced by increased postpartum hemorrhage or a decrease in post-operative maternal hemoglobin compared to early cord clamping, in very low birthweight (VLBW) cesarean section deliveries. The secondary objectives were to determine whether there are differences in maternal blood transfusions and neonatal outcomes with DCC versus ECC.
Methods
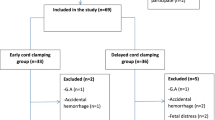
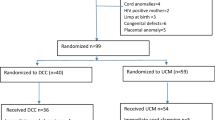
A retrospective study was conducted for deliveries that occurred from January 2018 to October 2021 at three Sharp Hospitals in San Diego, CA (Sharp Mary Birch Hospital for Women & Newborns, Sharp Chula Vista Medical Center, and Sharp Grossmont Hospital). The data was obtained from an institutional repository of delivery room data and approved by the local ethics board (Sharp HealthCare IRB).
Regardless of delivery route, delaying the clamping of the umbilical cord for at least 60 s has been standard practice at Sharp Hospitals since 2013 for stable infants born at 23 weeks gestation or greater. Any decision to clamp early was made by obstetrical discretion. The cutoff between DCC and ECC in timing of cord clamping was stratified from obstetric report in the medical record. Options for cord management reporting were (not done), (0–59 s), and (60 s or greater). Eligible infants were born with a birthweight under 1500 grams. Singleton and multiple gestation pregnancies were included. Exclusion criteria included infants born vaginally and infants with unknown cord management. Data collected included all indications of delivery regardless of maternal comorbidities and/or fetal indication for cesarean section. Rate of DCC in the extreme preterm gestational age group was anticipated to be less based on stability at delivery, reason for delivery, and obstetric judgment. Postpartum hemorrhage was defined as a cumulative blood loss of 1000 ml or more within 24 h of delivery. Estimated blood loss was recorded by obstetricians in the medical record. Delayed cord clamping was defined as a cord clamp time of 60 s or greater. Early cord clamping was defined as occurring any time between 0 to 59 s. Since cord milking (squeezing the intact umbilical cord several times before clamping and cutting the cord) would not have an impact on maternal outcomes, infants receiving this treatment before 60 s were analyzed as early cord clamping.
Statistical analysis
Maternal and neonatal outcomes were summarized using descriptive characteristics (means were calculated for normally distributed outcomes; counts and percentages were calculated for categorical outcomes). Categorical outcomes with rare events were calculated using Fishers exact tests. Logistic regression was used to determine if there was an association between delayed versus early cord clamping and dichotomous outcomes such as neonatal mortality, intraventricular hemorrhage (IVH), bronchopulmonary dysplasia, retinopathy of prematurity (ROP), and necrotizing enterocolitis. All statistical analyses were conducted at an α-level of 0.05 and 95% confidence intervals provided. All calculations and analyses were performed using SPSS. (IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp.)
Results
Of the 620 VLBW infants that met inclusion criteria, 166 infants received DCC and 454 infants received ECC and were born to 545 mothers (DCC = 155, ECC = 390). There was no difference in the incidence of multiples between groups (Table 1). There were no differences in postpartum hemorrhage or estimated blood loss (EBL) during DCC compared to ECC (Table 2). The incidence of maternal postpartum hemorrhage between DCC versus ECC was 8% versus 10%, p = 0.52. The post-operative hemoglobin was lower for ECC than DCC (10.4 [9.4–11.5] versus 10.8 [10.1–11.9] g/dl, p = 0.01). There was no difference in pre-operative to post-operative hemoglobin (ECC −1.2 [−2.0 to −0.3] versus DCC −1.2 [−2.1 to −0.6] g/dl, p = 0.46) or the rate of maternal blood transfusion between the groups (DCC 5% versus ECC 7%, p = 0.58). There was only one maternal death in the ECC group.
Maternal demographics including age, ethnicity, gravida, and para were similar between groups (Table 1). There was increased placental abruption (DCC 11% versus ECC 20%, p = 0.01) in the ECC group compared to mothers receiving DCC at delivery. There were no differences in maternal medications such as magnesium sulfate, uterotonics, or general anesthesia (Table 2). There were no differences in maternal morbidities including diabetes, chorioamnionitis, pregnancy induced hypertension (PIH) or pre-eclampsia. The reason for delivery, uterine atony, type of cesarean incision, and length membrane rupture prior to delivery were not different between groups (Tables 1 and 2).
Infants receiving early cord clamping had a lower gestational age and birthweight, a greater cord blood base deficit, lower 1- and 5-min Apgar scores, required more resuscitation (supplemental oxygen, positive pressure ventilation, and intubation) and had a higher mortality rate (Tables 3 and 4, not adjusted for gestational age). There was no difference in necrotizing enterocolitis, any grade IVH, oxygen requirement at 36 weeks corrected age, or need for red blood cell transfusion in neonates between the two groups (Table 4). After adjusting for gestational age using logistic regression modeling, death prior to discharge (p = 0.18) and ROP requiring treatment (p = 0.08) were no longer significant. Delivery room support values for CPAP (p = 0.004), PPV (p = 0.001), and intubation (p = 0.002) remained significant after adjusting for gestational age, however supplemental oxygen was no longer significant (p = 0.13). Cord gases remained statistically significant, adjusted values arterial cord pH (p = 0.017), arterial cord BE (p = 0.002), venous cord pH (p = 0.016), and venous cord BE (p = 0.001). After adjusting for gestational age using logistic regression modeling, 1- and 5-min Apgar scores (p = 0.001 and p = 0.05), cry prior to cord clamp (p < 0.001), and temperature at 5 min (p = 0.01) also remained significant.
Discussion
Given the beneficial properties of placental transfusion in newborns, delayed cord clamping is recommended and used globally for term and preterm births. Multiple randomized controlled trials and institutions including WHO, ACOG, and the American Academy of Pediatrics support the use of DCC [5, 7, 8]. However, most recommendations do not consider the implications on maternal safety during delayed cord clamping particularly during cesarean section. There are even fewer randomized controlled trials that investigate risk of postpartum hemorrhage or other maternal outcomes associated with DCC. Given the degree of blood loss during a cesarean section surgery, any intervention that increases surgical time even for the benefit of the newborn, should consider the maternal aspects at delivery. Preterm infants are also more likely to be delivered by a classical (vertical) incision in cesarean section due to the urgent nature of their deliveries and fetal position. A retrospective study found a greater risk for need of maternal blood transfusions with classical vertical incision when compared to transverse incision for deliveries of 23–34 week gestation infants [9]. Additional risk factors for hemorrhage at the time of delivery include pre-eclampsia, prolonged labor, and intraamniotic infection and are often common indications for a preterm cesarean section [10].
Early cord clamping has been practiced as standard of care for management of postpartum hemorrhage [11]. Causes of PPH include uterine atony, retained or invasive placenta, trauma from delivery, and coagulopathy [12]. In the past decade a number of treatments including the use of uterotonics, such as oxytocin (Pitocin), has reduced the risk of hemorrhage during the third stage of labor [13]. Pre-operative lab results and maternal history is also used in assessing risk for blood loss and indicators of PPH [8]. Our cohort of women with very low birth weight infants does not appear to have an increased risk of bleeding complications during cesarean section.
Other groups have also failed to demonstrate an association of increased maternal blood loss during cesarean sections. In a randomized controlled trial of delayed versus immediate cord clamping in full-term cesarean sections, there was no difference found in hemoglobin levels after 60 s compared to immediate cord clamping [6]. Data on preterm cesarean sections is limited. In a retrospective study comparing ECC to DCC in multiple gestation pregnancies, there were no differences in PPH, EBL, or total operative time when delivered by cesarean section [14]. Recently, a small single-center retrospective study demonstrated no difference in the hematocrit change pre- and post-delivery between DCC (N = 16) and ECC (N = 11) in preterm deliveries. Although the preterm data combined both modes of delivery, ~65% of the deliveries were cesarean section [15]. A pilot study compared mother term-infant dyads receiving an extended (90–120 s) delay in cesarean deliveries to historical controls of immediate cord clamping showed a decrease in maternal blood loss and the need for maternal blood transfusions [16]. The authors suggested that with a longer delay, the placenta may empty more efficiently and alter its response in the uterus. It remains to be seen whether a longer delay up to 120 s at preterm birth would result in a similar benefit with the extended delay.
While our study was not intended to demonstrate the differences in neonatal outcomes with delayed cord clamping or immediate cord clamping, we reported significant differences in Apgar scores, oxygen support, and cord gases, even after adjusting for gestational age. However, the study is limited by its retrospective nature with the potential for bias since the obstetrician may have had maternal and neonatal concerns at deliveries where early cord clamping was performed. Data regarding estimated blood loss was subjective as reported by the obstetrician and neonatal outcomes may have been similarly biased by those maternal infant dyads that may have been more ill. Additional maternal information on predisposition for bleeding risks and further complications secondary to hemorrhage were not available in the data set.
This retrospective study provides the largest sample size, to our knowledge, of VLBW cesarean deliveries supporting the safety of DCC during cesarean section. These data support the safety of delayed cord clamping by objective maternal measures such as pre- and post-operative hemoglobin, the absence of differences in postpartum hemorrhage, or the need for blood transfusions. As neonatal and obstetrical groups continue to promote longer delayed cord clamping in preterm deliveries, the need for ongoing assessment of maternal safety is critical [17].
Data availability
A deidentified dataset is available by written request to the corresponding author.
References
Delayed Umbilical Cord Clamping After Birth. ACOG Committee Opinion, Number 814. Obstet Gynecol. 2020;136:e100–6.
WHO Guidelines Approved by the Guidelines Review Committee. Guideline: delayed umbilical cord clamping for improved maternal and infant health and nutrition outcomes. Geneva: World Health Organization Copyright (© World Health Organization 2014); 2014.
Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2:e323–33.
Practice Bulletin No. 183. Postpartum hemorrhage. Obstet Gynecol. 2017;130:e168–86.
McDonald SJ, Middleton P, Dowswell T, Morris PS. Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes. Cochrane Database Syst Rev. 2013;2013:Cd004074.
Purisch SE, Ananth CV, Arditi B, Mauney L, Ajemian B, Heiderich A, et al. Effect of delayed vs immediate umbilical cord clamping on maternal blood loss in term cesarean delivery: a randomized clinical trial. JAMA. 2019;322:1869–76.
Rabe H, Gyte GM, Díaz-Rossello JL, Duley L. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev. 2019;9:Cd003248.
Fogarty M, Osborn DA, Askie L, Seidler AL, Hunter K, Lui K, et al. Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis. Am J Obstet Gynecol. 2018;218:1–18.
Luthra G, Gawade P, Starikov R, Markenson G. Uterine incision-to-delivery interval and perinatal outcomes in transverse versus vertical incisions in preterm cesarean deliveries. J Matern-Fetal Neonatal Med. 2013;26:1788–91.
Morey SS. ACOG releases report on risk factors, causes and management of postpartum hemorrhage. Am Fam Physician. 1998;58:1002.
Prendiville WJ, Harding JE, Elbourne DR, Stirrat GM. The Bristol third stage trial: active versus physiological management of third stage of labour. BMJ. 1988;297:1295–300.
Callaghan WM, Kuklina EV, Berg CJ. Trends in postpartum hemorrhage: United States, 1994-2006. Am J Obstet Gynecol. 2010;202:353.e1–6.
Begley CM, Gyte GM, Devane D, McGuire W, Weeks A. Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev. 2011:Cd007412. https://doi.org/10.1002/14651858.CD007412.pub3.
Ruangkit C, Leon M, Hassen K, Baker K, Poeltler D, Katheria A. Maternal bleeding complications following early versus delayed umbilical cord clamping in multiple pregnancies. BMC Pregnancy Childbirth. 2018;18:131.
Chiruvolu A, Estes E, Stanzo KC, Desai S, Cornelius BC. The effects of placental transfusion on mothers. J Matern-Fetal Neonatal Med. 2022:1–6. https://doi.org/10.1080/14767058.2022.2032636. Online ahead of print.
Chantry CJ, Blanton A, Taché V, Finta L, Tancredi D. Delayed cord clamping during elective cesarean deliveries: results of a pilot safety trial. Matern Health Neonatol Perinatol. 2018;4:16.
Knol R, Brouwer E, van den Akker T, DeKoninck P, van Geloven N, Polglase GR, et al. Physiological-based cord clamping in very preterm infants—randomised controlled trial on effectiveness of stabilisation. Resuscitation. 2020;147:26–33.
Acknowledgements
ACK was supported by the Cushman Foundation, the Chuck and Ernestina Kreutzkamp Foundation and the Stephen and Lynne Doyle Foundation. We thank the following individuals for their expertise and assistance throughout all aspects of our study: Alexis Rosete, Kaitlyn Fitzgerald, Ana Morales, Elise Mischke, Lukas Linares, Marcie Portillo, and Kathy Arnell.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conceptualization, design, and review of the work. CS substantially contributed to data curation, drafting, and writing manuscript. SAS contributed to data curation and initial manuscript. DMP contributed to data analysis and manuscript revision. ACK co-wrote manuscript and gave final approval of this version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Salcido, C., Shahidi, S.A., Poeltler, D.M. et al. Maternal bleeding complications and neonatal outcomes following early versus delayed umbilical cord clamping in cesarean deliveries for very low birthweight infants. J Perinatol 43, 39–43 (2023). https://doi.org/10.1038/s41372-022-01558-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01558-4
- Springer Nature America, Inc.