Abstract
Objectives
To examine whether leisure time physical activity changes predict subsequent body mass index (BMI) changes, and conversely, whether BMI changes predict subsequent leisure time physical activity changes.
Methods
This prospective cohort study included adults attending ≥3 consecutive Tromsø Study surveys (time: T1, T2, T3) during 1974–2016 (n = 10779). If participants attended >3 surveys, we used the three most recent surveys. We computed physical activity change (assessed by the Saltin-Grimby Physical Activity Level Scale) from T1 to T2, categorized as Persistently Inactive (n = 992), Persistently Active (n = 7314), Active to Inactive (n = 1167) and Inactive to Active (n = 1306). We computed BMI change from T2 to T3, which regressed on preceding physical activity changes using analyses of covariance. The reverse association (BMI change from T1 to T2 and physical activity change from T2 to T3; n = 4385) was assessed using multinomial regression.
Results
Average BMI increase was 0.86 kg/m2 (95% CI: 0.82–0.90) from T2 to T3. With adjustment for sex, birth year, education, smoking and BMI at T2, there was no association between physical activity change from T1 to T2 and BMI change from T2 to T3 (Persistently Inactive: 0.89 kg/m2 (95% CI: 0.77–1.00), Persistently Active: 0.85 kg/m2 (95% CI: 0.81–0.89), Active to Inactive: 0.90 kg/m2 (95% CI: 0.79–1.00), Inactive to Active 0.85 kg/m2 (95% CI: 0.75–0.95), p = 0.84). Conversely, increasing BMI was associated with Persistently Inactive (odds ratio (OR): 1.17, 95% CI: 1.08–1.27, p < 0.001) and changing from Active to Inactive (OR: 1.16, 95% CI: 1.07–1.25, p < 0.001) compared with being Persistently Active.
Conclusions
We found no association between leisure time physical activity changes and subsequent BMI changes, whereas BMI change predicted subsequent physical activity change. These findings indicate that BMI change predicts subsequent physical activity change at population level and not vice versa.
Similar content being viewed by others
Introduction
The prevalence of overweight and obesity is continuously growing worldwide, and now over 50% of the population is classified as either overweight or obese in western high-income countries [1]. As overweight and obesity is associated with a substantial increased risk of non-communicable diseases and premature death [2], it is one of the greatest threats to public health in western high-income countries [1, 2].
Weight gain prevention at populational level is challenging. Obviously, excessive adiposity and weight gain are effects of an imbalanced energy intake and expenditure [3]. Thus, increasing physical activity levels could potentially serve as an effective public health strategy to prevent population weight gain [3, 4]. However, studies examining whether population levels of physical activity can prevent weight gain show conflicting results [4, 5], which may be attributed to methodological issues [5]. For example, although current weight is a strong predictor of future weight gain [5], some studies failed to adjust for baseline weight or body mass index (BMI) [6,7,8,9,10,11,12,13,14]. Moreover, most studies did not take the temporal reciprocal relationship between changing physical activity and weight into account [5], as they assessed the association between baseline physical activity level and future weight or BMI change [9, 10, 15,16,17,18,19,20,21,22]. Other studies examined the associations between change scores in both physical activity and weight or BMI [6, 8, 11,12,13,14, 23,24,25,26,27,28,29,30,31,32,33,34,35,36,37], which basically are cross-sectional analyses of change scores [5]. Finally, the association between physical activity and weight change may be reverse as weight change may lead to physical activity change [5, 6, 22, 25, 26, 35, 37,38,39], or this may be bidirectional [5].
Furthermore, the association between physical activity change and BMI change may be modified by other behavioural or societal factors, including sex [10], age [17, 18, 28,29,30], smoking [23, 29], education [24], physical activity domain (e.g., occupation or leisure time) [29], and baseline BMI [28, 29]. However, these observations are not consistent [12, 15, 26, 33], which warrant further investigation.
Declines in both leisure time and occupational physical activity may contribute to population BMI gains [4]. We have previously reported on the association between occupational physical activity and BMI change in a population-based cohort (The Tromsø Study) from Norway followed through repeated examinations every ~6 years. Our results suggested that occupational physical activity declines did not contribute to population BMI gains [40]. As large proportions of the population are inactive during work hours [41, 42], leisure time physical activity may have greater potential to prevent weight gain. Thus, the aims of this study were to assess: (1) Whether changes in leisure time physical activity from examination 1 (time (T) 1) to the next (T2) predicted subsequent changes in BMI from T2 to the next examination (T3), and (2) Whether BMI changes from T1 to T2 predicted subsequent leisure time physical activity changes from T2 to T3, with ~6 years follow up between each examination.
Materials and methods
Design
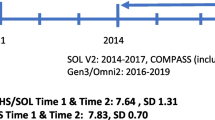
The study design is illustrated in Fig. 1. We studied participants from the Tromsø Study, a population-based cohort study in Tromsø Municipality, Norway. There are seven repeated Tromsø Study surveys (attendance of invited participants = %): 1974 (Tromsø 1; 83%), 1979–80 (Tromsø 2; 85%), 1986–87 (Tromsø 3; 81%), 1994–95 (Tromsø 4; 77%), 2001 (Tromsø 5; 79%), 2007–08 (Tromsø 6; 66%) and 2015–16 (Tromsø 7: 65%). Invited participants were selected from total birth cohorts and random samples of inhabitants in Tromsø municipality [41, 43]. Only men were invited to Tromsø 1 (1974), while in Tromsø 2–7 (1979–2016) both men and women were invited (details described elsewhere [41, 43]). In this study, we included participants attending at least three consecutive surveys (hereafter called T1, T2, T3). To assess the association between change in physical activity from T1 to T2 and change in BMI from T2 to T3, the inclusion criteria were information on: (1) physical activity at T1 and T2, and height and weight at T2 and T3; (2) information on educational level and smoking habits at T2; and (3) not pregnant at T2 and/or T3. We also reversed the analyses to assess whether BMI change from T1 to T2 predicted physical activity change from T2 to T3. Here, inclusion criteria were: (1) height and weight at T1 to T2, physical activity at T2 to T3; (2) educational level and smoking habits at T2; and (3) not pregnant at T1 and/or T2. If the participants attended more than three consecutive surveys, we used their data from the three most recent surveys in the analyses of the overall cohort, while their data could be included in multiple period-specific samples (Tromsø 1–3: 1974–1987, Tromsø 2–4: 1979–1995, Tromsø 5–7: 2001–2016).
Participants
Participant selection for our analyses is illustrated in Fig. 2. The overall cohort comprised 10779 participants, which derive from the participants´ three most recent Tromsø Study attendances. We also created period-specific samples where each participant may be included in multiple period-specific samples: Tromsø 1–3 (1974–1987, n = 3598), Tromsø 2–4 (1979–1995, n = 9691) and Tromsø 5–7 (2001–2016, n = 2206). Therefore, the period-specific samples do not add up to the overall cohort, which only includes participants with their three most recent consecutive surveys (Fig. 2).
The reversed analyses (BMI change from T1 to T2 followed by physical activity change from T2 to T3) were assessed in an overall cohort comprising 4385 participants (Fig. 3). The leisure time physical activity questionnaire was not included in Tromsø 4 and only those <70 years answered the questionnaire in Tromsø 5; this explains the lower sample size in the reversed analyses compared with the main analyses.
All participants from Tromsø 4–7 provided written informed consent and the present study was approved by the Regional Ethics Committee for Medical Research (ref. 2016/758410).
Self-reported physical activity
Physical activity was measured with the Saltin-Grimby Physical Activity Level Scale (SGPALS) questionnaire [44, 45], which asks participants to rank their physical activity by four hierarchical levels for leisure- and occupational time physical activity, separately, during the last 12 months [44]. The SGPALS in the Tromsø Study is slightly modified compared to the original by Saltin and Grimby [44] (Supplementary Table 1). The SGPALS is found to provide acceptable reliability [45] and validation studies have demonstrated acceptable ability to rank physical activity level when evaluated against accelerometry and cardiorespiratory fitness as the criterions [45].
Physical activity change was computed as (1) Persistently Inactive (reporting rank 1 at T1 and T2; n = 992); (2) Persistently Active (rank ≥ 2 at T1 and T2; n = 7314); (3) Active to Inactive (rank ≥ 2 at T1 and rank 1 at T2; n = 1167); and (4) Inactive to Active (rank 1 at T1 and rank ≥2 at T2; n = 1306).
The leisure time SGPALS was used in all Tromsø Study surveys except Tromsø 4 (1994–95), and in Tromsø 5 (2001) not by those ≥70 years. The occupational time SGPALS was used in all surveys by participants of all ages.
Body mass index and weight
Weight and height were measured in light clothing and are expressed as kilograms (kg) and metres (m). BMI was calculated as kg/m2 and categorized into normal weight (<25 kg/m2), overweight (25–29 kg/m2) and obese (≥30 kg/m2) for stratified analyses. Change in BMI from T2 to T3 was calculated with height being fixed at T2 and change in BMI from T1 to T2 fixed at T1, to avoid a possible effect of height loss between the measurements.
Confounders and effect modifiers
We included sex, birth year, smoking, education and BMI measured at T2 as confounders, and we also assessed potential effect modification of the confounders in addition to occupational physical activity change from T1 to T2. Data on smoking, education and occupational physical activity were retrieved from questionnaires. We categorized smoking into (1) Current smoker, (2) Previous smoker, and (3) Never smoker. The participants reported years of education in Tromsø 2 (1979–80), Tromsø 3 (1986–87) and Tromsø 5 (2001), which we categorized into (1) Primary school (<10 years), (2) High school (10–12 years), (3) University <4 years (13–15 years), and (4) University ≥4 years (≥16 years). In Tromsø 4 (1994–95) and Tromsø 6 (2007–08), the participants reported education with five response options, which included the four abovementioned groups and a fifth named “Technical school 2 years senior high” (vocational training), which we categorized as (2) High school.
Statistical analyses
Paired t tests were used to assess whether participants changed BMI from T2 to T3. Analyses of covariance (ANCOVA) were used to assess the association between physical activity change from T1 to T2 and BMI change from T2 to T3, adjusted for sex, birth year, smoking, education and BMI at T2. The ANCOVA was applied on the overall cohort and the period-specific samples, in total and stratified by sex, birth year, smoking, education and occupational physical activity change from T1 to T2. We interpreted the Q-Q plots of BMI change from T2 to T3 to not deviate from normal distribution. Although the Levene´s test of equality variance violated the assumption of homogeneity of variance across physical activity change groups (p < 0.001), we considered our large sample size in all physical activity change groups to make the ANCOVA robust for this heterogeneity. Interaction effects were tested between physical activity change and potential effect modifiers (sex, birth year, smoking, education and BMI at T2, and occupational time physical activity change from T1 to T2) in the overall cohort. We performed sensitivity analyses with leisure time physical activity change categorized into six groups; (1) Persistently Inactive, (2) Persistently Active, (3) Active but decreasing (rank 4 or 3 → 3 or 2), (4) Active and Increasing (rank 2 or 3 → 3 or 4), (5) Active to Inactive and (6) Inactive to Active. Alpha was set to 0.05 and data are shown as mean and 95% confidence intervals (CI) from t tests and ANCOVAs.
We performed multinomial logistic regressions to estimate odds ratios (OR) with 95% confidence intervals (CI) for changing leisure time physical activity from T2 to T3 per unit BMI change from T1 to T2, adjusted for sex, birth year, smoking and education at T2. The analyses were performed in the overall sample (n = 4385) and stratified by sex, birth year, smoking, education and occupational physical activity change (T1 to T2). We assessed interaction effects between BMI change and potential effect modifiers (sex, birth year, smoking, education and BMI at T2, and occupational physical activity change from T1 to T2). Persistently Active was set as reference category. We used the Statistical Package for Social Sciences (SPSS, Version 26, IBM, Armonk, NY, United States) for all statistical analyses.
Results
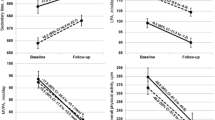
The descriptive characteristics at T2 for the overall cohort and period-specific samples (Tromsø 1–3, 1974–1987; Tromsø 2–4, 1979–1995; Tromsø 5–7, 2001–2016) are presented in Table 1. The participants increased their BMI from T2 to T3 (all p < 0.001), except for the Tromsø 5–7 sample (p = 0.96).
Change in BMI by preceding change in leisure time physical activity
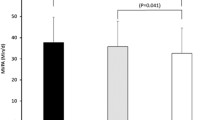
Changes in BMI by preceding leisure time physical activity change are presented in Table 2, and BMI at T2 and T3 by leisure time physical activity change are presented in Supplementary Table 2. In the overall cohort, we observed no differences in BMI change between categories of leisure time physical activity change (p = 0.84), and in general no associations in strata by sex, birth year, smoking, education and occupational physical activity change (Table 2).
In the period-specific sample Tromsø 5–7 (2001–2016), we observed differences in BMI change between the leisure time physical activity change groups, where those changing from Active to Inactive increased their BMI more than those changing from Inactive to Active (p = 0.01). In stratified analyses, higher BMI change was observed in those changing from Active to Inactive in men (p = 0.02) but not in women (p = 0.22), and among those born ≤1949 (p = 0.05). In those who never smoked, Persistently Inactive participants decreased their BMI more than those changing from Active to Inactive (p = 0.03). Finally, there were differences among the leisure time physical activity change groups among those having <4 years university education; those changing from Active to Inactive increased their BMI more than all other leisure time physical activity change groups (p = 0.003) (Supplementary Table 3). There were no differences in BMI increase by leisure time physical activity change in the Tromsø 1–3 (1974–1987) and Tromsø 2–4 (1979–1995) samples (Supplementary Table 4–5).
In the overall cohort, we observed no interaction for the association between leisure time physical activity change and BMI change by sex (p = 0.62), birth year (p = 0.23), smoking (p = 0.08) or BMI (p = 0.44) at T2, or occupational physical activity change from T1 to T2 (p = 0.10). However, we observed that education modified the association between leisure time physical activity change and BMI change (p = 0.002).
In the sensitivity analyses (in the overall cohort), with six physical activity change groups, the results were similar (Supplementary Table 6).
Change in leisure time physical activity with preceding BMI change
Participants who increased their BMI from T1 to T2 were more likely to be Persistently Inactive (OR: 1.17, 95% CI: 1.08 to 1.27 per 1 unit increase in BMI (kg/m2), p < 0.001) and to change from Active to Inactive (OR: 1.16, 95% CI: 1.07 to 1.25, p < 0.001) from T2 to T3 compared with those being Persistently Active at T2 and T3. Increasing BMI was not associated with changing from Inactive to Active (OR: 1.01, 95% CI: 0.94–1.08, p = 0.97) compared with those being Persistently Active at T2 and T3 (Table 3)
Sex, birth year, BMI, smoking and education at T2, and occupational physical activity change from T1 to T2, all modified the associations between BMI change and subsequent leisure time physical activity change (Table 3). Stratified analyses showed slight differences in ORs between strata. For example, men were more likely to be Persistently Inactive than Persistently Active per BMI-unit increase, while this was not observed in women. Those in higher birth year strata (1940–49, ≥1950) were more likely to be Persistently Inactive or changing from Active to Inactive with increasing BMI, which was not observed in those born ≤1939 (Table 3).
Discussion
In this prospective cohort study, we found no association between leisure time physical activity changes and subsequent BMI changes, whereas BMI increases predicted subsequent low and decreasing physical activity levels.
Most previous studies assessing the prospective association between leisure time physical activity and BMI either used baseline physical activity as the predictor [9, 10, 15,16,17,18,19,20,21,22,23, 30], which do not take temporal changes between physical activity and BMI into account [5], or assessed associations between change scores for both physical activity and BMI [6, 8, 11,12,13,14, 23,24,25,26,27,28,29,30,31,32,33,34,35,36,37], which basically are cross-sectional analyses that cannot provide an indication of the direction of the association [5]. One study examined the association between physical activity changes from a 1st to a 2nd examination and BMI changes from the 1st to a 3rd examination and found an association between physical activity decline and BMI gain [46]. Although assessing associations over three examinations are likely less influenced by confounding compared with two examinations, computing both exposure and outcome change from baseline still opens for reverse causation (i.e., weight gain potentially preceding physical activity decline). In the present study, we examined physical activity change from a 1st to a 2nd examination, followed by BMI change from the 2nd to a 3rd examination, which may be more suitable to assess the direction of the association, which provides an indication of causality [5].
Compared with the number of studies that examined whether physical activity is associated with BMI gain, fewer studies assessed a potential reverse association (i.e., BMI change predict physical activity change) [5]. In those that did, high baseline BMI [6, 37] and BMI gain [22, 25, 35, 37, 39] were associated with physical activity declines. In one study, baseline BMI, but not BMI changes, was associated with physical activity declines [26]. In a Mendelian randomization study, high body weight appeared causally associated with lower physical activity levels [38]. Thus, except for one previous study [26], our study corroborates previous studies, suggesting that BMI gain leads to lower physical activity level.
Lower physical activity levels following weight gain are likely due to movement limitations. In a case-control study of normal weight and obese adolescents, physical activity measured by accelerometry was substantially lower in obese individuals compared with their normal weight peers despite similar physical activity energy expenditures [47]. Similarly, this was also demonstrated in an experimental study of overfeeding with 4 MJ (1000 kilocalories (kcals)) per day over eight weeks, where free-living walking distances decreased due to lower walking velocity (i.e., movement limitation) in both normal weight and obese individuals following overfeeding, likely due to the increased weight [48].
Furthermore, our study contradicts a previous study, which reported that female but not male university alumni with high baseline BMI decreased their physical activity level over time [6], while we observed that both women and men were likely to decrease their physical activity with increasing BMI. This may be explained by demography (e.g., socioeconomic status, age) or by differences in analytical approach. In addition, we observed that sex, birth year, baseline (T2) BMI, smoking, education and occupational physical activity change all modified the association between BMI change and subsequent physical activity change. This indicates that the effect of BMI change on physical activity change is dependent on multiple behavioural and societal factors, which warrants additional research.
A pertinent question may be whether population levels of physical activity are sufficiently high to prevent weight gain. One previous study estimated that a physical activity energy expenditure increase of ~0.4 megajoule (MJ) (i.e., 100 kcals) per day would be sufficient to prevent weight gain at population level [49], which could be feasible for the general population. However, highly active women who performed 60 minutes per day of moderate intensity activity (considerably higher physical activity energy expenditure than 0.4 MJ per day) seemed to still gain weight, but at a lower rate than their less active peers, indicating that such physical activity levels at best mitigates weight gain [28]. Moreover, in another study, women and men being physically active at baseline had a lower baseline weight, but similar weight gain rate as those being inactive [26]. Energy intake has increased with ~2 MJ (i.e., 500 kcals) per day from the 1970 to 2000s in the United States, [50], which is similar to Western European countries from the 1960s to 2011 in a recent global study [51]. About 110–150 min of walking per day is needed to compensate for the increased energy intake of 2 MJ [50]. This is seven times more than the current minimal recommendations for physical activity of 150 minutes per week [52]. In Western high-income countries, one out of three fail to meet these recommendations [53]. Consequently, the current physical activity levels in the general population is unlikely preventing population weight gain [5].
Our study with a comprehensive analytical approach showed no association between leisure time physical activity change and subsequent BMI change. However, we observed that BMI gains were associated with subsequent lower leisure time physical activity, which is consistent with previous studies [6, 22, 25, 26, 35, 37, 38]. These observations are important, as public health initiatives aimed at weight gain prevention must acknowledge the major societal drivers for obesity in order to be successful [54, 55]. As physical activity has numerous health effects independent of weight change [56], it should not be neglected, but simply acknowledged in its limited potential for weight gain prevention [5]. Although still ineffective [57], well-designed whole system approaches targeting multiple factors associated with population weight gain may be needed to shift the current curve of the obesity epidemic [55, 57, 58].
Strengths and limitations
As BMI has gradually increased over decades [1], the long observation period in this study (~6 years between each examination) allowed us to examine whether physical activity change have affected the gradual long-term BMI gain [5]. Further, our analytical approach allowed us to interpret the direction of the association with more certainty [5]. Furthermore, the merged overall cohort increased our sample size, which allowed us to assess effect modification in the association between physical activity and BMI. Finally, the Tromsø Study cohorts have high attendance of invited participants, which indicate high generalizability to high-income countries´ populations [43].
There are also limitations that should be addressed. Self-reported physical activity change was categorized into crude groups; this may have introduced misclassification. Consequently, potential physical activity energy expenditure changes that could influence our results may have been missed. However, self-reported physical activity categorized into crude groups appears appropriate at population levels [59] and moreover, the SGPALS indicate predictive validity by being associated with multiple health outcomes [45]. Moreover, our sensitivity analysis of six groups physical activity change showed similar results as our main analyses. Further, self-reported physical activity is likely influenced by recall and social desirability bias, which indicate that over-reporting of physical activity levels is inevitable [59]. This is illustrated in our study by low variability in leisure time physical activity change, with most of the included participants (68%) being classified as Persistently Active. These biases are likely to under- or overestimate the effect magnitude between physical activity and health outcomes [5] and might have influenced our results. Future long-term studies using physical activity instruments with higher accuracy (e.g., device measured physical activity) are warranted to further examine whether population levels of physical activity influence weight change. Furthermore, disease onset may drive physical activity and weight change, which thus could be included as a potential confounder in our models. However, it is more likely that disease onset is a mediator (i.e. physical activity decline leads to disease, which leads to BMI change) or ancestor (i.e., disease onset leads to physical activity decline, which leads to BMI change) in the association between physical activity and BMI. Consequently, as our study´s aims were to assess the total effect of physical activity change on BMI change and vice versa, adjusting for disease would not assess the total effect [60]. Finally, our results may be influenced by residual confounding due to unavailable energy intake data.
Conclusion
In this prospective cohort study, there was no association between leisure time physical activity changes and subsequent BMI changes, whereas BMI increase was associated with subsequent consistently low and decreasing physical activity levels. These findings indicate that weight gain may lead to lower leisure time physical activity, while population levels of leisure time physical activity appears insufficient to prevent overweight and obesity.
Data availability
The data that support the findings of this study are available from the Tromsø Study but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. The data are however available from the Tromsø Study upon application to the Data and Publication Committee for the Tromsø Study: tromsous@uit.no.
References
NCD-RisC NRFC. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387:1377–96.
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27.
Hill JO, Wyatt HR, Peters JC. Energy balance and obesity. Circulation. 2012;126:126–32.
Jakicic JM, Powell KE, Campbell WW, Dipietro L, Pate RR, Pescatello LS, et al. Physical activity and the prevention of weight gain in adults: a systematic review. Med Sci Sports Exerc. 2019;51:1262–9.
Jones PR, Ekelund U. Physical activity in the prevention of weight gain: the impact of measurement and interpretation of associations. Curr Obes Rep. 2019;8:66–76.
Basterra-Gortari FJ, Bes-Rastrollo M, Pardo-Fernández M, Forga L, Martinez JA, Martínez-González MA. Changes in weight and physical activity over two years in Spanish alumni. Med Sci Sports Exerc. 2009;41:516–22.
Blanck HM, McCullough ML, Patel AV, Gillespie C, Calle EE, Cokkinides VE, et al. Sedentary behavior, recreational physical activity, and 7-year weight gain among postmenopausal U.S. women. Obesity (Silver Spring). 2007;15:1578–88.
Brown WJ, Kabir E, Clark BK, Gomersall SR. Maintaining a healthy BMI: data from a 16-year study of young Australian women. Am J Prev Med. 2016;51:e165–e78.
Hillemeier MM, Weisman CS, Chuang C, Downs DS, McCall-Hosenfeld J, Camacho F. Transition to overweight or obesity among women of reproductive age. J Womens Health. 2011;20:703–10.
Kaikkonen JE, Mikkilä V, Juonala M, Keltikangas-Järvinen L, Hintsanen M, Pulkki-Råback L, et al. Factors associated with six-year weight change in young and middle-aged adults in the Young Finns Study. Scand J Clin Lab Invest. 2015;75:133–44.
Rosenberg L, Kipping-Ruane KL, Boggs DA, Palmer JR. Physical activity and the incidence of obesity in young African-American women. Am J Prev Med. 2013;45:262–8.
Sjösten N, Kivimäki M, Singh-Manoux A, Ferrie JE, Goldberg M, Zins M, et al. Change in physical activity and weight in relation to retirement: the French GAZEL Cohort Study. BMJ Open. 2012;2:e000522.
Williams PT, Wood PD. The effects of changing exercise levels on weight and age-related weight gain. Int J Obes. 2006;30:543–51.
Williams PT, Thompson PD. Dose-dependent effects of training and detraining on weight in 6406 runners during 7.4 years. Obesity. 2006;14:1975–84.
Gebel K, Ding D, Bauman AE. Volume and intensity of physical activity in a large population-based cohort of middle-aged and older Australians: prospective relationships with weight gain, and physical function. Prev Med. 2014;60:131–3.
Gradidge PJ, Norris SA, Micklesfield LK, Crowther NJ. The role of lifestyle and psycho-social factors in predicting changes in body composition in Black South African women. PLoS One. 2015;10:e0132914.
MacInnis RJ, Hodge AM, Dixon HG, Peeters A, Johnson LE, English DR, et al. Predictors of increased body weight and waist circumference for middle-aged adults. Public Health Nutr. 2014;17:1087–97.
Sims ST, Larson JC, Lamonte MJ, Michael YL, Martin LW, Johnson KC, et al. Physical activity and body mass: changes in younger versus older postmenopausal women. Med Sci Sports Exerc. 2012;44:89–97.
Chiriboga DE, Ma Y, Li W, Olendzki BC, Pagoto SL, Merriam PA, et al. Gender differences in predictors of body weight and body weight change in healthy adults. Obesity. 2008;16:137–45.
Barone Gibbs B, Pettee Gabriel K, Carnethon MR, Gary-Webb T, Jakicic JM, Rana JS, et al. Sedentary time, physical activity, and adiposity: cross-sectional and longitudinal associations in CARDIA. Am J Prev Med. 2017;53:764–71.
Dugas LR, Kliethermes S, Plange-Rhule J, Tong L, Bovet P, Forrester TE, et al. Accelerometer-measured physical activity is not associated with two-year weight change in African-origin adults from five diverse populations. PeerJ. 2017;5:e2902.
Ekelund U, Kolle E, Steene-Johannessen J, Dalene KE, Nilsen AKO, Anderssen SA, et al. Objectively measured sedentary time and physical activity and associations with body weight gain: does body weight determine a decline in moderate and vigorous intensity physical activity? Int J Obes. 2017;41:1769–74.
Botoseneanu A, Liang J. The effect of stability and change in health behaviors on trajectories of body mass index in older Americans: a 14-year longitudinal study. J Gerontol A Biol Sci Med Sci. 2012;67:1075–84.
de Munter JS, Tynelius P, Magnusson C, Rasmussen F. Longitudinal analysis of lifestyle habits in relation to body mass index, onset of overweight and obesity: results from a large population-based cohort in Sweden. Scand J Public Health. 2015;43:236–45.
Drenowatz C, Gribben N, Wirth MD, Hand GA, Shook RP, Burgess S, et al. The association of physical activity during weekdays and weekend with body composition in young adults. J Obes. 2016;2016:8236439.
Hamer M, Brunner EJ, Bell J, Batty GD, Shipley M, Akbaraly T, et al. Physical activity patterns over 10 years in relation to body mass index and waist circumference: the Whitehall II cohort study. Obesity. 2013;21:E755–61.
Hankinson AL, Daviglus ML, Bouchard C, Carnethon M, Lewis CE, Schreiner PJ, et al. Maintaining a high physical activity level over 20 years and weight gain. JAMA. 2010;304:2603–10.
Lee IM, Djoussé L, Sesso HD, Wang L, Buring JE. Physical activity and weight gain prevention. JAMA. 2010;303:1173–9.
Moholdt T, Wisløff U, Lydersen S, Nauman J. Current physical activity guidelines for health are insufficient to mitigate long-term weight gain: more data in the fitness versus fatness debate (The HUNT study, Norway). Br J Sports Med. 2014;48:1489–96.
Parsons TJ, Manor O, Power C. Physical activity and change in body mass index from adolescence to mid-adulthood in the 1958 British cohort. Int J Epidemiol. 2006;35:197–204.
Smith KJ, Gall SL, McNaughton SA, Cleland VJ, Otahal P, Dwyer T, et al. Lifestyle behaviours associated with 5-year weight gain in a prospective cohort of Australian adults aged 26-36 years at baseline. BMC Public Health. 2017;17:54.
Kim Y, Lee JM, Kim J, Dhurandhar E, Soliman G, Wehbi NK, et al. Longitudinal associations between body mass index, physical activity, and healthy dietary behaviors in adults: a parallel latent growth curve modeling approach. PLoS ONE. 2017;12:e0173986.
Su C, Jia XF, Wang ZH, Wang HJ, Ouyang YF, Zhang B. Longitudinal association of leisure time physical activity and sedentary behaviors with body weight among Chinese adults from China Health and Nutrition Survey 2004-2011. Eur J Clin Nutr. 2017;71:383–8.
Brien SE, Katzmarzyk PT, Craig CL, Gauvin L. Physical activity, cardiorespiratory fitness and body mass index as predictors of substantial weight gain and obesity: the Canadian physical activity longitudinal study. Can J Public Health. 2007;98:121–4.
Drenowatz C, Hill JO, Peters JC, Soriano-Maldonado A, Blair SN. The association of change in physical activity and body weight in the regulation of total energy expenditure. Eur J Clin Nutr. 2017;71:377–82.
French SA, Mitchell NR, Hannan PJ. Decrease in television viewing predicts lower body mass index at 1-year follow-up in adolescents, but not adults. J Nutr Educ Behav. 2012;44:415–22.
Mortensen LH, Siegler IC, Barefoot JC, Grønbaek M, Sørensen TI. Prospective associations between sedentary lifestyle and BMI in midlife. Obesity. 2006;14:1462–71.
Richmond RC, Davey Smith G, Ness AR, den Hoed M, McMahon G, Timpson NJ. Assessing causality in the association between child adiposity and physical activity levels: a Mendelian randomization analysis. PLoS Med. 2014;11:e1001618.
Golubic R, Ekelund U, Wijndaele K, Luben R, Khaw KT, Wareham NJ, et al. Rate of weight gain predicts change in physical activity levels: a longitudinal analysis of the EPIC-Norfolk cohort. Int J Obes. 2013;37:404–9.
Sagelv EH, Ekelund U, Hopstock LA, Aars NA, Fimland MS, Jacobsen BK, et al. Do declines in occupational physical activity contribute to population gains in body mass index? Tromsø Study 1974–2016. Occup Environ Med. 2021;78:203–10.
Morseth B, Hopstock LA. Time trends in physical activity in the Tromsø study: an update. PLoS ONE. 2020;15:e0231581.
Church TS, Thomas DM, Tudor-Locke C, Katzmarzyk PT, Earnest CP, Rodarte RQ, et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS One. 2011;6:e19657.
Jacobsen BK, Eggen AE, Mathiesen EB, Wilsgaard T, Njølstad I. Cohort profile: the Tromsø Study. Int J Epidemiol. 2012;41:961–7.
Saltin B, Grimby G. Physiological analysis of middle-aged and old former athletes. Comparison with still active athletes of the same ages. Circulation. 1968;38:1104–15.
Grimby G, Börjesson M, Jonsdottir IH, Schnohr P, Thelle DS, Saltin B. The “Saltin-Grimby Physical Activity Level Scale” and its application to health research. Scand J Med Sci Sports. 2015;25:119–25. Suppl 4
Shibata AI, Oka K, Sugiyama T, Salmon JO, Dunstan DW, Owen N. Physical activity, television viewing time, and 12-year changes in waist circumference. Med Sci Sports Exerc. 2016;48:633–40.
Ekelund U, Åman J, Yngve A, Renman C, Westerterp K, Sjöström M. Physical activity but not energy expenditure is reduced in obese adolescents: a case-control study. Am J Clin Nutr. 2002;76:935–41.
Levine JA, McCrady SK, Lanningham-Foster LM, Kane PH, Foster RC, Manohar CU. The role of free-living daily walking in human weight gain and obesity. Diabetes. 2008;57:548–54.
Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science. 2003;299:853–5.
Swinburn B, Sacks G, Ravussin E. Increased food energy supply is more than sufficient to explain the US epidemic of obesity. Am J Clin Nutr. 2009;90:1453–6.
Dave D, Doytch N, Kelly IR. Nutrient intake: a cross-national analysis of trends and economic correlates. Soc Sci Med. 2016;158:158–67.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sport Med. 2020;54:1451–62.
Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Health. 2018;;6:e1077–e86.
Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378:804–14.
Vandevijvere S, Chow CC, Hall KD, Umali E, Swinburn BA. Increased food energy supply as a major driver of the obesity epidemic: a global analysis. Bull World Health Organ. 2015;93:446–56.
Warburton DER, Bredin SSD. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol. 2017;32:541–56.
Bagnall AM, Radley D, Jones R, Gately P, Nobles J, Van Dijk M, et al. Whole systems approaches to obesity and other complex public health challenges: a systematic review. BMC Public Health. 2019;19:8.
Lee BY, Bartsch SM, Mui Y, Haidari LA, Spiker ML, Gittelsohn J. A systems approach to obesity. Nutr Rev. 2017;75 Suppl 1:94–106.
Shephard R, Vuillemin A. Limits to the measurement of habitual physical activity by questionnaires. Br J Sports Med. 2003;37:197–206.
Aalen OO, Røysland K, Gran JM, Ledergerber B. Causality, mediation and time: a dynamic viewpoint. J R Stat Soc. 2012;175:831–61.
Acknowledgements
We would like to acknowledge Professor Bjarne Koster Jacobsen for valuable input on the study´s result and for revising working manuscript drafts.
Funding
The work of EHS is funded by Population Studies in the High North (Befolkningsundersøkelser i Nord: BiN). The remaining authors are funded by their respective positions/tenures. The funders had no role in the implementation and design of the study or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
EHS, BM, UE, LAH designed the study, EHS carried out data analysis, OL and TW provided statistical expertise, all authors interpreted the study results, EHS drafted the manuscript, and all authors contributed with manuscript revisions and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval and consent to participate
All participants from Tromsø 4–7 provided written informed consent and the present study was approved by the Regional Ethics Committee for Medical Research (ref. 2016/758410).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sagelv, E.H., Ekelund, U., Hopstock, L.A. et al. The bidirectional associations between leisure time physical activity change and body mass index gain. The Tromsø Study 1974–2016. Int J Obes 45, 1830–1843 (2021). https://doi.org/10.1038/s41366-021-00853-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00853-y
- Springer Nature Limited