Abstract
Increased blood pressure (BP) variability (BPV) is associated with high cardiovascular risk in hemodialysis. Patients with intradialytic hypertension (IDH) also exhibit an increased cardiovascular risk compared to hemodialysis patients without this condition. The impact of non-pharmacological BP-lowering interventions on BPV in this population remains unknown. This analysis evaluated the effect of low (137mEq/L) compared to standard (140mEq/L) dialysate sodium concentration on short-term BPV in patients with IDH. In a randomized cross-over manner, 29 IDH patients underwent 4 hemodialysis sessions with low (137mEq/L) followed by 4 sessions with standard (140mEq/L) dialysate sodium or vice versa. 48 h ambulatory BP measurement was performed from the start of the 4th session on each dialysate sodium. BPV indices during the 48 h, 24 h, day-time and night-time periods were calculated. Mean 48 h BP was 5.3/2.6 mmHg lower with low compared to standard dialysate sodium concentration, (p = 0.005/p = 0.007 respectively). All 48 h systolic BPV indices examined showed non-significant differences between low and standard dialysate sodium (SBP-SD: 16.99 ± 5.39 vs. 16.98 ± 4.33 mmHg, p = 0.982; SBP-wSD: 15.93 ± 5.02 vs. 16.12 ± 4.16 mmHg, p = 0.769; SBP-ARV: 11.99 ± 3.67 vs. 11.45 ± 3.35 mmHg, p = 0.392; SBP-CV: 12.36 ± 3.65 vs. 11.92 ± 3.18%, p = 0.302, with low vs. standard dialysate sodium, respectively). Diastolic BPV indices were numerically, but not statistically, lower with low dialysate sodium. Overall, significant differences were observed in some comparisons with a trend for lower BPV during day-time 2 and higher BVP during night-time 2 with low dialysate sodium. In conclusion, low dialysate sodium concentration does not affect BPV levels in patients with IDH. Future research should explore alternative interventions to reduce BP and BPV in this high-risk population.
Similar content being viewed by others
Introduction
Patients with end-stage kidney disease (ESKD) undergoing hemodialysis have an increased risk for cardiovascular events and mortality [1]. Hypertension is considered the most common modifiable cardiovascular risk factor in these individuals, with an estimated prevalence around 85% [2]. The typical trajectory of blood pressure (BP) through the intra- and interdialytic interval is a rapid decrease in BP during hemodialysis, as a response to ultrafiltration, followed by a progressive increase during the interdialytic interval in parallel to sodium and water accumulation [2,3,4]. However, a smaller subset, approximately 10–15% of the dialysis population, experience a deviant response, i.e. a “paradoxical” rise in BP during or immediately after dialysis, a phenomenon known as “intradialytic hypertension” (IDH) [5, 6]. Individuals with IDH exhibit an increased risk for cardiovascular events, cardiovascular and all-cause mortality, compared to patients displaying the usual pattern of BP fall during dialysis [7,8,9].
Blood pressure variability (BPV) refers to BP fluctuations over time and can be distinguished into very short-term (beat-by-beat), short-term (within 24 h), mid-term (day-by-day) and long-term (visit-to-visit) BPV based on the duration of measurement [10, 11]. Very short-term and short-term BPV represent a multifactorial response of neural, vascular, humoral and rheological mechanisms to environmental and behavioral stimuli, whereas mid-term BPV is mostly influenced by behavioral factors and long-term BPV by treatment-related factors and the process of ageing [10, 11]. Ambulatory blood pressure monitoring (ABPM) is used for the assessment of short-term and mid-term BPV, whereas office BP readings over relevant interval are usually used to evaluate long-term BPV.
Several studies assessed BPV in ESKD patients, producing several interesting observations. Patients with ESKD are probably the patient group with the highest BPV [12], which is similar to hemodialysis and peritoneal dialysis patients [13]. Further, in hemodialysis patients BPV appears significantly increased from the 1st to the 2nd day of the interdialytic interval [4], while several lines of evidence convincingly show and that increased intradialytic, short- and long-term BPV is associated with higher risk of cardiovascular events and mortality in this individuals independently of BP levels [14,15,16]. Based on these observations, strategies to reduce BPV could be beneficial to reduce cardiovascular risk in hemodialysis patients.
Studies evaluating BPV in patients with intradialytic hypertension are extremely rare. In a case-control study using ambulatory BP monitoring (ABPM), our group observed sustained higher BP levels during the whole 48 h interval in patients with IDH compared to hemodialysis patients without the phenomenon, whereas no significant differences were observed in short-term BPV [17]. A subsequent work that examined two different pharmacological interventions (nebivolol and irbesartan) in patients with IDH demonstrated a significant reduction in post-dialysis and 24 h BP with both drugs, while nebivolol was also associated with a reduction in BPV [18]. A few studies have previously investigated the effect of low dialysate sodium concentrations on, mainly peridialytic, BP levels in patients with IDH with promising results [19,20,21]. In a randomized crossover study, we recently showed that low dialysate sodium significantly reduced intradialytic, post-dialysis and 48-h BP levels in IDH patients [22]. As of this writing, no study has evaluated the effects of any non-pharmacological intervention on BPV in these individuals. Thus, the aim of this analysis was to examine the effect of low (137 mEq/L) compared to standard (140 mEq/L) dialysate sodium on short-term BPV during a 48-h intra- and interdialytic period in patients with IDH.
Materials and Methods
Study Participants
This is a (pre-specified) secondary analysis of a randomized, single-blind (participants were blinded), crossover study, that enrolled 30 patients from four hemodialysis units, three located in Greece and one in Slovenia, examining, as primary outcome, the effect of low versus standard dialysate sodium concentration on 48 h ambulatory BP in patients with IDH (NCT05430438), as described elsewhere [22]. Inclusion criteria were: (1) adult patients with ESKD on a standard thrice-weekly hemodialysis schedule for > 3 months; (2) IDH, defined as SBP rise ≥ 10 mmHg pre- to post-dialysis for at least 4 out of 6 consecutive hemodialysis sessions; (3) patients at dry weight, as assessed by clinical criteria; (4) informed written consent. Exclusion criteria were: (1) post-dialysis SBP < 130 mmHg in at least 4 out of 6 consecutive hemodialysis treatments during the selection period prior to study enrollment; (2) non-functional arteriovenous fistula in the contralateral brachial arm area of the one used for vascular access that could interfere with proper ABPM recording; (3) contraindications for the intervention of low dialysate sodium (e.g., frequent hypotensive episodes requiring fluid resuscitation); (4) pre-dialysis serum sodium < 130 mEq/L or > 142 mEq/L at recruitment; (5) modification of dry weight or antihypertensive treatment during one month prior to enrollment; (6) hospitalization for any cause during one month prior to enrollment; (7) history of seizures or dialysis disequilibrium syndrome; (8) active malignancy or any comorbidities with poor prognosis. The study protocol was approved by the Ethics Committee of the School of Medicine, Aristotle University of Thessaloniki and all procedures were performed according to the Declaration of Helsinki (2013 Amendment).
Study protocol
Patients were assessed for eligibility based on records of peridialytic BP measurements of a 2-week period to confirm the presence of IDH. Triplicate BP measurements were obtained, while patients were seated on the dialysis chair, with a validated device, i.e. Omron M3, according to European Society of Hypertension recommendations. Demographic and anthropometric characteristics, medical history, medication, co-morbidities, and other dialysis-related parameters were recorded for every participant. Eligible subjects had a baseline evaluation, performed before a mid-week dialysis session; among others, peridialytic and intradialytic BP were assessed with the Mobil-O-Graph device. After baseline assessment, patients were randomly assigned to two groups, which received the two interventions in the opposite order. The first group (group A) received low, i.e. 137 mEq/L, dialysate sodium followed by standard, i.e. 140 mEq/L dialysate sodium concentration and the second (group B) standard dialysate sodium followed by low dialysate sodium concentration. According to the randomization arm, participants underwent 4 hemodialysis sessions, starting from a mid-week session (i.e., Wednesday or Thursday), with low or standard dialysate sodium concentration. A 2-week washout period with standard dialysate sodium of 140 mEq/L followed for both groups, after which participants underwent another set of 4 hemodialysis sessions with the opposite dialysate sodium concentration. Before the start of the 4th session on each dialysate sodium level, patients were assessed with lung ultrasound and the 48 h ABPM started.
In each dialysis session, ultrafiltration volume was determined based on the participants’ prespecified dry weight, defined according to standard clinical criteria. Dry-weight and antihypertensive medication were not allowed to change during the study. Participants were also instructed to continue their usual daily activities, including physical activity, food and water intake, and follow their regular medication over the study period.
Ambulatory BP monitoring
ABPM was performed with the Mobil-O-Graph NG (IEM, Stolberg, Germany), an automated oscillometric monitor previously validated for brachial BP measurement [23]. The recording began before a mid-week dialysis session (i.e. the 4th session of each study period) and lasted for a complete 48 h period. The device was placed on the non-fistula arm with appropriate-size cuffs and recorded BP every 20 min during day-time (7:00 to 22:59) and every 30 min during night-time (23:00 to 6:59). Recordings were included in the analysis if > 80% of the total readings were valid and ≤ 2 non-consecutive day-hours had fewer than 2 valid measurements and ≤ 1 night-hour had no valid reading. In case of invalid recordings, dialysate sodium remained the same and the ABPM was repeated one week later. To minimize the possible effect of manual BP measurements on BPV, only measurements recorded at the time intervals at which the device was programmed to measure BP were used in this analysis.
BP variability parameters
The following BPV parameters of brachial SBP and DBP were calculated based on the ABPM recordings:
-
1.
Standard deviation (SD), calculated as: \({{SD}=\sqrt{\frac{1}{{{{\rm{N}}}}-1}{\sum }_{{{{\rm{k}}}}=1}^{{{{\rm{N}}}}}{{{\boldsymbol{|}}}}{{{{\rm{BP}}}}}_{{{{\rm{k}}}}+1} - \overline{{{{\rm{BP}}}}}}{{{\rm{|}}}};{{{\rm{N}}}}}\), the number of valid BP measurements, \(\overline{{{{\rm{BP}}}}}\), average of ABPM readings.
-
2.
Coefficient of variation (CV), defined as the ratio of the SD to the mean BP and calculated as: \({CV}=\frac{{{{\rm{SD}}}}}{{{{\rm{mean\; BP}}}}}\times 100\).
-
3.
Weighted SD (wSD), defined as the average of daytime and nighttime SD of BP, each weighted for the duration of the day- and nighttime periods, respectively and calculated as: \({wSD}=\frac{\left({{{\rm{daytime}}}\; {{\rm{SD}}}\; \times \; {{\rm{daytime}}}\; {{\rm{hrs}}}}\right)\, + ({{{\rm{nighttime}}}\; {{\rm{SD}}}\; \times \; {{\rm{nighttime}}}\; {{\rm{hrs}}}})}{24{{{\rm{hour}}}}{{{\rm{period}}}}}\)
-
4.
Average real variability (ARV), defined as the average of the absolute differences between consecutive BP measurements and calculated as: \({ARV}=\frac{1}{{{{\rm{N}}}}-1}\,{\sum }_{{{{\rm{k}}}}=1}^{{{{\rm{N}}}}-1}{{{\boldsymbol{|}}}}{{{{\rm{BP}}}}}_{k+1}{{{\boldsymbol{-}}}}\,{{{{\rm{BP}}}}}_{{{{\rm{k}}}}}{{{\boldsymbol{|}}}}\); N, the number of valid BP measurements, BPk, BP at measurement number k.
All BPV parameters were calculated for the 48 h period starting immediately before the beginning of the session and including a complete intra- and interdialytic period (day 1 = 24 h period including dialysis and day 2 = the following 24 hour period). Day-time periods were from 07:00 to 22:59 and night-time periods from 23:00 to 06:59. For patients dialyzing in the 1st shift the start of the 24 h period matched the start of the day-time periods, including consecutive hours, as performed elsewhere [17, 24]. For patients in the 2nd and 3rd dialysis shifts, the day-time periods did not include consecutive time (i.e. for a patient starting dialysis in the 2nd shift at 12:00, the daytime of day 1 for the 48 h period was considered the time between 12:00 and 23:59 followed by the time of the following morning between 07:00 and 11:59). Night-time periods were from 23:00 to 06:59.
The dipping pattern of nocturnal BP was calculated with the following formula: 1− (mean night/mean day) ratio of SBP (%). Patients were divided into three categories: dippers, with a nocturnal SBP fall of > 10% and ≤ 20%; non-dippers, with a fall of ≥0% and ≤ 10%; and reverse dippers, with a nocturnal SBP increase.
Statistical analysis
Statistical analysis was performed with Statistical Package for Social Sciences version 22.0 (SPSS Inc, Chicago, IL, USA). Continuous variables were presented as mean ± SD or median and interquartile range [Q1, Q3] depending on the normality, while categorical variables are expressed as frequencies and percentages (n, %). Shapiro-Wilk test was applied to examine the normality of distribution for continuous variables. Paired Student t-test or Wilcoxon’s signed rank test were used, depending on the normality of distribution, to investigate differences between low versus standard dialysate sodium in BPV parameters. Wilcoxon signed rank test was used to assess the difference between the three different categories of dipping pattern. A p-value < 0.05 (two-tailed) was considered statistically significant in all comparisons.
Results
Baseline characteristics
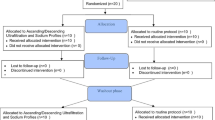
Baseline demographic, clinical, and laboratory characteristics of the study population are presented in Table 1. The flowchart of study participants is illustrated in Supplemental Fig. 1. Thirty participants fulfilled the inclusion/exclusion criteria;14 were randomized to group A and 16 to group B. Among them, 9 participants had to repeat one measurement due to an invalid recording; 3 of them repeated the ABPM during the standard dialysate sodium phase and 5 during the low dialysate sodium phase. One patient randomized to group A with an invalid first 48 h ABPM refused to repeat the recording and withdrew consent. Thus, a total of 29 patients (17 male and 12 female) with mean age of 64.6 ± 17.6 and median hemodialysis vintage 28.7 [8.3, 69.8] months were included in this analysis. Among major co-morbidities, all the participants had hypertension, 41.4% had diabetes mellitus, 37.9% had coronary heart disease and 31% had peripheral vascular disease. The most common antihypertensive drug classes were calcium channel blockers (CCBs) and β-blockers, both administered to 62.1% of the study population. Intradialytic (SBP/DBP: 141.4 ± 18.0/85.0 ± 13.4 mmHg with low vs 147.5 ± 13.6/88.1 ± 12.5 mmHg with standard dialysate sodium, p = 0.034/p = 0.013, respectively), post-dialysis (SBP/DBP: 150.3 ± 22.3/91.2 ± 15.1 mmHg with low vs. 166.6 ± 17.3/94.5 ± 14.9 mmHg with standard dialysate sodium, p < 0.001/p = 0.134 respectively) and 48 h SBP/DBP (137.6 ± 17.0/81.4 ± 13.7 mmHg with low vs. 142.9 ± 14.5/84.0 ± 13.9 mmHg with standard dialysate sodium, p = 0.005/p = 0.007 respectively) were significantly reduced with low compared to standard dialysate sodium concentration.
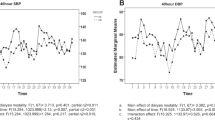
Effect of low dialysate sodium on 48 h and 24 h BPV parameters
The short-term BPV indices of SBP and DBP during the complete 48 h, intradialytic and the 24 h periods with the two different dialysate sodium concentrations are presented in Table 2. During the 48 h period, systolic BPV indices did not differ between low and standard dialysate sodium concentration (SBP-SD: 17.16 ± 5.34 vs. 16.99 ± 4.33 mmHg; p = 0.808; SBP-wSD: 16.08 ± 4.99 vs. 16.13 ± 4.16 mmHg, p = 0.943; SBP-CV: 12.46 ± 3.58 vs. 11.93 ± 3.18%, p = 0.201 and SBP-ARV: 12.22 ± 3.70 vs. 11.37 ± 3.34 mmHg, p = 0.181 with low vs. standard dialysate sodium, respectively, Fig. 1A, B). Similarly, no significant differences between the two dialysate sodium concentrations in systolic BPV parameters were observed during the 1st or the 2nd 24 h period, with an exception of SBP-CV over the 1st 24 h (12.73 ± 4.01 mmHg with low vs. 11.42 ± 3.63 mmHg with standard dialysate sodium, p = 0.006). During the intradialytic period, all BPV indices were higher with low compared to standard dialysate sodium); however, none of these differences reached statistical significance (Table 2).
With regards to diastolic BPV indices, 48 h BPV parameters studies were slightly lower with low compared to standard dialysate sodium, but without statistical significance (DBP-SD: 11.30 ± 2.82 vs. 11.50 ± 2.58 mmHg; p = 0.626; DBP-wSD: 10.71 ± 2.75 vs. 10.95 ± 2.49 mmHg, p = 0.542; DBP-CV: 14.12 ± 4.01 vs. 14.01 ± 4.13%, p = 0.817 and DBP-ARV: 8.27 ± 2.44 vs. 8.49 ± 1.93 mmHg, p = 0.561 with low vs. standard dialysate sodium, respectively, Fig. 1C, D). During the separate 24 h periods, no significant between-group differences in diastolic BPV indices were noted, although a similar pattern of numerically lower values with the low dialysate sodium was observed for all BPV parameters during the 2nd 24 h period.
Effect of low dialysate sodium on BPV parameters during day-time and night-time periods
BPV parameters of SBP and DBP during the day-time (Day-time 1 and Day-time 2) and night-time (Night-time 1 and Night-time 2) periods of the 48 h total observation period are presented in Table 3. During Day-time 1, all systolic and diastolic BPV indices did not differ significantly between the two dialysate sodium concentrations (SBP-ARV: 12.07 ± 4.05 vs. 11.76 ± 4.50 mmHg, p = 0.679; DBP-ARV: 8.23 ± 2.91 vs. 7.91 ± 2.18 mmHg, p = 0.580). Of note, during Day-time 2 all BPV parameters studied, with the exception of SBP-ARV, were considerably lower with the low dialysate sodium, with the difference being statistically significant only for DBP-SD (10.10 ± 3.11 vs. 11.40 ± 3.16 mmHg, p = 0.048).
With regards to night-time periods, non-significant differences were observed in all systolic and diastolic BPV indices examined during Night-time 1 (Table 3). During Night-time 2, all BPV parameters were numerically higher with the low compared to standard dialysate sodium, in contrast with what happened in most indexes during Day-time 2; these differences were statistically significant only for SBP-CV and SBP-ARV (SBP-CV: 10.60 ± 4.56 vs. 9.05 ± 3.59%, p = 0.044 and SBP-ARV: 12.33 ± 5.74 vs. 10.45 ± 3.71 mmHg, p = 0.041 with low vs. standard dialysate sodium, respectively).
Sensitivity analyses
Supplementary Table 1 presents the differences in 48 h BPV indices between low and high sodium dialysate in patients that were not on loop diuretics at baseline (n = 13); no significant differences in all 48 h BPV indices studied were detected. Supplementary Table 2 shows the differences in systolic and diastolic BPV indices during the 48 h with low vs standard dialysate sodium among patients treated with (n = 18) and without β-blockers (n = 11). There were not significant differences in BPV indices studied between low vs high sodium dialysate, except for 48 h DBP wSD and 48 h DBP CV that were higher with the high sodium dialysate in patients that were not receiving β-blockers. Similar observations were made regarding patients receiving or not α-blockers (Supplementary Τable 3).
Dipping pattern
Table 4 presents the dipping profile of the study participants during the 1st and the 2nd 24 h period. Νo significant differences were observed in the dipping pattern between low and standard dialysate sodium, during both the 1st 24 h (27.6%, 51.7% and 20.7% with low vs. 17.2%, 72.4% and 10.3% with standard dialysate sodium, p = 0.714) and the 2nd 24 h period (51.7%, 41.4%, and 6.9% with low vs. 34.5%, 55.2% and 10.3% with standard dialysate sodium, p = 0.167, for reverse dippers, non-dippers and dippers, respectively). Supplementary Tables 4 and 5 present the comparisons of 48 h BPV indices between non-dippers and reverse dippers with the low and high sodium dialysate, respectively. No significant between-group differences were detected in all studied BPV indices with both low and high dialysate sodium concentration.
Discussion
This is a prespecified secondary analysis of a randomized crossover study examining the effect of low (137 mEq/L) versus standard (140 mEq/L) dialysate sodium concentration on BPV indices during a complete 48 h period in patients with IDH. Ambulatory 48 h SBP/DBP was significantly lower with low dialysate sodium, with an observed mean difference of −5.3/−2.6 mmHg, compared with standard dialysate sodium concentration. However, in this analysis we noted no significant differences in BPV parameters during the 48 h period between low and standard dialysate sodium. Overall, this pattern of non-significant differences was consistent across the different 24 h periods, with an exception of SBP-CV during the 1st 24 h period. A trend towards non-significant decreases during the Day-time 2 was observed with the low dialysate sodium; a reverse trend towards higher values with the low compared to standard dialysate sodium was noted in all BPV indices during night-time 2, which was statistically significant only for SBP-ARV and SBP-CV.
The mechanistic background of IDH is multifactorial and involves several pathophysiological pathways, including volume and sodium overload, overactivity of sympathetic nervous system (SNS) and renin-angiotensin-aldosterone system (RAAS), endothelial dysfunction, and increased arterial stiffness [5, 6]. Among them, volume overload is considered to play a key role in the pathogenesis of the phenomenon and represents a rather consistent finding in these individuals. Evidence deriving from previous studies have shown that patients with IDH have higher percentage of total and extracellular water, as assessed with bioimpedance spectroscopy, compared to those without the phenomenon [25, 26]. A positive sodium gradient during hemodialysis has been also suggested to contribute in the development of IDH, through either an increase in IDWG [27], or a reduction in endothelial NO release, leading to vasoconstriction and increased peripheral vascular resistance [28]. SNS overactivation has been proposed to be another mechanism implicated in the pathophysiology of IDH. A study in 108 hemodialysis patients, showed that IDH episodes were associated with synchronous increases in heart rate and BPV, along with decreased baroreceptor sensitivity and enhanced sympatho-vagal balance; these findings support the hypothesis of an enhanced sympathetic outflow with feed-forward effects on BP in these individuals [29].
BPV components are determined by the complex interactions of cardiovascular regulatory mechanisms, humoral and rheological mechanisms, combined with environmental, emotional and behavioral factors [11]. In hemodialysis patients, we previously assesed BPV during the complete interdialytic interval and showed that BPV indices were particularly high and were all significantly increased, along with ambulatory BP, during the 2nd compared to the 1st 24 hour period [4]. Data regarding BPV levels in IDH patients are extremely rare. In a case-control study of our group including 41 patients with IDH and 82 controls, 48 h SBP/DBP levels were significantly higher in IDH patients. Overall, BVP indexes did not differ significantly between the two groups, although SBP-SD and SBP-wSD were numerically higher in cases compared to controls [17]. Increased BPV in the ESKD may be partly attributed to enhanced central sympathetic drive and impaired baroreflex function, suggesting that SNS overactivation is a potential common mechanism for both IDH and increased BPV [30].
Studies examining the effects of BP lowering strategies on BPV in dialysis patients are rare. Α randomized study in 40 hemodialysis patients showed lower 24 h SBP and DBP-CV values with losartan compared to treatment with any antihypertensive medication other than RAAS blockers [31]. Among non-pharmacological measures to reduce BP, the effect of dry-weight probing on short-term BPV was studied by our group in a randomized study in 71 hemodialysis patients. All SBP- and DBP-BPV indices, except 48 h SBP-CV and DBP-CV, were numerically lower after lung ultrasound guided dry-weight reduction, but not significantly different from baseline, despite a significant reduction in 48 h ambulatory BP [24]. With regards to dialysate sodium, one non-randomized study including 40 hemodialysis patients, previously showed a reduction in one-week average home systolic BPV-CV (home BP defined as average of 2 morning and 2 evening BP readings) after 8 weeks of low (136 mEq/L) dialysate sodium [32]. The only study examining BPV changes after a pharmacological intervention in IDH, evaluated in a randomized crossover design the effect of nebivolol and irbesartan on short-term BPV and demonstrated that 24 h, intradialytic and day-time systolic, but mostly diastolic BPV parameters were significantly reduced after nebivolol treatment [18]. Our study is the first to evaluate a non-pharmacological intervention, i.e. lowering dialysate sodium concentration, on short-term BPV indices in patients with IDH. It showed that low dialysate sodium, despite significantly reducing ambulatory BP levels through the whole interdialytic interval, has no sustained effect on BPV during the 48 h, 24 h or other specific time intervals. This finding can be explained by the mechanisms that mediate the studied phenomena. As has been previously suggested, changes in BPV may not be primarily attributed to change of BP per se and, thus, BPV decrease may not always follow BP decrease; changes in BPV depends rather on modification of the responsible pathogenetic mechanisms, i.e., SNS hyperactivity or reduced arterial compliance, which may be affected by specific but not all BP-lowering interventions [24]. In this case, SNS overactivation appears to be a common underlying mechanism for both IDH and increased BPV [30, 33]. However, other mechanisms contributing to IDH phenomenon, such as volume and sodium overload, may not be equally implicated in the pathogenesis of BPV. This notion is in perfect line with the previous observations in the field, such as reduction of BPV with nebivolol, a β-blocker interfering with SNS overactivation, but not irbesartan, in patients with IDH [18], as well as with the absence of effect in short-term BPV after applying a dry weight probing strategy [24]. Overall, all these strategies were effective in reducing ambulatory BP, but only one, i.e., β-blockade, was effective to reduce BPV, as it interfered with the most potent pathogenetic mechanism of BPV, i.e., SNS overactivation [33].
This study has strengths and limitations. It is the first study investigating the effect of low versus standard dialysate sodium concentration on BPV in patients with IDH in this population. It followed a careful randomized cross-over design, included a sufficient washout period of two weeks to avoid carryover effects and had a low drop out rate, as only 1 patient had invalid ABPM and refused to continue. Our main limitation is that our sample size was calculated based on the primary outcome of 48 h SBP, so this study may not be powered to detect changes in BPV indices. In addition, in this trial, we did not use individualized dialysate sodium for each patient and did not measure serum sodium in each phase of the study to detect changes in pre-dialysis sodium; we opted for a standard dialysate sodium concentration of 137 mEq/L for all participants, and not a lower level, that was deliberately made to avoid intradialytic complications, along with the longer exposure to standard dialysate sodium of 140 mEq/L, due to its use during the washout period, may have obscured higher between-group differences.
In conclusion, this is the first study examining the effect of low compared to standard dialysate sodium concentration on 48 h short-term BPV indices in patients with IDH. We showed that low dialysate sodium had no significant effect on BPV indices, despite the significantly lower ambulatory BP levels compared to standard dialysate sodium. These findings suggest that BP reducing measures may not have a parallel effect on BPV and therapeutic approaches that target common specific pathogenetic mechanisms of increased BP and BPV should be preferred in these individuals. As the full spectrum of BPV determinants is far from fully elucidated in clinical studies, future parallel-designed trials, powered to detect changes in BPV should further explore alternative interventions that effectively reduce BPV levels in patients with IDH. Furthermore, additional research is needed to investigate the potential association of BPV reduction with better cardiovascular outcomes in these individuals.
Summary
What is known about this topic
-
Patients with intradialytic hypertension (IDH) have an increased cardiovascular risk compared to hemodialysis patients exhibiting the usual BP fall during dialysis. Increased blood pressure (BP) variability (BPV) is also associated with high cardiovascular risk in hemodialysis patients and may contribute to the higher cardiovascular risk in these individuals.
-
The impact of non-pharmacological BP-lowering interventions on BPV in this population has not been previously studied.
What this study adds
-
This is the first study examining the effect of low (137 mEq/L) compared to standard (140 mEq/L) dialysate sodium concentration on 48-h short-term BPV parameters in patients with IDH.
-
Low dialysate sodium had no significant effect on BPV indices during the 48-h period, despite the significantly lower ambulatory BP levels compared to standard dialysate sodium.
Data availability
Access to trial data can be made available to researchers upon reasonable request to the corresponding author.
References
United States Renal Data System. 2022 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD. (2022).
Sarafidis PA, Persu A, Agarwal R, Burnier M, de Leeuw P, Ferro C, et al. Hypertension in dialysis patients: a consensus document by the European Renal and Cardiovascular Medicine (EURECA-m) working group of the European Renal Association - European Dialysis and Transplant Association (ERA-EDTA) and the Hypertension and the Kidney working group of the European Society of Hypertension (ESH). J Hypertens. 2017;35:657–76.
Karpetas A, Sarafidis PA, Georgianos PI, Protogerou A, Vakianis P, Koutroumpas G, et al. Ambulatory recording of wave reflections and arterial stiffness during intra- and interdialytic periods in patients treated with dialysis. Clin J Am Soc Nephrol. 2015;10:630–8.
Karpetas A, Loutradis C, Bikos A, Tzanis G, Koutroumpas G, Lazaridis AA, et al. Blood pressure variability is increasing from the first to the second day of the interdialytic interval in hemodialysis patients. J Hypertens. 2017;35:2517–26.
Georgianos PI, Sarafidis PA, Zoccali C. Intradialysis Hypertension in End-Stage Renal Disease Patients: Clinical Epidemiology, Pathogenesis, and Treatment. Hypertension. 2015;66:456–63.
Iatridi F, Theodorakopoulou MP, Papagianni A, Sarafidis P. Intradialytic hypertension: epidemiology and pathophysiology of a silent killer. Hypertens Res. 2022;45:1713–25.
Inrig JK, Patel UD, Toto RD, Szczech LA. Association of blood pressure increases during hemodialysis with 2-year mortality in incident hemodialysis patients: a secondary analysis of the Dialysis Morbidity and Mortality Wave 2 Study. Am J Kidney Dis. 2009;54:881–90.
Park J, Rhee CM, Sim JJ, Kim Y-L, Ricks J, Streja E, et al. A comparative effectiveness research study of the change in blood pressure during hemodialysis treatment and survival. Kidney Int. 2013;84:795–802.
Inrig JK, Oddone EZ, Hasselblad V, Gillespie B, Patel UD, Reddan D, et al. Association of intradialytic blood pressure changes with hospitalization and mortality rates in prevalent ESRD patients. Kidney Int. 2007;71:454–61.
Parati G, Ochoa JE, Bilo G, Agarwal R, Covic A, Dekker FW, et al. Hypertension in Chronic Kidney Disease Part 2: Role of Ambulatory and Home Blood Pressure Monitoring for Assessing Alterations in Blood Pressure Variability and Blood Pressure Profiles. Hypertension. 2016;67:1102–10.
Parati G, Bilo G, Kollias A, Pengo M, Ochoa JE, Castiglioni P, et al. Blood pressure variability: methodological aspects, clinical relevance and practical indications for management - a European Society of Hypertension position paper ∗. J Hypertens. 2023;41:527–44.
Sarafidis PA, Ruilope LM, Loutradis C, Gorostidi M, de la Sierra A, de la Cruz JJ, et al. Blood pressure variability increases with advancing chronic kidney disease stage: a cross-sectional analysis of 16 546 hypertensive patients. J Hypertens. 2018;36:1076–85.
Alexandrou ME, Loutradis C, Schoina M, Tzanis G, Dimitriadis C, Sachpekidis V, et al. Ambulatory blood pressure profile and blood pressure variability in peritoneal dialysis compared with hemodialysis and chronic kidney disease patients. Hypertens Res. 2020;43:903–13.
Flythe JE, Inrig JK, Shafi T, Chang TI, Cape K, Dinesh K, et al. Association of intradialytic blood pressure variability with increased all-cause and cardiovascular mortality in patients treated with long-term hemodialysis. Am J Kidney Dis. 2013;61:966–74.
Chang TI, Flythe JE, Brunelli SM, Muntner P, Greene T, Cheung AK, et al. Visit-to-visit systolic blood pressure variability and outcomes in hemodialysis. J Hum Hypertens. 2014;28:18–24.
Sarafidis PA, Loutradis C, Karpetas A, Tzanis G, Bikos A, Raptis V, et al. The association of interdialytic blood pressure variability with cardiovascular events and all-cause mortality in haemodialysis patients. Nephrol Dial Transplant. 2019;34:515–23.
Bikos A, Angeloudi E, Memmos E, Loutradis C, Karpetas A, Ginikopoulou E, et al. A Comparative Study of Short-Term Blood Pressure Variability in Hemodialysis Patients with and without Intradialytic Hypertension. Am J Nephrol. 2018;48:295–305.
Loutradis C, Bikos A, Raptis V, Afkou Z, Tzanis G, Pyrgidis N, et al. Nebivolol reduces short-term blood pressure variability more potently than irbesartan in patients with intradialytic hypertension. Hypertens Res. 2019;42:1001–10.
Inrig JK, Molina C, D’Silva K, Kim C, Van Buren P, Allen JD, et al. Effect of low versus high dialysate sodium concentration on blood pressure and endothelial-derived vasoregulators during hemodialysis: a randomized crossover study. Am J Kidney Dis. 2015;65:464–73.
Robberechts T, Allamani M, Galloo X, Wissing KM, Van Der Niepen P. Individualized Isonatremic and Hyponatremic Dialysate Improves Blood Pressure in Patients with Intradialytic Hypertension: A Prospective Cross-Over Study with 24-h Ambulatory Blood Pressure Monitoring. Open Journal of Nephrology. 2020;10:144–57.
Nair SV, Balasubramanian K, Ramasamy A, Thamizhselvam H, Gharia S, Periasamy S Effect of low dialysate sodium in the management of intradialytic hypertension in maintenance hemodialysis patients: A single-center Indian experience. Hemodial Int Published Online First: 18 March 2021. https://doi.org/10.1111/hdi.12921
Iatridi F, Malandris K, Ekart R, Xagas E, Karpetas A, Theodorakopoulou MP, et al. Low dialysate sodium and 48-h ambulatory blood pressure in patients with intradialytic hypertension: a randomized crossover study. Nephrol Dial Transplant. 2024:gfae104. https://doi.org/10.1093/ndt/gfae104. Epub ahead of print.
Wei W, Tölle M, Zidek W, van der Giet M. Validation of the mobil-O-Graph: 24 h-blood pressure measurement device. Blood Press Monit. 2010;15:225–8.
Loutradis C, Sarafidis PA, Theodorakopoulou M, Ekart R, Alexandrou ME, Pyrgidis N, et al. Lung Ultrasound-Guided Dry-Weight Reduction in Hemodialysis Patients Does Not Affect Short-Term Blood Pressure Variability. Am J Hypertens. 2019;32:786–95.
Nongnuch A, Campbell N, Stern E, El-Kateb S, Fuentes L, Davenport A. Increased postdialysis systolic blood pressure is associated with extracellular overhydration in hemodialysis outpatients. Kidney Int. 2015;87:452–7.
Van Buren PN, Zhou Y, Neyra JA, Xiao G, Vongpatanasin W, Inrig J, et al. Extracellular Volume Overload and Increased Vasoconstriction in Patients With Recurrent Intradialytic Hypertension. Kidney Blood Press Res. 2016;41:802–14.
Song JH, Park GH, Lee SY, Lee SW, Lee SW, Kim M-J. Effect of sodium balance and the combination of ultrafiltration profile during sodium profiling hemodialysis on the maintenance of the quality of dialysis and sodium and fluid balances. J Am Soc Nephrol. 2005;16:237–46.
Oberleithner H, Riethmüller C, Schillers H, MacGregor GA, de Wardener HE, Hausberg M. Plasma sodium stiffens vascular endothelium and reduces nitric oxide release. Proc Natl Acad Sci USA. 2007;104:16281–6.
Rubinger D, Backenroth R, Sapoznikov D. Sympathetic activation and baroreflex function during intradialytic hypertensive episodes. PLoS One. 2012;7:e36943.
Neumann J, Ligtenberg G, Klein II, Koomans HA, Blankestijn PJ. Sympathetic hyperactivity in chronic kidney disease: pathogenesis, clinical relevance, and treatment. Kidney Int. 2004;65:1568–76.
Mitsuhashi H, Tamura K, Yamauchi J, Ozawa M, Yanagi M, Dejima T, et al. Effect of losartan on ambulatory short-term blood pressure variability and cardiovascular remodeling in hypertensive patients on hemodialysis. Atherosclerosis. 2009;207:186–90.
Chen Z, Sun F, Shen Y, Ma L, Liu J, Zhou Y. Impact of Dialysate Sodium Concentration Lowering on Home Blood Pressure Variability in Hemodialysis Patients. Ther Apher Dial. 2019;23:153–9.
Parati G, Esler M. The human sympathetic nervous system: its relevance in hypertension and heart failure. Eur Heart J. 2012;33:1058–66.
Author information
Authors and Affiliations
Contributions
Research idea and study design: Fotini Iatridi, Pantelis Sarafidis; data acquisition: Fotini Iatridi, Efstathios Xagas, Robert Ekart, Antonios Karpetas, Ioanna Revela, Marieta Theodorakopoulou, Eleni Karkamani, Nikolaos Devrikis; data analysis/interpretation: Fotini Iatridi, Pantelis Sarafidis; statistical analysis: Fotini Iatridi; manuscript drafting: Fotini Iatridi, Pantelis Sarafidis; supervision or mentorship: Aikaterini Papagianni, Pantelis Sarafidis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study protocol was approved by the Ethics Committee of the School of Medicine, Aristotle University of Thessaloniki (Approval Number 4555).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Iatridi, F., Ekart, R., Xagas, E. et al. Dialysate sodium and short-term blood pressure variability in patients with intradialytic hypertension: a randomized crossover study. J Hum Hypertens (2024). https://doi.org/10.1038/s41371-024-00947-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41371-024-00947-w
- Springer Nature Limited