Abstract
Background/Objectives
Different approaches are used to classify obesity severity. Beyond classical anthropometric measurements, the Edmonton Obesity Staging System (EOSS) considers medical, physical and psychological parameters. However, this method has some limitations, principally due to the absence of an objective measure for physical impairment. The aim of our study is thus to overcome this limitation suggesting a new functional parameter obtained by cardiopulmonary exercise testing (CPET), i.e., cardiorespiratory fitness (CRF), expressed as weight-adjusted peak oxygen consumption (VO2peak/kg).
Subjects/Methods
This observational cross-sectional study conducted on a population of 843 patients affected by obesity finally enrolled 500 subjects. Every patient underwent clinical, anthropometric, biochemical assessment and CPET. First, participants have been classified according to standard EOSS in five stages. Second, patients were reclassified according to the new modified EOSS (EOSS-CRF) based on their age- and gender-appropriate VO2peak/kg percentiles as reported in the healthy normal-weight population of the FRIEND registry.
Results
VO2peak/kg was significantly different between standard EOSS classes 1 and 2 and classes 1 and 3 (ANCOVA p model = 0.004), whereas patients in classes 2 and 3 showed similar CRF. The EOSS-CRF classification varied in number of patients in each class compared to EOSS, particularly with a shift from class 2 to class 3. Moreover, CRF showed that physical impairment is less addressed by EOSS when compared to EOSS-CRF.
Conclusions
The integration of EOSS with CRF allowed us to assign to each patient a severity index that considers not only clinical parameters, but also their functional impairment through a quantitative and prognostically important parameter (VO2peak/kg). This improvement of the staging system may also provide a better approach to identify individuals at increased risk of mortality leading to targeted therapeutic management and prognostic risk stratification for patients with obesity.
Similar content being viewed by others
Introduction
Obesity has been spreading worldwide with around 2 billion adults affected by overweight or obesity [1]. Many medical societies have now defined obesity as a disease, as reviewed in a statement from the World Obesity Federation [2]. To classify obesity and assess cardiovascular risk, body mass index (BMI) and waist circumference are preferably used in clinical practice as surrogate measures of body and visceral fat, respectively [3]. However, the presence of comorbidities or the risk of diseases development can thereby not be assessed. Indeed, people with the same BMI may have very different body compositions, whereas a greater amount of visceral fat predisposes to obesity-related diseases and is associated with an increased mortality risk [4, 5]. Moreover, BMI does not provide information regarding functional capacity, quality of life or other prognostic contextual factors that may further characterise clinical risk and guide therapeutic management [6]. Thus, the need to identify more meaningful criteria to diagnose and classify obesity is an emerging matter [7]. In 2009, the Edmonton Obesity Staging System (EOSS) has provided a five-stage classification of obesity, considering medical, physical and psychological parameters, which allowed the clinician to describe comorbidities associated with excess weight [8]. It was suggested that EOSS may offer a useful approach to identify individuals at elevated risk of mortality [9, 10]. Conversely, a recent study has demonstrated that Cardiometabolic Disease Staging has better predictive ability for mortality than EOSS [11]. This fact could be explained by the different factors included in the evaluations, indeed, EOSS considers additionally functional and mental status, which may explain the differences in predicting the mortality risk. Hence, the EOSS criteria provide a wide flexibility in the assessments of these parameters, particularly for functional performance/impairment, currently rather subjectively evaluated by patients and clinicians. For instance, it is very difficult to define and differentiate mild, moderate and severe functional limitations in activities of daily living [8]. Therefore, it should be aimed to overcome this limitation for clinicians by introducing an objectively measurable parameter to grade functional impairment, i.e., cardiorespiratory fitness (CRF), expressed by weight-adjusted peak oxygen consumption (VO2peak, ml/kg/min), evaluated through cardiopulmonary exercise testing (CPET). Indeed, it is well known that CRF is a strong independent predictor of all-cause and cardiovascular mortality in health and different chronic diseases [12, 13]. VO2peak has an important role in assessing functional capacity and it can be considered the most direct measure of a person’s ability to perform physical activity; moreover, it has a direct impact on activities of daily living and is associated with future risk of disabilities [14]. The evaluation of CRF has begun to be considered as a vital sign, depending on its strong improvement of risk prediction and its association with total patient health [15]. Therefore, measurements of CRF through CPET may improve EOSS due to objective assessed functional capacity and impairment in patients with obesity. The objective was thus to propose a new modified EOSS (EOSS-CRF) in order to improve the clinical utility of obesity classification with therapeutic and prognostic impact on patients.
Materials and methods
Patients
In this observational cross-sectional study 843 patients with obesity were consecutively studied at the Center for the Study and Integrated Treatment of Obesity, Hospital University of Padua, Italy, in the period between 2014 and 2019. All patients underwent a multi-disciplinary evaluation according to a standardised clinical protocol and were subsequently assigned to surgical or medical treatment according to European criteria [16]. Consistent with the local diagnostic-therapeutic pathway of clinical assistance, patients were also evaluated at the Sport and Exercise Medicine Division of the University of Padua. In patients with indication for surgical treatment, who represent the majority of study population, the two evaluations were scheduled before bariatric surgery and before receiving a pre-surgery 4-week very low-calorie diet and physical activity prescriptions. Specific exclusion criteria for this study were previous bariatric surgery, anaemia, sign, symptoms and severe diseases that contraindicated maximal exercise stress test. Furthermore, only patients who presented all data to stage according EOSS classes were included. Thus, 500 patients (BMI 42.78 ± 6.63, range 30.02–67.90 kg/m2) were enrolled.
All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the ‘Padua Ethical Committee for Clinical Research’ (2892P, 10 June 2013).
Anthropometric measurements
All anthropometric measurements were taken with subjects wearing only light clothes without shoes. Height was measured to the nearest 0.01 m using a stadiometer. Body weight was determined to the nearest 0.1 kg using a calibrated balance beam scale. BMI was calculated as weight (kg) divided by height squared (m2).
Biochemical assessment
For each patient we measured fasting plasma glucose (FPG), insulin, lipid profile [total cholesterol, high-density lipoprotein-cholesterol and low-density lipoprotein-cholesterol (LDL), triglycerides], full blood count, alanine aminotransferase, aspartate aminotransferase and gamma glutamiltrasferase. All blood tests were performed after 8-h fasting. Samples were stored at −20 °C until analysis. All biochemical blood analyses have been performed with standard diagnostic kits according to the WHO First International Reference Standard. LDL cholesterol was calculated according to Friedewald [17]. In patients without known diabetes, a 3-h oral glucose tolerance test (OGTT) was performed monitoring blood glucose and insulin plasma levels after glucose load (75 g) [18]. Homeostasis model assessment-insulin resistance index (HOMA) was used to calculate the insulin-resistance index: [fasting serum insulin (μU/ml) × FPG (mmol/l)]/22.5 [19]. HOMA was not calculated for patients in insulin treatment.
Cardiopulmonary exercise testing (CPET)
Incremental and maximal CPET was performed preferentially on treadmill (COSMOS, T170 DE-med model) with the modified Bruce protocol (n = 430); bicycle ergometer with adapted protocols was used in patients with orthopaedic limitations (n = 70). Subjects were verbally encouraged to reach maximal exertion. Criteria of exhaustion were a Borg rating of perceived exertion of 18/20 [20], associated with either a maximal heart rate ≥85% of predicted (220 bpm – age) or a peak Respiratory Exchange Ratio >1.10 [21]. ECG, arterial blood pressure and peripheral oxygen saturation were continuously monitored at rest, during exercise as well as in the recovery phase. Ventilatory and gas exchange measurements were sampled breath-by-breath and measured by a low-resistance turbine and mass spectrometry, respectively (Masterscreen CPX Jaeger, Carefusion, Hoechberg, GE system) [22]. Main parameters of CRF and efficiency are here reported, i.e., VO2peak/kg and the oxygen uptake efficiency slope, determined as the coefficient of the linear relationship between VO2 and the logarithm of total ventilation [23].
VO2peak/kg reference values and relative percentiles of the FRIEND registry, which considered healthy and normal-weight subjects, were used to classify our study population regarding functional capacity [24]. Moreover, patients were thereby grouped according to the VO2peak/kg percentiles reported for age and gender, respectively:
-
Patients with VO2peak/kg over the 25th percentile were considered with a normal functional capacity.
-
Patients with VO2peak/kg between the 10th and 25th percentile were considered with a mild reduction of functional capacity.
-
Patients with VO2peak/kg between the 5th and 10th percentile were considered with a moderate reduction of functional capacity.
-
Patients with VO2peak/kg lower than the 5th percentile were considered with a severe reduction of functional capacity.
EOSS classification
We classified our population according to patients’ glycemic profile [18] in normal glycaemia, affected by prediabetes (pre-DM) (impaired fasting glycaemia and/or impaired glucose tolerance at the OGTT) and type 2 diabetes mellitus. Diagnosis of arterial hypertension (HYPT) [25], dyslipidaemia (DLP) [26], obstructive sleep apnoea syndrome (OSA) [27] and non-alcoholic fatty liver disease (NAFLD) [28, 29] was based on recent guidelines. We categorised patients to EOSS classes by using the highest-stage risk factor for each patient [8, 30]. Patients without any medical, functional and psychiatric symptoms were considered EOSS stage 0. Patients with obesity-related subclinical risk factors (i.e., pre-DM, subclinical DLP), as well as mild medical, functional and psychiatric symptoms were classified as EOSS 1. Patients with established obesity-related chronic disease (i.e., HYPT, DLP, OSA, NAFLD, gastric esophageal reflux, goat), those receiving pharmacological therapy or presenting moderate medical, functional and psychiatric symptoms, were considered EOSS 2. Patients with end-organ damage (e.g., heart failure, myocardial infarction, stroke, renal injury, cirrhosis) or significant medical, functional, psychiatric symptoms were included in EOSS 3. Patients with severe and potentially end-stage disabilities from obesity-related chronic diseases, severe disabling psychopathology or functional limitations, and those with impairment of well-being were classified as EOSS 4 [8, 30]. In the standard EOSS classification we used not quantitative parameters to define functional impairment as mild, moderate, severe and end-stage, considering limitations in activities of daily living and/or impairment of well-being (i.e., being able to tie your shoes or to do housework). In particular, when the distinction between classes was not adequately clear, patients who underwent a treadmill CPET were considered as mildly limited and thus included in EOSS 1, while people who were not able to perform a standard exam and need a bicycle ergometer for CPET were classified as moderately limited, i.e., EOSS 2. Patients with articular prosthesis or previous joint surgery were considered affected by significant functional limitation and thus assigned to EOSS 3. Patients with potentially end-stage functional limitation unable to perform CPET were excluded from the study. In the new EOSS-CRF we associated with each EOSS stage an objectively measured functional capacity marker in order to overcome these limitations. Moreover, clinical and psychiatric parameters of the standard EOSS were associated with ranges of VO2peak/kg percentiles to reclassify our patients in the new EOSS-CRF.
Statistical analysis
Data have been analysed with IBM SPSS Statistics (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). All continuous variables were analysed by normality tests (Shapiro–Wilk test). ANCOVA analysis was used to assess and compare estimated means of VO2peak/kg, corrected by age and gender covariates. The estimated sample size, applying an alpha error cut-off of 5%, is 165, obtaining a statistical power of 80%. P value ≤ 0.05 was considered statistically significant.
Results
Anthropometric and functional characteristics of 500 patients with obesity (BMI 42.78 ± 6.63, range 30.02–67.90 kg/m2) are reported in Table 1, where patients are also grouped by standard EOSS and EOSS-CRF, separately. Most patients belonged to EOSS 2, according to both standard (n = 401) and modified (n = 252) EOSS classification. Already from this first descriptive analysis, we observed the changes in distribution of patients among the two different classifications (Fig. 1). The diversion involved mainly patients in EOSS 2 who were redistributed in EOSS-CRF 3. Other patients were assigned from EOSS 1 to EOSS-CRF 2 or EOSS-CRF 3 and three patients from EOSS 0 to EOSS-CRF 1 or 2. EOSS 0 and EOSS 4 were excluded from further analyses because of small sample sizes.
Results are presented as number of patients, consensually to data presented in Table 1, considering all five classes.
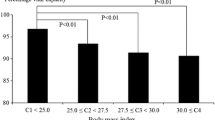
Figure 2 shows estimated average values of VO2peak/kg corrected for age and gender covariates as main intrinsic determinants, in different standard EOSS classes. Comparing these corrected values between groups, the ANCOVA model results statistically highly significant (p = 0.009), determined by the difference between EOSS 1 and EOSS 2 and EOSS 1 and EOSS 3. Interestingly, patients belonging to EOSS 2 and EOSS 3 displayed similar VO2peak/kg values.
The prevalence of the most important comorbidities associated with obesity is shown in Fig. 3 for EOSS and EOSS-CRF, respectively. Patients included in EOSS 1 showed obesity-related subclinical risk factors as well pre-DM or an alteration of plasma lipids without an overt DLP. In the modified version, the assignment versus a worse stage (EOSS 1 to EOSS 2 or 3, EOSS 2 to EOSS 3) explains different frequencies of comorbidities among the two classifications. Comorbidities did not show any significant differences between EOSS and EOSS-CRF, with the exclusion of NAFLD between EOSS 3 and EOSS-CRF 3 (p = 0.024).
On the other hand, Fig. 4 elucidates the severity of functional impairment according to the different classifications. Moreover, the evaluation of functional aspects as it was described by EOSS turned out difficult to apply, leading to fewer data than objective assessment through CPET in EOSS-CRF. In fact, 55.3% of the reclassified patients in EOSS-CRF 1 presented a mild functional impairment versus 20.3% of EOSS 1. Among EOSS-CRF 2 patients, 47.2% showed a mild impairment (versus 15%), whereas 27% displayed a moderate one (versus 9%). Most patients of EOSS-CRF 3 (93.2%) were affected by a severe reduction of functional capacity, while in standard EOSS 3 only 11.8% of patients were evaluated as severely functionally impaired.
To better understand the role of functional impairment and thus the impact of CPET in the evaluation of patient with obesity, Fig. 5 shows the reasons why patients were assigned to a specific group, visually comparing EOSS and EOSS-CRF. In other words, clinical and functional determinants were analysed for the assignment of patients to each EOSS class according both standard (inner circle) and modified EOSS (exterior circle). In classical EOSS, functional and clinical classifications agreed to determine the belonging classes in a smaller percentage of patients when compared to the modified version. Furthermore, in the EOSS-CRF, functional evaluation plays a more relevant role in staging, particularly for class 3, where patients were majorly assigned to this group for severe functional impairment (EOSS-CRF 85.5% versus EOSS 11.8%) and not for purely severe clinical reasons.
Discussion
EOSS provides a useful method to overcome BMI limits in the evaluation of patients with obesity. Nevertheless, different levels of physical impairment included as main EOSS criteria currently result not well defined and difficult to accurately assign [8, 30]. This could lead to a bias in assigning patients to the correct class, with a general underestimation of the importance of functional aspects in determining the severity of obesity. In fact, our study has shown how the traditionally defined functional capacity only minimally impacts the standard EOSS, which mostly depends on clinical parameters. In our study, to assign functional limitation according to standard EOSS, we have not only analysed patient’s history data, but also the ability of patients to perform exercise on treadmill rather than bicycle ergometer. This assessment may improve quality of functional parameter, but still remains not objectively quantifiable.
Therefore, 500 patients’ CRF was systematically evaluated, with the aim of proposing an integration for EOSS. This EOSS-CRF could make clinical and functional evaluation easier and more accurate when compared to EOSS in order to more appropriately classify patients’ severity of obesity as a chronic multi-dimensional disease.
Indeed, CRF is a strong independent predictor of all-cause mortality and cardiovascular disease [12, 13] and can quantitatively evaluate functional physical impairment. Moreover, VO2peak/kg can importantly decrease in individuals suffering from obesity, but represents a more reliable parameter than the absolute value of oxygen consumption in evaluating the ability to carry out activities of daily living [15, 21]. Indeed, VO2peak/kg is used in other clinical settings, for the assessment of patients with heart failure as objective criteria for transplantation, also due to its impact on functional performance and thus quality of life [31,32,33].
We compared estimated average values of VO2peak/kg, corrected for age and gender, in different standard EOSS classes and showed limited functional distinguishability between classes. This fact might be explained by the deficiency of the traditional staging system in differentiating the severity of functional impairment.
Thus, we have suggested to assign mild, moderate and severe reduction in functional capacity according to percentile-ranges based on the FRIEND registry [24]. In fact, it is known that a reduction of CRF below the 25th percentile is associated with a two- to five-fold increase in cardiovascular risk or death for all causes independently of other risk factors [34]. Because of the absence of functional capacity reference values for patients affected by obesity, we have considered functional CPET data from literature related to other fields of studies. Moreover, while a minimum of 15 ml/min/kg VO2peak might be needed to perform activities of daily living [35]. Other guidelines consider a VO2peak of 12–14 ml/min/kg as threshold for cardiac transplantation in heart failure [32]. Nevertheless, at the moment, no studies have demonstrated direct correlation between VO2peak and the impairment of daily activities in patients with obesity. However, it can be suggested that CRF could include in a single parameter all aspects of functional limitation during daily living. [15] Thus, from these general considerations, we used the classification based on percentile-ranges previously described in the Method section.
By re-classifying patients according to the new EOSS-CRF, we first noticed a numerical redistribution compared to standard EOSS for all classes but particularly affecting classes 2 and 3. Some differences in average values of age, BMI and gender were observed between EOSS and EOSS-CRF. These data can be easily explained by the fact that higher values of VO2peak/kg are expected from younger subjects, males and from patients with a lower BMI. By applying the modified criteria, patients were generally assigned to a worse EOSS-CRF stage, which explains different frequencies of comorbidities among the two classifications. However, only the NAFLD prevalence resulted statistically significant different between EOSS 3 and EOSS-CRF 3. This fact could be explained by the ectopic deposition of free fatty acids in patients with obesity, which involves also peripheral skeletal muscles and may thus reduce functional capacity and CRF.
Particularly, the new EOSS-CRF reassigned patients from classes 2 to 3, thereby distributing the well-known 80% of patients usually belonging to standard EOSS 2 [30]. Moreover, introducing this new measurable parameter of CRF, allows us to objectively evaluate a decrease in functional capacity that would otherwise not affect the overall clinical, physical and psychiatric disease severity in obesity. Moreover, the new staging method revealed an increase in numbers of patients reporting an impairment of functional capacity (mild, moderate or severe) in each class, compared to the standard EOSS. Conversely, the impact of only clinical parameters markedly decreased applying the EOSS-CRF, particularly for class 3. Indeed, patients were predominantly (85.5%) assigned to this group for severe functional impairment, while the previous functional markers determined EOSS class 3 in only 11.8%. Hence, we demonstrated that objectively measured CRF, as marker of physical impairment, should play a major role in determining clinically and prognostically useful, obesity-related, disease severity classes.
This study came across some limitations of the EOSS, which should be addressed by future trials. First, we enrolled patients affected by obesity in a centre where bariatric surgery is a commonly suggested treatment option because of selected patient recruitment. This may explain the high prevalence of obesity-related comorbidities. Second, psychiatric parameters are gained on self-reported patient history data only, even though based on Diagnostic and Statistical Manual of Mental Disorders classification. Conversely, we overcame some limitations such as the definitions and cut-offs for HYPT, DLP or glycaemic impairment that have been all updated at the current guidelines. Third, as shown in literature, EOSS class 0 and 4 are characterised by relatively small sample size in this population, which had thus to be excluded from further analyses [30]. A possible small bias of this study may consist in the inclusion of both treadmill and bicycle ergometer to perform CPET, with the risk of underestimation of VO2peak by the latter [36]. Nevertheless, this was clinically conditioned and may indeed reflect functional impairment in case of walking difficulties. Moreover, one of the major strengths of our study is that all patients performed a maximal exercise test. Finally, this study does not assess the predictive value of the new classification and a follow-up project will be requested.
In conclusion, we hereby propose an integration of EOSS, demonstrating that not only clinical aspects but also the impairment of functional capacity and CRF, measured by VO2peak/kg, affect the severity of obesity. Thus, CRF, as one of the most important prognostic marker of all-cause and cardiovascular mortality [12, 15], could be the right missing piece to have as global an evaluation as possible of this chronic disease. Furthermore, the EOSS-CRF allowed us to assign to each patient a disease severity index and thus to probably better identify individuals at elevated risk of mortality [9, 10], overcoming the restraints linked to the previously encountered limitation in evaluating patients’ functional impairment [11]. Consequently, EOSS-CRF may lead to clinical implications regarding therapeutic management and prognostic risk stratification for patients with obesity, just like in other chronic diseases [6].
References
Global Burden of Disease Collaborative Network. Global burden of disease study 2015 (GBD 2015) obesity and overweight prevalence 1980–2015. Seattle, United States Institute for Health Metrics and Evaluation 2017.
Bray GA, Kim KK, Wilding JPH. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev. 2017;18:715–23.
Bhaskaran K, dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6:944–53.
Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000;72:694–701.
Pischon T, Boeing H, Hoffmann K, Bergmann M, Schulze MB, Overvad K, et al. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008;359:2105–20.
Santini F, Busetto L, Cresci B, Sbraccia P. SIO management algorithm for patients with overweight or obesity: consensus statement of the Italian Society for Obesity (SIO). Eat Weight Disord. 2016;21:305–7.
Rubino F, Puhl RM, Cummings DE, Eckel RH, Ryan DH, Mechanick JI, et al. Joint international consensus statement for ending stigma of obesity. Nat Med. 2020;26:485–97.
Sharma AM, Kushner RF. A proposed clinical staging system for obesity. Int J Obes. 2009;33:289–95.
Kuk JL, Ardern CI, Church TS, Sharma AM, Padwal R, Sui X, et al. Edmonton Obesity Staging System: association with weight history and mortality risk. Appl Physiol Nutr Metab. 2011;36:570–6.
Padwal RS, Pajewski NM, Allison DB, Sharma AM. Using the Edmonton Obesity Staging System to predict mortality in a population-representative cohort of people with overweight and obesity. CMAJ. 2011;183:1059–66.
Ejima K, Xavier NA, Mehta T. Comparing the ability of two comprehensive clinical staging systems to predict mortality: EOSS and CMDS. Obesity. 2020;28:353–61.
Blair SN, Kohl HW, Paffenbarger RS, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. JAMA. 1989;262:2395.
Myers J, Prakash M, Froelicher V, Do D, Partington S, Edwin Atwood J. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801.
Rabiee R, Agardh E, Kjellberg K, Falkstedt D. Low cardiorespiratory fitness in young adulthood and future risk of disability pension: A follow-up study until 59 years of age in Swedish men. J Epidemiol Community Health. 2015;69:266–71.
Ross R, Blair SN, Arena R, Church TS, Després JP, Franklin BA, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134:e653–99.
Yumuk V, Tsigos C, Fried M, Schindler K, Busetto L, Micic D, et al. European guidelines for obesity management in adults. Obes Facts. 2015;8:402–24.
Bairaktari ET, Seferiadis KI, Elisaf MS. Evaluation of methods for the measurement of low-density lipoprotein cholesterol. J Cardiovasc Pharmacol Ther. 2005;10:45–54.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and?-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–81.
Balady GJ, Arena R, Sietsema K, Myers J, Coke L, Fletcher GF, et al. Clinician’s guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:191–225.
Fletcher GF, Ades PA, Kligfield P, Arena R, Balady GJ, Bittner VA, et al. Exercise standards for testing and training. Circulation. 2013;128:873–934.
Baba R, Nagashima M, Goto M, Nagano Y, Yokota M, Tauchi N, et al. Oxygen uptake efficiency slope: a new index of cardiorespiratory functional reserve derived from the relation between oxygen uptake and minute ventilation during incremental exercise. J Am Coll Cardiol. 1996;28:1567–72.
Kaminsky LA, Arena R, Myers J. Reference standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing data from the fitness registry and the importance of exercise national database. Mayo Clin Proc. 2015;90:1515–23.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). 2007 https://doi.org/10.1097/HJH.0b013e3281fc975a.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111–88.
Sateia MJ. International classification of sleep disorders-third edition. Chest. 2014;146:1387–94.
Marchesini G, Day CP, Dufour JF, Canbay A, Nobili V, Ratziu V, et al. EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. Obes Facts. 2016;9:65–90.
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–57.
Canning KL, Brown RE, Wharton S, Sharma AM, Kuk JL. Edmonton Obesity Staging System prevalence and association with weight loss in a publicly funded referral-based obesity clinic. J Obes. 2015;2015. https://doi.org/10.1155/2015/619734.
Guazzi M, Adams V, Conraads V, Halle M, Mezzani A, Vanhees L, et al. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2012;126:2261–74.
Mehra MR, Jessup M, Gronda E, Costanzo MR. Rationale and process: International Society for Heart and Lung Transplantation guidelines for the care of cardiac transplant candidates-2006. J Hear Lung Transplant. 2006;25:1001–2.
Malhotra R, Bakken K, D’Elia E, Lewis GD. Cardiopulmonary exercise testing in heart failure. JACC Hear Fail. 2016;4:607–16.
Swift DL, Lavie CJ, Johannsen NM, Arena R, Earnest CP, O’Keefe JH, et al. Physical activity, cardiorespiratory fitness, and exercise training in primary and secondary coronary prevention. Circ J. 2013;77:281–92.
Wasserman K, Hansen J, Sue D, Stringer W, Sietsema K, Sun X et al. Principles of exercise testing and interpretation. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2012.
Weisman IM, Weisman IM, Marciniuk D, Martinez FJ, Sciurba F, Sue D, et al. ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2003;167:211–77.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bettini, S., Quinto, G., Neunhaeuserer, D. et al. Edmonton Obesity Staging System: an improvement by cardiopulmonary exercise testing. Int J Obes 45, 1949–1957 (2021). https://doi.org/10.1038/s41366-021-00856-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00856-9
- Springer Nature Limited
This article is cited by
-
Phenotyping of Obesity Treatment Candidates: A Narrative Review
Current Obesity Reports (2024)
-
Updating obesity management strategies: an audit of Italian specialists
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2022)