Abstract
Background:
Identifying congenital hypothyroidism through newborn screening (NBS) is higher among moderate-to-late preterm (MLPT) infants. Currently, the same thyroid-stimulating hormone (TSH) cutoffs are used for term and preterm infants. TSH reference ranges for MLPT infants are not currently available.
Objective:
To determine TSH reference ranges for MLPT infants.
Methods:
We analyzed 10,987 TSH levels on NBS samples performed on 8499 MLPT infants born between 32 and 36 weeks gestation.
Results:
TSH median, 5th, 25th, 75th, 95th, and 99th percentiles were defined from day 1 until day 14 of life. TSH levels gradually decreased after birth and reached a plateau around day 6.
Conclusion:
Using a state-wide cohort, we constructed TSH reference charts from day 1 until day 14 for MLPT infants. Relationship between age-adjusted TSH percentiles and long-term neurodevelopmental outcomes should be determined in future studies to define optimal TSH cutoffs for MLPT infants.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Congenital hypothyroidism (CH) is diagnosed with increased frequency among preterm infants [1,2,3]. Incidence of CH is 2.5 times higher among moderate-to-late preterm (MLPT) infants (32–36 weeks) compared with infants born at term [3].
Differences in thyroid axis physiology exist among term and preterm born infants during the first month of life [4]. Preterm infants exhibit qualitatively smaller postnatal surge in thyroid-stimulating hormone (TSH) and thyroid hormone levels, which correlates with gestational age [4]. Despite these differences in thyroid axis physiology, the same TSH-screening cutoffs are used for term and preterm infants by newborn screening (NBS) programs, an approach that may misclassify preterm infants as hypothyroid. In a previous publication, we defined TSH reference ranges for extremely preterm (22–27 weeks) and very preterm infants (28–31 weeks) [5]. TSH reference ranges for MLPT infants are not currently available.
The objective of the current study was to determine TSH reference ranges for MLPT infants using a state-wide cohort of preterm infants in Wisconsin.
Methods
All preterm infants born between 32 and 36 weeks of gestation who underwent NBS in Wisconsin in 2015 and 2016 were included in the study. Infants who had their first NBS done after 96 hours of life and infants with incomplete data were excluded. Demographic data and TSH levels were extracted from NBS database maintained by the Wisconsin state NBS program. TSH values obtained after diagnosis of CH were removed from the analysis. The University of Wisconsin–Madison institutional review board determined that the study qualifies for exemption.
Wisconsin state NBS program uses primary TSH test-screening strategy and performs serial newborn screenings for infants with extended hospital stay. Initial specimen is collected at 24–48 hours of life. In infants with a birth weight <2200 g who has an extended hospital stay, a second specimen is collected at 2 weeks of life, a third specimen is collected at 28–30 days of life or at discharge, whichever comes first, and specimens are collected monthly thereafter until discharge. In infants with a birth weight ≥2200 g who has an extended hospital stay, a second specimen at the time of discharge or at one month of age, if hospital stay is longer than 1 month. Newborn-screening TSH was measured by solid phase, time-resolved fluoroimmunoassay from dried newborn blood spots using PerkinElmer’s AutoDELFIA platform (Waltham, MA, USA). The TSH measurements were then converted to estimated serum levels with the conversion fact: 1 µU/mL blood = 2.22 µU/mL serum (assuming 55% hematocrit). The software on AutoDELFIA platform rounded the TSH values to a whole number. TSH values recorded as 0 were included as truncated values <0.1 for the analysis.
Data analysis was performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). The non-parametric quantile regression approach on the basis of B-splines was used to construct the reference charts for TSH. Age distributions were assumed for TSH. Estimate of the slope parameter q was performed by using the computationally efficient simplex algorithm. The quantile regression was performed. TSH median, 5th, 25th, 75th, 95th and 99th percentiles were defined daily from day 1 until day 14 of life.
Results
A total of 9246 MLPT infants born between 32 and 36 weeks gestation underwent newborn screening in Wisconsin in 2015 and 2016. After the exclusion of 747 infants based on pre-defined exclusion criteria, the final study cohort consisted of 8499 infants. A total of 10987 TSH values done between birth and day of life fourteen were included in the analysis.
Mean gestational age and birth weight were 35.0 ± 1.2 weeks and 2477 ± 522 grams, respectively. The study cohort was comprised of 53% males and 73% Caucasians. Twins/ triplets accounted for 18% of the study cohorts (Table 1).
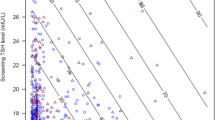
TSH values corresponding to percentiles are presented in Fig. 1 and Table 2. TSH level was highest on day one. Median TSH level on day 1 was 9.4 μIU/ml. TSH values corresponding to 95th and 99th percentiles on day 1 were 21.5 and 29.9 μIU/ml, respectively. TSH levels gradually decreased from day 1 and reached a plateau around day 6. The TSH concentration for 95th and 99th percentile on day 7 was 7.9 and 12.7 μIU/ml, respectively, whereas the TSH concentration for 95th and 99th percentile on day 14 was 8.9 and 13.3 μIU/ml, respectively.
Discussion
Using a state-wide cohort in Wisconsin, this study defines the TSH reference ranges from day 1 to day 14 of life for MLPT infants. Our group previously published similar reference ranges for extremely and very preterm infants [5]. These data help to fill the knowledge gap in understanding of postnatal TSH levels in MLPT infants.
MLPT infants make up ~8.5% of all births in the USA and account for >80% of all preterm births [6]. This group of infants has higher morbidity and mortality compared with term born infants [7, 8]. MLPT infants are also at higher risk of long-term neurodevelopmental sequelae such as learning difficulties and minor deficits in cognitive function [9].
During the study period, the incidence of CH among MLPT infants in Wisconsin was 1 in 616. This was 2.4 times higher than the CH incidence of 1 in 1468 among term infants and accounted for 12% of CH cases detected by the newborn screening program.
Previous studies have reported higher incidence of CH in low birth weight (1500–2500) infants. Low birth-weight infants likely represent MLPT infants even though these reports have not specified gestational age categories [2, 10]. Another study reported comparable CH detection rates in MLPT infants requiring neonatal intensive care admissions compared to infants born <32 weeks [11].
Results from the current study differ from previously available data on TSH levels of MLPT infants [4, 12]. Most importantly, the gestational age range defined in our study is different from previous studies. Median TSH levels on day 1 (average age 28 hours) in our cohort of 32–36 gestational age infants was 9.4 μIU/ml compared with mean TSH level of 7.3 μIU/ml at 24 hours of life of infants born at 31–34 weeks [12]. Another study reported median TSH levels of 2.6 and 2.5 μIU/ml on day 7 and 14 for infants born at 31–34 weeks [4]. These values were relatively similar to those of our study cohort, in whom corresponding median TSH levels at day 7 and 14 were 2.2 and 2.9 μIU/ml, respectively. By analyzing a much larger cohort than these prior studies, and including preterm infants born at 35–36 weeks of gestation, this study could define TSH reference ranges for MLPT infants.
Compared with extremely (22–27 weeks) and very (28–31 weeks) preterm infants, corresponding upper reference range TSH percentile values for MLPT infants were lower (Fig. 2). On day 7 of life TSH level corresponding to 95th percentile was 14, 13.1, and 7.9 μIU/ml for extremely, very, and MLPT infants respectively. On day 14 of life TSH level corresponding to 95th percentile was 12.7, 10.6, and 8.9 μIU/ml for extremely, very, and MLPT infants respectively [5].
The main strength of the current study is the size of the study cohort compared with previous similar studies, but there are also several limitations. Patients with chromosomal or multiple congenital anomalies were not excluded since this information was also not available. TSH values given here are estimated serum values from dried blood spot TSH values and TSH reference ranges were only defined up until day 14 of life. Although the majority of preterm infants are detected on screenings done on or after 2 weeks of life, the number of moderate-to-late preterm infants undergoing newborn screening was too few after 2 weeks to reliably define TSH reference ranges beyond this time.
The reference ranges described here provides a framework for designing future studies investigating possible relationships between gestational age-adjusted TSH percentiles and long-term growth and neurodevelopmental outcomes. These studies will define TSH percentiles that optimize sensitivity and specificity in identifying infants who require thyroxine supplementation. Standardization of CH-screening strategies using gestational age-adjusted TSH cutoffs across newborn-screening programs will also reduce misclassification of patients.
Conclusion
This study defines TSH reference ranges from birth to day 14 of life in MLPT infants. Upper limits of TSH reference ranges in this group were lower than preterm infants born <32 weeks of gestation. Long-term neurodevelopmental follow-up studies are needed to determine whether correct gestational age-adjusted TSH cutoffs can identify infants at risk for clinically significant CH necessitating thyroid hormone replacement therapy.
References
Wassner AJ, Brown RS. Congenital hypothyroidism: recent advances. Curr Opin Endocrinol Diabetes Obes. 2015;22:407–12.
Mitchell ML, Hsu HW, Sahai I. The increased incidence of congenital hypothyroidism: fact or fancy? Clin Endocrinol. 2011;75:806–10.
Kaluarachchi DC, Allen DB, Eickhoff JC, Dawe SJ, Baker MW. Increased congenital hypothyroidism detection in preterm infants with serial newborn screening. J Pediatr. 2019;207:220–5.
Williams FLR, Simpson J, Delahunty C, Ogston SA, Bongers-Schokking JJ, Murphy N, et al. Developmental trends in cord and postpartum serum thyroid hormones in preterm infants. J Clin Endocrinol Metab. 2004;89:5314–20.
Kaluarachchi DC, Allen DB, Eickhoff JC, Dawe SJ, Baker MW. Thyroid-stimulating hormone reference ranges for preterm infants. Pediatrics 2019;144:e20190290.
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: final data for 2018. Natl Vital- Stat Rep. 2019;68:1–47.
Walsh MC, Bell EF, Kandefer S, Saha S, Carlo WA, D’angio CT, et al. Neonatal outcomes of moderately preterm infants compared to extremely preterm infants. Pediatr Res. 2017;82:297–304.
Stewart DL., Barfield WD Committee on fetus and newborn. Updates on an at-risk population: late-preterm and early-term infants. Pediatrics. 2019;144:e20192760.
Vohr B. Long-term outcomes of moderately preterm, late preterm, and early term infants. Clin Perinatol. 2013;40:739–51.
Mandel SJ, Hermos RJ, Larson CA, Prigozhin AB, Rojas DA, Mitchell ML. Atypical hypothyroidism and very low birthweight infant. Thyroid. 2000;10:693–5.
Zung A, Yehieli A, Blau A, Almashanu S. Characteristics of delayed thyroid stimulating hormone elevation in neonatal intensive care unit newborns. J Pediatr. 2016;178:135–40.
Murphy N, Hume R, van Toor H, Matthews TG, Ogston SA, Wu SY, et al. The hypothalamic-pituitary-thyroid axis in preterm infants; responsiveness to birth over the first 24 h of postnatal life. J Clin Endocrinol Metab. 2014;89:2824–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaluarachchi, D.C., Nicksic, V.M., Allen, D.B. et al. Thyroid-stimulating hormone reference ranges for moderate-to-late preterm infants. J Perinatol 41, 2664–2667 (2021). https://doi.org/10.1038/s41372-020-00895-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-00895-6
- Springer Nature America, Inc.
This article is cited by
-
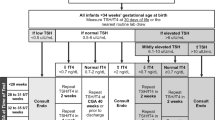
A practical gestational age-based algorithm for timely detection of hypothyroidism in premature infants
Journal of Perinatology (2024)