Abstract
Reliable assessments of reduced exercise capacity based on resting tests are one of the major challenges in clinical practice. The aim of this study was to evaluate the relationship between hemodynamic parameters obtained via resting tests (echocardiography and impedance cardiography (ICG)) and objective parameters of exercise capacity assessed via cardiopulmonary exercise testing and exercise ICG in patients with controlled arterial hypertension (AH). The left ventricular ejection fraction (LVEF), global longitudinal strain (GLS), diastolic function parameters (e′, E/A, E/e′), cardiac output (CO), stroke volume (SV), and systemic vascular resistance index were evaluated for any correlations with selected parameters of exercise capacity, such as peak oxygen uptake (VO2) and peak CO in 93 people with AH (mean age 54 years, 47 women). Statistically relevant correlations occurred between indices of exercise capacity (peak VO2; peak CO) and only the following hemodynamic parameters: diastolic blood pressure (R = 0.23, p = 0.026; R = 0.24, p = 0.021; respectively), e′ (R = 0.32, p = 0.002; R = 0.24, p = 0.027), E/e′ (R = 0.35, p < 0.001; ns), E/A (R = 0.23, p = 0.030; R = 0.21, p = 0.047), SV at rest (ns; R = 0.24, p = 0.019), and CO at rest (ns; R = 0.21, borderline p = 0.052). No significant correlations between the exercise capacity parameters and either LVEF or GLS were observed. No hemodynamic parameter proved to be an independent correlate of either peak VO2 or peak CO. The association between hemodynamic parameters at rest and parameters of exercise capacity was weak and limited to selected parameters of diastolic function. Exercise capacity assessment in patients with AH based on resting tests alone is insufficiently reliable and should be supplemented with exercise tests.
Similar content being viewed by others
Introduction
An individual’s functional capacity reflects the ability to perform activities of daily living based on aerobic metabolism, whose measurable parameter is called maximum oxygen consumption [1]. In clinical practice, functional capacity assessments are largely subjective, as they are based on history taking and questionnaires. In a large number of patients physical examination fails to show the cause of reported symptoms [2]. Moreover, additional investigations (such as resting echocardiography, resting electrocardiography, and serum N-terminal pro-B-type natriuretic peptide (NTproBNP) levels) recommended in heart failure (HF) diagnostics [3] often show no marked abnormalities. Therefore, being able to distinguish between a merely subjective impression of diminished functional capacity and objective cardiovascular failure based solely on resting tests constitutes a major challenge in clinical practice [3]. This issue affects a number of cardiology patients, including patients with arterial hypertension (AH), even when it is well-controlled.
The means of monitoring cardiovascular response to exercise include exercise electrocardiogram, cardiopulmonary exercise testing (CPET), echocardiography, and—recently—also a noninvasive hemodynamic assessment via impedance cardiography (ICG). These assessments may help explain the underlying cause of reduced exercise tolerance also in patients who do not meet the diagnostic criteria of HF [4,5,6,7]. Nonetheless, these assessments are difficult to perform and still not commonly accessible. Moreover, apart from CPET, there are no detailed standards for result interpretation [8]. Given these limitations of exercise testing, it seems reasonable to continue searching for new, objective markers of diminished cardiovascular capacity which could be assessed at rest.
We postulated that detailed echocardiographic assessment of systolic and diastolic left ventricular function parameters, including global longitudinal strain (GLS) and hemodynamic parameters via resting ICG, could be of diagnostic value in this respect. In patients with AH and HF, GLS is an independent prognostic factor, more sensitive in identifying impaired myocardial contractility than left ventricular ejection fraction (LVEF) [9,10,11,12].
Some previous studies also suggest that the hemodynamic profile at rest, assessed via ICG, may reflect exercise capacity [13,14,15,16].
Thus, the aim of this study was to assess the relationship between specific echocardiographic and ICG parameters at rest and certain known parameters of functional capacity in patients with AH.
Methods
Study group
It was the retrospective analysis of study group described in our previous papers [6, 16], male and female patients with AH, aged 40–75 years, were included in the study. The exclusion criteria were: confirmed secondary AH; history of ischemic heart disease; chronic kidney disease with an estimated glomerular filtration rate (eGFR) of <60 mL/min/1.73 m2 calculated using the Modification of Diet in Renal Disease Study (MDRD) formula; other severe comorbidities: LVEF < 50%; hypertrophic/dilated cardiomyopathy; clinically significant valvular disease; clinically significant arrhythmias; non-sinus rhythm (including permanent cardiac pacing); body mass index (BMI) of >40 kg/m2; previously diagnosed diabetes mellitus; polyneuropathy; exercise-limiting peripheral vascular disease and/or musculoskeletal disorders; psychiatric conditions preventing the patient’s full cooperation; history of lung disease (asthma, chronic obstructive pulmonary disease, pulmonary embolism). AH was determinated according to Mancia et al. guidelines [17].
Out of the 114 patients included in the study, 21 were excluded from analysis due to a lack of ICG or CPET or not reaching the anaerobic threshold (respiratory exchange ratio > 1.05) during testing.
The study was conducted in accordance with the principles of Good Clinical Practice and Declaration of Helsinki. The study protocol had been approved by the Institutional Review Board (approval No. 14/WIM/2014). Each patient provided a written informed consent to participate in the study. The study has been registered at ClinicalTrials.gov (NCT02634866).
Medical history and physical examination
The clinical examination included history taking of any concomitant conditions, antihypertensive therapy, and reported symptoms (especially the patients’ subjective assessment of their exercise capacity, including reduced exercise tolerance, shortness of breath, chest pain), as well as physical examination, including a thorough assessment of heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), signs of pulmonary congestion and/or edema, and body measurements (height, weight, BMI). Obesity was diagnosed according to American Heart Association guidelines [18].
Laboratory tests
Laboratory tests were conducted on fasting peripheral venous blood samples collected in the morning (07:00–08:30 a.m.). The levels of the following were evaluated: NTproBNP, creatinine, and hemoglobin (Hb). The eGFR was calculated based on the MDRD equation. The threshold values for Hb (Hb < 13 g/dL for men, Hb < 12 g/dL for women) were based on the current World Health Organization guidelines [19]. NTproBNP levels of <125 pg/mL meant that HF was excluded as the cause of impaired exercise tolerance [3].
Echocardiography
Echocardiographic examinations were conducted with Vivid S6 (GE Medical System, Wauwatosa, WI, USA), in standard parasternal, apical, and subcostal views. The size of the cardiac chamber, myocardial contractility, LVEF, and valve structure and function was assessed. Left ventricular hypertrophy was diagnosed, according to the current American Society of Echocardiography guidelines [20], based on left ventricular mass index (LVMI) (>95 g/m2 for females and >115 g/m2 for males). GLS was measured via two-dimensional speckle-tracking echocardiography, as described in our previous paper [9]. The LVEF was calculated using the Simpson method. Left ventricular diastolic dysfunction was diagnosed according to current guidelines [21]. Left ventricular filling pressure was assessed based on the mitral flow parameters (the E/A ratio, where A represents late diastolic mitral inflow velocity).
Cardiopulmonary exercise testing
All patients underwent CPET before noon (between 09:00 and 11:00 a.m.) after their morning dose of medications. Exercise testing was conducted with Ergoselect (Geratherm Respiratory GmbH; Germany) according to personalized ramp protocols (calculated to reach the target workload within 10 min). Prior to each test, the oxygen and carbon dioxide sensors and the Ergoflow flow sensor were calibrated (Geratherm Respiratory GmbH; Germany). Subsequently, resting spirometry was performed. Exercise testing was discontinued in any patient who developed symptoms (dyspnea, fatigue) or requested it to be stopped [22]. Respiratory gas exchange was measured via breath-by-breath analysis, with the use of a Geratherm Ergostik system (Geratherm Respiratory GmbH; Germany). Oxygen consumption (VO2) was continuously monitored throughout the test, measured at peak exercise (peak VO2), and the value presented as a percentage of the relevant predicted value. Peak VO2 was expressed as the highest mean value over the last 30 s of exercise. The predicted VO2 value (pred VO2) was estimated with the use of Wasserman’s equation [8]. After CPET was completed, the anaerobic threshold was determined noninvasively with the V-slope method [8]. Peak VO2 < 80% of the predicted value was considered abnormal [23].
Impedance cardiography (ICG) at rest
ICG parameters at rest were measured with a Niccomo™ monitor (Medis, Ilmenau, Germany) after 10 min of resting in a supine position prior to CPET. This device operates based on measuring the thoracic base impedance (Z0). Blood volume variations produce changes in electrical impedance, as blood conducts electricity better than other tissues. The final analysis involved the mean values of such hemodynamic parameters as: stroke volume (SV); cardiac output (CO); acceleration index (ACI), which is representative of the maximum change in aortic blood flow; velocity index (VI), which depends on cardiac preload and is representative of maximum aortic blood flow; Heather index (HI), which correlates well with myocardial contractility; and systemic vascular resistance index (SVRI), which depends on mean blood pressure, central venous pressure, and cardiac index.
Impedance cardiography (ICG) during exercise
ICG parameters during exercise were measured with a PhysioFlow device (Manatec, Paris, France) during CPET, according to the protocol described elsewhere [24]. Measuring hemodynamic parameters in ICG is based on the variations in electrical impedance caused by changes in thoracic volume during cardiac systole. This technique requires measuring neither base thoracic impedance (Z0) or blood impedance, while at the same time it analyzes changes in impedance signals, ensures advanced artifact elimination, and allows continuous (beat-to-beat) CO monitoring during exercise. With its well documented repeatability and accuracy [24], CO at peak exercise (peak CO) is the parameter of most importance in assessing exercise capacity [8]. Prior to each examination, the device was calibrated by conducting a measurement at rest, according to manufacturer’s instructions (autocalibration protocol).
Statistical analysis
The data were recorded, and the obtained results were analyzed statistically with Statistica 12.0 software (StatSoft Inc, Tulsa, OK, USA). Data distribution and normality were assessed by visual inspection and the Kolmogorov–Smirnov test. Continuous variables were presented as means ± standard deviation and categorical variables were presented as absolute and relative frequencies (percentages). The associations between peak VO2, peak CO and clinical, laboratory, echocardiographic and hemodynamic parameters were analyzed using Pearson’s/Spearman’s correlation coefficients and, for selected variables, a multiple linear regression model. Subgroup analysis was performed comparing subjects with correct exercise capacity (that achieved >80% peak VO2 of the predicted value) to subjects with reduced exercise tolerance (that achieved <80% peak VO2 of the predicted value) to identify possible resting difference related to this qualitative division. For this subgroup comparison, Student’s t/Mann–Whitney U test for continuous variables and chi-square test/Fisher’s exact test for categorical variables were used. The p value of <0.05 was considered statistically significant.
Results
Baseline characteristics
The baseline characteristics of the whole study group were presented in Table 1.
The analyzed group comprised 93 patients (47 women) at a mean age of 54 years (age range 40–71 years) with preserved LVEF (mean 64.9 ± 3.9%), generally well-controlled hypertension (mean BP 127/80 mmHg, with only 16.1% patients exhibiting a BP of >140/90 mmHg). Decreased exercise tolerance was reported by 41 patients, with dyspnea on exertion being the most common symptom (33%). Antihypertensive treatment most commonly included angiotensin-converting enzyme inhibitors (54.8%) and diuretics (46.2%). Sixty-four percent of subjects were treated with polytherapy, including five persons needing five antihypertensive medicines.
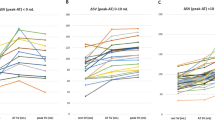
Correlations of clinical, laboratory, and hemodynamic variables at rest with peak VO2
Our analysis of any correlations between peak VO2 and clinical, laboratory, and hemodynamic parameters at rest yielded statistically significant, though only weak-to-moderate, correlations between peak VO2 and the following: age (R = −0.43, p < 0.001), DBP (R = 0.23, p = 0.026), NTproBNP (R = −0.55, p < 0.001), Hb (R = 0.33, p = 0.001), BMI (R = −0.31, p = 0.002), E/A (R = 0.23, p = 0.03), e′ (R = 0.32, p = 0.002), E/e′ (R = −0.35, p < 0.001). A linear regression model of certain variables (age, DBP, NTproBNP, Hb, BMI, E/A, e′, E/e′, HI) demonstrated Hb and NTproBNP to be the only parameters to be independently associated with peak VO2. An assessment of the possible association between peak VO2, presented as percentage of the predicted value (%pred peak VO2), and the above variables showed age to be the only one significantly associated with peak VO2 (R = 0.30; p = 0.003).
No significant correlations were observed between peak VO2 and SBP, HR (office measurement), LVMI, LVEF, GLS, LAVI, TRV (rest echocardiography), SV, or CO (ICG at rest), with only a trend toward correlation between peak VO2 and SVRI (R = 0.20, p = 0.055).
Correlations of clinical, laboratory, and hemodynamic variables at rest with peak CO
Analysis of possible associations between peak CO and the evaluated variables showed statistically significant but weak correlations between peak CO and the following: age (R = −0.30, p = 0.004), DBP (R = 0.24, p = 0.021), NTproBNP (R = −0.25, p = 0.021), Hb (R = 0.31, p = 0.003), E/A (R = 0.21, p = 0.047), e′ (R = 0.24, p = 0.027), SV at rest (R = 0.24, p = 0.019), and CO at rest (R = 0.21, borderline p = 0.052). Multivariate linear regression showed no significant correlation between peak CO and any of the other independent variables.
Comparison of the subgroups with normal and reduced peak VO2
A comparison of the subgroup with normal peak VO2 (≥80% of the predicted value, n = 51) and reduced peak VO2 (<80% of pred, n = 42) demonstrated no differences in terms of any of the evaluated parameters (variable of baseline clinical characteristics, laboratory tests, ICG, echocardiography), except age (Table 2).
Discussion
Our findings showed that the association between parameters of cardiovascular capacity and hemodynamic parameters at rest is weak, even if echocardiographic evaluation is expanded to include GLS assessment and supplemented by measuring hemodynamic parameters via resting ICG. Out of all the other evaluated clinical parameters only age, Hb, and NTproBNP levels proved to be independently associated with peak VO2. Despite the fact that these parameters were also shown to correlate with peak CO values, none of them proved to be an independent predictor for the latter variable. A comparison of the subgroups with normal and reduced peak VO2 showed them to be comparable in terms of all parameters, such as blood pressure readings, apart from age. It confirmed that resting hemodynamics failed to distinguish subjects with reduced physical tolerance.
Our findings confirm the reports from earlier studies in cardiovascular patients [10, 25,26,27], which presented a lack of association between LVEF and functional capacity assessed by peak VO2. Our study indicates a similar conclusion in terms of GLS. Although an association between resting GLS values and exercise capacity was previously reported by Tsougos et al. [5], those authors evaluated the relationship between GLS and the duration of exercise only and not peak VO2.
Despite the fact that our study showed no association between peak VO2 and left ventricular systolic function, the assessed resting parameters of diastolic function (E/A, e′, and E/e′) correlated with both peak VO2 and peak CO, albeit these correlations were weak. Somewhat more convincing are the findings of studies in patients with severely impaired left ventricular diastolic function (e.g., patients with HF or following anthracycline-based chemotherapy) which showed a stronger association between the e′ and E/e′ values and functional capacity [27, 28]. This is especially relevant in light of the evidence that the usefulness of assessing left ventricular filling (E/e′) in patients diagnosed with HF with preserved LVEF increases if exercise echocardiography is used [29].
Our study showed no significant association between hemodynamic parameters assessed with ICG at rest and either peak VO2 or hemodynamic parameters assessed with ICG during exercise. Earlier studies, including ours, gave grounds to suppose that such associations could be expected. However, it is worth noting that the methodology of those studies was different. Our previous paper [16] confirmed an association between peak VO2 and ICG during exercise, by indicating an increasing strength of correlation in the group of patients with reduced exercise tolerance. It was also the reason to choose peak VO2 < 80% of the predicted value as a discriminating parameter in the comparative analysis. Peak VO2 and its predicted value (corrected to age, sex, and body mass) are treated as equivalent to max VO2 in clinical settings [23]. Other parameters of exercise capacity might be disrupted in our group, such as, i.e., HR, which is interfered by beta blockers. To limit the potential effect of stopping exercise test on poor motivation or non-cardiovascular limitation, patients who failed to reach RER of >1.05 were excluded from analysis.
Studies by other authors demonstrated that reduced exercise capacity (a shorter distance during a 6-min walk test, 6MWT) correlated with a worse pumping function of the heart at rest and increased vascular stiffness [13, 15]. Nonetheless, the fact that 6MWT (instead of the ergospirometric parameter peak VO2, considered to be the gold standard [8, 23]) was used in those studies to assess exercise capacity limits the possibility of a direct comparison between these results and the results of our present study. Nevertheless, the beneficial effects of exercise training observed by Molisz et al. [14] in a group of healthy females aged 50–70 years, in the form of improved left ventricular pumping function and lower afterload, encourage further studies of these complex associations.
The laboratory results obtained in our study also warrant at least a brief comment. We observed a weak reverse correlation between NTproBNP levels and both peak VO2 and peak CO values, despite the fact that in most patients the NTproBNP levels were below the threshold for HF diagnosis. In patients with AH such correlation may be due to increasing hemodynamic abnormalities in the form of hypertrophy and diastolic dysfunction of the left ventricle, which precede the development of symptoms [30, 31]. A much stronger association between peak VO2 values and NTproBNP levels was demonstrated in HF patients [32,33,34].
Our study confirmed an association between functional capacity and Hb levels, even when the latter fall within normal limits, which is consistent with earlier reports [34, 35]. This phenomenon, when observed in patients with AH, may be due to a relatively less efficient use of Hb as an oxygen transporter, which is a result of impaired oxygen extraction in skeletal muscles and is enhanced particularly by a rise in BP disproportionate to the level of exertion and impaired peripheral vessel dilation [35].
It should be also kept in mind that both NTproBNP and Hb levels are strongly related to age and sex, the main determinants of VO2 [8, 36, 37]. Significant differences between hypertensives men and women in exercise tolerance also matter as we demonstrated in our earlier manuscript [6].
Limitations
One limitation of our study was a small sample size, which may have affected the results of statistical analyses. Therefore, we cannot exclude that the strength of the evaluated correlations could be different when evaluated in a larger population. Moreover, the applied pharmacotherapy could also affect investigated relations. Especially, the potential influence of beta blockers on exercise performance should be considered. However, in our study the supplementary comparative analysis between patients treated and not treated with beta blockers did not revealed any significant difference in exercise capacity (peak VO2) or any other clinically relevant indices (i.e., NTproBNP, SBP, DBP, HR, LVEF, GLS, e′avg, E/e′, SV, CO).
Our study focused on a selected group of relatively young patients with AH and no comorbidities, which precludes extrapolating the results onto the general population. We must also mention that our study protocol did not include iron level, which may affect the assessed exercise capacity [36].
Conclusions
The association between parameters of physical capacity and the cardiovascular parameters evaluated at rest was poor and—specifically in terms of hemodynamic parameters—limited only to selected parameters of diastolic function. None of the echocardiographic or ICG parameters assessed at rest proved useful in grading exercise capacity. We must thus conclude that assessing exercise capacity in patients with AH based on resting tests alone is not sufficiently reliable and should be supplemented with exercise tests.
Summary table
What is known about this topic
-
The knowledge about relationship between exercise capacity and resting tests in patient with uncomplicated hypertension is still deficient.
What this study adds
-
Resting echocardiography does not allow exclusion of cardiovascular abnormalities.
-
Resting impedance cardiography is insufficiently reliable to assess exercise capacity.
-
Asymptomatic patients with arterial hypertension should be assessed by exercise tests.
References
Arena R, Myers J, Williams MA, Gulati M, Kligfield P, Balady GJ, et al. Assessment of functional capacity in clinical and research settings: a scientific statement from the American Heart Association Committee on Exercise, Rehabilitation, and Prevention of the Council on Clinical Cardiology and the Council on Cardiovascular Nursing. Circulation. 2007;116:329–43.
Wolfel EE. Exploring the mechanisms of exercise intolerance in patients With HFpEF: are we too “cardiocentric?”. JACC Heart Fail. 2016;4:646–8.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891–975.
Guazzi M, Arena R, Halle M, Piepoli MF, Myers J, Lavie CJ. 2016 focused update: clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2016;133:694–711.
Tsougos E, Angelidis G, Gialafos E, Tzavara C, Tzifos V, Tsougos I, et al. Myocardial strain may predict exercise tolerance in patients with reduced and mid-range ejection fraction. Hellenic J Cardiol. 2018;59:331–5.
Kurpaska M, Krzesiński P, Gielerak G, Uziębło-Życzkowska B, Banak M, Stańczyk A, et al. Exercise impedance cardiography reveals impaired hemodynamic responses to exercise in hypertensives with dyspnea. Hypertens Res. 2019;42:211–22.
Myers J, Christle JW, Tun A, Yilmaz B, Moneghetti KJ, Yuen E, et al. Cardiopulmonary exercise testing, impedance cardiography, and reclassification of risk in patients referred for heart failure evaluation. J Card Fail. 2019;25:961–8.
Wasserman K, Hansen JE, Sue DY, Stringer WW, Sietsema KE, Sun XG, et al. Physiology of exercise. Principles of exercise testing and interpretations: including pathophysiology and clinical applications. Philadelphia: Lippincott Williams & Wilkins; 2012. p. 9–61.
Krzesiński P, Uziębło-Życzkowska B, Gielerak G, Stańczyk A, Kurpaska M, Piotrowicz K. Global longitudinal two-dimensional systolic strain is associated with hemodynamic alterations in arterial hypertension. J Am Soc Hypertens. 2015;9:680–9.
Hasselberg NE, Haugaa KH, Sarvari SI, Gullestad L, Andreassen AK, Smiseth OA, et al. Left ventricular global longitudinal strain is associated with exercise capacity in failing hearts with preserved and reduced ejection fraction. Eur Heart J Cardiovasc Imaging. 2015;16:217–24.
Galderisi M, Lomoriello VS, Santoro A, Esposito R, Olibet M, Raia R, et al. Differences of myocardial systolic deformation and correlates of diastolic function in competitive rowers and young hypertensives: a speckle-tracking echocardiography study. J Am Soc Echocardiogr. 2010;23:1190–8.
Hensel KO, Jenke A, Leischik R. Speckle-tracking and tissue-doppler stress echocardiography in arterial hypertension: a sensitive tool for detection of subclinical LV impairment. Biomed Res Int. 2014;2014:472562. https://doi.org/10.1155/2014/472562.
Kurpaska M, Krzesiński P, Gielerak G, Stańczyk A, Piotrowicz K, Uziębło‑Życzkowska B, et al. Hemodynamical conditions of exercise capacity in patients with arterial hypertension—preliminary report. Lek Wojsk. 2015;93:244–52.
Molisz A, Schmederer Z, Siebert J, Kadamani T, Glasner P, Rosłonkiewicz K, et al. Haemodynamic parameters in postmenopausal women—beneficial effect of moderate continuous exercise training. Ann Agric Environ Med. 2019;26:425–8. https://doi.org/10.26444/aaem/100620.
Ding L, Quan XQ, Zhang S, Ruan L, Zhang L, Zheng K, et al. Correlation between impedance cardiography and 6min walk distance in atrial fibrillation patients. BMC Cardiovasc Disord. 2016;16:133.
Kurpaska M, Krzesiński P, Gielerak G, Uziębło-Życzkowska B, Banak M, Piotrowicz K, et al. Multiparameter assessment of exercise capacity in patients with arterial hypertension. Clin Exp Hypertens. 2019;41:599–606.
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–357.
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129 25 Suppl 2:102–38.
WHO. Haemo globin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and mineral nutrition information system. Geneva: World Health Organization; 2011. http://www.who.int/vmnis/indicators/haemoglobin.pdf. Accessed 24 Feb 2020.
Marwick TH, Gillebert TC, Aurigemma G, Chirinos J, Derumeaux G, Galderisi M, et al. Recommendations on the use of echocardiography in adult hypertension: a report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE). Eur Heart J Cardiovasc Imaging. 2015;16:577–605.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016;17:1321–60.
Balady GJ, Arena R, Sietsema K, Myers J, Coke L, Fletcher GF, et al. Clinician’s guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:191–225.
American Thoracic Society, American College of Chest Physicians. ATS/ACCP statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2003;167:211–77.
Gordon N, Abbiss CR, Maiorana AJ, Marston KJ, Peiffer JJ. Intrarater reliability and agreement of the physioflow bioimpedance cardiography device during rest, moderate and high-intensity exercise. Kinesiology. 2018;50:140–9.
Lapu-Bula R, Robert A, De Kock M, D’Hondt AM, Detry JM, Melin JA, et al. Relation of exercise capacity to left ventricular systolic function and diastolic filling in idiopathic or ischemic dilated cardiomyopathy. Am J Cardiol. 1999;83:728–34.
Asrar ul Haq M, Mutha V, Lin T, Profitis K, Tuer Z, Lim K, et al. Left ventricular torsional dynamics post exercise for LV diastolic function assessment. Cardiovasc Ultrasound. 2014;12:8.
Smart N, Haluska B, Leano R, Case C, Mottram PM, Marwick TH. Determinants of functional capacity in patients with chronic heart failure: role of filling pressure and systolic and diastolic function. Am Heart J. 2005;149:152–8.
Christiansen JR, Kanellopoulos A, Lund MB, Massey R, Dalen H, Kiserud CE, et al. Impaired exercise capacity and left ventricular function in long‑term adult survivors of childhood acute lymphoblastic leukemia. Pediatr Blood Cancer. 2015;62:1437–43.
Kim KH, Kane GC, Luong CL, Oh JK. Echocardiographic diastolic stress testing: what does it add? Curr Cardiol Rep. 2019;21:109. https://doi.org/10.1007/s11886-019-1187-8.
Krzesiński P, Uziebło-Życzkowska B, Gielerak G, Stańczyk A, Piotrowicz K, Piechota W, et al. Echocardiographic assessment and N-terminal pro-brain natriuretic peptide in hypertensives with metabolic syndrome. Adv Clin Exp Med. 2017;26:295–301.
Bettencourt P, Ferreira A, Sousa T, Ribeiro L, Brandão F, Polónia J, et al. Brain natriuretic peptide as a marker of cardiac involvement in hypertension. Int J Cardiol. 1999;69:169–77.
Koç M, Bozkurt A, Yildiray-Sahin D, Unal I, Acartürk E. Cutoff values of NT-proBNP for the prediction of low functional capacity, decreased ejection fraction and cardiovascular events in patients with heart failure. Cardiol J. 2009;16:43–51.
Katsumata Y, Tamura Y, Kimura T, Kohsaka S, Sadahiro T, Nishiyama T, et al. A high BNP level predicts an improvement in exercise tolerance after a successful catheter ablation of persistent atrial fibrillation. J Cardiovasc Electrophysiol. 2019;30:2283–90.
van Wezenbeek J, Canada JM, Ravindra K, Carbone S, Kadariya D, Trankle CR, et al. Determinants of cardiorespiratory fitness in patients with heart failure across a wide range of ejection fractions. Am J Cardiol. 2020;125:76–81.
Dhakal BP, Malhotra R, Murphy RM, Pappagianopoulos PP, Baggish AL, Weiner RB, et al. Mechanisms of exercise intolerance in heart failure with preserved ejection fraction: the role of abnormal peripheral oxygen extraction. Circ Heart Fail. 2015;8:286–94.
Jankowska EA, von Haehling S, Anker SD, Macdougall IC, Ponikowski P. Iron deficiency and heart failure: diagnostic dilemmas and therapeutic perspectives. Eur Heart J. 2013;34:816–29.
Raymond I, Groenning BA, Hildebrandt PR, Nilsson JC, Baumann M, Trawinski J, et al. The influence of age, sex and other variables on the plasma level of N-terminal pro brain natriuretic peptide in a large sample of the general population. Heart. 2003;89:745–51.
Funding
The study was funded by the Ministry of Science and Higher Education/Military Institute of Medicine, Warsaw, Poland (Grant No. 336/WIM).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kurpaska, M., Krzesiński, P., Gielerak, G. et al. Limited usefulness of resting hemodynamic assessments in predicting exercise capacity in hypertensive patients. J Hum Hypertens 35, 613–620 (2021). https://doi.org/10.1038/s41371-020-0373-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-0373-x
- Springer Nature Limited