Abstract
Background
Public health policies attempt to increase parental identification of child overweight and obesity. The objective of the present research was to determine the cross-sectional, prospective and longitudinal associations between parental identification of child overweight and child mental health problems.
Methods
We made use of two cohort studies of Australian (Longitudinal Study of Australian Children, LSAC) and Irish children (Growing up in Ireland Study, GUI) that measured parental identification of child overweight and child mental health problems. Participant included 6502 (LSAC) and 7503 (GUI) children (49% female) and their parents. Child mental health problems were measured using child, parent and teacher-reported Strengths and Difficulties Questionnaires (SDQ) at ages 9/10 years old to 12/13 years old. In all analyses we controlled for child Z-BMI.
Results
In LSAC children whose parents identified them as being overweight at age 10 experienced worse mental health at age 10 (β = 0.21, SE = 0.04) and age 12 (β = 0.13, SE = 0.04) than children whose parents failed to identify them as overweight. In GUI children whose parents identified them as being overweight at age 9 experienced worse mental health at age 9 (β = 0.20, SE = 0.04) and age 13 (β = 0.22, SE = 0.04). In LSAC parental identification of child overweight at age 10 did not significantly predict changes in mental health problems from age 10 to 12 (β = −0.02, SE = 0.03). In GUI parental identification of child overweight was predictive of increases in mental health problems from age 9 to 13 (β = 0.08, SE = 0.03).
Conclusions
Parental identification of child overweight and obesity is associated with worse child mental health, independent of child body weight. Parents should be aware of the potential stigma and mental health difficulties associated with labelling a child as overweight.
Similar content being viewed by others
Introduction
The number of children with overweight and obesity has increased dramatically in both the US and worldwide in the recent past [1, 2]. There is evidence obesity increases susceptibility to mental health problems [3, 4]. Because overweight and obesity track strongly from childhood into adulthood [5, 6] and there is a substantial health and economic burden of obesity [7], reversing childhood obesity is now considered a global public health challenge [8]. A likely consequence of increases in childhood obesity prevalence is that heavier body weights have become normal and because of this large numbers of parents fail to identify that their children are medically considered to be overweight or obese [9,10,11]. Because it is widely assumed that parental failure to identify child overweight and obesity will be to the detriment of child health [10, 12, 13], a number of public health interventions in the US and elsewhere aim to increase parental recognition of excess child overweight [14,15,16,17]. However, there have been concerns that such approaches may stigmatise children with overweight and obesity and negatively impact on their mental health [18, 19]. To date, there is a dearth of evidence on the associations between parental identification of child overweight and obesity and child mental health outcomes.
One hypothesis is that parental identification of child overweight may motivate parents to behave in a way that will promote weight loss or prevent further weight gain and in doing so benefit the child’s physical and mental health. In support of this argument, parental identification of child overweight has been shown in some studies to be associated with intentions to make healthy lifestyle changes to children’s diet or physical activity [20, 21], which in turn may benefit subsequent weight management and mental health during childhood. An alternative hypothesis is that parental identification of child overweight and obesity may be associated with negative health outcomes. Although some results have been mixed [22], a number of studies show that parental identification of child overweight and obesity is associated with increased child weight gain: a parent identifying that their child is overweight increases that child’s risk of gaining further weight [23,24,25]. An explanation for these findings is that parental identification of child overweight may result in parents behaving in ways that make children feel stigmatised and this negatively impacts the child’s body image, which in turn promotes further weight gain [26]. Consistent with this argument, a number of studies document that children with obesity experience stigma and teasing from family members because of their weight [27, 28]. Parental identification of child overweight could, therefore, affect child mental health by influencing parenting behaviour around body weight (e.g. drawing attention to or being critical about child weight) [29, 30].
Given that a number of public health approaches aim to increase parental identification of child overweight [14,15,16,17] and no studies to date have examined the association between parental identification of child overweight and child mental health outcomes, in the present research we analysed data from two large, longitudinal cohort studies. We assessed both the cross-sectional and prospective associations between parental identification of child overweight and child mental health problems. To determine generalisability we examined associations between parental identification of child overweight and child mental health problems in Australian and Irish children separately.
Methods
Longitudinal Study of Australian Children (LSAC)
Sample information
LSAC is a cohort study of Australian children and their families. Two cohorts of children have been followed longitudinally as part of LSAC since 2003-2004, the first cohort was aged 0-1 years old and the second was aged 4-5 years on recruitment. For detailed information on LSAC see [31]. We made use of data from both cohorts of children and focused our analyses on data collected when children in both cohorts were aged 10 and 12 years old, as parental reports of child weight status were available for the first time in both cohorts at age 10 and child mental health problems (Strengths and Difficulties Questionnaire, SDQ) were available at age 10 and 12. Survey weights were applied to account for differential attrition between waves and ensure sample representativeness. Written informed consent was obtained for participating families and study procedures were granted ethical approval by the Australian Institute of Family Studies Ethics Committee.
Measures
Parental identification of child overweight and obesity
As part of the in-home visit interview at age 10, parents (96% mothers) were asked ‘Which of these best describes your child?’ ‘underweight’, ‘normal weight’, ‘somewhat overweight’, ‘very overweight’. As in previous research [23, 24], ‘somewhat overweight’ or ‘very overweight’ were recoded to represent parental identification of child overweight.
Mental health problems
Children, parents and teachers of children completed the SDQ at age 10 and 12. The SDQ [32, 33] is a commonly used measurement tool to identify mental health problems in childhood and consists of 25 items (scored on a 1–3 scale of ‘Not true’, ‘Somewhat true’ and ‘Certainly true’). The SDQ can be summed to provide a total score, in addition to sub-scale scales for mental health problems relating to conduct problems (e.g. ‘I get very angry’), peer relationship problems (e.g. ‘I am usually on my own’), emotional symptoms (e.g. ‘I am often unhappy’), hyperactivity (e.g. ‘I am restless’) and prosociality (e.g. ‘I try to be nice to other people’). We averaged child, mother, father, and teacher scores on the SDQ to account for potential reporting biases associated with reliance on only one reporter [34, 35]. Parental and teacher items of the SDQ are harmonised to be similar to child items (e.g. ‘I try to be nice to other people’ vs. ‘Considerate of other people’s feelings’). For 5995 children (92%) at least 3 reports were available and in the remaining 507 (8%) we averaged the 2 available reports; 69 children were not included because only 1 report was available.
Child BMI
Child weight and height were measured by trained research staff during an in-home visit. Bathroom glass scales were used to measure weight. Height was measured using a portable stadiometer. Age and sex-specific child BMI-Z scores based on the Centres for Disease Control and Prevention (CDC) growth charts [36] were calculated. Eleven participants were excluded from the analysis because of BMI-Z scores were outside the plausible range (BMIs under 8 or over 40) [37].
Covariates
Demographic variables (all self-reported by parents) were included in analyses; child sex, child age, household income (log transformed), child ethnicity, any child chronic health conditions, language other than English spoken at home. In supplementary analyses we controlled for mother BMI (researcher staff measured, as described above) and mother depressive symptoms (measured via the K6 Distress Scale [38]). To maximise the sample size missing data on these two variables (≈6% of observations) was replaced using mean imputation.
Response rate
A total of 7933 families were available at baseline (age 10 across both cohorts) from LSAC. Of these families, 6502 children and their parents had complete data at baseline (age 10) and 5876 had baseline and follow up data (age 12) and were included in our prospective/longitudinal analyses. Children who did not have complete baseline data (for the purpose of our analyses) were more likely to be from an indigenous background, spoke a language other than English at home, and had lower household income than children with complete baseline data (all ps < 0.01). There was no difference on other key covariates (age, sex, and BMI level).
Growing up in Ireland (GUI)
Sample information
GUI is a large-scale longitudinal study of the health and well-being of children living in the Republic of Ireland, Europe. A cohort of 8568 9-year-old children was recruited in 2007-2008 via random sampling within the national primary school system. Interviews were conducted in the child’s home at baseline (2007-2008) and follow-up four years later when the child was aged 13 (2011-2012). We made use of data collected at age 9 and age 13, as these were the first waves of data collection with parental perception of child weight and child mental health problems were measured. Written informed consent was obtained from children and a parent or guardian. GUI was approved by the ethics committee at the Health Research Board, Dublin, Ireland. Survey weights were applied to account for differential attrition between waves and ensure sample representativeness. For detailed information about GUI, see [39].
Measures
Parental perceptions of weight status
As part of the in-home visit interview at age 9, parents (98% mothers) were asked ‘Which do you think your child is’ ‘very underweight’, ‘moderately underweight’, ‘slightly underweight’, ‘about the right weight’, ‘slightly overweight’, ‘moderately overweight’, ‘very overweight’. If a parent selected ‘slightly’, ‘moderately’ or ‘very’ ‘overweight’, this represented parental identification of child ‘overweight’. Parents were considered to have classified their child as ‘underweight’ if they responded ‘very underweight’, ‘moderately underweight’, or ‘slightly underweight’.
Mental health problems, child BMI and other variables
Mental health difficulties were assessed using the SDQ which was completed by the primary caregiver only in GUI. Child BMI Z-scores were measured as in LSAC. Ten participants were excluded because of values outside the plausible range (BMIs under 8 or over 40) [37]. Demographic variables were parent reported in 2007-2008. Specifically, we included covariates assessing the child’s age and sex, whether the primary caregiver was a native English speaker, whether the child was born outside of Ireland, household income, and whether the child has any on-going long-term “physical or mental health problems, illness or disability”. In a further analysis we incorporated additional controls for parents’ (measured) BMI and parents’ depressive symptoms, assessed using the Centre for Epidemiological Studies Depression Scale (eight-item) (CESD-8) screening instrument [40]. To maximise the sample size missing data on these two variables (≈7% of observations) was replaced using mean imputation.
Response rate
A total of 8568 children were recruited and consented into GUI. Of these families, 7503 children and their parents had complete data at baseline (age 9) and 6633 had baseline and follow up data (age 13) and were included in our prospective/longitudinal analyses. Children who did not have complete baseline vs. complete baseline data (for the purpose of our analyses) did not differ on key covariates (age, sex, whether born outside Ireland, chronic medical conditions, language other than English spoken by primary caregiver and BMI level) with the exception of income. Those with complete baseline data had household income levels that were larger (p = 0.045) than those with incomplete data.
Main analysis strategy
Primary analyses
We followed the same analytic strategy in LSAC and GUI. In all analyses we compared parental identification of child overweight to parental identification of child normal weight. We first examined the cross-sectional association (age 10 LSAC, age 9 GUI) between parental identification of child overweight and SDQ scores (total and subscale totals) using OLS linear regression models, controlling for demographic variables (see method). In a set of sensitivity analyses with reduced sample size we also examined the effect of controlling for mother BMI and mother depressive symptoms measured at baseline. Next, we used the same approach in a set of prospective analyses to examine whether parental identification of child overweight (age 10 LSAC, age 9 GUI) was associated with future SDQ scores (age 12 LSAC, age 13 GUI). To examine whether parental identification of child overweight predicted longitudinal changes in SDQ scores over time, we used the same approach to predict follow-up SDQ scores (age 12 LSAC, age 13 GUI), controlling for baseline SDQ scores (age 10 LSAC, age 9 GUI). All outcome variables were standardized to have a mean of zero and standard deviation of one. Analyses were conducted in SPSS and results were considered significant at p < 0.05 in our main analyses
Results
Sample characteristics
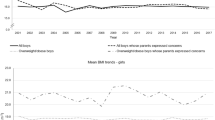
At baseline (age 10) in LSAC, 25% of children were classed as having overweight or obese. The sample was predominantly Caucasian and 16% of children were identified by their parent as being overweight. At baseline (age 9) in GUI, 29% of children were classed as having overweight or obese. The sample was predominantly born in Ireland and 15% of children were identified by their parent as having overweight. See Table 1 for sample characteristics.
Cross-sectional associations between identification of overweight and child mental health
In LSAC and GUI parental identification of child overweight was associated with worse overall mental health (SDQ total score) when measured concurrently in models that adjusted for baseline covariates. The same pattern of results was also observed for SDQ subscales of hyperactivity, emotional symptoms, peer problems, conduct problems, but not prosociality (either sample). Results remained significant in sensitivity analyses controlling for parental BMI and depressive symptoms. See Table 2.
Prospective associations between identification of overweight and child mental health
In LSAC and GUI parental identification of child overweight was prospectively associated with worse overall mental health (SDQ total score) and these results remained significant in sensitivity analyses. The same pattern of results was observed for SDQ subscales, except for prosociality in both cohorts and hyperactivity and conduct problems in LSAC. See Table 2.
Parental identification of overweight and longitudinal changes in child mental health
In LSAC parental identification of child overweight was not associated with changes in child mental health over time. In GUI parental identification of child overweight was associated with worsening overall child mental health (SDQ total). In particular, parental identification was associated with increases in emotional symptoms and peer relationship problems. These associations remained significant in sensitivity analyses controlling for parental BMI and depressive symptoms. See Table 2.
Further analyses: parental identification of underweight and exclusion of children with underweight
Analyses also allowed for the comparison of parent perceived underweight vs. parent perceived normal weight. See Table S1. As there were few children with underweight and few parents identified their children as underweight, the results of these analyses should be interpreted with caution. In LSAC and GUI, parent perceived child underweight tended to be associated with worse child mental health outcomes cross-sectionally and prospectively. Identification of underweight was not reliably associated with changes in mental health. We also examined the effect of removing children with underweight (based on Z-BMI) on the associations between identification of overweight and child mental health and results remained the same as in our main analyses. See Tables S2 and S3.
Further analyses: controlling for child perception of weight status
One potential explanation of the associations observed between parental identification of child overweight and child mental health outcomes could be that parental identification of child overweight is merely a proxy measure of child body image/perceived body size. In both LSAC and GUI, children completed self-report measures of their own perceived body size at baseline. To test this explanation we, therefore, examined the effect of including child perceived body weight as a covariate in our primary analysis. Although child perceived body weight tended to be associated with total SDQ scores (higher perceived body weight associated with worse mental health outcomes), results for parental identification of child overweight and SDQ scores remained significant in both studies. See Tables S4–S6.
Exploratory analyses: sex, child weight and parental identification of overweight
To examine whether associations differed by child sex or child weight (Z-BMI), in exploratory analyses we included interaction terms between sex and child weight with parental identification of child overweight in models predicting SDQ total score. To account for multiple comparisons we considered results significant at p < 0.01 in these analyses. There was no evidence of moderation by child sex or weight in either LSAC or GUI. In addition, we reran the main analysis limited to children with overweight and obesity. Results from this reduced sample size analysis produced similar results to the main analysis. See Table S7.
Exploratory analyses: LSAC vs. GUI differences in SDQ respondents
In LSAC, we were able to draw on multiple respondents reporting on child mental health, but GUI only had SDQ data from parents. However, limiting analyses in LSAC to parent-reported SDQ (data not reported) did not result in a significant longitudinal effect on total SDQ score (as observed GUI), indicating that this minor methodological difference does not account for the difference in findings between the two studies.
Discussion
Across two cohort studies of Australian and Irish children, we find that a parent recognising that their child has overweight was associated (independent of child weight) with that child being at an increased risk of experiencing mental health problems and this effect persists over time (prospective analysis). Parental recognition of child overweight was also associated with worsening child mental health (longitudinal change analysis) over two years in the sample of Irish children, but not Australian children. The effects of parental recognition of child overweight on mental health problems were observed consistently for both girls and boys and were not dependent on degree of child adiposity. In addition, an analysis limited to children with overweight and obesity only produced similar findings to the main analyses.
There is a well-established association between obesity and mental health problems that is observed during mid-childhood [4]. The present results indicate that children whose parents identify that they have overweight are particularly likely to experience mental health difficulties. One potential explanation of these findings is that parental identification may impact on weight-related parenting and this results in a child identifying experiencing emotional problems because of the stigma attached to heavier body weight. In line with this interpretation, we found that parental identification of child overweight was most consistently associated with the emotional problems facet of mental health difficulties. In additional analyses we found that the significant association between parental identification of child overweight and mental health problems remained after accounting for measures of child perceived body size (which themselves tended to be associated with worse mental health outcomes). This finding suggests that parental identification of child overweight being associated with worse child mental health outcomes is unlikely to be explained by parental identification being a mere proxy measure of child identification of overweight. Overall, the present findings reinforce the need for parents to be sensitive to the potential stigma and mental health difficulties associated with a child being labelled as overweight [41].
The present findings may also have implications for public health policy. Large numbers of parents fail to identify that their children have overweight or obesity and this has resulted in state-level intervention approaches to improve parental recognition of overweight and obesity [16, 19]. The potential adverse effects of parental identification of child overweight and obesity have been raised [18] and a large amount of research has shown there is considerable stigma directed towards and experienced by children of heavier body weight [42]. However, the present study is the first to examine the mental health outcomes among children whose parents do vs. do not identify their overweight and obesity. The findings of the present study, in addition to recent research showing that parental identification of child overweight is associated with increased child weight gain [24, 26], indicate that intervention approaches need to be aware of the potential adverse consequences of raising awareness of child overweight.
Strengths of the present study include the use of two large cohort studies in which we were able to examine both cross-sectional, prospective and longitudinal (change) associations, whilst controlling for a range of potential confounders (e.g. maternal BMI, maternal depressive symptoms, objectively measured child weight). Our study also measured mental health problems using a validated and widely used instrument (SDQ). We also replicated findings across two samples and this allows for conclusions concerning the generalisability of findings. Findings were very similar across both data sets, although the longitudinal effect of parental identification of child overweight on worsening total SDQ score was observed only in the Irish sample and further research examining why and whether these effects translate to other countries (e.g. US) is now needed. In LSAC we were able to draw on multiple respondents reporting on child mental health, but GUI only had SDQ data from parents. However, limiting analyses in LSAC to parent-reported SDQ (data not reported) did not result in a significant longitudinal effect on total SDQ score (as observed GUI), indicating that this minor methodological does not account for the difference in findings between the two studies.
We cannot infer causality from this observational study and although we controlled for a range of potential confounders, there may be other variables or residual confounding that explain the association between parental identification of child overweight and child mental health problems. Further work examining the potential behavioural (e.g. parenting practices) and/or psychological (e.g. child body dissatisfaction) consequences of parental identification of child overweight would therefore now be valuable. A limitation is that we were only able to examine child mental health problems from age 9/10 to 12/13 years. Both parental identification of child overweight and child mental health problems may occur prior to this [4, 11]. Therefore, longitudinal research tracking the temporal order and occurrence of parental identification of child overweight and the emergence of child mental health problems is needed. As the present samples were predominantly white, we cannot infer whether our findings would generalise to other ethnicities. Finally, the SDQ does not include measurement of child-eating pathology or body dissatisfaction and examining whether parental identification of child overweight is also associated with these mental health outcomes would now be informative.
Conclusions
Across two cohort studies of Australian and Irish children, in both cross-sectional and prospective analyses we find that a parent recognising that their child has overweight places that child at an increased risk of experiencing mental health problems, independent of the child’s measured body mass index. Both public health intervention approaches and parents need to be aware of the stigma and mental health difficulties associated with labelling a child as overweight.
References
de Onis M, Blossner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr. 2010;92:1257–64.
Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Rel Metabol Disord. 1998;22:39–47.
Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch General Psychiatry. 2010;67:220–9.
Patalay P, Hardman CA. Comorbidity, codevelopment, and temporal associations between body mass index and internalizing symptoms from early childhood to adolescence. JAMA Psychiatry. 2019;76:721–9.
Kvaavik E, Tell GS, Klepp K-I. Predictors and tracking of body mass index from adolescence into adulthood: follow-up of 18 to 20 years in the Oslo Youth Study. Arc Pediatrics Adolesc Med. 2003;157:1212–8.
Simmonds M, Llewellyn A, Owen C, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta‐analysis. Obes Rev. 2016;17:95–107.
Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. The Lancet. 2011;378:815–25.
Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5:4–85.
Robinson E. Overweight but unseen: a review of the underestimation of weight status and a visual normalization theory. Obes Rev. 2017;18:1200–9.
Lundahl A, Kidwell KM, Nelson TD. Parental underestimates of child weight: a meta-analysis. Pediatrics. 2014;133:e689–703.
Carnell S, Edwards C, Croker H, Boniface D, Wardle J. Parental perceptions of overweight in 3–5 y olds. Int J Obes. 2005;29:353–5.
Duncan DT. Parental misperception of their child’s weight status: clinical implications for obesity prevention and control. Obesity. 2011;19:2293–2293.
Duncan DT, Hansen AR, Wang W, Yan F, Zhang J. Change in misperception of childas body weight among parents of American Preschool Children. Childhood Obesity. 2015;11:384–93.
Falconer CL, Park MH, Croker H, et al. The benefits and harms of providing parents with weight feedback as part of the national child measurement programme: a prospective cohort study. BMC Public Health. 2014;14:549.
Grimmett C, Croker H, Carnell S, Wardle J. Telling parents their child’s weight status: psychological impact of a weight-screening program. Pediatrics. 2008;122:e682–688.
Thompson JW, Card-Higginson P. Arkansas’ experience: statewide surveillance and parental information on the child obesity epidemic. Pediatrics. 2009;124:S73–82.
Evans EW, Sonneville KR. BMI report cards: will they pass or fail in the fight against pediatric obesity? Current Opin Pediatrics. 2009;21:431–6.
Ikeda JP, Crawford PB, Woodward-Lopez G. BMI screening in schools: helpful or harmful. Health Education Res. 2006;21:761–9.
Thompson HR, Madsen KA. The report card on BMI report cards. Current Obes Rep. 2017;6:163–7.
Park MH, Falconer CL, Croker H, et al. Predictors of health-related behaviour change in parents of overweight children in England. Prev Med. 2014;62:20–24.
Sylvetsky-Meni AC, Gillepsie SE, Hardy T, Welsh JA. The impact of parents categorization of their own weight and their childs weight on healthy lifestyle promoting beliefs and practices. J Obes. 2015;2015:7.
Parkinson KN, Reilly JJ, Basterfield L, et al. Mothers’ perceptions of child weight status and the subsequent weight gain of their children: a population-based longitudinal study. Int J Obes. 2017;41:801.
Gerards SM, Gubbels JS, Dagnelie PC, et al. Parental perception of child’s weight status and subsequent BMIz change: the KOALA birth cohort study. BMC Public Health. 2014;14:291.
Robinson E, Sutin AR. Parental perception of weight status and weight gain across childhood. Pediatrics. 2016:e20153957.
Min J, Wang VHC, Xue H, Mi J, Wang Y. Maternal perception of child overweight status and its association with weight-related parenting practices, their children’s health behaviours and weight change in China. Public Health Nutrition. 2017;20:2096–103.
Robinson E, Sutin AR. Parents’ perceptions of their children as overweight and children’s weight concerns and weight gain. Psychol Sci. 2017;28:320–9.
Berge JM, Trofholz A, Fong S, Blue L, Neumark-Sztainer D. A qualitative analysis of parents’ perceptions of weight talk and weight teasing in the home environments of diverse low-income children. Body Image. 2015;15:8–15.
Neumark-Sztainer D, Bauer KW, Friend S, Hannan PJ, Story M, Berge JM. Family weight talk and dieting: how much do they matter for body dissatisfaction and disordered eating behaviors in adolescent girls? J Adolesc Health. 2010;47:270–6.
Gillison FB, Lorenc AB, Sleddens EFC, Williams SL, Atkinson L. Can it be harmful for parents to talk to their child about their weight? A meta-analysis. Prev Med. 2016;93:135–46.
Madowitz J, Knatz S, Maginot T, Crow SJ, Boutelle KNTeasing. depression and unhealthy weight control behaviour in obese children. Pediatric Obes. 2012;7:446–52.
Growing up in Australia, Longitudinal Study of Australian Children. http://www.growingupinaustralia.gov.au/pubs/technical/tp1.pdf. Accessed 13 Sep 19.
Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. 1997;38:581–6.
Davis E, Sawyer MG, Lo SK, Priest N, Wake M. Socioeconomic risk factors for mental health problems in 4–5-year-old children: Australian population study. Acad Pediatrics. 2010;10:41–47.
Muris P, Meesters C, Eijkelenboom A, Vincken M. The self-report version of the strengths and difficulties questionnaire: its psychometric properties in 8- to 13-year-old non-clinical children. Brit J Clin Psychology. 2004;43:437–48.
De Los Reyes A, Thomas SA, Goodman KL, Kundey SM. Principles underlying the use of multiple informants’ reports. Ann Rev Clin Psychol. 2013;9:123–49.
Must A, Anderson SE. Body mass index in children and adolescents: considerations for population-based applications. Int J Obes. 2013;30:590–4.
Lobstein TJ, James WPT, Cole TJ. Increasing levels of excess weight among children in England. Int J Obes. 2003;27:1136–8.
Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60:184–9.
Growing Up In Ireland. http://www.growingup.ie/fileadmin/user_upload/documents/Technical_Reports/DIPR_Template_05.10.2010.pdf. Accessed 01 Aug 2019.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Haynes A, Kersbergen I, Sutin A, Daly M, Robinson E. Does perceived overweight increase risk of depressive symptoms and suicidality beyond objective weight status? A systematic review and meta-analysis. Clin Psychol Rev. 2019:101753.
Puhl RM, Latner JD. Stigma, obesity, and the health of the nation’s children. Psychol Bull. 2007;133:557.
Author information
Authors and Affiliations
Contributions
All authors conceived and designed the study. MD and AS analysed the data. ER drafted the manuscript. All authors revised the manuscript, contributed to the intellectual content and approved the final version. All authors are accountable for the accuracy and integrity of the work.
Corresponding author
Ethics declarations
Conflict of interest
MD and AR report no conflict of interests. ER has previously received funding from Unilever and the American Beverage Association, but does not consider this to be a conflict of interest for the present work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Robinson, E., Daly, M. & Sutin, A. Association of parental identification of child overweight and mental health problems during childhood. Int J Obes 44, 1928–1935 (2020). https://doi.org/10.1038/s41366-020-0587-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-0587-6
- Springer Nature Limited