Abstract
Objective
The goal of this study was to assess the impact of infant-driven feeding (IDF) compared to traditional feeding protocols in promoting earlier successful feeding outcomes.
Study design
We performed a cross-sectional analysis of infants admitted to a level three neonatal intensive care unit (NICU) over a 2-year period. We compared infants fed with the traditional protocol to those under the IDF protocol.
Results
Infants in the IDF group were younger at first feed (p < 0.001). There was no difference in age at nasogastric (NG) tube removal or at discharge, length of stay, or percentage breastfeeding at discharge. There were no differences in outcomes within two subgroups born at <35 and <32 weeks gestation, respectively.
Conclusion
The IDF program led to earlier initiation of oral feeding. However, this did not lead to earlier NG tube removal or discharge, a shorter length of stay, or increase in the rates of breastfeeding.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
The World Health Organization has reported that between 5 and 18% of infants are delivered prematurely every year [1]. These infants are at great risk for oral feeding problems [1,2,3]. The successful initiation of oral feeding in preterm infants is a complex activity that requires an infant to obtain appropriate developmental maturity. Emerging research suggests that the initiation of oral feedings in preterm infants is best done in response to the infant’s developmental cues [4]. Poor oral feeding initiation is associated with increased long-term feeding problems in early childhood, increased need for enteral tube feedings, and increased length of stay (LOS) in the NICU setting [5].
Preterm infants have multiple feeding challenges that term infants do not encounter as frequently. Preterm infants also have increased caloric needs and decreased tolerance of large volumes compared to their term counterparts [6]. The development of neurological pathways is required for the coordination of suck-swallow-breath (SSB), and this begins occurring from 32 to 36 weeks post-menstrual age (PMA) along with increasing alertness [7, 8]. Feeding drives significant changes in the SSB pattern in the first 6 months of life, accompanied by advancement in alert motor activities and greater visual exploration [9]. Preterm infants fed before the adequate development of SSB are at an increased risk for aspiration [10, 11]. There is now considerable evidence that maturation of sucking may be accelerated by the early cue-based, or infant-driven, introduction of suckling feeding where the infant controls the timing and amount [12,13,14,15]. The unique feeding challenges of preterm infants necessitate a nuanced approach to initiating oral feedings.
Historically, infants admitted in a neonatal intensive care unit (NICU) setting were fed according to provider orders that were primarily based on the infant’s weight and gestational age. These feedings were volume-driven and scheduled on a time-based interval [16]. Continuing to feed an infant once they have shown satiety cues creates a stressful feeding experience [16]. Volume-driven feeding is associated with increased stress during feedings, as well an increase in infants’ oral aversion to breast and bottle feedings [4]. Alternatively, infant and cue-based feeding techniques have also been shown to lead to higher rates of breastfeeding at discharge and longer breastfeeding duration [17, 18]. Considering that bottle feeding has been shown to increase infants’ risk for overfeeding, impaired satiety responsiveness, and rapid weight gain, the greater breastfeeding rates achieved by this method may contribute to improved long-term feeding outcomes [19].
Infant-driven feeding (IDF) is a protocol developed to initiate oral feedings based on the infant’s developmental cues and readiness to fed. This model involves the nursing staff using scales to determine infant readiness to feed, as well as quality measures describing the feeding, and caregiver feeding skills. Previous research examining the use of the IDF protocol in NICU settings were quality improvement projects that showed IDF lead to infants achieving earlier full oral ad libitum feedings [20,21,22,23,24,25]. Other studies also observed decreased LOS in the comparison group of infants [5, 26]. However, these studies utilized small sample sizes over a short time period. Additionally, one study found that infants at 32 weeks who had low scores on the IDF Readiness protocol were more likely to have feeding difficulties, supporting that the IDF protocol could also be used to identify infants at risk for this [27].
Identifying the most effective feeding protocol for infants in the NICU will allow for the selection of a protocol that reduces the likelihood of long-term feeding issues and increases the likelihood of achieving successful oral feeding in the NICU that persists after discharge. The aim of this study was to assess the outcomes of the IDF protocol compared to a traditional feeding protocol at a large midwestern Level III NICU.
Methods
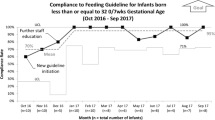
We performed a retrospective chart review of infants (n = 777) admitted to the Level III NICU from May 2015 to July 2017 at a regional center with an embedded children’s hospital in Fargo, ND. This included infants born at the hospital and infants born at surrounding hospitals but admitted to our NICU on the day of birth. We compared the outcomes of infants (n = 280) cared for using traditional scheduled feeds prior to the initiation of the IDF protocol (May 2015 to May 2016) to infants (n = 209) who were fed according to the IDF model (May 2016 to July 2017) (Fig. 1).
Prior to the introduction of IDF, infants admitted to the NICU were fed according to a time-based schedule. Infants were considered eligible for oral feeding initiation after they were older than 34 weeks PMA and did not require respiratory intervention greater than 2 liters of flow via nasal canula. If mother desired to breastfeed, infants were offered non-nutritive breastfeeding, and then nutritive breastfeeding feeding first before bottle feeding was introduced. Infants whose mothers did not desire to breastfeed were offered bottle feeding. All infants who were eligible for oral feedings were offered a bottle on a time schedule (most often every 3 h). Infants were fed using a standard bottle using one of two disposable nipples. The infant was not fed using the parent’s choice of bottle until after discharge. If an infant was sleeping at its scheduled feeding time and was not woken during the process of obtaining vitals, the prescribed volume was given by NG tube. If the infant alerted at all during vitals, a bottle feeding was attempted. All infants that were awake were given an attempt at oral feeding, without any assessment of feeding readiness cues. Breastfeeding was offered if mother was at bedside and interested in breastfeeding. Infants were offered breastfeeding no more than two times per day while admitted.
A multidisciplinary feeding team was formed at the hospital in 2015 to look at strategies for improving feeding in the NICU setting. This team included nurses (representatives from each shift), occupational therapists, speech therapists, lactation consultants, discharge coordinators, neonatal nurse practitioners, a pediatric behavioral psychologist, and neonatologists. The team reviewed current available evidence and selected the IDF program. In May 2016, the hospital implemented the IDF program and trained all staff in the NICU with a 4-h formalized module. To date, this training module continues to be utilized in the onboarding of all new hires into the NICU. All infants born prior to 33 weeks received nutrition through either an orogastric or nasogastric (NG) tube. Infants were assessed beginning at 33 weeks using the standardized IDF Readiness Scale, and when they met the outlined criteria, they initiated the IDF protocol.
The IDF protocol adopted by our institution in May of 2016 has been previously described in Ludwig et al. [28]. It consists of three scales. The “Readiness” scale assigns a numerical score based on feeding cues beginning at 32 weeks PMA. An infant that is older than 33 weeks and consistently scores a 1 or 2 begins oral feeds. The “Quality” scale is an objective way to document the quality of the feed that is independent of volume. Finally, the “Caregiver Technique” form allows for documentation of caregiver interventions designed to support the infants feeding. This aims to facilitate greater consistency in feeds between caregivers [28].
This study excluded infants admitted for a brief surgical procedure, infants with a LOS <4 days, infants who were discharged from the normal nursery, or who died before discharge. We also excluded infants with chromosomal abnormalities, cardiac abnormalities requiring intervention, serious gastrointestinal abnormalities (omphalocele, gastroschisis), or neurologic abnormalities such as intraventricular hemorrhage grade 4 (Fig. 1). Data were collected on PMA at first full oral feedings, G-tube placement at discharge, G-tube placement before 1 year of life, readmission for failure to thrive (FTT) in the first year of life, PMA at NG tube removal (during or after NICU stay), home NG at discharge, PMA at discharge, breastfeeding at the time of discharge, and LOS in days.
We also studied two subsets of the larger group. The first contained infants born earlier than 35 weeks who were fed according to the traditional scheduled feeding (n = 147) and infants who were fed using the IDF protocol (n = 145) (Fig. 1). We further analyzed the data limited to infants born prior to 32 weeks who were fed according to the traditional scheduled feeding (n = 57) and infants who were fed using the IDF protocol (n = 60) (Fig. 1).
SPSS 25.0 for Windows was used to analyze demographic and clinical characteristics of the patients. Frequencies and relative percentages were computed for each categorical variable. Fisher’s exact tests were performed to determine differences in rates of categorical variables and Student’s t test were used to determine differences in continuous variables. Fisher’s exact test was used for the breastfeeding analysis. All p values were two-sided and p value <0.05 was considered significant. The study was approved by the Institutional Review Boards of the University of North Dakota and the hospital.
Results
In total 489 infants were analyzed, with 280 being in the IDF group and 209 in the traditional feeding group. Infants fed according to the traditional protocol were significantly older at admission than infants fed according to the IDF protocol, 34.8 ± 4.4 weeks vs 33.7 ± 3.8 weeks (p value = 0.004, Table 1). Infants in the IDF protocol demonstrated a significantly earlier PMA at first feeding when compared with those in the traditional protocol, 35.5 ± 3.4 vs 36.5 ± 2.5 (p value ≤ 0.001, Table 1). However, among a sub-group of infants born at <35 weeks of GA, there was no significant difference in PMA at first feed in the IDF group compared to the traditional group, 34.2 ± 3.0 vs 34.6 ± 1.0 (p value = 0.112, Table 2). Among all infants and the <35 week cohort there were no differences between traditional and IDF feeding groups with regard to PMA at NG removal, PMA at discharge, the LOS in days, and rate of breastfeeding at discharge (Tables 1 and 2). Infants <32 weeks fed according to the IDF protocol were significantly older at admission than infants fed according to the traditional protocol, 29.1 ± 2.1 vs 27.9 ± 2.5 (p value = 0.005, Table 3). Infants <32 weeks in either the traditional or IDF protocol showed no difference in PMA at first feeding (p value = 0.120, Table 3). Infants within this group in the IDF protocol did demonstrate a significantly shorter LOS in days compared to the traditional protocol, 56.5 ± 26.2 vs 68.6 ± 29.7 (p value = 0.021, Table 3). There were no differences in the other outcomes analyzed, including PMA at NG removal, PMA at discharge, and the rate of breastfeeding at discharge (Table 3).
The outcomes of G-tube placement at discharge, G-tube placement before 1 year of life, readmission for FTT in the first year of life, and home NG at discharge had too small a number of infants in either protocol to be compared and thus were not included in the analysis.
Discussion
Our study showed that infants fed using the IDF protocol achieved their first oral feeding at an earlier PMA compared to infants using the traditional feeding protocol. This finding is congruent with those observed by other studies [5, 20,21,22,23,24,25, 29, 30]. However, we did not find a difference in the PMA at first feeding among the <32 weeks or the <35 weeks cohorts. This may indicate that infants older than 35 weeks are the ones that are deriving the benefit of the IDF protocol. We observed that infants <32 weeks experienced a shorter LOS in days despite not achieving earlier full feeding, which could suggest that IDF has a unique impact on or be related with factors that determine LOS in this group of premature infants. For all cohorts, we did not find a difference between the IDF and traditional protocols in terms of PMA at NG tube removal, PMA at discharge, presence of breastfeeding at discharge, or LOS in days with only the 32 week cohort in exception as noted. Age at first feed for infants fed using a traditional approach has differed between studies. Some reported an age at first feed comparable to ours and other studies reported an earlier age at first feed [29, 31].
While our findings for the <35 week cohort differ from prior studies, they are supported by a systematic review and meta-analysis that evaluated nine randomized control trials (RCTs) or quasi-RCTs published through 2016 which compared responsive vs scheduled feeding for preterm infants [23]. This review noted a number of methodological weaknesses in the included studies and concluded that overall, there was modest, low-quality evidence suggesting an earlier achievement of full oral feeding and PMA at discharge. While this review was conducted before the Settle [5] and Fry [29] reviews, those reviews only examined quality improvement initiatives and thus the failure to demonstrate the other positive findings in the more rigorous RCTs concurs with the lack of association found in our study. The conclusion of the Cochrane review is that currently available evidence does not provide strong or consistent evidence that responsive/cue-based feeding influences important outcomes for preterm infants or their families [23]. This conclusion calls into question most of the prevailing findings from previous IDF studies and could explain why our study only achieved one of these outcomes.
The impact of significant age differences between the two protocols for all infants and the <32 week cohort on our outcomes is unclear. Among all infants, it is possible that the younger GA at NICU admission in the IDF group contributed to the earlier oral feedings. In the <32 week cohort, the older GA at NICU admission in the IDF group was not accompanied by a difference in PMA at first oral feeding. However, this group did have a shorter LOS despite equivalent PMA at discharge, which could be attributed to benefits of the IDF protocol or, more likely, is related to their older age at admission and greater developmental maturity.
It is possible that the lack of significant differences between the two groups could be attributed to the effects of history that unfortunately could not be formally measured. At the time the IDF model was implemented, the multidisciplinary feeding team had spent several months with nursing staff and NICU providers assessing feeding in the NICU and identifying areas for improvement. Through this process, bedside in situ training was naturally provided to bedside nursing staff, prior to them completing formal IDF training modules. This training may have resulted in earlier changes in bedside nursing behaviors, as well as improved teaching of caregivers at the bedside. Unfortunately, we do not have data to support this possible early learning impact on infant feeding.
Unexpectedly, the earlier PMA at first feed found in the IDF group did not correspond to an earlier PMA at NG removal. The lack of a difference in age at NG removal between the protocols could be related to specific protocols at our NICU that dictate when and how NG tubes should be removed, independent of the age at which oral feeding is established. Prior to the initiation of IDF, there was no formal protocol in place for NG tube removal, and was instead directed by each provider, many of whom waited until closer to 100% of required volumes were achieved. We currently remove the infants’ NG tubes once they have reached 70% of their required volumes. This variation in protocol over time could account for the failure to detect a difference in this metric. We also predicted that IDF protocols would lead to increased rates of breastfeeding at discharge [17], and the lack of a difference between the two protocols suggests that there are likely other factors that play a more significant role in determining whether an infant will be breastfed. For instance, despite our NICU’s emphasis on feeding quality, caregiver desire to quantify volume consumed could contribute to a preference for bottle feeding. Another factor could be maternal perceptions and beliefs about breastfeeding. Previous research has demonstrated that personal, cultural, social, and environmental factors are common influencing factors in the decision to breastfeed alongside mother’s knowledge and attitudes coupled with partners’ support [32, 33]. Considering the benefit of breastfeeding on infant weight gain during the first year of life, it would be useful to further study how NICU feeding protocols impact caregiver decisions [19, 34, 35].
Among all infants and the <35 week cohort, we did not find that the IDF protocol lead to earlier PMA of infants at discharge or impact their LOS. However, we did observe the IDF protocol led to a shorter LOS in the 32 week cohort despite not achieving earlier oral feedings or PMA at discharge. The discrepancy between these two findings is noteworthy, as it suggests the IDF protocol may have a unique impact on and/or interrelate with factors that determine LOS such as medical status and provider comfort. The shorter LOS for these infants could also be related to the home NG program our hospital operates, allowing some infants to leave the hospital before NG discontinuation. The lack of significant difference in LOS for infants that did attain successful oral feeding earlier with the IDF protocol is notable, as multiple quality improvement projects noted decrease LOS for these infants [4, 5, 30, 36, 37]. This lack of difference among all infants and in the <35 week cohort may also be explained by patient, institution, and provider-specific factors independent of the IDF protocol that impact LOS, such as provider comfort, family involvement in feeding, weight gain, number of days without NG tube in place, along with the presence and length of concerning cardiopulmonary events.
To our knowledge, this is the largest study to retrospectively analyze the outcomes following initiation of the IDF protocol and there are several noteworthy implications of our findings. The first is that IDF protocols can be instituted to achieve earlier successful oral feeding in NICU patients, although their use does not seem to increase the likelihood that these patients will be breastfeeding at discharge or have shorter LOS. The second is that there are likely several factors independent of the use of IDF and the earlier establishment of oral feedings, such as underlying health status and medical comorbidities, that impact outcomes like age at NG removal, age at discharge and LOS.
Many of the factors that influence the decision to discharge infants from the NICU have been identified including physiologic stability, an active program of parental involvement and preparation for care of the infant at home, arrangements for health care after discharge by a physician or other health care professional who is experienced in the care of high-risk infants, and an organized program of tracking and surveillance to monitor growth and development [34]. Family factors such as substance abuse, relationship instability, parental age, mental health problems, and socioeconomic status all play a role in dictating LOS and age at discharge as well [38]. Understanding the relationship between earlier initiation of oral feeding with an IDF program and these factors should be the target of future study. Inadequate oral feeding has been previously shown to be the most common barrier to discharge in moderately preterm infants [39, 40], but our results indicate that even if a preterm infant has an earlier age at first feed that does not mean they will reach full oral feeds sooner. IDF did not decrease the barrier that inadequate oral feeding poses to discharge.
We note some limitations to the study. Inherent to the cross-sectional design is the ability to only demonstrate association and not cause and effect. Further, there were an insufficient number of infants in our cohort who experienced long-term feeding difficulties that necessitated interventions such as gastrostomy tube placement, long-term NG use, or admission for FTT, making it impossible to differentiate if our IDF program had an impact on these outcomes. Additionally, we did not collect data on many of the aforementioned NICU discharge factors and thus could not identify if there was an independent relationship between these factors and age at discharge or LOS. Our exclusion criteria were similar to prior studies and contained many of the established risk factors for FTT [41, 42]. These factors include mechanical feeding problems (I.e., cleft palate or central nervous system dysfunction), increased metabolic demands (I.e., congenital heart defects), poor utilization (I.e., trisomy 21), or malabsorption (I.e., necrotizing enterocolitis). As these infants were excluded, the results of our study are not generalizable to infants with these conditions. We also had a smaller number of infants in the <32 week sub-group (n = 117). Increasing the number of subjects born in this period might demonstrate greater effect of IDF on feeding behaviors in this group.
There are several areas for future research based on our findings. A prospective, randomized controlled trial that followed infants after NICU discharge could provide more compelling evidence for the benefits of the IDF protocol and determine the long-term implications of earlier successful oral feedings such as need for later G-tube placement or FTT admission. A prospective trial with special attention to the uniform application of the IDF protocol would also be able to more effectively assess its impact. Specifically, under our current protocol all nurses were trained with a 4-h IDF course and had a nurse champion to complete bedside training. The addition of a treatment fidelity follow-up assessment would further ensure consistent protocol application over the time period of our study. A prospective study could also clarify whether there is an independent association between the IDF protocol and the decision to breastfeed, the age at NG removal, the NICU LOS, and the age at discharge. Further defining what infant and family-specific factors influence these outcomes is an area for futures study. Additionally, it would be valuable to study the impact of the IDF protocol on the special populations of infants excluded in this study. Our study did not demonstrate a decreased LOS or significant difference in age at NG removal for the IDF infants.
There are potential benefits that IDF may provide that were not measured in our study. The IDF protocol aims to decrease negative feeding experiences that can result in the development of feeding aversions [43]. This is a very worthwhile goal as children who were born preterm have been documented to make up a large percentage of patients later seen within a pediatric feeding disorder clinic [44]. A previous study indicated an increase in perceived parent satisfaction along with increased provider satisfaction with the implementation of the IDF protocol [24]. In addition, previous research has shown that the IDF Readiness Scale can be used as a metric to identify infants who are at increased risk for feeding difficulties, this is a promising potential benefit of IDF in that it would allow for earlier targeted interventions [27]. While the present study did not examine these effects, the aforementioned studies evince clear benefit in addition to the earlier initiation of oral feeding we observed. Further examining these outcomes would be another compelling aim for future study.
In conclusion, we showed that the utilization of an IDF program in a large midwestern NICU led to the initiation of oral feeding at an earlier PMA overall compared with a traditional feeding protocol, although not for infants <35 weeks of gestation. IDF corresponded to a shorter LOS only in the cohort of infants born <32 weeks. However, the initiation of this program did not lead to earlier PMA at NG tube removal, PMA at discharge, or increases in the rates of breastfeeding at discharge.
References
Jadcherla S, Wang M, Vijayapal A, Leuthner S. Impact of prematurity and co-morbidities on feeding milestones in neonates: a retrospective study. J Perinatol. 2009;30:201–8.
Kirk A, Alder S, King J. Risk factors for poor oral feeding progression in premature infants. J Investigative Med. 2006;54:S98.
Park J, Knafl G, Thoyre S, Brandon D. Factors associated with feeding progression in extremely preterm infants. Nurs Res. 2015;64:159–67.
Gelfer P, McCarthy A, Turnage, Spruill C. Infant driven feeding for preterm infants: learning through experience. Newborn Infant Nurs Rev. 2015;15:64–7.
Settle M, Francis K. Does the infant-driven feeding method positively impact preterm infant feeding outcomes? Adv Neonatal Care. 2019;19:51–5.
Underwood MA. Human milk for the premature infant. Pediatr Clin North Am. 2013;60:189–207.
Bu’Lock F, Woolridge MW, Baum JD. Development of co‐ordination of sucking, swallowing and breathing: ultrasound study of term and preterm infants. Developmental Med Child Neurol. 1990;32:669–78.
Weber F, Woolridge MW, Baum JD. An ultrasonographic study of the organisation of sucking and swallowing by newborn infants. Dev Med Child Neurol. 1986;28:19–24. https://doi.org/10.1111/j.1469-8749.1986.tb03825.x.
Paul K, Dittrichová J, Papousek H. Infant feeding behavior: development in patterns and motivation. Dev Psychobiol. 1996;29:563–76. 10.1002/(SICI)1098-2302(199611)29:7<563::AID-DEV2>3.0.CO;2-S.
Whetten CH. Cue-based feeding in the NICU. Nurs Women’s Health. 2016;20:507–10. https://doi.org/10.1016/j.nwh.2016.08.006.
Lau C. Development of oral feeding skills in the preterm infant. Arch Pediatr. 2007;14S35–41. https://doi.org/10.1016/s0929-693x(07)80009-1.
Whyte RK. Neonatal management and safe discharge of late and moderate preterm infants. Semin Fetal Neonatal Med.2012;17:153–8. https://doi.org/10.1016/j.siny.2012.02.004.
Mizuno K, Ueda A. The maturation and coordination of sucking, swallowing, and respiration in preterm infants. J Pediatr. 2003;142:36–4.
Berseth CL. Gastrointestinal motility in the neonate. Clin Perinatol. 1996;23:179–90.
Breton S, Steinwender S. Timing introduction and transition to oral feeding in preterm infants: current trends and practice. Newborn Infant Nurs Rev. 2008;8:153–9.
Shaker CS. Cue-based feeding in the NICU: using the infant’s communication as a guide. Neonatal Netw. 2013;32:404–8.
Newland L, L’huillier MW, Petrey B. Implementation of cue-based feeding in a level III NICU. Neonatal Netw. 2013;32:132–7.
Brown A, Arnott B. Breastfeeding duration and early parenting behaviour: the importance of an infant-led, responsive style. PLoS ONE. 2014;9:e83893. https://doi.org/10.1371/journal.pone.0083893.
Ventura AK, Thompson K. Predictors of resilience among infants at risk for rapid weight gain. Obesity. 2019;27:130–6.
McCain GC, Gartside PS, Greenberg JM, Lott JW. A feeding protocol for healthy preterm infants that shortens time to oral feeding. J Pediatr. 2001;139:374–9.
McCain GC, Moral TD, Duncan RC, Fontaine JL, Pino LD. Transition from gavage to nipple feeding for preterm infants with bronchopulmonary dysplasia. Nurs Res. 2012;61:380.
Kish MZ. Improving preterm infant outcomes: implementing an evidence-based oral feeding advancement protocol in the neonatal intensive care unit. Adv Neonatal Care. 2014;14:346–53.
Watson J, McGuire W. Responsive versus scheduled feeding for preterm infants. Cochrane Database Syst Rev. 2016:CD005255. https://doi.org/10.1002/14651858.
Wellington A, Perlman JM. Infant-driven feeding in premature infants: a quality improvement project. Arch Dis Child Fetal Neonatal Ed. 2015;100:F495–500.
Davidson E, Hinton D, Ryan-Wenger N, Jadcherla S. Quality improvement study of effectiveness of cue-based feeding in infants with bronchopulmonary dysplasia in the neonatal intensive care unit. J Obstet Gynecol Neonatal Nurs. 2013;42:629–40.
Puckett B, Grover VK, Holt T, Sankaran K. Cue-based feeding for preterm infants: a prospective trial. Am J Perinatol. 2008;25:623–8.
Giannì ML, Sannino P, Bezze E, Plevani L, Esposito C, Muscolo S, et al. Usefulness of the infant driven scale in the early identification of preterm infants at risk for delayed oral feeding independency. Early Hum Dev. 2017;115:18–22.
Ludwig S, Waitzman R. Changing feeding documentation to reflect infant-driven feeding practice. Newborn Infant Nurs Rev. 2007;7:155–60.
Fry T, Marfurt S, Wengier S. Systematic review of quality improvement initiatives related to cue-based feeding in preterm infants. Nurs Women’s Health. 2018;22:401–10.
Kirk A, Alder S, King J. Cue-based oral feeding clinical pathway results in earlier attainment of full oral feeding in premature infants. J Perinatol. 2007;27:572–8.
Dalgleish SR, Kostecky LL, Blachly N. Eating in “SINC”: safe individualized nipple-feeding competence, a quality improvement project to explore infant-driven oral feeding for very premature infants requiring noninvasive respiratory support. Neonatal Netw. 2016;35:217–27.
Kong SK, Lee DT. Factors influencing decision to breastfeed. J Adv Nurs. 2004;46:369–379. https://doi.org/10.1111/j.1365-2648.2004.03003.
Arora S, McJunkin C, Wehrer J, Kuhn P. Major factors influencing breastfeeding rates: mother’s perception of father’s attitude and milk supply. Pediatrics. 2000;106:e67. https://doi.org/10.1542/peds.106.5.e67.
Li R, Magadia J, Fein SB, Grummer‐Strawn LM. Risk of bottle‐feeding for rapid weight gain during the first year of life. Arch Pediatr Adolesc Med. 2012;166:436.
Ventura AK. Developmental trajectories of bottle‐feeding during infancy and their association with weight gain. J Dev Behav Pediatr. 2017;38:119.
Chrupcala KA, Edwards TM, Spatz DL. A continuous quality improvement project to implement infant-driven feeding as a standard of practice in the newborn/infant intensive care unit. J Obstet Gynecol Neonatal Nurs. 2015;44:654–64.
American Academy of Pediatrics Committee on Fetus and Newborn. Hospital discharge of the high-risk neonate. Pediatrics. 2008;122:1119–26.
Smith V, Hwang S, Dukhovny D, Young S, Pursley DM. Neonatal intensive care unit discharge preparation, family readiness and infant outcomes: connecting the dots. J Perinatol. 2013;33:415–21.
Brumbaugh J, Colaizy T, Saha S, Van Meurs K, Das A, Walsh M, et al. Oral feeding practices and discharge timing for moderately preterm infants. Early Hum Dev. 2018;120:46–52.
Edwards L, Cotton CM, Smith PB, Goldberg R, Saha S, Das A. et al. Inadequate oral feeding as a barrier to discharge in moderately preterm infants. J Perinatol. 2019;39:1219–28. https://doi.org/10.1038/s41372-019-0422-x.
Crosson DD, Pickler RH. An integrated review of the literature on demand feedings for preterm infants. Adv Neonatal Care. 2004;4:216–25.
Nangia S, Tiwari S. Failure to thrive. Indian J Pediatr. 2013;80:585–9.
Browne JV, Ross ES. Eating as a neurodevelopmental process for high-risk newborns. Clin Perinatol. 2011;38:731–43.
Jung JS, Chang HJ, Kwon JY. Overall profile of a pediatric multidisciplinary feeding clinic. Ann Rehabil Med. 2016;40:692–701. https://doi.org/10.5535/arm.2016.40.4.692.
Acknowledgements
The authors would like to thank the healthcare team involved in selecting and implementing the IDF protocol and sharing electronic medical record information for the relevant patients. There were no sources of support or material to report.
Author information
Authors and Affiliations
Contributions
CBB, WMB, AL, JP, AES, and JRB: involved in study conception and design. AL and JP: involved in data acquisition. JRB and AES: involved in data analysis. CBB, AL, and JP: involved in interpretation of data analysis and first draft of manuscript. CBB, WMB, SFR, AES, and JRB: critical revision of the manuscript. All authors: approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lane, A., Pacella, J., Beal, J.R. et al. A cross-sectional analysis of infant-driven and traditional feeding outcomes for neonatal intensive care unit infants. J Perinatol 41, 1865–1872 (2021). https://doi.org/10.1038/s41372-021-01084-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01084-9
- Springer Nature America, Inc.