Abstract
Objective
Pharmacokinetic (PK) data to guide cefazolin dosing in premature infants are virtually non-existent. Therefore, we aimed to characterize cefazolin PK in infants aged ≤32 weeks of gestation at birth.
Study Design
We conducted a prospective, open-label PK and safety study of cefazolin in infants ≤32 weeks gestation from a University Medical Center. We administered intravenous cefazolin and collected both timed and scavenged blood samples. We analyzed data using non-linear mixed effect modeling and simulated several dosage regimens to achieve target concentrations against methicillin-susceptible Staphylococcus aureus.
Results
We analyzed 40 samples from nine infants and observed that premature infants had lower clearance and greater volume of distribution for cefazolin compared to older children. The median (range) individual Bayesian estimates were 0.03 L/h/kg (0.01–0.08) for clearance and 0.39 L/kg (0.31–0.52) for volume.
Conclusion
Simulations suggested reduced cefazolin dosing based on postmenstrual age achieve target concentrations and potentially reduce unnecessary exposure.
Similar content being viewed by others
Introduction
Suboptimal dosing in premature infants can occur when dosage regimens do not account for physiologic changes affecting drug disposition [1]. Cefazolin is a cephalosporin approved in children >1 month of age to treat indicated susceptible infections [2] at an initial total daily dose of 25–50 mg/kg [2]. Maximum cefazolin effect occurs when free concentrations are greater than minimum inhibitory concentrations (MIC) for 60–70% of the dosing interval [3]. The surrogate pharmacodynamic marker of concentration at 75% of the dosing interval (C75) can predict target attainment [1].
Cefazolin is commonly used off-label in premature infants. While weight and postnatal age (PNA) affect cefazolin pharmacokinetics (PK) [4], data in premature infants are virtually non-existent. In children 0.8–10 years of age, estimates of volume of distribution (Vz) for cefazolin are 0.08–0.263 L/kg and estimates of clearance are 0.048–0.1 L/h/kg [5,6,7]. Cefazolin binds to albumin, with mean (range) protein binding estimates of 49% (17–78) in neonates [8]. Because up to 80% of cefazolin undergoes glomerular filtration and active tubular secretion as intact drug, the reduced renal function in premature infants may substantially increase cefazolin exposure.
Methods
Study design
We conducted a prospective, open-label PK and safety study (NCT00850122) in accordance with the Declaration of Helsinki. Duke University and Universidade Federal de São Paulo/Hospital São Paulo IRBs approved the protocol. We obtained signed informed consent from all participants. We determined sample size based on the ability to observe a serious adverse event.
Population
Between 2013 and 2015, we enrolled infants aged ≤32 weeks at birth, >48 h of age, and <121 days of age who (1) had a suspected systemic infection, (2) were receiving cefazolin for prophylaxis, or (3) were receiving cefazolin to treat a systemic infection. We excluded infants with a history of β-lactam anaphylaxis, cefazolin exposure ≤1 month from enrollment, or serum creatinine >1.7 mg/dL.
Dosing and sample collection
We administered cefazolin via intravenous (IV) infusion over 30 min to infants with PNA ≤28 days (25 mg/kg Q12h) and >28 days (25 mg/kg Q8h) [6,7,8]. We collected up to four scavenged blood samples throughout the dosing interval supplemented with up to six timed (non-scavenged) blood samples (200 μL each) as follows: Q8h dosing: 0.5–1, 1–3, 6–8 h after the first and fourth, fifth, or sixth dose; Q12h dosing: 0.5–1, 1–3, 6–12 h after the first and fourth dose.
Analytics
We quantified cefazolin plasma concentration using high-performance liquid chromatography/mass spectrometry (HPLC-MS/MS). We prepared calibration standards and quality-control samples using drug-free human EDTA plasma, with a linear concentration range from 0.5 to 500 µg/mL and lower limit of quantitation of 0.5 µg/mL.
Population PK analysis
We analyzed data with NONMEM 7 using the first-order conditional estimation method with interaction algorithm. We explored one- and two-compartment structural models and proportional, additive, and proportional-plus-additive residual error models. We included weight as a covariate for structural parameters by estimating or fixing weight on clearance to 0.75, and fixing weight on volume to 1. We assessed model fit using diagnostic plots, parameter precision, and objective function value (OFV).
Model building
We investigated continuous covariates for their influence on PK parameters, including postmenstrual age (PMA), PNA, gestational age (GA), and serum creatinine. We included concomitant gentamicin, ampicillin, and amikacin as categorical covariates. We plotted individual participant deviations from the typical population parameter values (ETAs) against covariates and evaluated those with a graphical relationship for inclusion in the model. We defined the threshold for significance of a single covariate as a reduction of OFV by >3.84 (p < 0.05) and used backward-elimination when >1 covariate was statistically significant.
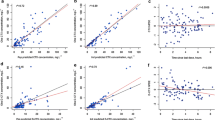
Model evaluation
We performed prediction-corrected visual predictive checks (pcVPCs) for the final model by generating 1000 Monte Carlo simulation replicates/time point. We used the dosing and covariate values from the study population to simulate concentrations, and compared simulated to observed results. To evaluate parameter precision, we generated 95% confidence intervals using nonparametric bootstrapping (1000 replicates).
Dosing simulation
We simulated total and free cefazolin concentrations using the final population PK model, the Empirical Bayesian Estimates (EBEs), and clinical data for each participant. We estimated free concentrations using fraction unbound (fu) 0.34 and 0.68 [8]. For each participant, we simulated several dosage regimens infused over 0.5 h, using a primary target of simulated free steady-state C75 > 1× MIC of cefazolin (4 µg/mL) against methicillin-susceptible Staphylococcus aureus (MSSA) [9]. We also simulated free steady-state C75 > 5× MIC as a surrogate marker for excessive exposure.
Results
Participant characteristics
Clinical characteristics of the infants are described in Table 1, with individual subject data in supplemental Table 1. Altogether, 41 samples were obtained from nine infants; one concentration below the quantifiable limit was excluded. For scavenged samples, the median (range) time from sample collection to freezing was 2.8 (0.7–7.9) h. The median (range) of infant characteristics were: PNA 16 days (3–91); PMA 30.7 weeks (25.7–44.6); weight 1.3 kg (0.7–2.8); albumin 3.0 g/dL (2.6–3.0); and serum creatinine 1.0 mg/dL (0.1–1.4). Using appropriate racial/ethnic growth parameters [10], two infants (22.2%) were small for GA with birth weight less than the tenth percentile for GA based on sex. We obtained 6 (2–6) samples per infant, and the median cefazolin concentration was 59.3 μg/mL (10.1–183). Six infants received Q12h dosing, and three infants received Q8h dosing. All infants received treatment with concomitant antimicrobials, most commonly ampicillin (5/9), gentamicin (4/9), and amikacin (3/9).
PK model development
A summary of PK model building is outlined in Table 2. A one-compartment model provided the best fit based on the goodness of fit and pcVPC plots, although the model over-predicted at concentrations >80 μg/mL. Univariable addition of PMA, PNA, GA, or creatinine to the clearance model did not result in a significant decrease in OFV (i.e. OFV reduction <3.84). However, PMA < 34 weeks, PMA < 37 weeks, PNA < 17 days, and PNA < 25 days as categorical covariates on clearance significantly reduced OFV. Of these, PMA < 37 weeks on clearance had optimal performance based on visual inspection of the clearance vs. PMA relationship and the reduction in OFV (−4.2). Although PNA < 17 days had greater reduction in the OFV (−4.3), we implemented the PMA cutoff of <37 weeks on clearance because (1) cefazolin is cleared predominantly through the kidneys and (2) nephrogenesis finishes before 37 weeks [11]. We did not observe a relationship between volume and PMA, PNA, or GA. Addition of amikacin or ampicillin as a covariate on clearance resulted in a significant drop in OFV (4.5 and 4.3, respectively, p < 0.05) but was not included due to confounding, whereby subjects with high creatinine received concomitant ampicillin while subjects with normal creatinine received amikacin. Further, addition of concomitant medications did not reduce the OFV once PMA was included as a covariate on clearance.
The final model revealed that 96% of bootstrap datasets converged to >2 significant digits. The median of bootstrap fixed effects parameter estimates were within 17% of population estimates from the original dataset for all parameters. The pcVPC revealed 10% (4/40) of observed concentrations were slightly outside the 90% prediction interval. The median (range) individual EBEs were 0.03 L/h/kg (0.01–0.08) for clearance and 0.39 L/kg (0.31–0.52) for volume. The relative standard error was 44% for clearance and 9% for volume. Other PK parameter estimates are outlined in Table 3.
Dosing simulation
Simulations predicted that target attainment was sensitive to protein binding for some dosage regimens for each of the nine subjects (Table 4). The regimen used in the clinical study (25 mg/kg Q12h for PNA ≤ 28 days, 25 mg/kg Q8h > 28 days) resulted in 100% attainment of > 1× MIC with wide ranges of protein binding, but with 56–78% of subjects having free C75 > 5× MIC. Conversely, regimen 5 also resulted in 100% attainment of >1× MIC, but with fewer subjects (11–22%) having exposure > 5× MIC.
Discussion
We developed a one-compartment PK model to characterize cefazolin disposition in infants ≤ 32 weeks of gestation. Despite a small cohort, our model had good performance based on pcVPCs and parameter precision, with only a slight tendency for over-prediction. We found that PMA (categorical) was a significant covariate for cefazolin clearance. However, unlike other reports [4], PMA (continuous) was not significant, probably due to low sample size and limited age distribution. Because cefazolin is renally filtered and actively secreted, the association between PMA and clearance may reflect renal maturation [11]. The median EBE clearance estimate in our study was 0.03 L/h/kg (range 0.01–0.08), approximately one-half that reported for a 9-day-old infant weighing 2720 g (0.068 L/kg/h) [4]. Lower clearance estimates may be due to differences in study populations; the median GA in our study was 29.1 weeks, compared with 37 weeks elsewhere [4]. As expected from immature renal function, the cefazolin clearance for premature infants in our study was significantly lower than clearance reported in older children (0.048-0.1 L/h/kg) [5,6,7]. Furthermore, the cefazolin EBE volume (0.39 L/kg) was higher than that reported in older children (0.08–0.263 L/kg) [5,6,7], likely because premature infants have a higher percentage of total body water.
Using the dosage regimen administered during this study, 100% of infants would obtain free C75 > 1× MIC; further, more than half would have exposure > 5× MIC for MSSA regardless of estimated unbound fraction. Simulations predict that a reduced dosage regimen (6 mg/kg IV Q12h for PMA < 37 weeks, 25 mg/kg IV Q8h for PMA ≥ 37 weeks and <120 days) would also result in 100% attainment >1× MIC; however, target attainment may be lower if deep tissue infections are targeted. Notably, this dosing is lower than other published simulations [4], likely from modeling differences (e.g., using unbound drug concentrations), simulation endpoint, and the degree of prematurity/critical illness of the underlying population. Although estimating free concentration using binding percentages has limitations [4], we simulated free concentrations using a wide range of published binding estimates to determine dosing implications across the binding spectrum.
Infants in the study received cefazolin for a variety of clinical indications, including prophylaxis or treatment for a systemic infection. Therefore, it is possible that infants receiving cefazolin for treatment a systemic infection had more physiologic alterations that could impact PK. Despite this potential limitation, all nine infants were critically ill with a median (range) of 7 (4–12) comorbid medical conditions.
There are some limitations of our study. Notably, our sample size was small and therefore our power to detect covariates was limited. In addition, the infants in our study had a limited distribution of GAs and were recruited from a Hispanic/Latino population. As a result, our proposed dosing regimen should be prospectively tested in a larger population before widespread clinical use.
In conclusion, premature infants exhibited a lower clearance and greater volume of distribution for cefazolin compared with older children. Dosage regimen simulations suggested reduced doses of cefazolin based on PMA may achieve target concentrations in neonates, and potentially reduce unnecessary drug exposure.
References
Cohen-Wolkowiez M, Watt KM, Zhou C, Bloom BT, Poindexter B, Castro L, et al. Developmental pharmacokinetics of piperacillin and tazobactam using plasma and dried blood spots from infants. Antimicrob Agents Chemother. 2014;58:2856–65.
Product Information. Cefazolin Injection. Sagent Pharmaceuticals. Schaumburg, IL. 2017.
Drusano GL. Prevention of resistance: a goal for dose selection for antimicrobial agents. Clin Infect Dis. 2003;36(Suppl 1):S42–S50.
De Cock RFW, Smits A, Allegaert K, de Hoon J, Saegeman V, Danhof M, et al. Population pharmacokinetic modelling of total and unbound cefazolin plasma concentrations as a guide for dosing in preterm and term neonates. J Antimicrob Chemoth. 2014;69:1330–8.
Schmitz ML, Blumer JL, Cetnarowski W, Rubino CM. Determination of appropriate weight-based cutoffs for empiric cefazolin dosing using data from a phase 1 pharmacokinetics and safety study of cefazolin administered for surgical prophylaxis in pediatric patients aged 10 to 12 years. Antimicrob Agents Chemother. 2015;59:4173–80.
Koshida R, Nakashima E, Ichimura F, Nakano O, Watanabe R, Taniguchi N, et al. Comparative distribution kinetics of cefazolin and tobramycin in children. J Pharmacobiodyn. 1987;10:436–42.
Nahata MC, Durrell DE, Ginn-Pease ME, King DR. Pharmacokinetics and tissue concentrations of cefazolin in pediatric patients undergoing gastrointestinal surgery. Eur J Drug Metab Pharmacokinet. 1991;16:49–52.
Deguchi Y, Koshida R, Nakashima E, Watanabe R, Taniguchi N, Ichimura F, et al. Interindividual changes in volume of distribution of cefazolin in newborn infants and its prediction based on physiological pharmacokinetic concepts. J Pharm Sci. 1988;77:674–8.
Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing. 27th ed. CLSI supplement M100. Wayne, PA: Clinical and Laboratory Standards Institute; 2017. Accessed 28 December 2017.
Pedreira C, Pinto F, Pereira S, Costa E. Birth weight patterns by gestational age in Brazil. An Acad Bras Cienc. 2011;83:619–25.
Sulemanji M, Vakili K. Neonatal renal physiology. Semin Pediatr Surg. 2013;22:195–8.
Acknowledgements
This work was supported by NIH-1K23HD060040-04 (NICHD), 2T32GM086330-06 (NIGMS/NICHD), K23 HD091398-01 (NICHD), R35 GM122576 (NIGMS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SJB received salary and/or research support from the National Institutes of Health (2T32GM086330-06, 5R01-HD076676-04, HHSN275201000003I, HHSN275201800003I, 5U24-TR001608-03), the Rheumatology Research Foundation’s Scientist Development Award, and the Thrasher Research Fund. The National Institutes of Health sponsor open access. PBS receives support from industry (www.dcri.duke.edu/research/coi.jsp). HW receives salary support for research from the National Institutes of Health Clinical and Translational Science Award (5UL1TR001117-05). KLRB receives funding from NIGMS, R35 GM122576. KOZ receives support for research from the National Institute for Child Health and Human Development (NICHD) (HHSN275201000003I and K23HD091398) and the Duke Clinical and Translational Science Awards (KL2TR001115). NDR-C received funding from training grant T32 from the National Institute of Child Health and Human Development (T32GM086330-06). DKBJr receives support from the National Institutes of Health (award 2K24HD058735-10, National Institute of Child Health and Human Development (HHSN275201000003I), National Institute of Allergy and Infectious Diseases (HHSN272201500006I), ECHO Program (1U2COD023375-02), and the National Center for Advancing Translational Sciences (1U24TR001608-03); he also receives research support from Cempra Pharmaceuticals (subaward to HHSO100201300009C) and industry for neonatal and pediatric drug development (www.dcri.duke.edu/research/coi.jsp). MC-W receives support for research from the NIH (5R01-HD076676, HHSN275201000003I), NIAID/NIH (HHSN272201500006I), FDA (1U18-FD006298), the Biomedical Advanced Research and Development Authority (HHSO1201300009C), and from the industry for the drug development in adults and children (www.dcri.duke.edu/research/coi.jsp). The remaining author declare that he has no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Balevic, S.J., Smith, P.B., Testoni, D. et al. Cefazolin pharmacokinetics in premature infants. J Perinatol 39, 1213–1218 (2019). https://doi.org/10.1038/s41372-019-0368-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0368-z
- Springer Nature America, Inc.