Abstract
Objective
To describe trends in the incidence and severity of meconium aspiration syndrome (MAS) around the release of revised Neonatal Resuscitation Program (NRP) guidelines in 2016.
Study design
The California Perinatal Quality Care Collaborative database was queried for years 2013–2017 to describe the incidence and outcomes of infants with MAS. Results were analyzed based on both individual years and pre- vs. post-guideline epochs (2013–15 vs. 2017).
Result
Incidence of MAS decreased significantly from 2013–15 to 2017 (1.02 to 0.78/1000 births, p < 0.001). Among infants with MAS, delivery room intubations decreased from 2013–15 to 2017 (44.3 vs. 35.1%; p = 0.005), but similar proportion of infants required invasive respiratory support (80.1 vs. 80.8%), inhaled nitric oxide (28.8 vs. 28.4%) or extracorporeal membrane oxygenation (0.81 vs. 0.35%).
Conclusion
While the study design precludes confirmation of implementation of the recent NRP recommendation, there was no increase in the incidence or severity of MAS following its release.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
The 17 edition of the Neonatal Resuscitation Program (NRP) revised the approach to nonvigorous infants born through meconium stained amniotic fluid (MSAF) [1]. Current NRP guidelines state that resuscitation of infants with MSAF should follow the same principles as for those with clear fluid, but an individual skilled in tracheal intubation should be present at the time of birth. If a baby is born through MSAF and has depressed respirations or poor muscle tone, the baby is to be placed on the radiant warmer and initial steps of newborn care are implemented. Positive pressure ventilation should be initiated if the baby is not breathing or the heart rate is less than 100/min with emphasis on provision of ventilation in nonbreathing or ineffectively breathing infants within the first minute after delivery. Prior to these changes, the recommendation was to do immediate tracheal suctioning in depressed babies born via MSAF [1,2,3]. This is the most recent in a series of changes in managing these infants over the last two decades. These guidelines were published in October 2015. The NRP instructor course with new recommendations became available in spring 2016, it recommended mandatory instruction of new guidelines by January 1, 2017.
Several large multicenter trials were conducted over the last two decades and led to important changes in our approach to infants born with MSAF. Wiswell et al. conducted a multicenter, randomized controlled trial evaluating suction vs. no suction among 2094 vigorous infants born with MSAF and showed no difference in outcome [4]. Similarly, routine amnioinfusion and suctioning of the mouth and nose after delivery of the head were found to be ineffective in reducing the incidence of meconium aspiration syndrome (MAS) in multicenter randomized controlled trials involving 1998 and 2514 subjects, respectively [5, 6].
In contrast, the three randomized controlled trials evaluating nonvigorous infants born with MSAF and comparing routine tracheal suction vs. no suction involved a smaller number of subjects (total of 449) and were conducted in single centers in India [7,8,9]. The first two studies showed no difference in the incidence of MAS, mortality or other available outcomes [7, 8]. Singh et al. reported a shorter length of stay in the suction group (9.91 ± 3.06 vs. 11.17 ± 3.73, p = 0.02) and a trend towards a lower incidence of MAS (41.3% vs. 57.1%, p = 0.052) [9]. Combining data from these three studies generates an unadjusted odds ratio of 0.89 (95% confidence intervals 0.61, 1.31, p = 0.56).
Recently, Chiruvolu et al. reported increased NICU admissions for respiratory causes without any significant difference in MAS in an observational study (n = 231) among nonvigorous infants born through MSAF before and after implementing the no-suction policy in their institutions [10]. In an accompanying editorial, Dr Wiswell emphasized the importance of ongoing surveillance following significant changes to the NRP algorithm [11]. There are no studies evaluating the prevalence of MAS in a wide geographic region before and after release of the most recent guidelines.
The aim of this study was to evaluate trends in the incidence of MAS in California and associated morbidity and mortality among infants who were admitted to NICU with MAS around the release of change in NRP recommendations. All NICUs belonging to the California Perinatal Quality Control Collaborative (CPQCC, ~93% of NICUs in the state) from 2013 to 2017 were included in the study.
Methods
The study was approved as exempt from full review by the Institutional Review Board of the University of California Davis Health System. The total number of births and hospital admissions related to meconium aspiration in California was obtained from the patient discharge data (PDD) compiled by California Office of Statewide Health and Planning Development (OSHPD) from 2013–2017. OSPHD collects PDD from all birthing hospitals in California, except for military hospitals. To maintain data accuracy and ensure that a patient was not counted multiple times in case of transfer to a center for higher level of care, only the patients with meconium aspiration diagnosed at birth in the admitting hospital were included in this OSHPD analysis. Meconium aspiration incidences with and without respiratory symptoms were identified by screening PDD using International Classification of Disease (ICD) 9th and 10th revision codes. P24.00 in ICD-10-CM (and 770.11 in ICD-9-CM) refers to meconium aspiration without respiratory symptoms, whereas P24.01 (and 770.12 in ICD-9) refers to meconium aspiration with respiratory symptoms and includes meconium aspiration pneumonia/pneumonitis and MAS not otherwise specified. These diagnoses codes were used in the OSHPD PDD dataset. The total number of admissions to the NICUs in California was obtained from California Children’s Services (CCS) data. Details on the source of information and number of infants can be found in Fig. 1.
The CPQCC database was queried to describe the incidence, therapeutic modalities, and outcome characteristics for infants who were born at a CPQCC center and developed MAS for the years 2013–2017. All CCS approved and about 93% of all NICUs in California reported their data to CPQCC over the study period. Around ten NICUs in the state do not share the data. The dataset contains de-identified patient information, using standard definitions as outlined by the Vermont Oxford Network [12]. This database is designed to count each infant only once even if a patient is transferred from one CPQCC NICU to other for higher level of care. Data are abstracted by NICU personnel (i.e., physicians, nurses and other trained abstractors) and submitted through an online portal. Demographics, maternal and delivery history, postdelivery diagnosis, and interventions are collected for every eligible infant (all infants with birth weight ≤ 1500 g or gestational age ≤ 32 weeks plus infants above 1500 g and >32 weeks gestational age at birth who meet the following eligibility criteria: death, acute transport, early bacterial sepsis, major surgery, intubated or nonintubated assisted ventilation > 4 h, suspected encephalopathy or asphyxia, or active therapeutic hypothermia).
We used a combination of individual level data and aggregate data collection for this study. In addition to the individual patient-level data collection for those eligible infants noted above, each NICU provides annual data on total NICU admissions and total births to their center according to gestational age categories.
Data were extracted for infants who were admitted with a diagnosis of MAS. The CPQCC criteria for the diagnosis of MAS includes all of the following: (a) presence of MSAF at birth, (b) respiratory distress with onset within 1 h of birth, (c) central cyanosis in room air or a requirement of supplemental oxygen to maintain PaO2 > 50 mm Hg, (d) abnormal chest radiograph compatible with the diagnosis of MAS, (e) absence of culture-proven early onset bacterial sepsis or pneumonia. If all the criteria’s are not met, than the patient is not labeled as MAS as per CPQCC definition.
All neonates receiving care at a CPQCC NICU reporting on data variables used for this study were included. Antenatal details collected included maternal demographics and other factors such as hypertension during pregnancy, intrauterine growth restriction, fetal distress, prolonged labor, prolonged rupture of membranes, chorioamnionitis, and mode of delivery. Postnatal variables to determine the severity of respiratory distress and amount of respiratory support provided to infants during their NICU stay were collected. Information on final disposition, average length of stay and associated comorbidities were also analyzed.
To compare outcomes prior to and following the recommendation changes surrounding routine tracheal suctioning, we selected two epochs: prerecommendation epoch 1 (2013–15) and postrecommendation epoch 2 (2017). The year 2016 was omitted as a washout year from these analyses.
Statistical analysis
The yearly incidence of meconium aspiration as a proportion of all deliveries and all NICU admissions were calculated with numbers obtained from the statewide hospital admission summary and the CCS database. For a secondary analysis on overall estimates of state incidence of MAS as per CPQCC criteria, we assumed that the majority of infants with MAS requiring NICU care would be either delivered at or transferred to a CPQCC center.
The Cochran–Armitage test for trend was performed to access yearly trends in MAS admissions and associations between meconium aspiration admission to hospitals, meconium aspiration with respiratory symptoms, NICU admissions at birth, NICU admissions at birth meeting CPQCC criteria, and MAS patients admitted to CPQCC centers meeting CPQCC definition (inborn and outborn) over the years 2013 through 2017. Simple linear regression was conducted to investigate linear trends for rates during the study period. Chi square test or Fisher exact test was performed to investigate differences in associations of proportions in delivery room respiratory support, maternal and obstetric characteristics, clinical characteristics, and outcomes of inborn infants appropriately.
Bivariate analysis was conducted to evaluate maternal and obstetric characteristics of infants, baseline characteristics of neonates, and characteristics of postdelivery room respiratory support and outcome by year. P-values for categorical outcomes were calculated with the chi-squared or Fisher’s exact test. T-tests were conducted to calculate the p-values for continuous outcomes. Bivariate analysis was conducted to evaluate the differences in the incidence of NICU admissions with MAS and associated clinical features between the years 2013–2015 and 2017. Chi-squared tests were conducted to assess for statistical significance.
Results
Incidence of MAS in the state of California
Between 2013 and 2017; 2,392,524 infants were born in California as per OSHPD PDD database. ICD-9-CM (770.11 and 770.12) and ICD-10-CM (P24.00 and P 24.01) diagnoses codes were used in the OSHPD PDD dataset to determine the incidence of meconium aspiration with and without respiratory symptoms. 8852 neonates (average incidence of 3.7 per 1000 births) had a diagnosis of meconium aspiration during the study period; 3157 (35.6%) of whom had meconium aspiration with respiratory symptoms (average incidence of 1.32 per 1000 births). Details on the source of information and number of infants can be found in Fig. 1. The Cochran–Armitage trend test showed a significant decrease in hospital admissions for meconium aspiration (p < 0.001) from 2013–2017, while incidence of meconium aspiration with respiratory symptoms was unchanged (p = 0.68) (Table 1). Similar statistical results were noted when OSHPD dataset was used to compare incidence per 1000 births between 2013–15 (epoch 1) and 2017 (epoch 2). The overall incidence of meconium aspiration decreased from 4% in epoch 1 to 3.3% in epoch 2 (p < 0.0001). However, the decline in the incidence of patients with meconium aspiration and respiratory symptoms was not significant (1.37 vs. 1.26%, p = 0.06).
More than 90% of neonates requiring NICU care in California receive it at one of the CPQCC participating institutions and this proportion did not change significantly during the study period. From 2013–2017; 277,883 infants (as per CCS data) were admitted to the NICU and 76,534 had a CPQCC qualifying diagnosis. Two thousand five hundred and thirty eight of these admitted neonates had clinical characteristics of MAS as per CPQCC definition (790 were transferred from non-CPQCC birthing facilities). A significant decline in the incidence of MAS as per CPQCC criteria (p < 0.001) was noted during the study period (Table 1).
Incidence of MAS among infants born at CPQCC centers
A total of 1,830,388 infants were born at CPQCC participating institutions from 2013 to 2017, of which 221,144 (12.1%) were admitted to the NICU. Among the NICU admissions, 52,475 infants (2.9% of all births) had a CPQCC qualifying diagnosis; 1748 (0.8% of all NICU admissions) were diagnosed with MAS as per CPQCC criteria. Average incidence of MAS per CPQCC criteria among the inborn infants during the study period was 0.95 per 1000 live births. A significant decline in the incidence of MAS as a percentage of total live births and NICU admissions was noted during the study period (p < 0.05) (Table 2). No significant difference was noted when MAS incidence was compared year by year. Incidence was 1.1 vs. 1.04 (p 0.4), 1.04 vs. 0.93 (p 0.12), 0.93 vs. 0.92 (p 0.88) and 0.92 vs. 0.78 (p 0.054) between 2013–14, 2014–15, 2015–16 and 2016–17, respectively.
Characteristics of infants with MAS born at CPQCC centers
Among inborn infants admitted with MAS at participating centers, maternal, and fetal characteristics were comparable from year to year except for a significant increase in maternal age (p = 0.01), proportion of vaginal births (p = 0.01) and signs of chorioamnionitis around delivery (p = 0.01) (Table 3). A gradual increase in gestational age and birth weight (p < 0.0001) was also noted among infants with MAS during the study period (Table 3). One hundred and seventy one (9.78%) were born with gestational age < 32 weeks and 139 (7.95%) had birth weight < 1500 g. Change in delivery room resuscitation practice was reflected by increased use of noninvasive breathing support with continuous positive airway pressure (CPAP) and a trend towards less intubation in 2017 (p = 0.08, Table 3) among infants with MAS. Umbilical cord pH was available in 27% of infants from 2014 onwards, average (mean ± sd) values were 6.98 ± 0.2, 7.01 ± 0.2, 7.05 ± 0.2, 7.04 ± 0.16 for 2014, 2015, 2016, and 2017 respectively, with a p value of 0.07 (Tables 3–5).
A similar proportion of infants with MAS received respiratory support and intubated (invasive) mechanical ventilation over time in California NICUs (Table 4). The use of noninvasive ventilation for MAS in the NICU increased during the study period (p < 0.001). The utilization of enhanced respiratory support such as inhaled nitric oxide, high frequency ventilation, extracorporeal membrane oxygenation (ECMO), and postnatal use of steroids, did not change among infants admitted with MAS during the study period. The prevalence of morbidities (hypoxic-ischemic encephalopathy and pneumothorax) remained unchanged from year to year (Table 4). Average length of stay gradually decreased during the study period (p = 0.01).
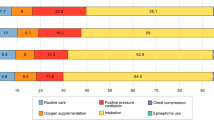
Table 5 compares the characteristics of neonates with MAS in prerecommendation epoch 1 (2013–15) and postrecommendation epoch 2 (2017). A significant decrease in the incidence of MAS as per CPQCC criteria was noted between the two groups (Table 5).
In 2017, after the release of new NRP guidelines, fewer infants with MAS were intubated in the delivery room (Table 5). Noninvasive respiratory support in the NICU was used more often in epoch 2 as compared with epoch 1. There was no significant difference in the use of intubated ventilation, high frequency ventilation, inhaled nitric oxide, or ECMO in 2017 compared with the previous years. Associated conditions such as pneumothorax and moderate/severe hypoxic-ischemic encephalopathy were similar between the two epochs.
Discussion
The guidelines from International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment in October 2015 states that “routine tracheal intubation for suctioning of meconium in nonvigorous infants should not be considered as a standard of care but may be considered a reasonable alternative to no tracheal intubation if a meconium plug is suspected” [3]. The American Heart Association/NRP guidelines in 2015 stated that if the infant born through MSAF presents with poor muscle tone and inadequate breathing efforts, the initial steps of resuscitation should be completed under the radiant warmer. Positive pressure ventilation should be initiated if the infant is not breathing or the heart rate is <100 bpm after initial steps are completed. Routine intubation for tracheal suction in this setting is not suggested [2]. The NRP instructor update was published in spring 2016, it suggested mandatory instruction of the new recommendations by January 1, 2017.
The values that guided the revision of the recommendation were to minimize the risks of intubation and to decrease the time to positive pressure ventilation for the compromised infant, given the lack of evidence to support benefit from routine tracheal suctioning. The two recent publications showing (1) an increase in length of hospital stay and a trend towards increased incidence of MAS and (2) increased respiratory admissions to NICU in nonvigorous infants without routine tracheal suction have questioned this decision [9,10,11]. The current study is the first large geographic area-based surveillance report evaluating the potential impact of these guidelines. We demonstrate that there has not been an increase in the incidence or severity of MAS following the release of new NRP guidelines in California.
Different criteria have been used to characterize the spectrum of disease associated with meconium aspiration in the past [13]. This variation in defining criteria can explain the difference in the incidence when CPQCC vs. statewide admission database was used. While CPQCC uses a strict definition to describe MAS and patients are identified by trained personnel, identifying patients using ICD codes can be more heterogeneous and there would not be standard criteria used by all clinicians throughout the state. Furthermore, ICD codes include all severity levels of meconium aspiration, while only moderate to severe forms of MAS are identified with CPQCC criteria.
Other than the NRP recommendations for increased use of CPAP in the delivery room and no routine tracheal suction for nonvigorous infants born with MSAF, there have been no other major changes in management of these infants since 2013. We queried a large database of nearly 2 million births and 50,000 NICU admissions and found a small increase in NICU admissions over the study period, but no increase in the incidence or severity of MAS. On the contrary, both as a percentage of all births and of NICU admissions, there was a significant decrease in NICU admissions for MAS per CPQCC definition from 2013–15 to 2017. This difference was seen in both year by year and pre- vs. post-epoch guideline analyses. This decline in the incidence was also noted when a statewide hospital admission database was used.
A gradual increase in average maternal age and proportion of babies born via vaginal delivery was noted in the studied cohort; these findings are consistent with the data published in national vital statistics reports [14]. We noted a decline in the incidence of MAS despite a significant increase in average gestational age of the studied cohort. Mean gestational age of the subjects born in 2017 was 1.5 weeks more than the ones born in 2013. These findings are in contrast with those reported by Fischer et al. and Cheng et al., who in their large population-based studies amongst term neonates reported an association between increasing gestational age and incidence of MAS [15, 16]. Contrary to the findings published by Lee et al. showing an association between chorioamnionitis and MAS, our results showed a decrease in the incidence of MAS despite an increase in frequency of chorioamnionitis over the years in the studied cohort [17]. Despite more frequent and early use of noninvasive ventilation, a similar proportion of MAS babies required invasive mechanical ventilation or surfactant over the years. These findings are in contrast to those of Pandita et al. who reported less invasive ventilation with early use of CPAP [18]. It is not possible to determine from the CPQCC database if noninvasive ventilation was used as an initial or weaning mode of respiratory support. The proportion of subjects requiring mechanical ventilation did not change significantly (80%), perhaps indicating that the incidence of severe MAS had come down over the years.
How might not performing routine tracheal suctioning lead to a reduction in admissions with MAS? We speculate that severe MAS and persistent pulmonary hypertension are most likely the result of in-utero aspiration of meconium and remodeling of small pulmonary arteries in the lung [19]. Many nonvigorous infants born with MSAF have evidence of perinatal depression and acidosis as evidenced by low cord/postnatal pH in our cohort. Prompt resuscitation and ventilation of the lungs with positive pressure ventilation without delaying for tracheal suction may potentially limit asphyxia and hypoxic-ischemic damage to both the brain and heart. Animal models have shown higher left atrial pressure and pulmonary venous hypertension following tracheal suctioning for MSAF [20]. Pulmonary venous hypertension and asphyxia can reduce responsiveness to inhaled nitric oxide and increase the need for ECMO [21,22,23]. During the study period, fewer infants were noted to require ECMO; this trend in our database is consistent with the report from the extracorporeal life support organization registry [24]. Whether this decline is secondary to initiation of prompt resuscitation and ventilation in 2017 compared with previous years cannot be determined retrospectively. In addition, tracheal suctioning among nonvigorous neonates born with MSAF results in removal of more than streaks of meconium in only 38% of neonates, limiting the potential benefit of this procedure in the majority [25]. Increases in the use of CPAP in the delivery room and noninvasive ventilation in the NICU occurred during the study period. These factors, along with increase in gestational age and birth weight among infants with MAS, may also have contributed to changes in outcome.
Our study has several limitations. In the OSHPD database, to improve accuracy of the dataset only the patients with meconium aspiration diagnosed at birth in admitting hospitals were included, by doing so we might have missed some babies with meconium aspiration who were either born at home or at a birthing center. Also, by using inborn babies as a filter in the dataset we might have missed some meconium aspiration patients who were not correctly diagnosed at the birth hospital.
We do not know the exact date when each center in the CPQCC changed their delivery room management from routine suction to no-suction for nonvigorous infants with MSAF, or even if they have changed practice at all. Some early adapters might have changed their practice soon after publication of new guidelines in October 2015 and some may have waited until January 2017. Some neonatal resuscitation providers who trained in late 2016 using guidelines from the 6th edition of NRP textbook may potentially continue to provide tracheal suction to nonvigorous infants born through MSAF through 2018. Ultimately, we do not know the strategy that was employed in individual delivery room practice for each patient other than the variables collected by CPQCC.
We could not collect the exact total number of infants with MAS as per CPQCC criteria in the state of California. We included inborn and out born infants with MAS transferred to CPQCC centers to estimate the overall incidence. As CPQCC centers account for 93% of NICUs in the state, we feel confident that the numbers shown in Table 1 are a close approximation of the total incidence of moderate/severe MAS as per CPQCC definition in the state.
Another major limitation to the current study is its retrospective nature and lack of information regarding the presence of MSAF, neonatal state (vigorous vs. nonvigorous) in the delivery room, frequency of tracheal suctioning and reason for intubation in delivery room. Several investigators are planning prospective studies to collect this important information. The study by Chiruvolu et al. demonstrated an increase in NICU respiratory admissions (22 vs. 40%) but no statistically significant change in the incidence of MAS (5 vs. 11% with and without routine tracheal suction) among nonvigorous infants with MSAF [10]. These results are a cause for concern and emphasize the need for further studies evaluating the impact of changes in NRP guidelines as outlined in a recent editorial by Dr Wiswell [11].
What is the ideal denominator for evaluating the incidence of MAS? In our study, we used all births and all NICU admissions and documented a significant reduction in meconium aspiration with both calculations. Chiruvolu et al. used nonvigorous infants born with MSAF as the denominator and reported an increase in respiratory admissions to NICU. While the incidence of deliveries complicated by MSAF in this study was similar between the routine suction and no-suction epochs (12%), the incidence of nonvigorous infants decreased from 10 to 8% possibly secondary to stimulation by obstetric and neonatal providers. The unadjusted odds ratio for respiratory admissions to the NICU using data provided by Chiruvolu et al. changes from 2.28 (1.29, 4.05) if the denominator is nonvigorous infants with MSAF [10] to 1.41 (0.87, 2.30) for all infants with MSAF and 1.44 (0.89, 2.32) for all births. It may be prudent to express the incidence of MAS as a percent of all births, all NICU admissions, all infants with MSAF, and nonvigorous infants with MAS in future publications.
We conclude that the release of guidelines suggesting a change in approach to nonvigorous infants born with MSAF did not result in an increase in the incidence of MAS among CPQCC affiliated NICUs in California. On the contrary, the incidence of MAS decreased following the release of the recommendation. Based on the current study design, we could not confirm the implementation of revised guidelines across California in 2017. Hence, there is not yet conclusive evidence that immediate stimulation and resuscitation is superior to routine intubation for nonvigorous infants with MSAF, though these data do not support a return to the previous recommendation. Further surveillance over time in population-based studies, prospective evaluations, and large randomized or quasi-randomized trials may help to build the evidence for this question.
References
Weiner GM, Zaichkin J. Textbook of neonatal resuscitation. Elk Grove: American Academy of Pediatrics and American Heart Association; 2016.
Wyckoff MH, Aziz K, Escobedo MB, Kapadia VS, Kattwinkel J, Perlman JM, et al. Part 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015;132(18Suppl 2):S543–60.
Perlman JM, Wyllie J, Kattwinkel J, Wyckoff MH, Aziz K, Guinsburg R, et al. Part 7: Neonatal Resuscitation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2015;132(16Suppl 1):S204–41.
Wiswell TE, Gannon CM, Jacob J, Goldsmith L, Szyld E, Weiss K, et al. Delivery room management of the apparently vigorous meconium-stained neonate: results of the multicenter, international collaborative trial. Pediatrics. 2000;105(1 Pt 1):1–7.
Fraser WD, Hofmeyr J, Lede R, Faron G, Alexander S, Goffinet F, et al. Amnioinfusion for the prevention of the meconium aspiration syndrome. N Engl J Med. 2005;353:909–17.
Vain NE, Szyld EG, Prudent LM, Wiswell TE, Aguilar AM, Vivas NI. Oropharyngeal and nasopharyngeal suctioning of meconium-stained neonates before delivery of their shoulders: multicentre, randomised controlled trial. Lancet. 2004;364:597–602.
Chettri S, Adhisivam B, Bhat BV. Endotracheal suction for nonvigorous neonates born through meconium stained amniotic fluid: a randomized controlled trial. J Pediatr. 2015;166:1208–13.e1.
Nangia S, Sunder S, Biswas R, Saili A. Endotracheal suction in term non vigorous meconium stained neonates-A pilot study. Resuscitation. 2016;105:79–84.
Singh SN, Saxena S, Bhriguvanshi A, Kumar M, Chandrakanta, Sujata. Effect of endotracheal suctioning just after birth in non-vigorous infants born through meconium stained amniotic fluid: A randomized controlled trial. Clin Epidemiol Glob Health. 2019;7:165–70.
Chiruvolu A, Miklis KK, Chen E, Petrey B, Desai S. Delivery room management of meconium-stained newborns and respiratory support. Pediatrics. 2018;142:e20181485.
Wiswell TE. Appropriate management of the nonvigorous meconium-stained neonate: an unanswered question. Pediatrics. 2018;142:e20183052.
Edwards EM, Lakshminrusimha S, Ehret DEY, Horbar JD. NICU admissions for meconium aspiration syndrome before and after a national resuscitation program suctioning guideline change. Children. 2019;6:68.
Vain NE, Batton DG. Meconium “aspiration” (or respiratory distress associated with meconium-stained amniotic fluid?). Semin Fetal Neonatal Med. 2017;22:214–9.
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2017. Natl Vital Stat Rep. 2018;67:1–50.
Fischer C, Rybakowski C, Ferdynus C, Sagot P, Gouyon JB. A population-based study of meconium aspiration syndrome in neonates born between 37 and 43 weeks of gestation. Int J Pediatr. 2012;2012:321545.
Cheng YW, Nicholson JM, Nakagawa S, Bruckner TA, Washington AE, Caughey AB. Perinatal outcomes in low-risk term pregnancies: do they differ by week of gestation? Am J Obstet Gynecol. 2008;199:370 e1–7.
Lee J, Romero R, Lee KA, Kim EN, Korzeniewski SJ, Chaemsaithong P, et al. Meconium aspiration syndrome: a role for fetal systemic inflammation. Am J Obstet Gynecol. 2016;214:366.e1–9.
Pandita A, Murki S, Oleti TP, Tandur B, Kiran S, Narkhede S, et al. Effect of nasal continuous positive airway pressure on infants with meconium aspiration syndrome: a randomized clinical trial. JAMA Pediatr. 2018;172:161–5.
Murphy JD, Vawter GF, Reid LM. Pulmonary vascular disease in fatal meconium aspiration. J Pediatr. 1984;104:758–62.
Lakshminrusimha S, Mathew B, Nair J, Gugino SF, Koenigsknecht C, Rawat M, et al. Tracheal suctioning improves gas exchange but not hemodynamics in asphyxiated lambs with meconium aspiration. Pediatr Res. 2015;77:347–55.
Kinsella JP. Inhaled nitric oxide in the term newborn. Early Hum Dev. 2008;84:709–16.
Konduri GG, Kim UO. Advances in the diagnosis and management of persistent pulmonary hypertension of the newborn. Pediatr Clin North Am. 2009;56:579–600.
Lakshminrusimha S, Konduri GG, Steinhorn RH. Considerations in the management of hypoxemic respiratory failure and persistent pulmonary hypertension in term and late preterm neonates. J Perinatol. 2016;36(Suppl 2):S12–9.
Mahmood B, Newton D, Pallotto EK. Current trends in neonatal ECMO. Semin Perinatol. 2018;42:80–8.
Viraraghavan VR, Nangia S, Prathik BH, Madarkar BS, Rani D, Saili A. Yield of meconium in non-vigorous neonates undergoing endotracheal suctioning and profile of all neonates born through meconium-stained amniotic fluid: a prospective observational study. Paediatr Int Child Health. 2018;38:266–70.
Acknowledgements
We gratefully acknowledge all site data abstractors of the California Perinatal Quality Care Collaborative (CPQCC). The project described was supported by NIH Grant (HD 072929) and Faculty development fund at UC Davis School of Medicine.
Author information
Authors and Affiliations
Contributions
VKK and SL conceptualized and designed the study, submitted IRB application, drafted and analyzed tables, drafted initial paper, and reviewed and revised the subsequent paper. HCL contributed to study design, critically reviewed and revised the paper for important intellectual content. LS contributed to study design, conducted statistical analysis, and critically reviewed and revised the paper for important intellectual content. AWR critically reviewed the paper and performed statistical analysis. MU critically reviewed and revised the paper for intellectual content. All authors approve the final paper as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kalra, V.K., Lee, H.C., Sie, L. et al. Change in neonatal resuscitation guidelines and trends in incidence of meconium aspiration syndrome in California. J Perinatol 40, 46–55 (2020). https://doi.org/10.1038/s41372-019-0529-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0529-0
- Springer Nature America, Inc.
This article is cited by
-
Characteristics and spending patterns of high-cost child patients: findings from Fujian in China
BMC Public Health (2024)
-
Kindliche Notfälle im Kreißsaal – Teil 1
Die Gynäkologie (2023)
-
Neonatal outcomes of non-vigorous neonates with meconium-stained amniotic fluid before and after change in tracheal suctioning recommendation
Journal of Perinatology (2022)
-
Versorgung und Reanimation des Neugeborenen nach der Geburt
Notfall + Rettungsmedizin (2021)
-
Current Practices and Updates in Neonatal Resuscitation
Current Pediatrics Reports (2020)