Abstract
Health studies on spatially-varying exposures (e.g., air pollution) during pregnancy often estimate exposure using residence at birth, disregarding residential mobility. We investigated moving patterns in pregnant women (n = 10,116) in linked cohorts focused on Connecticut and Massachusetts, U.S., 1988–2008. Moving patterns were assessed by race/ethnicity, age, marital status, education, working status, population density, parity, income, and season of birth. In this population, 11.6% of women moved during pregnancy. Movers were more likely to be younger, unmarried, and living in urban areas with no previous children. Among movers, multiple moves were more likely for racial/ethnic minority, younger, less educated, unmarried, and lower income women. Most moves occurred later in pregnancy, with 87.4% of first moves in the second or third trimester, although not all cohort subjects enrolled in the first few weeks of pregnancy. Distance between first and second residence had a median value of 5.2 km (interquartile range 11.3 km, average 57.8 km, range 0.0–4277 km). Women moving larger distances were more likely to be white, older, married, and work during pregnancy. Findings indicate that residential mobility may impact studies of spatially-varying exposure during pregnancy and health and that subpopulations vary in probability of moving, and timing and distance of moves.
Similar content being viewed by others
Introduction
Mothers’ exposure to spatially-varying environmental exposures during pregnancy has been linked to critical infant and childhood health outcomes. Exposure to air pollution during pregnancy has been associated with restricted fetal growth and risk of preterm birth and birth defects [1, 2]. Mother’s residence in coal mining areas was linked to low birth weight [3], and agrichemicals in surface water were associated with higher risk of birth defects [4]. Other studies investigated birth outcomes in relation to the mothers’ residential proximity to power lines [5], airborne chlorinated solvents [6], coke and steel industrial facilities [7], roadways [8], natural gas development [9], gasoline service stations [10], use of methyl bromide [11], nuclear power plants [12], and waste sites [13]. These types of studies assess spatially-varying exposures during pregnancy in relation to adverse pregnancy and childhood health outcomes including fetal growth, birth defects, preterm delivery, allergic disorders, spontaneous abortion, childhood cancer, fetal death, and autism spectrum disorders [14].
Our ability to estimate how spatially-varying environmental exposures during pregnancy affect infant and childhood health is dependent on the approach used to assess exposure throughout the gestational period. Further, many relevant potential confounders vary spatially, such as community-level socio-economic status. A key challenge is that many relevant health datasets, such as birth certificate registries, may provide information on residence at time of birth but not the mother’s exact addresses throughout pregnancy. In other words, such studies are missing information on the mothers’ residential mobility throughout pregnancy, which can introduce exposure misclassification for spatially-varying factors.
While data on residential mobility are available in some datasets, such as the Norway Statistics database, which can be linked to birth certificate registry data [15], such information is rare. Studies based on cohort information may include detailed address information throughout pregnancy, although such data are often collected retrospectively after birth [16]. Still numerous studies depend on residence at time of birth to assess exposure to spatially-varying factors throughout pregnancy. This assumes that either the mother does not move during pregnancy or that any moves have minimal impact on estimates of exposure, such as moves of short distances or strong spatial homogeneity of the exposure of interest.
A recent study of residential mobility during pregnancy in United Kingdom based on the Congenital Abnormality Survey, with 5399 births, found that 24.4% of women moved during pregnancy [17]. A review of residential mobility during pregnancy identified 14 studies with such information, with overall mobility rates from 9 to 32% [14]. The review found evidence that some populations moved more frequently or different distances than others; however, the review noted that evidence in the identified papers was limited as residential history was typically assessed after delivery rather than during pregnancy. Further, the identified studies, while providing some information on residential mobility, were largely focused on other research questions, and were not aimed at providing a comprehensive description of which types of populations moved, how often, how far, etc.
The degree to which residential mobility may affect estimates of spatially-varying environmental exposures may differ by subpopulation in terms of who moves, how far they move, and when the move takes place during pregnancy. We investigated these questions with a study population of more than 10,000 women followed prospectively in related cohort studies. Mobility was assessed with respect to distance moved, timing of moves in pregnancy, and differences in moving patterns by subpopulation. We hypothesize that for some spatially-varying environmental exposures, exposure misclassification may occur due to use of residence at birth rather than residences throughout pregnancy. However, we aim to discern whether such exposure misclassification could be differential as some groups may move more often, farther distances, or earlier in pregnancy than others. Understanding population differences in residential mobility during pregnancy is especially important for studies investigating whether some subpopulations are particularly vulnerable or susceptible to environmental exposures during pregnancy.
Materials and methods
Cohort data
We combined information from four cohorts previously conducted by the Yale Center for Perinatal, Pediatric, and Environmental Epidemiology: the Environmental Tobacco Smoke Study, conducted 1988–1992 [18]; the Nutrition in Pregnancy cohort, conducted 1996–2000 [19,20,21]; the Asthma in Pregnancy cohort, conducted 1997–2000 [22,23,24]; and the Pink and Blue—Pregnancy and Depression cohort, conducted 2005–2008 [25, 26] (Supplemental Table 1). Informed consent was obtained and study protocols were approved by the Institutional Review Board at Yale University. The cohorts focused primarily on Connecticut and Massachusetts, and include some study participants who lived outside these areas at the start of pregnancy.
Mothers for each cohort were recruited and followed prospectively using the same general protocols and with the same team of lead investigators, resulting in compatible data across cohorts [18,19,20,21,22,23,24,25,26]. At private obstetricians offices women received a letter at first prenatal visit describing the cohort study. If the woman returned the letter indicating interest in the study, she was telephoned and screened for eligibility. Screening requirements for participation in the cohorts were independent of residential mobility. Additional information on screening (e.g., did not have insulin-dependent diabetes mellitus) is provided elsewhere [18,19,20,21,22,23,24,25,26].
At clinics, where there were a larger number of patients, research assistants approached women and described the study. If the woman was interested, she was screened at the clinic. All eligible women who agreed to participate were interviewed in their homes during the first or early second trimester of pregnancy. They were followed with one or more telephone interviews during pregnancy and were interviewed in the hospital postpartum or by telephone if they could not be interviewed prior to their discharge (15%). After delivery, medical records of both mother and infant were reviewed and outcome data abstracted using a standardized form under the supervision of experienced midwives.
The initial dataset for this study was based on 10,617 women. Six women (0.06%) were lost to follow-up, resulting in a remaining 10,611 women. Data include mother’s age, education level, race/ethnicity, marital status, working status during pregnancy, parity, and moves during pregnancy including approximate move dates and exact locations. Mother’s characteristics were assessed at time of enrollment. Family income was not collected for the Environmental Tobacco Smoke Study, and was collected in the other three cohorts. As the years of data for recruitment through birth spanned 1988 to 2008, income was adjusted to year 2000 values for comparability. Residential addresses were geocoded using GIS ArcMap 10.1 (ESRI Inc., Redlands, CA).
Analysis of residential mobility
We investigated the frequency of moves during pregnancy and the distance moved. Subpopulations were defined as mother’s race/ethnicity, age, marital status, education, working status during pregnancy, and annual family income adjusted to year 2000 $ values. For each residence throughout pregnancy, we calculated population density based on 2000 U.S. Census data at the Census tract level. Distance moved was calculated as between each residence and the subsequent or previous residence (e.g., distance from first to second residence, distance from second to third residence) and as the distance between the first residence of pregnancy and the residence at birth.
We investigated residential mobility patterns by subpopulation based on: (1) whether a woman moved (yes/no), (2) the number of moves for those who moved more than once during pregnancy, and (3) the distance moved. Chi-squared (χ2), Fisher’s Exact tests, and t-tests were used to compare the distribution of population characteristics for movers vs. non-movers and for comparing those who moved once vs. those who moved two or more times. Kruskal-Wallis χ2 test was used to compare distance between first and final residence by population characteristic. Univariate and multivariate regression was performed to explore differences in moving patterns by population.
Results
Study population
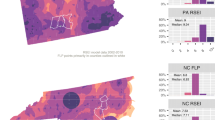
The study included 10,611 women, with enrollment and follow-up from 1988 to 2008, with the most participants living in Connecticut or Massachusetts at enrollment. The study population was predominantly white (75.3%), married (75.9%), and higher income (60.4% with household income > $50,000/year). Those with lower household income were more likely to be ethnic/racial minorities, older, and live in less urban environments. Those with less education were more likely to be younger and single.
Differences between movers and non-movers
In this study, 11.6% of women moved at least once during pregnancy. Those who moved (movers) and those who did not (non-movers) had statistically different characteristics with respect to race/ethnicity, age, marital status, education, working status, parity, family income, and urbanicity as measured by population density (Table 1). Populations more represented in the movers than non-movers were African-Americans (11.4% of movers vs. 7.2% of non-movers), Hispanics (19.6% of movers vs. 12.3% of non-movers) and single persons (39.3% vs. 18.7%). Those who moved were more likely to be younger (30.8% of movers were <25 years vs. 13.9% of non-movers), less educated (16.5% with less than high school education vs. 7.7%), and low income (29.5% with income < $20,000/year vs. 15.6%). Figure 1 depicts the relationship between the percent of the population who moved and age, parity, income, and age. Movers were more likely to live initially in an urban environment. First time mothers, of whom 14.3% moved during pregnancy, were more likely to move than those having their second or later child, of whom 10.0% moved (Fig. 1). No differences between movers and non-movers were detected regarding season of birth. Women who worked during pregnancy were less likely to move than those who did not (12.7% of workers moved, 15.0% of non-workers moved).
These factors were also associated with probability of moving in univariate regression, which identified associations between all of the population characteristics in Table 1, other than season of birth, and probability of moving during pregnancy (Table 2). Some of these associations did not remain after adjustment for other variables. The final model selected mother’s age, marital status, population density, and parity. For example, single women were 1.85 (95% confidence interval 1.52, 2.27) times more likely to move than married women, and divorced/separated women were 2.07 (1.45, 2.95) times more likely to move than married women. Those most likely to move were younger, unmarried, living in an urban area (highest quartile of population density), and having their first child.
Differences by number of moves, among movers
Most study participants who moved during pregnancy did so once (90.8% of movers). Of the movers 8.3% moved twice and 1% moved three times (Table 3). Patterns observed between those who moved once and those who moved more often during pregnancy were similar to patterns between non-movers and movers. Racial/ethnic minorities (African-American, Hispanics) were more likely to move multiple times compared to non-Hispanic whites. Among movers, the likelihood of moving multiple times decreased with mother’s age (Fig. 2), education, and family income. Multiple moves during pregnancy were more likely for mothers who were unmarried.
Timing of moves during pregnancy
Details on the timing of the moves within pregnancy were available for 58.7% of movers (n = 724). For other movers, data include the residences, but not timing of moves. Of these 724, the timing of the first move ranged from the first week to the 42nd week of pregnancy (Supplemental Figure 1). The average week of the first move was 22.8 weeks (median 22 weeks, interquartile range 11 weeks). Moves early in pregnancy were less frequent than moves later in pregnancy (12.6, 44.2, and 43.2% of first moves in the first, second, and third trimester, respectively). Although most women who moved did so in the second or third trimester of pregnancy (87.4%); those having their first child were more likely to move in the first trimester than mothers having their second or later child. The timing of the move was not associated with other population characteristics. Our results on timing of moves during pregnancy should be considered in the context of the cohort study design in which participants were generally not enrolled for the first few weeks of pregnancy.
Distance moved
Comparing first and last residences, most moves were short distances (median 5.1 km or 3.2 miles), with 7.9% moving over 4000 km. The distance between first and second residences ranged from 0.0 km (e.g., moves within an apartment building) to 4277 km (mean 57.8 km, median 5.2 km, interquartile range (IQR) 11.3 km). The distance between first and final residences averaged 58.8 km (IQR 11.4 km) (Supplemental Figure 2). Of those who moved, 17% moved 0.0 km; however, comparing first and last residences masks mobility of those who moved away from and then back towards their initial residence (7.3%). These include 6% of movers, who whose total distance across moves (from first to second residence, from second to third residence, etc.) exceeded the distance between first and final residence by >1 km, and a small number (<1%) whose total distance moved exceeded the distance between first and final residences by >100 km.
Table 4 shows the distance between the first residence and the residence at time of birth, for movers by subpopulation. Those who moved larger distances were more likely to be White, older, married, and to work during pregnancy (Supplemental Figure 3). A higher distance moved was associated with moving later in pregnancy (Supplemental Table 2).
Discussion
Previous studies have examined residential mobility with some research focused on pregnant women. In an earlier study, we reviewed research reporting residential mobility during pregnancy, finding that most studies were case-control analyses of birth defects and therefore may not be representative of the general population of pregnant women [14]. In most earlier studies, residential history was assessed after delivery, rather than prospectively. Our findings from this cohort study were generally consistent with that of the review. The review found overall mobility rates of 9–32% with most moves in the second trimester, whereas this cohort study identified a mobility rate of 11.6% with 44.3% and 43.1% of first moves in the second and third trimesters, respectively. We found that mobility was generally higher for mothers who were younger, unmarried, having their first child, and less educated; results on these factors were not consistent across previous studies identified in our earlier review.
Our results indicate that the degree of exposure misclassification resulting from residential mobility will depend on the characteristics of the study population. In particular, studies that examine populations with lower socio-economic status may have a higher fraction of movers than the general population, based on our results regarding mother’s marital status and education. Health responses from air pollution can differ by socio-economic status [2], therefore this population is of special interest. Our results suggest that exposure misclassification may be a particularly important issue for subpopulations that face higher risk from air pollution.
Further, the degree of exposure misclassification introduced by residential mobility will depend on study design, spatial heterogeneity of the exposure, and characteristics of the move. For studies of short-term periods, such as time-series analysis, residential mobility is unlikely to impact exposure assessment, especially for studies that limit study participants to residents. However, understanding of moving patterns is crucial for studies of spatially-varying exposures, or with spatially-varying factors as covariates, when exposures are assessed for periods of a few months or years before the health event, such as preterm delivery. Residential mobility for spatially-varying exposures has implications for health studies other than childhood and infant outcomes. Exposure misclassification can be introduced when cancer studies estimate community-level socio-economic conditions based on residence at time of diagnosis [27].
For studies that base exposure assessment on residence at a single time, longer timeframes of exposure are more likely to be impacted by residential mobility, especially for moves that occur earlier during the exposure period. Research on in utero exposures often bases exposure on residence at birth, thus moves earlier in pregnancy have higher potential to introduce exposure misclassification. Our results indicate that the timing of moves during pregnancy is associated with population characteristics. Studies that aim to identify critical exposure windows are hindered by higher exposure misclassification for earlier exposure windows compared to later exposure windows closer to time of birth. A related topic is the vulnerable gestational window of development for the health outcome of interest. For example, if the outcome develops late in pregnancy, the lack of residential mobility for early periods of pregnancy is not highly relevant.
The generalizability of this work is affected by the study population, which was predominantly white, married, and higher income. Although we were able to identify differences in residential moving patterns during pregnancy by subpopulation, a study with more diverse study participants may be able to identify additional findings. Nonetheless, our study population is somewhat more diverse than the general Connecticut or Massachusetts populations. Further, the moving patterns of this population may differ from those in other countries or regions of the U.S. Because our data are based on cohorts, study participants may differ from those who declined to enroll in the original studies or were lost to follow-up; however, this issue would hinder other cohorts as well.
A strength of this study was the consistency with which race/ethnicity was assessed across the four distinct cohorts; however, other categorizations of race/ethnicity are possible including some with more detailed information. As examples, our data did not distinguish between White Hispanic and Black/African-American Hispanic and included 200 participants categorized as “unknown.” Categorization of race/ethnicity is not consistent in scientific research and could result in different assumptions and interpretations of data [28]. Changing perceptions and understanding of race/ethnicity, including mixed race, have resulted in changes to the structure of Census questions for the U.S. and elsewhere [29]. Future work may involve more comprehensive investigation of race/ethnicity in relation to residential mobility during pregnancy and the implications for exposure and health effects estimates.
A limitation in our dataset was lack of information on the earliest part of pregnancy due to enrollment in the cohort design. Not all moves early in pregnancy and before enrollment are captured, although many observations do include such information. For some study participants, our dataset indicated that the mother moved during pregnancy but did not provide the timing of the move. While this is a key limitation in our dataset, the information provided is still an improvement over the most standard datasets with address at birth only.
Moves to locations close to the original residence (e.g., within neighborhood) could have minimal impact on exposure estimates, depending on the spatial heterogeneity of those exposures, whereas moves of larger distances could introduce dramatic exposure misclassification. Spatial heterogeneity can vary by exposure type, such as with different air pollutants or chemical components of fine particles [30, 31], and has been investigated for a wide range of spatially-varying exposures including soil contaminants [32] to drinking water [33]. Even if spatial heterogeneity of exposure is low, misclassification is likely for participants moving large distances. We observed that those who moved large distances had different demographic characteristics than those moving short distances. Some participants moved away from and then back towards their initial residence, which indicates that addresses recorded at several times throughout pregnancy may obscure exposure differences that would be captured by a full account of residential mobility.
Residential moving patterns involve the complex intersections of personal choice, housing availability, family structure and history, community, financial options, as well as employment and educational opportunities and are related to socio-economic conditions, social support structures, education, race/ethnicity, and other factors. Moving can impact family dynamics; relationships are more likely to dissolve in couples that move frequently [34], and residential mobility often benefits male partners more than women [34]. Our findings suggest that moving patterns of pregnant women are associated with age, marital status, parity, and urbanicity. These factors could further be related to exposure levels.
An additional complexity is that frequent moving is itself related to children’s health [35]. In a study of over 60,000 U.S. children, frequent movers had worse overall physical and oral health, after adjustment for race/ethnicity, age, presence of special health needs, family structure, parents’ education, poverty, and health insurance status [36]. In children, residential mobility has been associated with emotional and behavioral problems, higher rates of teenage pregnancy, and adolescent depression [37], although other work suggests that children who move more frequently may have better educational outcomes [38] and that residential mobility did not affect alcohol use in adolescents [39]. One study found that residential mobility is associated with lower self-worth in adolescents, but that this impact is lessened for those with strong social support systems [40]. The impact of moving on health can vary by the child’s personality; for introverts, children with frequent moves had lower well-being as adults [41]. These studies relate moving during childhood to children’s and adult health outcomes, but demonstrate broader links between family’s residential mobility and health. Children of mothers who move during pregnancy may have higher residential mobility during childhood and similarly have different health patterns than their more residentially stable counterparts.
Our findings demonstrate that moving patterns during pregnancy vary by subpopulation, which could result in differential exposure misclassification for spatially-varying exposures. Environmental health studies that aim to discern whether some persons face a disproportionate health burden are further hindered by the different patterns of residential mobility by subpopulation.
References
Wilhelm M, Ghosh JK, Su J, Cockburn M, Jerrett M, Ritz B. Traffic-related air toxics and preterm birth: a population-based case-control study in Los Angeles county, California. Environ Health. 2011;10:Art. No. 89.
Bell ML, Ebisu K, Belanger K. Ambient air pollution and low birth weight in Connecticut and Massachusetts. Environ Health Perspect. 2007;115:1118–25.
Ahern M, Mullett M, Mackay K, Hamilton C. Residence in coal-mining areas and low-birth-weight outcomes. Matern Child Health J. 2011;15:974–9.
Winchester PD, Huskins J, Ying J. Agrichemicals in surface water and birth defects in the United States. Acta Paediatr. 2009;98:664–9.
Auger N, Joseph D, Goneau M, Daniel M. The relationship between residential proximity to extremely low frequency power transmission lines and adverse birth outcomes. J Epidemiol Community Health. 2011;65:83–5.
Brender JD, Shinde MU, Zhan FB, Gong X, Langlois PH. Maternal residential proximity to chlorinated solvent emissions and birth defects in offspring: a case-control study. Environ Health. 2014;13:96.
Porter TR, Kent ST, Su W, Beck HM, Gohlke JM. Spatiotemporal association between birth outcomes and coke production and steel making facilities in Alabama, USA: a cross-sectional study. Environ Health. 2014;13:85.
Dadvand P, et al. Residential proximity to major roads and term low birth weight: the roles of air pollution, heat, noise, and road-adjacent trees. Epidemiology. 2014;25:518–25.
McKenzie LM, Guo R, Witter RZ, Savitz DA, Newman LS, Adgate JL. Birth outcomes and maternal residential proximity to natural gas development in rural Colorado. Environ Health Perspect. 2014;122:412–7.
Huppe V, Kestens Y, Auger N, Daniel M, Smargiassi A. Residential proximity to gasoline service stations and preterm birth. Environ Sci Pollut Res Int. 2013;20:7186–93.
Gemmill A, Gunier RB, Bradman A, Eskenazi B, Harley KG. Residential proximity to methyl bromide use and birth outcomes in an agricultural population in California. Environ Health Perspect. 2013;121:737–43.
Wang SI, Lee LT, Zou ML, Fan CW, Yaung CL. Pregnancy outcome of women in the vicinity of nuclear power plants in Taiwan. Radiat Environ Biophys. 2010;49:57–65.
Langlois PH, et al. Maternal residential proximity to waste sites and industrial facilities and conotruncal heart defects in offspring. Paediatr Perinat Epidemiol. 2009;23:321–31.
Bell ML, Belanger K. Review of research on residential mobility during pregnancy: consequences for assessment of prenatal environmental exposures. J Expo Sci Environ Epidemiol. 2012;22:429–38.
Blaasaas KG, Tynes T, Lie RT. Residence near power lines and the risk of birth defects. Epidemiology. 2003;14:95–98.
Brauer M, Lencar C, Tamburic L, Koehoorn M, Demers P, Karr C. A cohort study of traffic-related air pollution impacts on birth outcomes. Environ Health Perspect. 2008;116:680–6.
Hodgson S, Lurz PW, Shirley MD, Bythell M, Rankin J. Exposure misclassification due to residential mobility during pregnancy. Int J Hyg Environ Health. 2015;218:414–21.
Sadler L, et al. Environmental tobacco smoke exposure and small-for-gestational-age birth. Am J Epidemiol. 1999;150:695–705.
Grosso LM, Triche EW, Belanger K, Benowitz NL, Holford TR, Bracken MB. Caffeine metabolites in umbilical cord blood, cytochrome P-450 1A2 activity, and intrauterine growth restriction. Am J Epidemiol. 2006;163:1035–41.
Bracken MB, Triche EW, Belanger K, Hellenbrand K, Leaderer BP. Association of maternal caffeine consumption with decrements in fetal growth. Am J Epidemiol. 2003;157:456–66.
Bracken MB, Triche E, Grosso L, Hellenbrand K, Belanger K, Leaderer BP. Heterogeneity in assessing self-reports of caffeine exposure: implications for studies of health effects. Epidemiology. 2002;13:165–71.
Triche EW, Saftlas AF, Belanger K, Leaderer BP, Bracken MB. Association of asthma diagnosis, severity, symptoms, and treatment with risk of preeclampsia. Obstet Gynecol. 2004;104:585–93.
Belanger K, Hellenbrand ME, Holford TR, Bracken M. Effect of pregnancy on maternal asthma symptoms and medication use. Obstet Gynecol. 2010;115:559–67.
Triche EW, et al. Indoor heating sources and respiratory symptoms in nonsmoking women. Epidemiology. 2005;16:377–84.
Rogal SS, et al. Effects of posttraumatic stress disorder on pregnancy outcomes. J Affect Disord. 2007;102:137–43.
Spoozak L, Gotman N, Smith MV, Belanger K, Yonkers KA. Evaluation of a social support measure that may indicate risk of depression during pregnancy. J Affect Disord. 2009;114:216–23.
Bryere J, Pornet C, Dejardin O, Launay L, Guittet L, Launoy G. Correction of misclassification bias induced by the residential mobility in studies examining the link between socioeconomic environment and cancer incidence. Cancer Epidemiol. 2015;39:256–64.
Drevdahl DJ, Philips DA, Taylor JY. Uncontested categories: the use of race and ethnicity variables in nursing research. Nurs Inq. 2006;13:52–63.
Valles SA, Bhopal RS, Aspinall PJ. Census categories for mixed race and mixed ethnicity: impacts on data collection and analysis in the US, UK and NZ. Public Health. 2015;129:266–70.
Ito K, Xue N, Thurston G. Spatial variation of PM2.5 chemical species and source-apportioned mass concentrations in New York City. Atmos Environ. 2004;38:5269–82.
Bravo MA, Bell ML. Spatial heterogeneity of PM10 and O3 in São Paulo, Brazil, and implications for human health studies. J Air Waste Manag Assoc. 2011;61:69–77.
Hu XF, Du Y, Feng JW, Fang SQ, Gao XJ, Xu SY. Spatial and seasonal variations of heavy metals in wetland soils of the tidal flats in the Yangtze Estuary, China: environmental implications. Pedosphere. 2013;23:511–22.
Rice J, Westerhoff P. Spatial and temporal variation in de facto wastewater reuse in drinking water systems across the U.S.A. Environ Sci Technol. 2015;49:982–9.
Boyle PJ, Kulu H, Cooke T, Gayle V, Mulder CH. Moving and union dissolution. Demography. 2008;45:209–22.
Brown D, Benzeval M, Gayle V, Macintyre S, O’Reilly D, Leyland AH. Childhood residential mobility and health in late adolescence and adulthood: findings from the West of Scotland Twenty-07 Study. J Epidemiol Community Health. 2012;66:942–50.
Busacker A, Kasehagen L. Association of residential mobility with child health: an analysis of the 2007 National Survey of Children’s Health. Matern Child Health J. 2012;16(Suppl 1):S78–87.
Jelleyman T, Spencer N. Residential mobility in childhood and health outcomes: a systematic review. J Epidemiol Community Health. 2008;62:584–92.
Haelermans C, De Witte K. Does residential mobility improve educational outcomes? Evidence from the Netherlands. Soc Sci Res. 2015;52:351–69.
Jackson N, Denny S, Ameratunga S. Social and socio-demographic neighborhood effects on adolescent alcohol use: a systematic review of multi-level studies. Soc Sci Med. 2014;115:10–20.
Hendershott AB. Residential mobility, social support and adolescent self-concept. Adolescence. 1989;24:217–32.
Oishi S, Schimmack U. Residential mobility, well-being, and mortality. J Pers Soc Psychol. 2010;98:980–94.
Acknowledgements
We thank the Yale Center for Perinatal, Pediatric, and Environmental Epidemiology and study participants. This work was funded by NIEHS (R01ES01587 and R01ES019560), the U.S. Environmental Protection Agency (EPA RD 83479801 and RD 835871) and an NHMRC Early Career Fellowship grant (1052236 to GP). This paper has not been formally reviewed by the EPA. The views expressed in this document are solely those of the authors and do not necessarily reflect those of the Agency. EPA does not endorse any products or commercial services mentioned in this publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Bell, M.L., Banerjee, G. & Pereira, G. Residential mobility of pregnant women and implications for assessment of spatially-varying environmental exposures. J Expo Sci Environ Epidemiol 28, 470–480 (2018). https://doi.org/10.1038/s41370-018-0026-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-018-0026-0
- Springer Nature America, Inc.
Key words
This article is cited by
-
Predictors of early life residential mobility in urban and rural Pennsylvania children with acute lymphoblastic leukemia and implications for environmental exposure assessment
Journal of Exposure Science & Environmental Epidemiology (2023)
-
Assessing Exposure to Unconventional Oil and Gas Development: Strengths, Challenges, and Implications for Epidemiologic Research
Current Environmental Health Reports (2022)
-
On the potential of iPhone significant location data to characterize individual mobility for air pollution health studies
Frontiers of Environmental Science & Engineering (2022)