Abstract
Arterial stiffness is an independent cardiovascular risk factor. However, the association between sodium/potassium intake and arterial stiffness in the Chinese population is unclear. Therefore, we performed a large, community-based cross-sectional study to reach a more definitive conclusion. The study was conducted at the Third Xiangya Hospital in Changsha between August 2017 and September 2019. Urinary sodium, potassium, and creatinine levels were tested from spot urine samples during physical examinations of each recruited participant. The 24-hour estimated urinary sodium excretion (eUNaE) and estimated urinary potassium excretion (eUKE) levels were calculated using the Kawasaki formula (used as a surrogate for intake). The brachial-ankle pulse wave velocity (baPWV) and ankle brachial index (ABI) were measured using an automatic waveform analyzer. In 22,557 subjects with an average age of 49.3 ± 10.3 years, the relationships of the ABI and baPWV with the levels of eUNaE, eUKE and the ratio of sodium to potassium (Na/K ratio) were analyzed. A significant negative relationship was found between the eUKE and baPWV levels (β = 2.41, p < 0.01), whereas the Na/K ratio was positively associated with baPWV (β = 2.46, p < 0.01), especially in the overweight and hypertensive populations (both pinteraction = 0.04). The association of eUNaE quartiles with baPWV presented a J-shaped curve after adjusting for confounders. In addition, a positive association was observed between the Na/K ratio and the ABI (β = 0.002, p < 0.01). In this study, high potassium and/or low sodium intake was further confirmed to be related to vascular stiffness in Chinese individuals.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide. Arterial stiffness has been identified as an independent CVD risk factor and a predictor of all-cause mortality [1]. Previous studies have demonstrated that arterial stiffness is involved in the pathology of many diseases, including vascular calcification, heart failure, atherosclerosis, and ultimately CVD [2, 3]. Furthermore, studies consistently demonstrate that changes in arterial stiffness occur in advance of CVD [4]. Thus, assessments of arterial stiffness are useful for detecting, predicting, and eventually preventing CVD [5].
Arterial stiffness can be measured by several noninvasive methods, of which the measurement of pulse wave velocity (PWV) is the most common [6]. PWV represents the speed of the pressure wave propagating along the artery and is directly correlated to the rigidity of the vessel with a higher velocity indicating increased vessel stiffness [7, 8]. Different measurement techniques focus on the carotid-femoral pulse wave velocity (cfPWV), brachial-ankle pulse wave velocity (baPWV), and segment-specific PWVs [9]. Recently, baPWV, which reflects the stiffness of both the central conduit and the peripheral arteries, has been used more frequently than other measurements [10]. An individual participant data meta-analysis showed that measuring baPWV is more effective at predicting the risk of CVD than measuring the Framingham risk score [11]. Moreover, peripheral arterial disease (PAD) can be diagnosed simply, accurately and noninvasively by ankle/brachial index (ABI) measurement [12]. The ABI is calculated by dividing the systolic pressure of each of the ankles by the highest brachial pressure of either arm [13]. A high ABI is an important indicator of a high risk of cardiovascular events in individuals who have been diagnosed with PAD [14, 15].
Dietary intervention helps prevent arterial stiffness [16]. A meta-analysis including 14 cohorts showed that an 89.3 mmol/day decrease in average sodium intake was associated with a 2.84% (95% CI: 0.51–5.08) reduction in PWV [17]. Potassium intake also plays a role in cardiovascular health. A low-sodium and high-potassium Mediterranean diet has been shown to be an effective model for preventing arterial stiffness in older adults[18]. The Korean Multi-Rural Communities Cohort study found that baPWV may be positively associated with dietary sodium intake and the ratio of sodium to potassium (Na/K ratio) in adults over 40 years old [19]. However, the effects of sodium and potassium on arterial stiffness are inconsistent with other studies. For example, Zhang’s study indicated a negative relationship between 24 h urinary sodium excretion and PWV in a Chinese population [20], and another study indicated that sodium or potassium intake presented a J-shaped curve relationship to arterial stiffness [21]. In China, the average sodium intake is approximately double the recommended maximum limit, and the potassium intake is less than half the recommended level [22, 23]. We reported a similar result in our previous study [24]. It is uncertain whether there is a relationship exist between sodium and potassium intake levels and arterial stiffness in Chinese individuals with a high sodium and low potassium intake level. Therefore, we used an institution-based cross-sectional study to evaluate the associations of the ABI and baPWV with estimated urinary sodium excretion (eUNaE), estimated urinary potassium excretion (eUKE), and their ratio (Na/K ratio) in a health check-up population based on data from the Third Xiangya Hospital located in Changsha, China.
Methods
Study design and population
The cross-sectional study population comprised more than 20,000 individuals from a mixed urban and rural area who visited the health management center at the Third Xiangya Hospital in Changsha between August 2017 and September 2019. In addition to the physical and laboratory examination, personal details (health-related habits, family history, and self-reported disease history) were obtained from the National Physical Examination Questionnaire [24, 25]. Participants with missing values for age, blood pressure, weight, height, eUNaE, or eUKE were excluded. Additionally, those aged <18 or >80 years old or with systolic blood pressure (SBP) < 70 mmHg or >260 mmHg, diastolic blood pressure (DBP) < 40 mmHg or >140 mmHg, eUNaE >12 g/day or eUKE >4 g/day, or baPWV >40 m/s were removed from the analysis.
Informed consent and the protocol of the overall physical examination were reviewed and approved by the institutional review board at the Third Xiangya Hospital (No. 2018-S393). The study was approved by an independent ethics committee at the Third Xiangya Hospital, and all the participants provided written informed consent according to the general recommendations of the Declaration of Helsinki.
Measurement of baPWV and ABI
As previously reported [26], the participants’ baPWV and ABI were measured in a quiet, temperature-controlled room. After the participants rested for a minimum of 5 min in the supine position, an automatic waveform analyzer (BP-203 RPE III, Omron Health Medical, Dalian, China) was used to measure the ABI and baPWV simultaneously. The cuffs were wrapped around the extremities (upper arm and ankle) and then connected to the plethysmography sensor (volume pulse form) and the oscillometric pressure sensor. Pressure waveforms were recorded at both the brachial and tibial arteries to assess the transmission time between the initial increases in these waves. The measurements were performed twice, and the average values of the left- and right-side assessments were calculated. The ABI was calculated by dividing the ankle SBP by the highest brachial SBP of either arm [13]. According to a previous study, lower ABI values from both sides were used [27]. Given that this study enrolled a health check-up population, there were only six people with an ABI > 1.40. Thus, in the current study, the ABI was categorized into three ranges: ABI ≤ 0.90 (abnormal ABI), 0.91 ABI 0.99 (borderline ABI), and 1.00 ABI 1.40 (normal ABI) [28].
Physical examination and laboratory measurements
As previously reported [29], we used the Kawasaki formulas to estimate 24-hour urinary sodium and potassium excretion from spot urine samples. These estimates were used as surrogates for intake in the current study. The midstream urine of the subjects was collected in labeled containers. After the collection was completed, each sample was quickly sent to the clinical laboratory department to detect the sodium and potassium contents within 2 hours using the ion-selective electrode method (Beijing LEADMAN Biochemical Co., Ltd., China). The methods of physical examination, as well as the definitions of hypertension, hyperlipidemia, diabetes, and cardiovascular disease, were also detailed in our previous study [29].
Statistical analyses
All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, North Carolina, USA). Continuous variables are shown as the means ± standard deviation (SD), and categorical variables are reported as percentages (%) and numbers (n). Multivariable linear regressions were performed to evaluate the changes and their 95% confidence intervals (CIs) for baPWV and ABI by the levels of eUNaE, eUKE and the Na/K ratio. The association of baPWV and ABI with the eUNaE, eUKE levels and the Na/K ratio in quartile subgroups were also performed. Potential covariates were adjusted for age, sex, body mass index (BMI), smoking, alcohol use, and the presence of hypertension, diabetes mellitus, dyslipidemia and cardiovascular disease. In addition, given that the Na/K ratio is associated with blood pressure rather than the PWV value [30], we adjusted SBP and antihypertensive drugs and creatinine instead of hypertension in model 4. In assessing the associations of the Na/K ratio with baPWV and ABI, the influence of participant sex (female or male), age (<45 years, 44-55 years and ≥45 years), body mass index (BMI) (<18.5 kg/m2, 18.5-23.9 kg/m2, ≥24 kg/m2), and hypertension status (yes or no) were investigated using interaction tests adjusted for the abovementioned covariates. All the p values were two-tailed.
Results
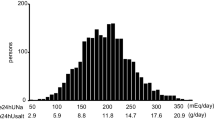
A total of 22,606 subjects enrolled in physical examinations, which included assessment with an automatic waveform analyzer, between August 2017 and September 2019. Based on the baPWV and ABI measurements, one subject was excluded because his baPWV was >40 m/s. Furthermore, we excluded 48 subjects based on their eUNaE and eUKE levels. Among these subjects, 13 had eUNaE levels >12 g/day, and 35 had eUKE levels >4 g/day. Ultimately, 22,557 subjects were included in the analyses (Fig. 1).
Table 1 lists the characteristics according to the quartile of the Na/K ratio. The mean age of the participants was 49.3 ± 10.3 years old, and 62.6% (n = 14,130) were male. A total of 26.8% of the participants were diagnosed with hypertension, 9.1% with diabetes mellitus, 41.7% with dyslipidemia, and 1.1% with cardiovascular disease. In total, 37.9% of the individuals were self-reported current smokers, and 38.4% of the individuals were self-reported current alcohol users. Univariate analysis revealed significant positive associations between the urinary Na/K ratio quartiles and age, BMI, SBP, DBP, waist circumference (WC), fasting serum glucose (FSB), low-density lipoprotein cholesterol (LDL-C), baPWV, ankle SBP, brachial SBP and ABI (all ptrend < 0.01). In addition, a significant positive association was found between urinary Na/K ratio quartiles and high-density lipoprotein cholesterol (HDL-C) levels (ptrend = 0.007). The percentage of hypertension (ptrend < 0.01) was significantly positively related to the urinary Na/K ratio quartile, while the percentages of current smokers (ptrend < 0.01) and dyslipidemia (ptrend = 0.006) were significantly negatively related to the urinary Na/K ratio quartile.
We used a multivariate linear regression model to analyze the associations of baPWV and ABI with the levels of eUNaE, eUKE and the Na/K ratio. The results are shown in Table 2. We found that the eUKE level was negatively associated with baPWV (β = –17.25, p < 0.01 and β = –17.84, p < 0.01 in models 3 and 4, respectively) and that the Na/K ratio was positively associated with baPWV (β = 2.41, p < 0.01 and β = 2.43, p < 0.01 in models 3 and 4, respectively). No significant relationship was found between the levels of eUNaE and baPWV. A positive association of ankle SBP with an increase in the eUNaE level was observed after adjusting for age, sex, BMI, smoking status, and alcohol use (β = 1.06, p < 0.01). A similar result was also observed for the eUNaE level and brachial SBP (β = 0.66, p < 0.01). In addition, the eUKE level was negatively associated with ankle and brachial SBP (β = –1.98, p < 0.01, β = –1.51, p < 0.01, respectively), and the Na/K ratio was positively associated with ankle and brachial SBP (β = 0.71, p < 0.01, β = 0.40, p < 0.01, respectively). Furthermore, among the ABI ≤ 0.9 population, the eUNaE level was positively correlated with the ABI (both β = 0.006, p = 0.04 in models 3 and 4). We also found that the eUKE level was negatively correlated with the ABI (β = –0.002, p = 0.003, β = –0.002, p = 0.01, in models 3 and 4, respectively), while the eUNaE level (both β = 0.001, p < 0.01 in models 3 and 4) and the Na/K ratio (both β = 0.001, p < 0.01 in models 3 and 4) were positively correlated with the ABI in the normal group.
Figure 2 illustrates the association of baPWV and ABI with the levels of eUNaE, eUKE and the Na/K ratio in quartile individuals after adjusting for confounding factors. As shown in Fig. 2A–C, associations of the eUNaE level with baPWV presented a J-shaped curve (β = –0.91, ptrend = 0.49). In addition, a dose-response trend in baPWV was observed with a decrease in the eUKE level (β = –11.46, ptrend < 0.0001). A positive dose-response trend in baPWV was observed for the Na/K ratio (β = 7.04, ptrend < 0.0001). Additionally, no significance was observed between the ABI and the eUKE level (β = 0.00, ptrend = 0.73) (Fig. 2E). Figure 2D and F illustrates the obvious dose-response trend in the ABI with an increase in the eUNaE level and Na/K ratio (both β = 0.03, ptrend < 0.0001).
A The associations of eUNaE with baPWV in quartile eUNaE subgroups. Q1: β = −18.87, p < 0.01; Q2: β = −11.37, p = 0.04; Q3: β = 1.76, p = 0.89; Q4: β = 2.78, p = 0.41. B The associations of eUKE with baPWV in quartile eUKE subgroups. Q1: β = 15.66, p = 0.08; Q2: β = 5.81, p = 0.85; Q3: β = –65.75, p = 0.03; Q4: β = −4.271, p = 0.64. C The relationship of the Na/K ratio with the baPWV in quartile Na/K ratio subgroups. Q1: β = −28.60, p = 0.06; Q2: β = 19.06, p = 0.45; Q3: β = 67.34, p < 0.01; Q4: β = –2.53, p = 0.06. D The associations of eUNaE with ABI in quartile eUNaE subgroups. Q1: β = 0.003, p = 0.16; Q2: β = 0.09, p = 0.08; Q3: β = –0.003, p = 0.51; Q4: β = 0.000, p = 0.84. E The associations of eUKE with ABI in quartile eUKE subgroups. Q1: β = −0.009, p < 0.01; Q2: β = 0.006, p = 0.61; Q3: β = 0.021, p = 0.07; Q4: β = 0.003, p = 0.41. F The associations of the Na/K ratio with the ABI in quartile eUNaE subgroups. Q1: β = 0.004, p = 0.44; Q2: β = –0.001, p = 0.904; Q3: β = 0.010, p = 0.21; Q4: β = 0.001, p = 0.01. Note: baPWV, brachial-ankle pulse wave velocity; ABI, ankle brachial index; Na/K ratio, ratio of estimated urinary sodium excretion to potassium excretion; eUNaE, estimated urinary sodium excretion; and eUKE, estimated urinary potassium excretion. Adjusted by age, sex, body mass index, alcohol and smoking status, hypertension, diabetes mellitus, dyslipidemia and cardiovascular disease.
Figure 3 illustrates the forest plots of changes in the baPWV and ABI per unit increase in the Na/K ratio across various subgroups. The positive association of the Na/K ratio with baPWV was more significant in the overweight population (increment of 4.282 cm/s, 95% CI: 1.935 to 6.612) than in the normal weight (increment of –0.426 cm/s, 95% CI: –3.114 to 2.261) and underweight populations (increment of 3.148 cm/s, 95% CI: –10.740 to 17.035, pinteraction = 0.04). Moreover, the positive association of the Na/K ratio with baPWV was more significant in hypertensive patients (increment of 5.347 cm/s, 95% CI: 1.115–9.579) than in the normal population (increment of 1.158 cm/s, 95% CI: –0.599 to 2.915, pinteraction = 0.04). No significant differences in the associations between the Na/K ratio and baPWV were noted between the subgroups by age and sex (all pinteraction > 0.05). In addition, no significant differences were found in the associations between the Na/K ratio and the ABI between the subgroups by sex, age, BMI and hypertensive status (all pinteraction > 0.05).
A The associations of the Na/K ratio with baPWV in certain subgroups. B The associations of the Na/K ratio with the ABI in certain subgroups. Note: baPWV brachial-ankle pulse wave velocity; ABI ankle brachial index; Na/K ratio, ratio of estimated urinary sodium excretion to potassium excretion. Adjusted by age, sex, body mass index, alcohol and smoking status, hypertension, diabetes mellitus, dyslipidemia and cardiovascular disease.
Discussion
In this large cross-sectional study, we investigated the association between urinary sodium and/or potassium excretion and baPWV and ABI in Chinese individuals. Overall, our study further confirmed that the intake of sodium and potassium were associated with arterial stiffness after adjusting for confounding factors, and this association was more significant in overweight and hypertensive populations.
Arterial stiffness is recognized as a major contributor to mortality and survival in cardiovascular events [17, 31]. Previous studies have indicated that the association between the eUNaE level and CVD events was J-shaped among high-risk populations [32] or the general population [33]. In the current study, we found that associations of the eUNaE level (which was used as a surrogate for intake) with baPWV presented a J-shaped curve. This result was similar to that noted in other studies [20, 21] and may provide clues for the J-shaped association of salt intake with CVD events [32, 33]. However, the mean eUNaE level in the current study was lower than that in Zhang’s and PURE-China’s studies [20, 33]. Thus, further studies are needed to verify the J-shaped association and “safe” zone of sodium intake. As mentioned before, a meta-analysis demonstrated that the average sodium intake was reduced by 89.3 mmol/day and that baPWV was reduced by 2.84% [17]. In contrast, Zhang’s study indicated that the eUNaE level was negatively associated with baPWV (β = –21.48, p = 0.005). Our study’s results indicated that no significant trend was found between the eUNaE level and baPWV, whereas a negative association was found in the lowest eUNaE group. We hypothesized that the observed deviation might be primarily attributed to sampling bias, measurement of surrogates for sodium and potassium intake, average amount of sodium and potassium intake, and status of blood pressure. Furthermore, previous studies indicated no significant decreasing or increasing trend between sodium intake and arterial stiffness among normotensive individuals [17, 34], and other studies confirmed that sodium intake leads to a greater increase in arterial stiffness in a male subgroup [35]. Since the Na/K ratio is related to baPWV in the entire population, we analyzed the associations of the Na/K ratio with baPWV in different subgroups.
Moreover, we found that the eUKE level was negatively correlated with baPWV in the current study, which is consistent with previous studies [36, 37]. In addition, a positive dose-response trend in baPWV was observed for the Na/K ratio. Because the involvement of eUNaE in baPWV was nearly null, the positive relationship between baPWV and the Na/K ratio may be mainly attributed to a decrease in eUKE. In addition, a significant association between the Na/K ratio or eUKE and baPWV was unaffected by adjustment for blood pressure, suggesting that mechanisms other than blood-pressure effects may play a role. Sun’s study illustrated a causative link between reduced dietary potassium and arterial stiffness and uncovered the underlying mechanisms that integrate enhanced intracellular calcium influx, activated CREB signaling, and elevation of autophagy [38]. However, no direct association was observed between Na/K and baPWV after adjusting for blood pressure in Tabara’s study [30]. Thus, more studies are still needed to reveal the true relationship between dietary potassium and arterial stiffness in the future.
Furthermore, we found that the association of the Na/K ratio with arterial stiffness was more significant in the hypertensive and overweight populations. In 2019, Michelle et al. first indicated that the urinary Na/K ratio was associated with cfPWV in diabetic hypertensive patients [39]. The PURE study showed that the association between the Na/K ratio and CVD events was only significant in patients with hypertension [33]. We hypothesized that a high urinary Na/K ratio or a low eUKE excretion level may increase susceptibility to accelerated arterial stiffness in the hypertensive population. A previous study [40] found that the association between the urinary Na/K ratio and carotid atherosclerosis tended to be more significant in normal-weight individuals, which was inconsistent with the current study. Both sodium and potassium closely interact and greatly influence the process of essential cellular functions and mortality [41, 42]. Thus, whether the combined effect of sodium and potassium is different in certain populations still requires further research.
A positive association was found between eUNaE and ankle or brachial SBP. Moreover, a high eUNaE level had a higher ABI (1.0–1.4) in the current study, which was similar to that noted in Hu’s study [12]. In addition, a negative association was noted between the eUKE level and the ABI. Research on the relationship between the ABI and the eUKE level is rarely reported. Using the ApoE-deficient mouse model, Yong Sun found that increased dietary potassium (2.1%) attenuated vascular calcification and aortic stiffness. Researchers believe that a low potassium concentration activates a cAMP response element-binding protein signal that subsequently enhances autophagy and promotes vascular smooth muscle cell calcification [38]. Moreover, we found a positive association of the Na/K ratio with the ABI (1.0-1.4). For the first time, at least to our knowledge, a direct correlation was observed between the ABI and the Na/K ratio in the general population. We also analyzed the associations between the Na/K ratio and the ABI between the subgroups by sex, age, BMI and hypertensive status. Unfortunately, no significant relationship was found in our study. More studies on the effect of sodium or potassium intake on ABI are needed.
Our study has several limitations. First, we did not use the gold standard 24-hour urine test to evaluate sodium and potassium intake. In He’s study, they compared estimated sodium intake with that measured by the gold-standard method of multiple nonconsecutive 24-h urine collections and assessed their relationship with mortality. The results indicated that 24-h urine collection measured sodium intake showed a linear relationship with mortality, while the average estimated sodium appeared to show a J-shaped relationship with mortality. They concluded that the average estimated sodium was systematically biased, with overestimation at lower levels and underestimation at higher levels [43]. Thus, the truly relationship between sodium intake and arterial stiffness still need furether study. Second, we had only one institution in which physical examinations were performed in Changsha. Hence, our results may not be generalizable to China. Third, some confounding factors, such as physical activity, were not completely adjusted, which might mask or attenuate the true associations. Finally, due to the nature of a cross-sectional study, we were unable to determine any causal relationship between arterial stiffness and the urinary Na/K ratio. The exact causal relationship between the urinary Na/K ratio and arterial stiffness requires further verification.
Conclusion
Our study further confirmed that a lower sodium and/or increased potassium intake was associated with arterial stiffness, especially in overweight and hypertensive populations in the Chinese population. The relationship of sodium intake with baPWV resembles a J-shaped curve, which is similar to what has been proposed in the case of cardiovascular mortality. Prospective cohort studies or randomized clinical trials with large numbers of subjects are needed to confirm the observed relationship.
Summary
What is known about topic
-
Arterial stiffness is an independent cardiovascular risk factor.
-
Arterial stiffness is associated with the intake of sodium and potassium.
-
The effects of sodium and potassium intake on arterial stiffness may be inconsistent among various population.
What this study adds
-
The association of eUNaE quartiles with baPWV presents a J-shaped curve after adjusting for confounders.
-
A significant negative relationship is found between the eUKE and baPWV levels, whereas the Na/K ratio is positively associated with baPWV, especially in the overweight and hypertensive populations.
-
The positive association of the Na/K ratio with the ABI is observed for the first time in the current study.
Data availability
The dataset and code supporting the conclusions of this article are available upon reasonable request from the authors.
References
Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;37:1236–41.
Mitchell GF, Powell JT. Arteriosclerosis: a primer for “in focus” reviews on arterial stiffness. ATVB. 2020;40:1025–7.
Chirinos JA, Segers P, Hughes T, Townsend R. Large-artery stiffness in health and disease: JACC state-of-the-art review. J Am Coll Cardiol. 2019;74:1237–63.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–219. 2013
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–605.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, et al. Abridged version of the expert consensus document on arterial stiffness☆. ARTRES. 2007;1:2.
Schellinger IN, Mattern K, Raaz U. The Hardest Part. Arterioscler Thromb Vasc Biol. 2019;39:1301–6.
Munakata M. Brachial-Ankle pulse wave velocity: background, method, and clinical evidence. Pulse (Basel). 2016;3:195–204.
Baier D, Teren A, Wirkner K, Loeffler M, Scholz M. Parameters of pulse wave velocity: determinants and reference values assessed in the population-based study LIFE-Adult. Clin Res Cardiol. 2018;107:1050–61.
Tomiyama H, Shiina K. State of the art review: Brachial-Ankle PWV. J Atheroscler Thromb. 2020;27:621–36.
Ohkuma T, Ninomiya T, Tomiyama H, Kario K, Hoshide S, Kita Y, et al. Brachial-Ankle Pulse Wave Velocity and the Risk Prediction of Cardiovascular Disease: An Individual Participant Data Meta-Analysis. Hypertension. 2017;69:1045–52.
Hu B-C, Li Y, Liu M, Sheng C-S, Wang J-G. Ankle-brachial index in relation to the natriuretic peptide system polymorphisms and urinary sodium excretion in Chinese. Atherosclerosis. 2013;230:86–91.
Giugliano G, Sannino A, Brevetti L, Perrino C, Schiattarella GG, Franzone A, et al. Ankle/brachial index to everyone. BMC Surg. 2012;12:S18. Suppl 1
Golledge J, Moxon JV, Rowbotham S, Pinchbeck J, Quigley F, Jenkins J. High ankle brachial index predicts high risk of cardiovascular events amongst people with peripheral artery disease. PLoS One. 2020;15:e0242228.
Resnick HE, Lindsay RS, McDermott MM, Devereux RB, Jones KL, Fabsitz RR, et al. Relationship of high and low ankle brachial index to all-cause and cardiovascular disease mortality: the Strong Heart Study. Circulation 2004;109:733–9.
Blanch N, Clifton PM, Keogh JB. Postprandial effects of potassium supplementation on vascular function and blood pressure: a randomised cross-over study. Nutr Metab Cardiovasc Dis. 2014;24:148–54.
D’Elia L, Galletti F, La Fata E, Sabino P, Strazzullo P. Effect of dietary sodium restriction on arterial stiffness: systematic review and meta-analysis of the randomized controlled trials. J Hypertens. 2018;36:734–43.
Jennings A, Berendsen AM, de Groot LCPGM, Feskens EJM, Brzozowska A, Sicinska E, et al. Mediterranean-style diet improves systolic blood pressure and arterial stiffness in older adults. Hypertension. 2019;73:578–86.
Jung S, Kim MK, Shin J, Choi BY, Lee Y-H, Shin DH, et al. High sodium intake and sodium to potassium ratio may be linked to subsequent increase in vascular damage in adults aged 40 years and older: the Korean multi-rural communities cohort (MRCohort). Eur J Nutr. 2019;58:1659–71.
Zhang Z, Liao H, Zhang X, Meng Q, Shi R, Feng J, et al. Associations of urinary sodium excretion with central hemodynamics and changes in vascular structure and function at high altitude. J Clin Hypertens (Greenwich). 2021;23:1907–14.
García-Ortiz L, Recio-Rodríguez JI, Rodríguez-Sánchez E, Patino-Alonso MC, Agudo-Conde C, Rodríguez-Martín C, et al. Sodium and potassium intake present a J-shaped relationship with arterial stiffness and carotid intima-media thickness. Atherosclerosis. 2012;225:497–503.
Tan M, He FJ, Wang C, MacGregor GA. TwEnty-four-hour Urinary Sodium And Potassium Excretion In China: A Systematic Review And Meta-analysis. J Am Heart Assoc. 2019;8:e012923.
Sun N, Mu J, Li Y. Working Committee of Salt evaluation, Blood Pressure Management, Chinese Medical Association Hypertension Professional Committee, Hypertension Group, Chinese Society of Cardiology. An expert recommendation on salt intake and blood pressure management in Chinese patients with hypertension: A statement of the Chinese Medical Association Hypertension Professional Committee. J Clin Hypertens (Greenwich). 2019;21:446–50.
Yang P, Chen Z, Yin L, Peng Y, Li X, Cao X, et al. Salt intake assessed by spot urine on physical examination in Hunan, China. Asia Pac J Clin Nutr. 2019;28:845–56.
Li Y, Yin L, Peng Y, Liu X, Cao X, Wang Y, et al. The association of blood pressure with estimated urinary sodium, potassium excretion and their ratio in hypertensive, normotensive, and hypotensive Chinese adults. Asia Pac J Clin Nutr. 2020;29:101–9.
Lu Y, Pechlaner R, Cai J, Yuan H, Huang Z, Yang G, et al. Trajectories of Age-Related Arterial Stiffness in Chinese Men and Women. J Am Coll Cardiol. 2020;75:870–80.
Diehm C, Allenberg JR, Pittrow D, Mahn M, Tepohl G, Haberl RL, et al. German Epidemiological Trial on Ankle Brachial Index Study Group. Mortality and vascular morbidity in older adults with asymptomatic versus symptomatic peripheral artery disease. Circulation. 2009;120:2053–61.
Natsuaki C, Inoguchi T, Maeda Y, Yamada T, Sasaki S, Sonoda N, et al. Association of borderline ankle-brachial index with mortality and the incidence of peripheral artery disease in diabetic patients. Atherosclerosis 2014;234:360–5.
Peng S, Wang J, Xiao Y, Yin L, Peng Y, Yang L, et al. The association of carotid artery atherosclerosis with the estimated excretion levels of urinary sodium and potassium and their ratio in Chinese adults. Nutr J. 2021;20:50.
Tabara Y, Takahashi Y, Kumagai K, Setoh K, Kawaguchi T, Takahashi M, et al. Descriptive epidemiology of spot urine sodium-to-potassium ratio clarified close relationship with blood pressure level: the Nagahama study. J Hypertens. 2015;33:2407–13.
Andrus EC, Allen EV, Merritt HH, Duff GL, Moore RA, Kendall FE, et al. The pathogenesis of arteriosclerosis. Int J Epidemiol. 2015;44:1791–3.
O’Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011;306:2229–38.
O’Donnell M, Mente A, Rangarajan S, McQueen MJ, Wang X, Liu L, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371:612–23.
Todd AS, Macginley RJ, Schollum JBW, Williams SM, Sutherland WHF, Mann JI, et al. Dietary sodium loading in normotensive healthy volunteers does not increase arterial vascular reactivity or blood pressure. Nephrol (Carlton). 2012;17:249–56.
Lennon-Edwards S, Ramick MG, Matthews EL, Brian MS, Farquhar WB, Edwards DG. Salt loading has a more deleterious effect on flow-mediated dilation in salt-resistant men than women. Nutr Metab Cardiovasc Dis. 2014;24:990–5.
Polónia J, Maldonado J, Ramos R, Bertoquini S, Duro M, Almeida C, et al. Estimation of salt intake by urinary sodium excretion in a Portuguese adult population and its relationship to arterial stiffness. Rev Port Cardiol. 2006;25:801–17.
Lennon-Edwards S, Allman BR, Schellhardt TA, Ferreira CR, Farquhar WB, Edwards DG. Lower potassium intake is associated with increased wave reflection in young healthy adults. Nutr J. 2014;13:39.
Sun Y, Byon CH, Yang Y, Bradley WE, Dell’Italia LJ, Sanders PW, et al. Dietary potassium regulates vascular calcification and arterial stiffness. JCI Insight. 2017;2:e94920.
Cunha MR, Cunha AR, Marques BCAA, Mattos SS, D’El-Rei J, França NM, et al. Association of urinary sodium/potassium ratio with structural and functional vascular changes in non-diabetic hypertensive patients. J Clin Hypertens (Greenwich). 2019;21:1360–9.
Dai XW, Wang C, Xu Y, Guan K, Su YX, Chen YM. Urinary Sodium and Potassium Excretion and Carotid Atherosclerosis in Chinese Men and Women. Nutrients. 2016;8:612.
Yang Q, Liu T, Kuklina EV, Flanders WD, Hong Y, Gillespie C, et al. Sodium and potassium intake and mortality among US adults: prospective data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2011;171:1183–91.
Castro H, Raij L. Potassium in hypertension and cardiovascular disease. Semin Nephrol. 2013;33:277–89.
He FJ, Campbell NRC, Ma Y, MacGregor GA, Cogswell ME, Cook NR. Errors in estimating usual sodium intake by the Kawasaki formula alter its relationship with mortality: implications for public health. Int J Epidemiol. 2018;47:1784–95.
Acknowledgements
We gratefully acknowledge the voluntary participation of all the study subjects. This work was supported by funding from the National Science Foundation of China (81973324, 81872685, and 82003537), the Hunan Young Talent grant (2020RC3063), the Hunan Science Foundation (2020JJ5858, 2020JJ4439) and the Wisdom Accumulation and Talent Cultivation Project of the Third XiangYa Hospital of Central South University (YX202002).
Author information
Authors and Affiliations
Contributions
QY, WH, Lu Yin, YM, and Xin Huang produced data for analysis. QY, WH, Lin Yang and YL wrote the manuscript. YL designed the study. CK, LJ, PT, and Xiao Hui included patients for the study. All authors reviewed and edited the manuscript. YL and Xin Huang handled funding and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, Q., Jiang, W., He, Y. et al. The association of arterial stiffness with estimated excretion levels of urinary sodium and potassium and their ratio in Chinese adults. J Hum Hypertens 37, 292–299 (2023). https://doi.org/10.1038/s41371-022-00671-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-022-00671-3
- Springer Nature Limited