Abstract
Background
Current evidence supports the association between the high sperm DNA fragmentation (SDF) and the poor fertilization rate following either natural conception or assisted reproductive techniques (ART). On the other hand, there are conflicting results regarding the decreased sperm DNA integrity in men with high body mass index (BMI).
Objective
We aimed at the present systematic review and meta-analysis at evaluating the association between BMI and SDF.
Methods
We searched databases of Medline, Embase, Scopus, and Web of Science up to May 2019, to identify observational studies that assessed the associations between BMI and SDF. BMI was classified, according to the standard BMI classifications, into six categories including underweight (<18.5), normal weight (18.5–24.99), overweight (25–29.99), class I obesity (30–34.99), class II obesity (35–39.99), and class III obesity (≥40). Standardized mean differences (SMDs) and 95% confidence intervals (CIs) of SDF were calculated by using a random-effects model for BMI categories.
Results
The initial extensive literature search yielded 33,739 potentially relevant articles (3,917 from Medline, 781 from Embase, 12,685 from Scopus, and 9,348 from Web of Science). Fourteen studies (nine cross-sectional, four cohort, and one case–control studies), with a total number of 8,255 participants, were included in the meta-analysis. Finally, three studies reported higher SDF levels in obese men (BMI = 30–34.99) compared with normal-weight men (BMI < 25) (SMD: 0.23, 95% CI: 0.01, 0.46, P = 0.05, I2 = 0%), but there was no difference between other categories.
Conclusions
There is insufficient data to demonstrate a positive association between BMI and SDF. Our findings provide a rationale for conducting further cohort studies for evaluation of the association between BMI and SDF, considering potential confounders.
Similar content being viewed by others
Introduction
It has been proven that the high level of sperm DNA fragmentation (SDF) (≥30%) reduces fertilization and pregnancy rates following either natural conception or assisted reproductive techniques (ART) [1]. The main etiology of SDF is complex and still unclear, but it can be caused by defects in spermatogenesis following testicular and post-testicular injuries like toxins, hyperthermia, oxidants, and hormonal disorders [2]. Obesity is one of the potential lifestyle factors that can increase oxidative stress (OS) levels and consequently DNA damage, in different body organs [3, 4], including testis and germinal cells [5]. Due to the changes toward a more sedentary lifestyle, as well as dietary changes, obesity is currently a cause of concern worldwide and has even reached epidemic proportions in several countries. Individuals with obesity or overweight currently represent more than two-thirds of the population of developed and developing countries. Previous studies showed a decline in sperm DNA integrity in parallel to the obesity epidemic. Nevertheless, the studies addressing the specific association between obesity and SDF have yielded contradictory results. Although some recent data suggest a correlation between the increase in obesity and a reduction in sperm integrity, other studies did not detect statistically significant adverse effects [6,7,8,9,10,11]. Given the discrepancies among study results and the belief that an understanding of the association between obesity and SDF will allow better counseling of infertile couples, we aimed at determining the association between BMI and SDF in this systematic review and meta-analysis.
Methods
Search strategy and selection criteria
A systematic review and meta-analysis were done according to the Meta-analysis of Observational Studies in Epidemiology guidelines. Published and unpublished observational studies have been sought by computer-aided literature searches, manual searches of citations and reference lists of the identified studies, and pertaining review papers. The following electronic databases were searched: Medline (through PubMed), Embase, Scopus, and Web of Science, from inception until May 2019. Search terms included “DNA Fragmentation” OR “sperm DNA damage” OR “sperm DNA integrity” OR “human sperm chromatin” OR “Apoptotic DNA Degradation” AND “obesity” OR “adiposity” OR “body mass index” OR “overweight” OR “Quetelet Index” OR “bodyweight” OR “weight” OR “body fat” OR “body mass”. Full details of the search strategy-used terms and database-specific indexing terminology are provided in Supplementary Table 1. We selected studies that meet the following criteria: (1) observational studies (cohort, case–control, and cross-sectional) that evaluated the associations of BMI and SDF, as assessed by the DNA fragmentation index (DFI), (2) SDF detected by the Sperm Chromatin Structure Assay (SCSA), the Sperm Chromatin Dispersion test, the Terminal deoxynucleotidyl transferase, dUTP Nick-End Labeling (TUNEL) assay, or the single-cell gel electrophoresis (Comet) assay, and (3) categorized BMI into six groups: underweight (<18.5), normal weight (18.5–24.99), overweight (25–29.99), class I obesity (30–34.99), class II obesity (35–39.99), and class III obesity (≥40). We excluded studies if (1) they were designed as interventional study (trials and studies undertaken to assess the effects of any intervention), review, case reports, case series, animal studies, cell experiment, and laboratory-based research; (2) we were not able to extract the exact details about the research method or results; (3) presented only as abstracts or conference paper.
Selection of articles and data extraction
Studies were selected in a two-stage process. First, all titles and abstracts in database results were scrutinized for relevance to this systematic review. Second, the full texts of relevant articles were read, and all studies that potentially meet the selection criteria were obtained. The final decision on inclusion or exclusion of the studies was made on the evaluation of the full papers. In cases of duplicate publication, the most recent and complete versions were selected. Methodological quality appraisal was completed by using the Newcastle–Ottawa Quality Assessment Scales for observational studies (NOS). The NOS is a validated tool for assessing the quality of nonrandomized studies in meta-analyses, which uses a star system based on three components: the selection of the study groups (up to four points), comparability of the groups (up to two points), and exposure or outcome (up to three points). Data extraction was conducted for each retrieved article using a standardized, pilot-tested data collection form. Information was extracted from each study regarding author names, publication year, location, study design, type of participants (people with infertility or healthy), the sample size in each BMI category, age of participants, SDF damage assay, and mean ± standard deviation of SDF in each BMI category. All stages were conducted independently by two reviewers (MS and MR). Any disagreements were resolved by the discussion or arbitration by a third reviewer (AM-H).
Statistical analyses
BMI was categorized into six categories to denote the standard BMI classifications of underweight (<18.5), normal weight (18.5–24.99), overweight (25–29.99), class I obesity (30–34.99), class II obesity (35–39.99), and class III obesity (≥40). Standardized mean differences (SMDs) and 95% confidence intervals (CIs) of SDF were calculated for BMI categories. Extracted SMDs from primary studies were pooled using inverse-variance weighted random-effects model. To investigate whether the results of the meta-analysis depended on a particular study or group of studies, we recomputed the meta-analysis statistic after omitting one study at a time (sensitivity analysis). Heterogeneity was evaluated graphically using forest plots and statistically using the Higgins I2 statistic that measures the percentage of total variation across studies that are due to heterogeneity rather than chance. In addition, we assessed the probability of publication bias with the Egger’s test, with a P value < 0.10 considered representative of statistically significant publication bias. All comparisons were two-tailed, and 95% CIs were described where applicable. Statistical analyses were performed using RevMan5.3 (Cochrane Collaboration, Oxford, UK) and Stata13.0 (Stata Corp, TX, USA).
Results
Literature search
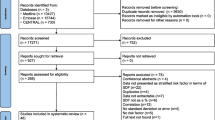
The initial extensive literature search yielded 33,739 potentially relevant articles (3,917 from Medline, 781 from Embase, 12,685 from Scopus, and 9,348 from Web of Science). Following the removal of duplicate articles and the addition of studies by hand searching (eight studies), 9,647 studies were identified to be potentially eligible for inclusion. Of these, 9,614 were excluded from the studies based on their titles (n = 8,217) and abstracts (n = 1,397). Full texts of 33 studies were retrieved as they addressed the study question, but 19 studies were excluded because they did not qualify eligibility criteria. Finally, 14 studies met all of the inclusion criteria and were included in the meta-analysis (Fig. 1).
Study characteristics
Table 1 outlines the main characteristics of the included studies. The 14 studies, including ten cross-sectional and four cohort studies, were published between 2006 and 2018. The studies were conducted in the United States (three studies) [7, 9, 12], Brazil (two studies) [11, 13], Norway (two studies) [14, 15], France (one study) [8], Denmark (one study) [16], China (one study) [10], Egypt (one study) [17], South Africa (one study) [18], Czech Republic (one study) [19], and one in Europe (Ukraine, Poland, Sweden, and Norway) [6]. The sample sizes ranged from 42 to 2,321 participants.
Methodological assessment
A summary of methodological quality appraisal is shown in Supplementary Table 2. In cross-sectional studies, five (50%) were of high quality with an average NOS score of 9.2, and five (50%) showed moderate quality with an average NOS score of 6.8. All studies, except two, selected representative samples from the population. All cohort studies selected their exposed and nonexposed participants from the same community sample. All studies provided adequate criteria for the diagnosis of the outcomes of interest and provided a proper description of how the outcomes were measured. There was no description of the response rate or the characteristics of the responders and nonresponders in all cross-sectional studies.
The mean of DFI in BMI categories
Men with obesity (BMI > 30) compared with men with normal weight (BMI = 18.5–24.99)
Six studies with a total number of 3,620 men (639 obese men and 2,981 men with normal weight) were included in this meta-analysis. Two of the six studies found a positive association between BMI and SDF, while the remaining four studies showed no statistically significant association. Most of these studies (230 obese men and 1810 men with normal weight) found an identical unadjusted mean SDF percentage between two groups of obese and normal-weight men. The pooled analysis indicated that there is no association between BMI category and SDF (SMD = 0.85; CI: −0.16, 1.87, P = 0.10, Fig. 2) with considerable heterogeneity between the studies (I2 = 99%, P < 0.001). There was no evidence of publication bias (P = 0.27). In a subgroup analysis, no significant difference was observed in the subset of studies that determined SDF with the SCSA (SMD: 0.40; CI: −0.81, 1.60, I2 = 99%, P = 0.52) and the TUNEL tests (SMD: 1.85; CI: −1.79, 5.49, I2 = 99%, P = 0.32) (Fig. 2).
Men with overweight (BMI = 25–29.99) compared with men with normal weight (BMI = 18.5–24.99)
A total of seven studies (including 2,139 overweight and 3,089 normal-weight men) assessed the association between BMI and SDF, with SMDs ranging from −0.19 (95% CI: −0.27, −0.12) to 2.80 (95% CI: 2.51, 3.10). Overweight men demonstrated a higher mean of SDF compared with normal-weight men (SMD = 0.66; 95% CI: 0.09, 1.22, P = 0.02, I2 = 99%, Fig. 3). When we limited the meta-analysis to the studies that determined SDF with the SCSA, the SMD increased by 0.05, but it was statistically nonsignificant with a high heterogeneity (SMD = 0.71; CI: −0.09, 1.51, I2 = 99%, P = 0.08, Fig. 3). As well, we limited the meta-analysis to studies that used the TUNEL test for determination of the SDF, and observed an increase of 0.26 SMD; however, this result was still nonsignificant and heterogeneous (SMD = 0.92; CI: −0.90, 2.74, I2 = 98%, P = 0.32, Fig. 3). There was only one study that determined SDF with the Comet technique (SMD = −0.03; CI: −0.26, 0.20, I2 = 99%, P = 0.80, Fig. 3).
Men with obesity (BMI > 30) compared with men with overweight (BMI = 25–29.99)
Ten studies (including 1,312 obese and 3,064 overweight men) evaluated the association between BMI and SDF, with SMDs ranging from −1.02 (95% CI: −1.28, −0.75) to 1.67 (95% CI: 1.13, 2.20). Out of these ten studies, four reported a positive association with SDF, while meta-analysis showed no difference between two groups (obese and overweight men) (SMD = 0.17; CI:−0.12, 0.46, I2 = 93%, P = 0.25, Fig. 4). Subgroup analysis showed no significant difference in the mean of SDF for studies that determined SDF with the SCSA (SMD: −0.17, 95% CI: −0.62, 0.29, P = 0.47, I2 = 95%, Fig. 4) and the TUNEL tests (SMD: 0.57, 95% CI: −0.07, 1.21, P = 0.08, I2 = 93%, Fig. 4). There was only one study that used the Comet test (SMD = 0.56; CI: 0.20, 0.92, P = 0.002, Fig. 4).
Men with obesity (BMI = 30–34.99) compared with men with overweight (BMI = 25–29.99)
We retrieved four studies with 696 participants, in which SDF was compared between obese (n = 245) and overweight men (n = 451). After combining the data, there was no significant difference between obese and overweight men (SMD: −0.08, 95% CI: −0.24, 0.07, P = 0.30, Fig. 5). No heterogeneity was observed for this outcome (I2 = 0%, P = 0.95).
Men with obesity (BMI = 30–34.99) compared with men with normal weight (BMI < 25)
The results for this association were reported in three studies that represented 304 participants (174 obese men and 130 normal-weight men). The mean of SDF was significantly higher in obese men compared with normal-weight subjects (SMD: 0.23, 95% CI: 0.01, 0.46, P = 0.05, Fig. 6). No heterogeneity was observed for this outcome (I2 = 0%, P = 0.40).
Men with obesity (BMI > 35) compared with men with normal weight (BMI < 25)
The meta-analysis of the three studies that reported the endpoint SDF demonstrated considerable heterogeneity (I2 = 85%, P = 0.001). The use of the random-effect model did not reveal any significant difference between two groups (SMD: 0.56, 95% CI: −0.17, 1.28, P = 0.13, Fig. 7).
Men with overweight (BMI = 25–29.99) compared with men with underweight (BMI < 18.5)
Three studies, including a total of 1654 men (1569 overweight and 85 underweight men), were included in this meta-analysis. The pooled analysis showed that there is an association between BMI category and SDF (SMD = 0.12; CI: −0.26, 0.50, P = 0.54, Fig. 8) with a moderate heterogeneity (I2 = 58%, P = 0.09).
Discussion
To the best of our knowledge, the present study is the first systematic review and meta-analysis evaluating the association of BMI and SDF levels. Accurate eligibility criteria were applied, and a subgroup analysis was conducted regarding the type of SDF assay. Based on the studies included in this systematic review, there was no strong evidence for an overall detrimental effect of BMI on SDF. Although three studies reported higher SDF levels in obese men (BMI = 30–34.99) compared with normal-weight men (BMI < 25), the overall results do not support such conclusions [12, 14, 15]. We concluded that if such association exists, it is not statistically significant enough to be detected by the meta-analysis of observational studies with a total number of 8255 men; however, we are not able to draw a definitive conclusion, and considering the probable clinical importance of this issue, we should interpret the results with caution.
During the last decade, the SDF has played a significant role in predicting pregnancy rates, both in natural conception and ART [20,21,22,23,24,25], and appropriate treatment may increase the possibility of successful pregnancy [26]. The causes of SDF remain unknown, although hypotheses such as OS, defects in chromatin maturation, and apoptosis have been suggested [27]. Aitken and De Iuliis demonstrated that the most common cause of DNA fragmentation in spermatozoa is OS [28]. Reactive oxygen species (ROS), the natural by-products of aerobic metabolism, are chemically reactive chemical species containing oxygen, such as the superoxide anion (O2), hydroxyl radical (HO•), or hydrogen peroxide (H2O2). Under normal conditions, due to the short half-life of free oxygen radicals and antioxidant activity, there is an equilibrium for the harmless function of free oxygen radicals in spermatozoa [29].
Minor concentrations of ROS are essential for the proper functioning of spermatozoa, especially capacitating, hyperactivation, and acrosomal reaction [30]. In vitro experiments have demonstrated that ROS can stimulate capacitation by tyrosine phosphorylation, zona pellucida binding, and promotion of chemotaxis and chromatin compaction in maturing spermatozoa during epididymal transit [1]. Aktan and Chen have shown more concentrations of free oxygen radicals in the semen of infertile men [31]. More concentration of ROS can be important mediators of damage to biomolecules involving lipids, proteins, and DNA. Three major effects of OS impacting spermatozoa are the single- and double-strand DNA fragmentation, the oxidation of membrane polyunsaturated fatty acids, and the loss of mitochondrial membrane potential [32].
Several possible mechanisms may account for the effect of obesity on OS. Mitochondrial and peroxisomal oxidation of fatty acids, which elevated by adipose tissue, can produce ROS in oxidation reactions. Mitochondrial oxidative phosphorylation, along with the respiratory chain in mitochondria, leads to the production of free oxygen radicals, by reducing the concentration, and activity of antioxidant enzymes, such as superoxide dismutase, catalase, and glutathione peroxidase, along with increased adipose tissue. OS is associated with endothelial dysfunction, a pro-inflammatory state that is characterized by a reduction in the bioavailability of vasodilators, particularly nitric oxide, and an increase in endothelium-derived contractile factors [33, 34].
It seems that the heterogeneity between the included studies is the most important reason for not observing the association between BMI and SDF. The most important causes of heterogeneity include the type of study population, different eligibility criteria, various BMI classification systems, study design, and different measurement methods of SDF.
Strengths and limitations of the study
The strengths of the present study are the following: (1) the inclusion of studies from different countries around the world (11 countries), which allowed us to draw more generalizable conclusions; (2) a large number of studies (14 studies with a total number of 8255 participants), which could make the results more precise; (3) inclusion of methodologically high-quality and well-designed studies based on the results from the appraisal. However, this systematic review and meta-analysis have several limitations that need to be addressed. First, the high heterogeneity existed between the studies. The most probable causes of heterogeneity are the different populations included in the studies, different eligibility criteria, various BMI classifications, study design, and different SDF measurement methods. More than half of the studies did not have specific exclusion criteria for their participants, so one of the possible causes of heterogeneity was the difference between the exclusion criteria. Another reason for heterogeneity can be the differences in the study populations. Five studies examined the association in healthy populations, while the remaining assessed subfertile population. In most of the included studies, the BMI was categorized based on the classification systems other than the World Health Organization’s standard classification. Unfortunately, due to insufficient data, we were not able to perform subgroup analysis based on population type, eligibility criteria, and study design. Second, a number of the included studies selected the exposed and nonexposed participants at the beginning of the study. The results from these studies are often vulnerable to be influenced by selection bias, and the selection of an appropriate group of nonexposed participants can be one of the most challenging aspects of these studies. An important principle is that the distribution of potential confounding variables should be the same among exposed and nonexposed participants; in other words, both groups should stem from the same source population. Considering the nature of the question, we have based this systematic review on the data from observational studies, which are at higher risk of confounding factors compared with randomized controlled trials. Some of the included studies in this meta-analysis did not control for the same confounder variables. Several studies did not control the effect of confounders. There are many variables like semen collection methods, storage temperature, varicocele, infection, and the temperature of the testes that can affect the result of SDF tests. The lack of strategies for control of confounding variables in all included studies made us unable to do meta-analysis based on the adjusted MD.
Conclusion
To date, a large number of studies assessed the association between BMI and SDF. There is insufficient data to demonstrate a positive association between BMI and SDF. Our findings suggest a need for conducting further cohort studies for evaluating the association between BMI and SDF considering potential confounders.
References
Wright C, Milne S, Leeson H. Sperm DNA damage caused by oxidative stress: modifiable clinical, lifestyle and nutritional factors in male infertility. Reprod Biomed Online. 2014;28:684–703.
Henkel RR, Franken DR. Sperm DNA fragmentation: origin and impact on human reproduction. J Reprod Stem Cell Biotechnol. 2011;2:88–108.
Chrysohoou C, Panagiotakos DB, Pitsavos C, Skoumas I, Papademetriou L, Economou M, et al. The implication of obesity on total antioxidant capacity in apparently healthy men and women: the ATTICA study. Nutr Metab Cardiovasc Dis. 2007;17:590–7.
Fernández-Sánchez A, Madrigal-Santillán E, Bautista M, Esquivel-Soto J, Morales-González Á, Esquivel-Chirino C, et al. Inflammation, oxidative stress, and obesity. Int J Mol Sci. 2011;12:3117–32.
Craig JR, Jenkins TG, Carrell DT, Hotaling JM. Obesity, male infertility, and the sperm epigenome. Fertil Steril. 2017;107:848–59.
Bandel I, Bungum M, Richtoff J, Malm J, Axelsson J, Pedersen HS, et al. No association between body mass index and sperm DNA integrity. Hum Reprod. 2015;30:1704–13.
Chavarro JE, Toth TL, Wright DL, Meeker JD, Hauser R. Body mass index in relation to semen quality, sperm DNA integrity, and serum reproductive hormone levels among men attending an infertility clinic. Fertil Steril. 2010;93:2222–31.
Dupont C, Faure C, Sermondade N, Boubaya M, Eustache F, Clement P, et al. Obesity leads to higher risk of sperm DNA damage in infertile patients. Asian J Androl. 2013;15:622–5.
Kort HI, Massey JB, Elsner CW, Mitchell-Leef D, Shapiro DB, Witt MA, et al. Impact of body mass index values on sperm quantity and quality. J Androl. 2006;27:450–2.
Lu JC, Jing J, Chen L, Ge YF, Feng RX, Liang YJ, et al. Analysis of human sperm DNA fragmentation index (DFI) related factors: a report of 1010 subfertile men in China. Reprod Biol Endocrinol. 2018;16:23.
Oliveira JBA, Petersen CG, Mauri AL, Vagnini LD, Renzi A, Petersen B, et al. Association between body mass index and sperm quality and sperm DNA integrity. A large population study. Andrologia 2018;50:e12889.
Eisenberg ML, Kim S, Chen Z, Sundaram R, Schisterman EF, Buck Louis GM. The relationship between male BMI and waist circumference on semen quality: data from the LIFE study. Hum Reprod. 2014;29:193–200.
Fariello RM, Pariz JR, Spaine DM, Cedenho AP, Bertolla RP, Fraietta R. Association between obesity and alteration of sperm DNA integrity and mitochondrial activity. Bju Int. 2012;110:863–7.
Andersen JM, Herning H, Aschim EL, Hjelmesaeth J, Mala T, Hanevik HI, et al. Body mass index is associated with impaired semen characteristics and reduced levels of anti-mullerian hormone across a wide weight range. PLoS ONE 2015;10:e0130210.
Andersen JM, Ronning PO, Herning H, Bekken SD, Haugen TB, Witczak O. Fatty acid composition of spermatozoa is associated with BMI and with semen quality. Andrology. 2016;4:857–65.
Thomsen L, Humaidan P, Bungum L, Bungum M. The impact of male overweight on semen quality and outcome of assisted reproduction. Asian J Androl. 2014;16:749–54.
Taha EA, Sayed SK, Gaber HD, Abdel Hafez HK, Ghandour N, Zahran A, et al. Does being overweight affect seminal variables in fertile men? Reprod Biomed Online. 2016;33:703–8.
Leisegang K, Bouic PJD, Menkveld R, Henkel RR. Obesity is associated with increased seminal insulin and leptin alongside reduced fertility parameters in a controlled male cohort. Reprod. Biol. Endocrinol. 2014;12:34.
Rybar R, Kopecka V, Prinosilova P, Markova P, Rubes J. Male obesity and age in relationship to semen parameters and sperm chromatin integrity. Andrologia. 2011;43:286–91.
Zini A, Boman JM, Belzile E, Ciampi A. Sperm DNA damage is associated with an increased risk of pregnancy loss after IVF and ICSI: systematic review and meta-analysis. Hum Reprod. 2008;23:2663–8.
Simon L, Zini A, Dyachenko A, Ciampi A, Carrell DT. A systematic review and meta-analysis to determine the effect of sperm DNA damage on in vitro fertilization and intracytoplasmic sperm injection outcome. Asian J Androl. 2017;19:80.
Li Z, Wang L, Cai J, Huang H. Correlation of sperm DNA damage with IVF and ICSI outcomes: a systematic review and meta-analysis. J Assist Reprod Genet. 2006;23:367–76.
Zhao J, Zhang Q, Wang Y, Li Y. Whether sperm deoxyribonucleic acid fragmentation has an effect on pregnancy and miscarriage after in vitro fertilization/intracytoplasmic sperm injection: a systematic review and meta-analysis. Fertil Steril. 2014;102:998–1005. e8
Zhang Z, Zhu L, Jiang H, Chen H, Chen Y, Dai Y. Sperm DNA fragmentation index and pregnancy outcome after IVF or ICSI: a meta-analysis. J Assist Reprod Genet. 2015;32:17–26.
Osman A, Alsomait H, Seshadri S, El-Toukhy T, Khalaf Y. The effect of sperm DNA fragmentation on live birth rate after IVF or ICSI: a systematic review and meta-analysis. Reprod Biomed Online. 2015;30:120–7.
Tamburrino L, Marchiani S, Montoya M, Marino FE, Natali I, Cambi M, et al. Mechanisms and clinical correlates of sperm DNA damage. Asian J Androl. 2012;14:24.
Sakkas D, Alvarez JG. Sperm DNA fragmentation: mechanisms of origin, impact on reproductive outcome, and analysis. Fertil steril. 2010;93:1027–36.
Aitken RJ, De Iuliis GN. Origins and consequences of DNA damage in male germ cells. Reprod Biomed Online. 2007;14:727–33.
Kumar N, Singh AK. Reactive oxygen species in seminal plasma as a cause of male infertility. J. Gynecol. Obstet. Hum. Reprod. 2018;47:565–72.
Lobascio A, De Felici M, Anibaldi M, Greco P, Minasi M, Greco E. Involvement of seminal leukocytes, reactive oxygen species, and sperm mitochondrial membrane potential in the DNA damage of the human spermatozoa. Andrology. 2015;3:265–70.
Aktan G, Doğru-Abbasoğlu S, Küçükgergin C, Kadıoğlu A, Özdemirler-Erata G, Koçak-Toker N. Mystery of idiopathic male infertility: is oxidative stress an actual risk? Fertil Steril. 2013;99:1211–5.
Zini A, San Gabriel M, Baazeem A. Antioxidants and sperm DNA damage: a clinical perspective. J Assist Reprod Genet. 2009;26:427–32.
Ferramosca A, Di Giacomo M, Moscatelli N, Zara V. Obesity and male infertility: role of fatty acids in the modulation of sperm energetic metabolism. Eur J Lipid Sci Technol. 2018;120:1700451.
Aitken RJ, Koppers AJ. Apoptosis and DNA damage in human spermatozoa. Asian J Androl. 2011;13:36.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sepidarkish, M., Maleki-Hajiagha, A., Maroufizadeh, S. et al. The effect of body mass index on sperm DNA fragmentation: a systematic review and meta-analysis. Int J Obes 44, 549–558 (2020). https://doi.org/10.1038/s41366-020-0524-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-0524-8
- Springer Nature Limited
This article is cited by
-
Obesity increases genomic instability at DNA repeat-mediated endogenous mutation hotspots
Nature Communications (2024)
-
Sperm DNA fragmentation and infertility: a narrative review
World Journal of Urology (2024)
-
Male obesity is associated with sperm telomere shortening and aberrant mRNA expression of autophagy-related genes
Basic and Clinical Andrology (2023)
-
Lifestyle-, environmental-, and additional health factors associated with an increased sperm DNA fragmentation: a systematic review and meta-analysis
Reproductive Biology and Endocrinology (2023)
-
Ultra-processed food and the risk of overweight and obesity: a systematic review and meta-analysis of observational studies
International Journal of Obesity (2020)