Abstract
Hypertension is a leading cause of non-communicable morbidity in Sub Saharan Africa. Recent studies suggest and increase in the prevalence of hypertension in rural Sub-Saharan Africa. Using a three-phase approach, a structured questionnaire was used to determine the prevalence of hypertension in a rural settlement is Enugu State, Southeast Nigeria. Blood pressure measurement was done according to the guidelines of the European Society of Hypertension. Out of 1576 participants aged 18 years and above, 1082 (68.7%) completed the full survey, their blood pressure was measured, and data analyzed. The prevalence of hypertension in this study was 27.6%, (95%CI 25–30.4), similar in males 29.2, (95%CI 24.7–30.4) and females 26.8%, (95%CI 23.5–30.2). p = 0.39. The prevalence of hypertension increased with age reaching a peak of 32.8% (95%CI 26.2–40) in the 40–49 age group, however this was not statistically significant P = 0.22. This age-related increase in the prevalence of hypertension tended towards significance in males (p = 0.05) but not in females (p = 0.44). Awareness of hypertension was 7.2%. Systolic blood pressure positively correlated with older age, higher blood glucose levels and waist-hip ratio. Diastolic blood pressure correlated with the type of work the patients is involved in and blood glucose levels. In conclusion, the prevalence of hypertension in a rural southeastern Nigeria community was 27.6%, however awareness was very low (7.9%). Most participants had mild hypertension thus offering a window of opportunity for public health educators in preventing the complications of hypertension. There is therefore the need for awareness campaigns to be intensified in rural communities.
Similar content being viewed by others
Introduction
Hypertension is a leading cause of noncommunicable morbidity in Sub-Saharan Africa (SSA) [1,2,3,4,5,6,7,8]. The high prevalence of hypertension is reflected in high rates of complications reported in several studies [3, 9, 10]. Most recent studies have persistently reported prevalence rates of 20 to 50% and more than 50% in some Nigerian populations [2, 3, 11,12,13] A mean prevalence of 30.6% was reported in the country as at 2002 [4]. Although the prevalence of hypertension has generally been found to be lower in rural areas and semi urban areas, nevertheless this is also on the increase [1, 14]. In one mixed urban and rural study; the prevalence of hypertension was higher in rural compared to urban communities [15]. The burden and treatment of hypertension in SSA is wrought with several peculiarities such as lack of access to medications, the use of substandard and adulterated drugs, use of non-orthodox modes of treatment, late presentation and generally poor knowledge, attitude, and practice of hypertension [5]. These factors are more accentuated in rural areas because of several reasons including lower rates of literacy, lack of access to standard health care, and cultural beliefs [3, 4, 14, 16, 17].
Surprisingly relatively large number studies have been focused on the prevalence of hypertension in rural compared to urban communities in Nigeria [14]. In a review by Adeloye et al. [14] out of 53 studies, 18 (34%) were dedicated to rural communities and 13 (24.5%) were carried out in mixed urban and rural settings. The mean prevalence of hypertension among rural dwellers based on the review was 24.5% compared to 33.6% in urban centers. There is therefore a general trend towards lower prevalence rates in rural compared to urban areas [1, 14]. There are also differences between the prevalence of hypertension and practice of hypertension between males and females with females having lower rates and being more aware [16,17,18].
In Nigeria, the knowledge and practice of hypertension is affected by poor socio-economic status of patients as well as shortage of qualified specialists; hence, treatment is often uncoordinated, and drugs changed as patient moves from one doctor to another [19,20,21]. It was our hypothesis that since most of the factors that undermine the treatment of hypertension are more acute in rural settings, the prevalence of hypertension may be higher than previously reported. The aim of this study was to document the prevalence and pattern of hypertension among a rural settlement in Enugu south Local Government Area in Enugu State, Southeast Nigeria.
Materials and methods
This study was carried out in Ugwuomu Village in Enugu South Local Government area of Enugu State. There was no reliable data on the population of the village available at the time of the study. The village is located 20 kilometers from the city center and about 4 km from the nearest semi-urban settlement. Ugwuomu has one primary and one secondary school which is also attended by people from surrounding villages. There was a health center in the village at the time of the study. Although most health-care needs within the villages are delivered by auxiliary nurses, many people travel to the nearest semi- urban area for their healthcare needs. People can also access care from other government health institution within Enugu metropolis. Sources of drinking water are mainly well water or streams. Formal sewage disposal system is non-existent in the village, but several homes have either pit latrines or water closet system.
Study design and recruitment of participants
A three-phase cross-sectional descriptive study was carried out to survey residents of the village. The first phase of the study was sensitization of the community through meetings with elected community leaders. Announcements were also made in churches as well as by town announcer. The first phase of the study was carried in the first week but also continued into the second phase (3weeks in all).
In the second phase of the study, participants were visited in their homes. During this phase a structured questionnaire was used to collect data on selected socio-demographic characteristics. All consenting individuals were interviewed at their respective homes or offices/places of work. Participants were also invited to come to the clinic on any day of their choice within the stipulated time and when necessary for follow up. This phase of the study started on the second week and lasted till the end of the third week. (2 weeks in all).
The third phase of the study was carried out in a field clinic during the fourth week of the study, however it also overlapped with the last week of the second phase. In this phase, the remaining part of the questionnaire on physical measurements of weight, height, blood pressure and fasting blood glucose were carried out. Medical history of hypertension was also obtained from the subjects. The third phase of the survey lasted for one week.
The duration of the study was 4 weeks (1st to the 4th week of August 2019). All consecutive consenting adults 18 years and above were included in the study.
The scope of the present study is limited to behavioral and physical measurements and did not include biochemical measurements (apart from fasting blood glucose).
The study protocol was reviewed on behalf of State (Enugu State) Ministry of Health by the Ethics committee of the Enugu State University of Science and Technology Teaching Hospital and University of Nigeria Teaching Hospital, Enugu. All participants gave their informed consent after reading or having the consent form read for and explained to them.
Blood pressure measurement
All eligible participants who gave their consent where interviewed. If a household have more than one eligible person all were recruited and interviewed. All participants were first interviewed at home, but blood pressure measurement was done in the field clinic. After resting for at least 10 min, blood pressures were recorded at least 3 times by means of mercury sphygmomanometer according to the guidelines of the European Society of Hypertension. [22] Blood pressure was measured by either a trained nurse or by one of the investigators (the doctors). All the doctors that participated in the study were either senior residents or consultants in the Department of Medicine. Blood pressure measurements were obtained from the non-dominant arm using a standard cuff with an inflatable bladder of 22 × 12 cm2 if the arm circumference was 32 cm, and cuffs with a 35 × 15 cm2 bladder on larger arms. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were taken at the first and fifth Korotkoff sounds, respectively. The average of the three blood pressure measurements was used for the analysis. Fasting blood glucose was measured using a glucometer (Fine test premium; Infobia Co. Ltd, Dongan-gu, South Korea). The waist and hip circumference were measured using a standard centimeter tape, by standard method.
Definition of terms
Hypertension was defined as an SBP of ⩾140 mmHg and/or DBP of ⩾90 mmHg, and/or reporting use of antihypertensive drug therapy. Elevation in blood pressure was define as follows: Normal blood pressure systolic blood pressure less than 140 and diastolic blood pressure less than 90 mmHg, stage I hypertension as systolic blood pressure from ranging 140 to 159 and diastolic blood pressure from 90 to 99 mmHg, stage II hypertension as systolic blood pressure ranging from 160 to 179 and diastolic blood pressure from 100 to 109 mmHg, and stage III hypertension systolic blood pressure equal or greater than 180 and diastolic blood pressure equal or 110 90 mmHg. Awareness was confirmed by asking for past medical history of raised blood pressure recorded by a health professional or identifying those who were taking blood pressure lowering medications. A patient is defined as having hypertension awareness if there was a history of hypertension diagnosed by a qualified health worker (nurses or doctors). All new cases of hypertension were started on medications and were referred to the health center of any hospital nearest to them for continued care.
Occupation was defined as the respondent’s primary job and or source of income in a month. An artisan was defined as a skilled manual worker in a particular trade or craft, such as masonry, mechanics, tailoring, welding, metal working and other crafts. Professional drivers were also grouped as artisans. Office workers included teachers, civil servants and individuals that spend most of their working hours in the office. Level of education was the highest educational attainment (primary education, secondary, and tertiary) at the time of the study. Farmers and artisans well considered to be manual workers, while the rest were grouped and non-manual workers.
Sample size
The sample size was calculated using the proportion (23.2%) of a rural population with hypertension in Southeast Nigeria.
Using the formula: N = (Z2pq)d2.
Where N = desired sample size and population.
P = prevalence rate of hypertension, d=desired precision limit assumed at 5%
N = (1.96)2 × 0.231 × 0.77/0.0025 = 273.3
N = 273.3. Adding 10% of the sample size to mitigate for attrition of participants, we obtained a minimum sample size of 300 participants.
Statistical methods
For database management and statistical analyses, we used the SPSS version 26 (IBM Corporation, New York, NY, USA). Data were presented in tables and figures. For continuous variables, mean values and standard deviation were calculated. Prevalence of hypertension was expressed as percentages, and confidence interval (CI) was calculated. Other statistical methods also included Student’s T-test for unpaired observations to compare means. Bivariate correlation analysis was done (age, Waist-Hip ratio, fasting blood glucose, level of education (1 primary, 2 secondary, 3 tertiary) and occupation [1 Low level of activity (students, unemployed), 2 moderate level of activity (office workers and teachers), and 3 high levels of activity (farmers and artisans) as 3], depending of the level of physical activity involved). Correlation analysis was done using Spearman correlation statistics for dichotomous variables and Pearson’s statistic for continuous variables. In all, P value < 0.05 was regarded as statistically significant. Conclusions were drawn at the level of significance. The confidence level was kept at 95%.
Results
Characteristics of the participants
Out of 1576 participants who were initially surveyed, 1082 (68.7%) completed the full survey, their blood pressures were measured, and their data analyzed. Females were 695 (64.2%) and males 387 (35.8%). The age distribution of the participants is shown in Table 1 and Fig. 1. The mean age of the participants was 41.9 (95% CI, 40.9–41.2) years.
The age and sex distribution of those who were excluded showed that 172 (34.8%) were males and 322 (65.2) were females. Their mean age was 42.4 ± 16.8 years. There was no statistical difference in their ages (males 41.3 ± 17.5 and females 43 ± 16.4. p = 0.3).
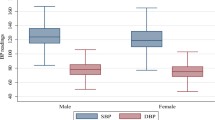
Within the group that was analyzed, there was no significant difference in the mean age of female and male participants (p = 0.78). Waist and hip circumferences were larger in females P < 0.01 respectively (Table 1). The educational attainment of the participants and their occupations are also shown in Table 1. Mean systolic and diastolic blood pressures were similar in both sexes. Fasting blood glucose was higher in males (111.6(95% CI,108.1–117.3) than in females (106.4(95% CI,104.5–109.2). P = 0.03.
Blood pressure
Table 2 shows the age distribution of blood pressure measurements in males and females. In females, the average systolic blood pressure increased with age reaching a peak of 128.5(95%CI 125.5–131.5) mmHg in people aged 40–49 years. There were no significant changes in the age distribution of blood pressure measurements in males.
The blood pressure measurement recorded during the study showed that 19% had mild elevation in systolic blood pressure and 7.1% had mild elevation of diastolic blood pressure. Table 3. Severe elevation in systolic blood pressure was recorded in 41 (3.8%) and diastolic blood pressure in 25 (2.3%) of the population studied.
The prevalence of hypertension in this study was 27.6%, (95%CI 25–30.4), similar in males 29.2, (95%CI 24.7–30.4) and females 26.8%, (95%CI 23.5–30.2). p = 0.39. Table 2. The prevalence of hypertension increased with age reaching a peak of 32.8% (95%CI 26.2–40) in the 40–49 age group, however, this was not statistically significant P = 0.22. This age-related increase in the prevalence of hypertension tended towards significance in males (p = 0.05) but not in females (p = 0.44). Table 2.
Age, Systolic and diastolic blood pressure measurements, and waist hip ratio were found to be abnormally distributed after normality check. (Shapiro-Wilk test, p < 0.01 in all cases). Using Spearman’s rho correlation statistic, systolic and diastolic blood pressures positively correlated with older age and higher blood glucose levels. Systolic blood pressure also correlated with waist-hip ratio (Table 4).
Discussion
This study found a 27.6% prevalence of hypertension in a rural community most of them detected for the first time (92.2%). Systolic blood pressure correlated with older age, higher fasting blood glucose levels and increased waist-hip ratio. Diastolic blood pressure correlated the type of occupation and blood glucose levels.
The prevalence of hypertension and its complications are increasing in Africa [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20, 23]. Across the continent the burden of hypertension is compounded by poor health infrastructure, dearth of manpower and competition for resources with other communicable and non-communicable diseases [1, 2]. Hypertension is strongly related to other non-communicable disease such as diabetes, obesity and the metabolic syndrome which in turn lead to a rising incidence and prevalence of stroke, heart disease, and renal disease in the country. Reasons for the rapid rise in the prevalence of hypertension among black Africans can be related to urbanization, diet and sedentary lifestyle [24]. There is also the associated increase in rates of alcohol consumption and smoking [25,26,27]. Overall, the prevalence of hypertension in Nigeria has remained above 25% in most studies, with studies from rural setting giving lower prevalence [1, 14].
The prevalence of hypertension in this study was 27.6%, out of which 97.2% were not aware of their condition. Some studies in Nigeria have reported prevalence rates of hypertension higher than 50% depending on the population studied [3, 12, 28,29,30]. Factors that may lead to lower rates of hypertension in rural areas include vigorous physical activities associated with farming, artisanal work, trekking long distances and possibly undernutrition [31]. Diet may also be contributory because most rural dwellers are less likely to overindulge in refined fatty meals associated with urban dwellers.
It is evident from some recent studies that the differences between rural and urban rates of hypertension in Nigeria may be narrowing [2] which may in turn be related to population movements and changing lifestyles. Other factors likely to be associated with the rising burden of hypertension in rural areas include poor knowledge and practice of hypertension [1] and older age of rural dwellers (retirees) [32, 33]. Other factors which are often modifiable and preventable are the same for rural and urban areas.
In Nigeria as well in the rest of the continent the prevalence of hypertension in both rural and urban areas varies widely both within and between regions [1, 34,35,36,37,38]. In the index study, the prevalence of hypertension is similar to some studies that were done among rural dwellers. Adebayo et al [38] reported a prevalence rate of 26.4%. Reports from other surveys ranged from 13.8% to 44.5% [3,4,5, 14, 39, 40].
In the index study the prevalence of hypertension peaked at 40–49 years. This is slightly different from other studies from southeast Nigeria [3, 4]. Most of the participants in the index study had mild hypertension and this finding brings to the fore the need for early and multi-dimensional public health programs targeting middle aged and older adults in the prevention of hypertension and its complications.
The correlation between blood pressure and age and blood glucose [3, 17, 31, 39, 40] was also confirmed in the index study. The relationship between hypertension and age has been attributable to several factors including higher rates of obesity, glucose intolerance, sedentary lifestyles, and arterial stiffness [3, 23].
Awareness of hypertension is defined as a fraction of people who have hypertension in a given population that have been previously diagnosed. Hypertension unawareness (newly diagnosed) in this study was 97.2%. Long distance to hospitals, poor knowledge and practice of hypertension, the severity of hypertension (most participants had mild uncomplicated hypertension) and lack of health workers in the rural areas may be some of the reasons why many cases of hypertension were not detected in the present study. In a previous study among sub-urban dwellers, we reported a 40% rate of hypertension awareness much higher than 2.8% in the index study [3]. In Sub-Saharan Africa, hypertension awareness ranges from 8% in Nigeria to 65% in Seychelles [24]. Okello et al [17] reported an average of 57.2% of hypertension awareness across 7 settlements in Africa. Unlike in most studies, in the index study there was no difference in the rates of hypertension awareness between men and women [8].
One of the commonest factors leading to complications in hypertension is unawareness. This is primarily because hypertension is largely asymptomatic, therefore, to reduce the complications of hypertension, awareness needs to be increased through checks in adults at every given opportunity. This task should be undertaken by public and private health care providers on regular basis. Awareness of hypertension may be a surrogate for the capacity of the health system to provide diagnostic health services for the general population at all levels because blood pressure measurement is an integral part of all forms of health assessment irrespective the disease or medical subspecialty in question. Unfortunately, our primary and secondary healthcare services are primarily under private health care providers and is largely constrained by communicable diseases and child and maternal diseases.
Mean SBP and DBP measurements are similar in males and females in this study, a pattern different from other studies [3, 4, 14,15,16]. Over the decades, statistics have shown a gradual increase in the mean systolic and diastolic blood pressure values among Nigerians [41]. This may be related to the some of the factors earlier stated. Both systolic and diastolic blood pressure measurements significantly increased with age reaching a peak of 128.5/70.1 mmHg in 40–49 age-group. The peak blood pressure measurement within this age group may be related to higher levels of unawareness among them (98.4% in 40–49-year-old and 94.4% in those 60 years and above). Older people are likely to be diagnosed and on treatment.
Most individuals in the index study were found to have mild hypertension. This finding is the same in males and females and presents a window of opportunity in primary prevention of the complications of hypertension. Our study showed strong correlation between age, blood glucose level, waist hip ratio and systolic blood pressure. Diastolic blood pressure also positively correlated with blood glucose levels. These findings support already known relationships between these variables. The higher number of women in the index study have affected our results. Typically, in rural southeast Nigeria, women are more likely to be at home during working hours and thus were more likely to be recruited.
Diastolic blood pressure was higher in individuals who were engaged in more strenuous jobs like farmers and artisans. This may be related to the age of the participants. In the index study the mean age of farmers was 48.9 years compared to 25.6 years in students.
The present study documented the prevalence of hypertension in a rural setting in southeast Nigeria. Considering that most Nigerians live in rural areas, this survey therefore provides data in an area where hitherto data on prevalence of hypertension has been lacking. Data on hypertension in rural areas therefore will help to reduce the high burden of hypertension in the country and consequently the rising prevalence of stroke and other complications of hypertension.
Limitations
This study is not without some limitations. The mean age of 41.9 years in this study suggests that our findings may reflect the younger age group. This notwithstanding, our tables showed age specific prevalence of hypertension to be similar to previous studies. Secondly, we did not collect data on risk factors, such as alcohol use, tobacco use and physical activity. The knowledge of the pattern of these risk factors would have helped to explain further the reasons for some of our findings. Thirdly, population dynamics might have affected our findings because some people who were interviewed may work in urban centers, while living in the village, thus some of the factors affecting the prevalence of hypertension in urban areas may also be applicable in this study. Fourthly, the significantly higher proportion of female subjects may also introduce some bias. Lastly data on hypertension awareness were self-reported, and there was no supporting medical records or data accessed. These shortcomings notwithstanding; based on external consistency of our data with those of similar studies, our results may well be a representative of rural areas in Enugu State.
Conclusion
The prevalence of hypertension in a rural southeastern Nigeria community is 27.6%, however awareness was very low (2.8%). Most participants had mild hypertension thus offering a window of opportunity for public health education in preventing the complication of hypertension. There is therefore the need for awareness campaigns to be intensified in rural communities by means of radio, religious groups as well as social events. Medical care both in public and private facilities should always be wholistic and blood pressure checked at every possible occasion with emphasis on healthy adopting healthy lifestyle and adherence to medications.
Summary
What is known about the topic
-
High rates of mild hypertension in a rural village in Nigeria.
-
Possible lower prevalence of hypertension in rural Nigeria.
-
Poor blood pressure control.
What this study adds
-
High prevalence of hypertension in rural Africa.
-
Overall high rate of hypertension but very low rates of severe hypertension.
-
Very low rate of hypertension awareness.
References
Adeloye D, Basquill C. Estimating the prevalence and awareness rates of hypertension in Africa: a systematic analysis. PLoS ONE. 2014;9:e104300.
Ebirim CIC, Udujih OG, Dozie UW, Agbaka CA, Orji SM, et al. Prevalence of Hypertension among adults aged 40 years and above in Ahiazu Mbaise, Imo State, Nigeria. Arch Community Med Public Health. 2018;4:013–6.
Ezeala-Adikaibe BA, Orjioke C, Ekenze OS, Ijoma U, Onodugo O, Chime P, et al. Population-based prevalence of high blood pressure among adults in an urban slum in Enugu, South East Nigeria. J Hum Hypertens [Internet]. 2016;30. https://pubmed.ncbi.nlm.nih.gov/26016595/. Accessed 6 Mar 2023.
Ulasi II, Ijoma CK, Onwubere BJC, Arodiwe E, Onodugo O, Okafor C. High prevalence and low awareness of hypertension in a market population in enugu, Nigeria. Int J Hypertens. 2011;2011:869675.
Odili AN, Chori BS, Danladi B, Nwakile PC, Okoye IC, Abdullahi U, et al. Prevalence, awareness, treatment and control of hypertension in Nigeria: data from a nationwide survey 2017. Glob Heart. 2020;15:47.
Odili AN, Thijs L, Hara A, Wei FF, Ogedengbe JO, Nwegbu MM, et al. Prevalence and determinants of masked hypertension among Black Nigerians compared with a reference population. Hypertension. 2016;67:1249–55.
Ugwuja E, Ezenkwa U, Nwibo A, Ogbanshi M, Idoko O, Nnabu R. Prevalence and determinants of hypertension in an agrarian rural community in Southeast Nigeria. Ann Med Health Sci Res. 2015;5:45–9.
Addo J, Smeeth L, Leon DA. Hypertension in sub-saharan Africa: a systematic review. Hypertension. 2007;50:1012–8.
Arodiwe EB, Ike SO, Nwokediuko SC. Case fatality among hypertension-related admissions in Enugu, Nigeria. Niger J Clin Pract. 2009;12:153–6.
M’Buyamba-Kabangu JR, Biswika RT, Thijs L, Tshimanga GM, Ngalula FM, Disashi T, et al. In-hospital mortality among black patients admitted for hypertension-related disorders in Mbuji Mayi, Congo. Am J Hypertens. 2009;22:643–8.
Ezejimofor MC, Uthman OA, Maduka O, Ezeabasili AC, Onwuchekwa AC, Ezejimofor BC, et al. The burden of hypertension in an oil- and gas-polluted environment: a comparative cross-sectional study. Am J Hypertens. 2016;29:925–33.
Olamoyegun M, Iwuala S, Asaolu S, Oluyombo R. Epidemiology and patterns of hypertension in semi-urban communities, south-western Nigeria. Cardiovasc J Afr. 2016;27:356–60.
Amole IO, OlaOlorun AD, Odeigah LO, Adesina SA. The prevalence of abdominal obesity and hypertension amongst adults in Ogbomoso, Nigeria. Afr J Prim Health Care Fam Med. 2011;3:188.
Adeloye D, Owolabi EO, Ojji DB, Auta A, Dewan MT, Olanrewaju TO, et al. Prevalence, awareness, treatment, and control of hypertension in Nigeria in 1995 and 2020: A systematic analysis of current evidence. J Clin Hypertens. 2021;23:963–77.
Effiong EA, Udeme EE, Udo AIA, Bassey BE. Prevalence of hypertension in Akwa Ibom State, South-South Nigeria: rural versus urban communities study. Int J Hypertens. 2015;2015:975819.
Isezuo AS, Opara TC. Hypertension awareness among Nigeria hypertensives in a Nigerian tertiary health institution. Sahel Med J. 2000;3:93.
Okello S, Muhihi A, Mohamed SF, Ameh S, Ochimana C, Oluwasanu AO, et al. Hypertension prevalence, awareness, treatment, and control and predicted 10-year CVD risk: a cross-sectional study of seven communities in East and West Africa (SevenCEWA). BMC Public Health. 2020;20:1706.
van de Vijver S, Akinyi H, Oti S, Olajide A, Agyemang C, Aboderin I, et al. Status report on hypertension in Africa—consultative review for the 6th Session of the African Union Conference of Ministers of Health on NCD’s. Pan Afr Med J. 2013;16:38.
Ezeala‐Adikaibe B, H O, C O, T O, Aneke E, Chime P, et al. Prescription pattern of anti-hypertensive drugs in Enugu: a report of ESUT research group. Eur J Biomed Pharm Sci. 2016;3:72–7.
Isezuo AS, Njoku CH. Blood pressure control among hypertensives managed in a specialised health care setting in Nigeria. Afr J Med Med Sci. 2003;32:65–70.
Etuk E, Isezuo SA, Chika A, Akuche J, Ali M. Prescription pattern of anti-hypertensive drugs in a tertiary health institution in Nigeria. Ann Afr Med. 2008;7:128–32.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Cappuccio FP, Miller MA. Cardiovascular disease and hypertension in sub-Saharan Africa: burden, risk and interventions. Intern Emerg Med. 2016;11:299–305.
World Health Organization. Noncommunicable diseases country profiles 2011 [Internet]. World Health Organization; 2011. https://apps.who.int/iris/handle/10665/44704. Accessed 6 Mar 2023.
Global status report on alcohol and health 2018 [Internet]. https://www.who.int/publications-detail-redirect/9789241565639. Accessed 6 Mar 2023.
Onodugo OD, Ezeala-Adikaibe BA, Anyim OB, Ezeme M, Ijoma UN, Obumneme-Anyim IN, et al. Prevalence and pattern of alcohol use among adults in an urban slum in South East Nigeria. Open J Psychiatry. 2019;09:179–91.
Donatus OO, Casmir O, Anyim OB, Adikaibe EAB, Peter C, Nkiruka OP, et al. Correlates of tobacco and marijuana use among urban dwellers in Enugu, Nigeria. Open J Prev Med. 2019;9:80–94.
Bello-Ovosi BO, Asuke S, Abdulrahman SO, Ibrahim MS, Ovosi JO, Ogunsina MA, et al. Prevalence and correlates of hypertension and diabetes mellitus in an urban community in North-Western Nigeria. Pan Afr Med J. 2018;29:97.
Sawaya AL, Sesso R, Florêncio TM, de MT, Fernandes MTB, Martins PA. Association between chronic undernutrition and hypertension. Matern Child Nutr. 2005;1:155–63.
Okeke C, Uzochukwu B, Nawfal E, Abada E, Uzochukwu B. Prevalence of hypertension and awareness of the causes and effects of hypertension in rural and urban communities of Enugu State Nigeria. Int J Sci TEchnol Res. 2017;6:26–32.
Hendriks ME, Wit FWNM, Roos MTL, Brewster LM, Akande TM, de Beer IH, et al. Hypertension in sub-Saharan Africa: cross-sectional surveys in four rural and urban communities. PloS One. 2012;7:e32638.
Gaye B, Janeczek AL, Narayanan K, N’Guetta R, Vignac M, Gallardo V, et al. Prevalence of severe hypertension in a Sub-Saharan African community. Int J Cardiol Hypertens. 2019;2:100016.
Guwatudde D, Nankya-Mutyoba J, Kalyesubula R, Laurence C, Adebamowo C, Ajayi I, et al. The burden of hypertension in sub-Saharan Africa: a four-country cross sectional study. BMC Public Health. 2015;15:1211.
Isara AR, Okundia PO. The burden of hypertension and diabetes mellitus in rural communities in southern Nigeria. Pan Afr Med J. 2015;20:103.
Orji IA, Ikechukwu-Orji MU. Burden of hypertension and associated risk factors in rural communities of Abuja. Texila Int J Pub Health. 2019;7. https://doi.org/10.21522/TIJPH.2013.07.01.ART004
Ibama AS, Uzondu PU, Amadi AN, Ibulobo R, Timothy T. Prevalence of hypertension among adults in rural setting in Nigeria: the need for paradigm shift in prevention and control. Med Clin Case Rep [Internet]. 2021;1. https://scivisionpub.com/pdfs/prevalence-of-hypertension-among-adults-in-rural-setting-in-nigeria-the-need-for-paradigm-shift-in-prevention-and-control-1657.pdf. Accessed 6 Mar 2023.
Ahaneku GI, Osuji CU, Anisiuba BC, Ikeh VO, Oguejiofor OC, Ahaneku JE. Evaluation of blood pressure and indices of obesity in a typical rural community in eastern Nigeria. Ann Afr Med. 2011;10:120–6.
Adebayo RA, Balogun MO, Adedoyin RA, Obashoro-John OA, Bisiriyu LA, Abiodun OO. Prevalence of hypertension in three rural communities of Ife North Local Government Area of Osun State, South West Nigeria. Int J Gen Med. 2013;6:863–8.
Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009;27:963–75.
Kayima J, Wanyenze RK, Katamba A, Leontsini E, Nuwaha F. Hypertension awareness, treatment and control in Africa: a systematic review. BMC Cardiovasc Disord. 2013;13:54.
World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks [Internet]. World Health Organization; 2009. https://apps.who.int/iris/handle/10665/44203. Accessed 6 Mar 2023.
Acknowledgements
The author acknowledges the contribution of the community and church leaders during the study.
Author information
Authors and Affiliations
Contributions
Birinus A Ezeala-Adikaibe conceptualized the work and wrote the manuscript. All authors contributed financially for the study and physically collected data and examined the participants. All the authors also revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ezeala-Adikaibe, B.A., Mbadiwe, C.N., Okafor, U.H. et al. Prevalence of hypertension in a rural community in southeastern Nigeria; an opportunity for early intervention. J Hum Hypertens 37, 694–700 (2023). https://doi.org/10.1038/s41371-023-00833-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-023-00833-x
- Springer Nature Limited
This article is cited by
-
Hypertension in sub-Saharan Africa: the current profile, recent advances, gaps, and priorities
Journal of Human Hypertension (2024)
-
Journal of Human Hypertension special issue on sex and gender differences in hypertension
Journal of Human Hypertension (2023)