Abstract
Objective
Pulmonary hypertension (PH) is associated with bronchopulmonary dysplasia (BPD). Screening strategies, a thorough investigation of co-morbidities, and multidisciplinary involvement prior to anti-PH medications have been advocated by recent guidelines. We sought to evaluate current practices of neonatologists caring for premature infants with PH.
Design
Electronic survey of American Academy of Pediatrics neonatology members.
Results
Among 306 neonatologist respondents, 38% had an institutional screening protocol for patients with BPD; 83% screened at 36 weeks for premature neonates on oxygen/mechanical ventilation. In those practicing more than 5 years, 54% noted increasing numbers of premature infants diagnosed with PH. Evaluation for PH in BPD patients included evaluations for micro-aspiration (41%), airways anomalies (29%), and catheterization (10%). Some degree of acquired pulmonary vein stenosis was encountered in 47%. A majority (90%) utilized anti-PH medications during the neonatal hospitalization.
Conclusions
Screening for PH in BPD, and subsequent evaluation and management is highly variable.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
A large number of births occur at less than 28 weeks of estimated gestational age (GA) in the US every year (>55,000 per year) [1]. Although numerous strategies have been implemented to limit the pulmonary complications of this fragile population, bronchopulmonary dysplasia (BPD) remains a significant burden with a diagnosis in up to 68% of extremely premature infants [2]. The association between pulmonary parenchymal disease and pulmonary vascular disease is well described [2,3,4,5,6,7,8,9,10]. Recognized risk factors for BPD include extreme prematurity, severity of pulmonary disease, duration of mechanical ventilation and oxygen exposure, growth restriction, necrotizing enterocolitis, and maternal hypertensive disorders [2, 7, 10, 11]. One of the most devastating sequelae of BPD is pulmonary hypertension. The incidence of PH associated with BPD remains poorly defined but is in the range of 25% [10, 12], and the approach to screening, diagnosing and managing BPD-associated PH varies widely.
Recent (2015) guidelines endorsed by the American Heart Association (AHA) and the American Thoracic Society (ATS) have advocated echocardiography (ECHO) based screening for pulmonary hypertension (PH) in premature newborns with established moderate to severe BPD [11]. Some have argued, and instituted, even more aggressive screening as there are numerous reports of PH affecting premature newborns with, at most, mild BPD, and increasing awareness of pulmonary vein stenosis in this population suggests a potential multi-factorial etiology [10, 13,14,15,16,17,18,19].
When PH is diagnosed, the guidelines recommend evaluation and management of underlying pulmonary disease, hypoxemia, aspiration, and structural airway disease before initiation of systemic anti-PH therapy. Cardiac catheterization to assess disease severity and contributing factors has also been recommended when considering therapy in this population. The purpose of this study was to solicit and report the national, current practice of neonatologists (i.e. a “state of the union”) with respect to the evaluation and treatment of BPD-associated PH a few years after the publication of the AHA/ATS guidelines.
Material and methods
Recruitment and distribution
The survey was developed after review of the literature and consisted of 29 questions (Supplementary material). It was designed by three neonatologists and one cardiologist (specialist in PH) at our institution for content. The study was approved by the institutional review board of Stanford University and by the American Academy of Pediatrics (AAP) section on neonatal-perinatal medicine (SoNPM) for electronic distribution by email. Target respondents were neonatologists practicing in a tertiary care nursery with babies born ≤28 weeks of estimated GA. A cover letter outlining the objectives of the survey and estimated time for completion was provided to the participant. All respondents were required to consent to participation in the survey and confirm that they were practicing neonatologists caring for the target population. A reminder for survey participation was sent by the SoNPM 2 weeks after the initial invite and responses were collected for a total of 4 weeks. Study data were collected and managed using Research electronic data capture (REDCap) tools hosted at the Stanford Center for Clinical Informatics [20]. REDCap is a secure, web-based application designed to support data capture for research studies.
The survey consisted of the following sections: the participant demographics, the general approach to BPD diagnosis and management, the PH screening, evaluation and management, as well as the avenues for future research. The term “bronchopulmonary dysplasia” was used for “chronic lung disease” or “chronic neonatal lung disease.” Participants were queried on their definition of BPD with choices including the National Institute of Child Health and Human development (NICHD) Workshop definition [21] and/or the physiologic definition based on the oxygen reduction test [22]. Participants were also queried on the use of the “6 to 12 h pulse oximetry monitoring during all levels of activity” criteria for the use of home oxygen therapy in the context of BPD [23].
Data analysis
Results are described as mean with standard deviation or median with interquartile range for continuous variables and counts with proportions for categorical variables. We compared answers provided by neonatologists working in a university-based environment, vs. those working in a public or private non-university based unit. The Fisher’s exact and chi-square tests were used to compare categorical characteristics. Student's t test and Wilcoxon–Mann–Whitney test were used to compare continuous variables for parametric and non-parametric variables, respectively. Statistical analyses were completed with Stata SE (Version 14.2, College Station, Texas). The level of significance was set at 0.05 for all comparisons.
Results
Demographic characteristics
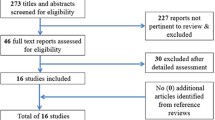
SoNPM confirmed 3000 professionals on the mailing list of the section, including 100 neonatal nurse practitioners and 350 fellows, which resulted in an estimated 2550 neonatologists in the SoNPM email list. A total of 306 surveys were analyzed and only 1 additional survey excluded because the responder was not caring for babies less than 28 weeks of estimated GA at birth. This resulted in a response rate of 12%, in line with a reported usual survey response rate of 10 to 15% by SoNPM [24].
Demographic characteristics of respondents are shown in Table 1. A majority were confronted with various pathologies in their practice, which included: prematurity, hypoxic ischemic encephalopathy, and cardiac and surgical conditions. Most had more than 20 years of experience, were working in a NICU with more than 30 beds and were in a university based setting. A very small proportion of respondents had another subspecialty, with only 1.4 % being trained in PH.
Bronchopulmonary dysplasia
A majority of neonatologists reported utilizing the NICHD definition of BPD, with one-third using a combination of the NICHD and the oxygen reduction test (Table 2). Home oxygen therapy for BPD was mostly based on neonatologist’s advice and on oxygen targets. Only half of the respondents answered that they consistently performed a prolonged pulse oximetry study for patients with established moderate to severe BPD to determine the need for home oxygen therapy (49% always, 13% sometimes, 33 % never and 4% who did not know). For a majority of clinicians, minimum saturation targets at 36 weeks post-menstrual age (PMA) were 90–92%.
Pulmonary hypertension
Among those with more than 5 years of practice, 54% noted an increasing number of extremely premature infants diagnosed with PH. Only 10% of respondents had a universal (i.e. ±BPD) institutional protocol for babies born at <28 weeks of estimated GA to screen for PH by ECHO when they were close to 36 weeks of PMA (or before discharge). Thirty-eight percent had a formal protocol for those with BPD of any severity level and 46% for those with moderate to severe BPD. However, in their personal practice, 83% of respondents indicated they would screen an extremely preterm infant requiring oxygen and/or mechanical ventilation by ECHO at 36 weeks PMA, while 11% did not routinely screen for PH, and 11% screened all extreme preterm patients in their practice. Acquired PV stenosis had been encountered by 45% of respondents in association with BPD.
When investigating comorbidities related to PH and BPD, and establishing etiology for PH, most would involve cardiology (83%) and pulmonology (53%), order a blood gas (71%) and a chest X-ray (81%), and ensure follow-up with an ECHO (89%) (Table 3), while only a minority would initially evaluate for microaspiration (41%) and airway obstruction (21%) or would order a formal cardiac catheterization study (11%). In most institutions, follow-up of these patients occurred with separate outpatient visits with cardiology, pulmonology, and high-risk infant follow-up clinics. Only 30% reported having a PH clinic and program at their institution.
Once PH diagnosed, home oxygen therapy was an absolute indication for BPD patients in 65% of respondents, though only 37% would order a prolonged oximetry study (regardless of the degree of BPD). Management of PH in BPD patients, during the neonatal hospitalization, included use of systemic PH medications (e.g., phosphodiesterase 5 inhibitors, endothelin antagonists, and/or prostacyclines) by 90.3% of respondents. Before starting such medications 33% never obtain a cardiac catheterization, 36% do so rarely, 23% sometimes, 7% often, and 1% always. Of the respondents who reported encountering PV stenosis and using PH therapies, a majority started medication without a cardiac catheterization (sometimes = 33%; rarely = 38%, never = 17%).
Future research
A majority of neonatologists would be supportive of participating in studies that randomize neonatal patients with PH at 36 week PMA to different therapeutic regimens (yes 75.5%, no 4.8%, unsure 19.7%). When looking at different categories of patients, most would be amenable to randomizing patients still requiring invasive mechanical ventilation (74%) and showing signs of suprasystemic PH on ECHO (81%) or isosystemic PH on ECHO (56%) to therapeutic interventions. Patients requiring only oxygen (45%) or with less than systemic-level PH (37%) were considered less urgent patient populations for investigation.
University practice
Respondents who were practicing within an academic setting (67% of all respondents) were compared to those practicing in a non-academic (private and public) neonatal unit (Table 4). University-based neonatologists practiced in larger units and were more inclined to have noted an increased number of cases of PH and BPD, and acquired PV stenosis in the past 5 years. University centers had more protocols to screen premature infants for PH at 36 weeks PMA. Although most neonatologists had used systemic anti-PH medications, a higher proportion of those practicing in a university setting utilized them in the NICU.
Discussion
We sought to determine the current practices related to prematurity and BPD with or without PH amongst neonatologists subsequent to the 2015 publication of PH guidelines by the AHA and ATS. While these guidelines recommend screening for PH by ECHO in patients with established BPD, only 46% of respondents declared that a formal screening protocol was in place at their institution targeting this population; practice in an academic center was associated with a higher proportion of formal screening. Nonetheless, 83% of all respondents indicated that they would obtain an ECHO at 36 weeks PMA in their own clinical practice, for premature infants with moderate to severe BPD. The published guidelines recommend the evaluation of airway obstruction and reflux when facing PH in a BPD infant, as airway co-morbidities such as subglottic stenosis, vocal cord movement anomalies, laryngomalacia and tracheo-bronchomalacia can lead to obstructive airway disease and CO2 retention [25], yet only 29% of respondents mentioned ordering such evaluation for airway obstruction. Finally, although a majority mentioned that they have prescribed an anti-PH medication, only a minority followed the 2015 guidelines recommending evaluation of these patients by cardiac catheterization (7% often, 1% always).
BPD definition and pulmonary hypertension
Understanding of ante-natal and post-natal contributors to pulmonary vascular and parenchymal disease of the premature infant has evolved since 2001, when clinical definition of BPD was established by the NICHD. Since then, studies on oxygen targets and approach to ventilation may have altered the practice in many centers [26,27,28]. Despite attempts to standardize the definition of BPD, wide variation among centers has been reported with the diagnosis of BPD ranging from 6 to 57% depending on the definition chosen [29]. Hence, it is not surprising to find such heterogeneity in the criteria used for diagnosis of BPD amongst neonatologists in our survey. With the increasing recognition that PH is a strong contributor to mortality and morbidities in the context of BPD, an updated unified definition should consider including oxygen saturation targets, degree of respiratory support and PH.
There are increasing reports of premature newborns with pulmonary vascular disease and relatively benign respiratory phenotype [10, 13]. These patients would fall out from the current recommendations for screening. About 10% of respondents mentioned that their institutional protocol was screening all premature infants born at <28 weeks of GA, regardless of their BPD status. The question remains about the cost-effectiveness and test characteristics of extending screening practices and the significance of PH in this category of patients. Indeed, lack of natural history data and of consensus for grading severity of PH remains a challenge. Premature infants with no or mild BPD may benefit from screening with a relatively inexpensive and non-invasive test. Furthermore, refinement of criteria for screening may include recognized risk factors for PH in this population other than respiratory phenotype, such as small for GA status or history of necrotizing enterocolitis.
Home oxygen therapy
While guidelines and expert recommendations have advocated for prolonged monitoring of oxygen while awake, asleep, and feeding, only a minority of the respondents have been using this as a criterion for initiation of home oxygen therapy [13, 23]. Repeated intermittent episodes of hypoxemia have been reported to be associated with PH, with some data indicating that adults are susceptible to development of PH at saturations of 88 to 92% [23]. Recent AHA/ATS guidelines have recommended the use of supplemental oxygen to maintain saturations between 92 and 95 % in the context of PH. In our survey, most neonatologists had a lower target of saturation of 90 to 92% in the context of BPD and only 65% considered PH to be an absolute indication for home oxygen therapy.
Therapeutic approaches to PH for BPD patients
Factors contributing to PH in premature infants are numerous and include ventilation/perfusion mismatch, abnormal vascular growth and muscularization, disturbed response to endogenous and exogenous dilators and constrictors, abnormal venous vasculature with possible stenosis leading to postcapillary obstruction, concomitant left ventricular hypertrophy with potential for increased end-diastolic pressure, as well as chronic aspiration, reflux, airway obstruction, inflammation, and altered nutrition [7, 30, 31]. Limited data exists pertaining to the medical management of PH in BPD patients [13]. Effects of pulmonary vasodilator therapy in the population of BPD-PH remains unclear in light of the heterogeneous pulmonary vascular disease in this population. In the recent years, acquired PV stenosis has been reported increasingly in association with prematurity and BPD [14,15,16,17,18,19]. While this entity has been reported in case series, a surprisingly high number of neonatologists have described encountering it in their clinical practice (45 %). Most respondents encountering PV stenosis reported having used anti-PH medications, with a majority not formerly assessing these patients by cardiac catheterization. Pulmonary vasodilators in the context of post-capillary obstruction may lead to a heterogenous pulmonary vascular congestion, altered pulmonary mechanics and disturbed gas exchange. These medications may also theoretically promote redistribution of pulmonary vascular flow towards the unaffected area and, as such, could hypothetically provide some benefit. Patients with BPD and PH may have a component of reversible pulmonary vascular constriction with response upon vasoreactivity testing during cardiac catheterization. [32]. However, the component of decreased vascular surface area and/or post-capillary PH will not be reversed by these treatments and may even cause harm. Future studies should investigate the optimal approach for diagnosis and management of PH in the BPD population. No randomized control trials have been done to evaluate the safety and efficacy of these medications in the BPD patient. However, there is a great sense of urgency to better study these medications amongst neonatologists.
Cardiac catheterization
AHA/ATS guidelines have advocated for cardiac catheterization prior to initiation of anti-PH medication. Few respondents of our survey were following this recommendation. This is not surprising considering concern for exacerbation of pulmonary disease or for PH crisis in the context of re-intubation and/or sedation. Patients already intubated at PH diagnosis are also at high risk for perioperative complications [33]. As such, these patients may not tolerate transport within the institution or to another hospital with expertize in cardiac catheterization in the PH population (as recommended by AHA/ATS [11]). Some clinicians may therefore prefer to defer these evaluations and opt for empiric therapy in the hope to improve clinical status. Beyond the catheterization, recovery in the days following the procedure is of concern, especially in patients who had prior difficulty with extubation, prolonged respiratory support, and poor respiratory reserve. PH has been recognized in both adults and children as a risk factor for cardiac arrest (2.5 to 5.7%) and death (1.4%) from cardiac catheterization [34]. Pediatric patients with suprasystemic PH seem to be the most at risk for cardiac arrest and PH crisis (up to 6% reported) [35, 36]. A recent PPHNet review, published after this survey, is consistent with our findings of current clinical practice, suggesting that catheterization should be “considered” prior to initiation of medications, but may be delayed by the treating team based on the possible risks of the procedure [32].
Conclusions
Multiple studies have reported an association between BPD and pulmonary hypertension. Recent guidelines have advocated for screening by ECHO of patients with BPD at 36 weeks of PMA and most clinicians have adopted this recommendation in their practice. Limited data exist about the incidence, natural history and optimal management of BPD-PH patients. Hence, in our survey, the evaluation, the treatment, and the follow-up of these patients was highly variable across centers in the US. Guidelines have advocated for cardiac catheterization prior to the initiation of anti-PH therapies, but only a minority of neonatologists have adopted this practice. Most clinicians have used anti-PH medications, but a majority are in agreement that there is an urgency to better study the efficacy of these therapies in the BPD-PH population.
References
Osterman MJ, Kochanek KD, MacDorman MF, Strobino DM, Guyer B. Annual summary of vital statistics: 2012–2013. Pediatrics. 2015;135:1115–25.
Mourani PM, Sontag MK, Younoszai A, Miller JI, Kinsella JP, Baker CD, et al. Early pulmonary vascular disease in preterm infants at risk for bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2015;191:87–95.
Subhedar N, Shaw N. Changes in pulmonary arterial pressure in preterm infants with chronic lung disease. Arch Dis Child Fetal Neonatal Ed. 2000;82:F243–F247.
Mourani PM, Abman SH. Pulmonary vascular disease in bronchopulmonary dysplasia: pulmonary hypertension and beyond. Curr Opin Pediatr. 2013;25:329–37.
Khemani E, McElhinney DB, Rhein L, Andrade O, Lacro RV, Thomas KC, et al. Pulmonary artery hypertension in formerly premature infants with bronchopulmonary dysplasia: clinical features and outcomes in the surfactant era. Pediatrics. 2007;120: 1260–9.
Mourani PM, Sontag MK, Younoszai A, Ivy DD, Abman SH. Clinical utility of echocardiography for the diagnosis and management of pulmonary vascular disease in young children with chronic lung disease. Pediatrics. 2008;121:317–25.
Altit G, Dancea A, Renaud C, Perreault T, Lands LC, Sant’Anna G. Pathophysiology, screening and diagnosis of pulmonary hypertension in infants with bronchopulmonary dysplasia-a review of the literature. Paediatr Respir Rev. 2016;23:16–26.
Wright T, Filbrun A, Bryner B, Mychaliska G. Predictors of early lung function in patients with congenital diaphragmatic hernia. J Pediatr Surg. 2014;49:882–5.
Bhat R, Salas AA, Foster C, Carlo WA, Ambalavanan N. Prospective analysis of pulmonary hypertension in extremely low birth weight infants. Pediatrics. 2012;129:e682–e689.
Weismann CG, Montgomery AM, Asnes JD, Bazzy-Asaad A, Tolomeo C, Ehrenkranz RA, et al. Prospective Echocardiographic and Biochemical Screening for Pulmonary Hypertension in Infants with Bronchopulmonary Dysplasia. Paper presented at: UCSF 9th International Conference Neonatal & Childhood Pulmonary Vascular Disease 2016 2016.
Abman SH, Hansmann G, Archer SL, Ivy DD, Adatia I, Chung WK, et al. Pediatric pulmonary hypertension guidelines from the american heart association and american thoracic society. Circulation. 2015;132:2037–99.
An HS, Bae EJ, Kim GB, Kwon BS, Beak JS, Kim EK, et al. Pulmonary hypertension in preterm infants with bronchopulmonary dysplasia. Korean Circ J. 2010;40:131–6.
Abman SH. Pulmonary Hypertension in Bronchopulmonary Dysplasia. Respiratory Outcomes in Preterm Infants. Springer, 2017, pp 197-213. DOI https://doi.org/10.1007/978-3-319-48835-6_12. Online ISBN 978-3-319-48835-6.
Latson LA, Prieto LR. Congenital and acquired pulmonary vein stenosis. Circulation. 2007;115:103–8.
Amin R, Kwon S, Moayedi Y, Sweezey N, Pulmonary vein stenosis: case report and literature review. Can Respir J. 2009;16:e77–e80.
Edwards J. Congenital stenosis of pulmonary veins. Pathologic and developmental considerations. Lab Invest. 1959;9:46–66.
Laux D, Rocchisani MA, Boudjemline Y, Gouton M, Bonnet D, Ovaert C. Pulmonary hypertension in the preterm infant with chronic lung disease can be caused by pulmonary vein stenosis: a must-know entity. Pediatr Cardiol. 2016;37:313–21.
Swier NL, Richards B, Cua CL, Lynch SK, Yin H, Nelin LD, et al. Pulmonary vein stenosis in neonates with severe bronchopulmonary dysplasia. Am J Perinatol. 2016;33:671–7.
Mahgoub L, Kaddoura T, Kameny AR, Lopez Ortego P, Vanderlaan RD, Kakadekar A, et al. Pulmonary vein stenosis of ex‐premature infants with pulmonary hypertension and bronchopulmonary dysplasia, epidemiology, and survival from a multicenter cohort. Pediatr Pulmonol. 2017;52:1063–70.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Walsh MC, Wilson-Costello D, Zadell A, Newman N, Fanaroff A. Safety, reliability, and validity of a physiologic definition of bronchopulmonary dysplasia. J Perinatol. 2003;23:451–6.
Balfour-Lynn I, Field D, Gringras P, Hicks B, Jardine E, Jones R, et al. BTS guidelines for home oxygen in children. Thorax. 2009;64:ii1–ii26.
Feltman D, Du H, Leuthner S. Survey of neonatologists’ attitudes toward limiting life-sustaining treatments in the neonatal intensive care unit. J Perinatol. 2012;32:886–92.
Amin RS, Rutter MJ. Airway disease and management in bronchopulmonary dysplasia. Clin Perinatol. 2015;42:857–70.
SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network, Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. 2010;2010:1970–9..
Schmidt B, Whyte RK, Asztalos EV, Moddemann D, Poets C, Rabi Y, et al. Effects of targeting higher vs lower arterial oxygen saturations on death or disability in extremely preterm infants: a randomized clinical trial. Jama. 2013;309:2111–20.
Subramaniam P, Ho JJ, Davis PG Prophylactic nasal continuous positive airway pressure for preventing morbidity and mortality in very preterm infants. Cochrane Database Syst Rev. 2016;CD001243.
Hines D, Modi N, Lee SK, Isayama T, Sjors G, Gagliardi L, et al. Scoping review shows wide variation in the definitions of bronchopulmonary dysplasia in preterm infants and calls for a consensus. Acta Paediatr. 2017;106:366–74.
Stenmark KR, Abman SH. Lung vascular development: implications for the pathogenesis of bronchopulmonary dysplasia. Annu Rev Physiol. 2005;67:623–61.
Mourani PM, Abman SH. Pulmonary hypertension and vascular abnormalities in bronchopulmonary dysplasia. Clin Perinatol. 2015;42:839–55.
Krishnan U, Feinstein JA, Adatia I, Austin ED, Mullen MP, Hopper RK, et al. Evaluation and management of pulmonary hypertension in children with bronchopulmonary dysplasia. J Pediatr. 2017;188:24–34.e1.
Lauer R, Vadi M, Mason L. Anaesthetic management of the child with co-existing pulmonary disease. Br J Anaesth. 2012;109:i47–i59.
Friesen RH, Williams GD. Anesthetic management of children with pulmonary arterial hypertension. Paediatr Anaesth. 2008;18:208–16.
Carmosino MJ, Friesen RH, Doran A, Ivy DD. Perioperative complications in children with pulmonary hypertension undergoing noncardiac surgery or cardiac catheterization. Anesth Analg. 2007;104:521–7.
Taylor C, Derrick G, McEwan A, Haworth S, Sury M. Risk of cardiac catheterization under anaesthesia in children with pulmonary hypertension. Br J Anaesth. 2007;98:657–61.
Author information
Authors and Affiliations
Contributions
GA is the author that wrote the first draft.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Altit, G., Lee, H.C., Hintz, S. et al. Practices surrounding pulmonary hypertension and bronchopulmonary dysplasia amongst neonatologists caring for premature infants. J Perinatol 38, 361–367 (2018). https://doi.org/10.1038/s41372-017-0025-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-017-0025-3
- Springer Nature America, Inc.
This article is cited by
-
Role of functional echocardiographic parameters in the diagnosis of bronchopulmonary dysplasia-associated pulmonary hypertension
Journal of Perinatology (2022)
-
Screening Echocardiography Identifies Risk Factors for Pulmonary Hypertension at Discharge in Premature Infants with Bronchopulmonary Dysplasia
Pediatric Cardiology (2022)
-
Utility of echocardiography in predicting mortality in infants with severe bronchopulmonary dysplasia
Journal of Perinatology (2020)
-
Factors influencing decision making in neonatology: inhaled nitric oxide in preterm infants
Journal of Perinatology (2019)
-
Agreement of an echocardiogram-based diagnosis of pulmonary hypertension in infants at risk for bronchopulmonary dysplasia among masked reviewers
Journal of Perinatology (2019)