Abstract
Background
Physical activity improves insulin sensitivity in obesity. Hypoxia training is claimed to augment this effect. We tested the hypothesis that normobaric hypoxia training would improve insulin sensitivity in obese patients with metabolic syndrome.
Methods
In a randomized controlled trial, 23 obese men with metabolic syndrome who were not informed of the FiO2 conditions underwent a 6-week physical exercise intervention under ambient (n = 11; FiO2 21%) conditions or hypoxia (n = 12; FiO2 15%) using a normobaric hypoxic chamber. Three 60-min sessions of interval training were performed each week at 60% of individual V̇O2max. Assessment of myocellular insulin sensitivity by euglycemic hyperinsulinemic clamp was performed in 21 of these subjects before and after 6 weeks of training. Comprehensive phenotyping also included biopsies of subcutaneous adipose tissues.
Results
The intermittent moderate physical exercise protocol did not substantially change the myocellular insulin sensitivity within 6 weeks under normoxic conditions (ISIClamp: 0.035 (IQR 0.016–0.075) vs. 0.037 (IQR 0.026–0.056) mg* kg−1 *min−1/(mU* l−1); p = 0.767). In contrast, ISIClamp improved during hypoxia training (0.028 (IQR 0.018–0.035) vs. 0.038 (IQR 0.024–0.060) mg * kg−1 *min−1/(mU *l−1); p < 0.05). Between group comparison of ISIClamp change revealed a small difference between groups (Cohen's d = 0.26). Within the hypoxic group, improvement of ISIClamp during training was associated with individual increase of circulating vascular endothelial growth factor (VEGF) levels (r = 0.678, p = 0.015), even if mean VEGF levels were not modified by any training condition. Atrial natriuretic peptide (ANP) system components were not associated with increased ISIClamp during hypoxic training.
Conclusions
Physical training under hypoxic conditions could partially augment the favorable effects of exercise alone on myocellular insulin sensitivity in obese men with metabolic syndrome. Concomitant changes in VEGF might represent an underlying pathophysiological mechanism.
Similar content being viewed by others
Background
Insulin resistance, hallmark of the metabolic syndrome in obesity, increases the risk to develop diabetes mellitus and cardiovascular disease [1, 2]. Weight loss and increased physical activity ameliorate insulin sensitivity [3,4,5,6]; however, both are difficult to achieve in daily practice [7]. Even center-based exercise programs have no long-term effect on physical activity in a primary care setting [8]. Therefore, alternative approaches are necessary. High-intensity interval training might have utility. In contrast to moderate continuous training, comparable bouts of high-intensity interval training thrice weekly improved insulin sensitivity within 16 weeks [9]. However, this type of exercise may not be suitable for many patients with obesity and metabolic syndrome. Normobaric hypoxia training is frequently used in athletes to enhance exercise performance [10, 11] and might benefit metabolism. A preliminary randomized controlled trial from our group revealed improved body fat content, reduced triacyglycerol levels, and improved homeostatic model-assessment for insulin resistance (HOMA-IR), already after 4 weeks in healthy volunteers [12]. A follow-up randomized controlled trial in healthy overweight and obese subjects further supported our optimism [13]. Interestingly, this effect was achieved at a lower workload compared to normoxia. However, these studies did not include patients with the metabolic syndrome and relied solely on HOMA-IR. This estimate does not reflect myocellular insulin sensitivity, which is a crucial regulator of glucose disposal during exercise.
Now, we report on a third randomized controlled trial in obese subjects who also suffered from metabolic syndrome. First data demonstrated that exercise had overriding effects on lowering blood pressure, improving lipid profiles, energy expenditure (EE), and performance, independent of hypoxia [14]. However, the effect on metabolic function of skeletal muscle is still unknown. Here, we aimed to specifically analyze the impact of hypoxic moderate-intensity training on myocellular insulin sensitivity, a secondary endpoint in our study. Measurement of myocellular insulin sensitivity was performed in a subgroup of those subjects using hyperinsulinemic euglycemic clamp as the gold standard method.
Despite the known effects of exercise and hypoxia on gene hypoxia inducible factor 1 (HIF-1) expression [15, 16], no such hypoxia-specific effect was seen regarding mRNA expression of known target genes in skeletal muscle [14]. Given the well-known interaction of hypoxia and physical activity on vascular endothelial growth factor (VEGF) [17, 18] as well as the atrial natriuretic peptid (ANP) [19,20,21], both also strongly regulated by adipose tissue, we further analyzed if those hormonal systems are involved in effects of hypoxic training on insulin sensitivity. Such a mechanism would further underscore the assumed impact of adipose tissue on myocellular insulin sensitivity.
Methods
Participants
We performed a prospective, randomized controlled trial in our clinical research unit. In total, 23 men between 18 and 70 years characterized by a body mass index (BMI) between 27 and 40 kg m−2 and a metabolic syndrome according to the NCEP ATP III definition [22] were enrolled in the entire study. However, only 21 of these subjects underwent euglycemic hyperinsulinemic clamp before and after training intervention. Only these subjects were included in all current analyses (Fig. 1).
All participants were initially screened for any systemic disease or biochemical evidence of severe hepatic or renal dysfunction, for serious health problems and current medication. The subjects were advised to continue their current diets and physical activity level aside from our protocol throughout the study. The study protocols were approved by the Institutional Review Board of the Charité Medical School and all subjects gave written informed consent.
Study design
Participants were randomized to a moderate-intensity 6-week endurance exercise training thrice weekly under either normoxic (21% O2) or hypoxic (15% O2) normobaric conditions. For allocation, a computer-generated list of random numbers was used according to SPSS 18 (SPSS, Inc., Chicago, IL, USA) statistical software with a 1:1 allocation using random block sizes of 2, 4, and 6. The participants, but not the person who supervised the training, were otherwise unaware of the training conditions. Phenotyping as well as intervention procedure were performed by a medical doctor and study nurses.
Phenotyping
Patients underwent a detailed evaluation of cardiorespiratory and metabolic function on three consecutive days at 8:00 AM after a 12-h overnight fast. This was performed before and after the 6-week training program at the Experimental and Clinical Research Center at the Charité Medical School. Patients were asked to abstain from (1) any kind of physical activity, (2) caffeine and alcohol containing beverages, and (3) from smoking at the day before the phenotyping. Body composition was assessed by air displacement plethysmography (BodPod, COSMED Deutschland GmbH, Fridolfing, Germany).
On day one, an oral glucose load was performed [14]. On day two, patients arrived again at 8:00 AM after a 12-h overnight fast in our study center. Then, patients were placed in our metabolic chamber in order to monitor V̇O2 consumption and V̇CO2 production at rest (30 min) to assess resting EE and during moderate bicycle exercise (60 min) on a bicycle ergometer (VIASprint 150P, Ergoline, Bitz, Germany). This chamber is a comfortable, airtight room (width: 2.5 m, depth: 2.0 m, height: 2.2 m; 11 m3) that is constantly supplied with fresh air like an open-circuit indirect calorimeter. This bicycle exercise session, required to monitor V̇O2 consumption and V̇CO2 production, was performed at a pre-defined workload of 50% calculated V̇O2max followed by a 40-min recovery period. Measured V̇O2 consumption and V̇CO2 production were used to calculate resting and exercise activity EE and respiratory exchange ratio (RER = V̇CO2/V̇O2). During exercise, heart rate and O2-saturation were continuously monitored and rates of perceived exertion on a 10-point scale were recorded every 10 min. After this exercise session within the metabolic chamber, patients had a 2-h lunch break. Then, cardiorespiratory fitness (V̇O2max) was directly determined by an incremental cycle ergometer test (Sana cardio 250 SE, Ergosana, Germany) until exhaustion. The test started with a 1-min rest to determine baseline parameters followed by a 2-min warm-up (20 W). Initial exercise workload was set to 25 W followed by a stepwise increase of 25 W every 3 min until subjective exhaustion or meeting discontinuation criteria. After exhaustion, there was a 5-min recovery period without workload. During the test, breath-by-breath gas exchange and an electrocardiogram were recorded (Quark RMR, COSMED Deutschland GmbH, Fridolfing, Germany), and at the end of every increment, blood samples were taken from an earlobe in order to analyze lactate.
On day three, abdominal subcutaneous tissue biopsies (app. 2.0 g) were obtained by needle biopsies from the periumbilical region using an aspiration through a conventional 12 G needle. After anesthetization of skin with 1% lidocaine without epinephrine, a skin incision (3–4 mm) was made and biopsies were obtained. Fat samples were snap-frozen in liquid nitrogen and stored at −80 °C until further analysis.
Hyperinsulinemic euglycemic clamps were performed in fasting state before and after the exercise protocols (1.0 (IQR 1.0–1.0) day after the last exercise session) as described previously [23, 24]. In brief, 40 mIU *m−2 *min−1 human insulin (Actrapid®, Novo Nordisk, Bagsvaard, Denmark) and a variable infusion of 10% glucose (Serag Wiessner, Naila, Germany) was used. Capillary glucose concentration was monitored every 5 min and was maintained between 4.0 and 4.9 mmol* l−1 via variation of the glucose infusion rate (GIR). Blood samples were collected before the clamp and at least 2 h after starting the clamp during steady-state conditions. Blood samples were centrifuged, and plasma and serum samples were frozen immediately at −80 °C. Skeletal muscle insulin sensitivity, predefined as a secondary endpoint, was assessed by dividing the average GIR (mg glucose *min−1) during the steady state of the clamp by the body weight (M-value). The insulin sensitivity index (ISIClamp) was calculated as ratio of glucose metabolized during the steady-state period (M-value) to mean serum insulin concentration (I, mU *l−1) in this period of the euglycemic clamp. Whole-body insulin sensitivity was assessed by HOMA-IR, which was calculated as previously described [25]. Changes of BMI, fat mass (FM), workload (WL), HOMA-IR, ISIClamp, mid-regional pro-atrial natriuretic peptide (MR-proANP) as well as NPR-A (natriuretic peptide receptor-A) and NPR-C mRNA expression were expressed as percent change from baseline and defined as ΔBMI, ΔFM, ΔWL, ΔHOMA-IR, ΔISIClamp, ΔMR-proANP, ΔNPR-A, and ΔNPR-C, respectively.
All cardiac MR scans were performed on a clinical 1.5 Tesla MR scanner (Avanto, Siemens Medical Solutions AG, Erlangen, Germany) using a 12-channel cardiac array coil. We performed cine imaging with a standard steady-state free precession sequence to assess cardiac structure and function. We acquired three long axes and a complete short-axis package covering the left ventricle from base to apex during repetitive breath holds in end-expiration [26].
Training intervention
Patients completed a moderate-intensity, aerobic exercise program over 6-weeks/thrice a week on a motorized treadmill (mercury 4.0, h/p/cosmos sports & medical GmbH, Germany) at 50–60% of their individual maximal heart rate, which was determined in the incremental cycle ergometer test. Corresponding training workload (WLT) was assessed during each session. One training session lasted 60 min with three intervals of 15 min walking on the treadmill and a 5-min break for recovery. The intervention group trained under normobaric hypoxia (15% FiO2) simulating an altitude of 2500 m, while the control group trained under normobaric normoxia (21% FiO2). Individual training heart rate was adjusted by changing treadmill slope and/or pace by the supervisor and was—similarly to the O2 saturation—monitored continuously throughout the entire session. All participants were advised to continue their diet during the entire study.
All trainings sessions took place in a normobaric hypoxia chamber (11 m2, 38 m3, Linde AG, Berlin, Germany). The oxygen content within the chamber was reduced by mixing the incoming air with nitrogen. Throughout the trainings sessions, O2 and CO2 concentrations were controlled by two independent sensors each (HTK, Hamburg, Germany). Depending on the measured gas concentrations, the inflow of fresh air and nitrogen was automatically adjusted by the system.
Laboratory tests
Capillary blood glucose was measured using the glucose oxidase method (Dr. Müller Super GL, Freital, Germany). Lipids were measured by standard laboratory methods. Serum insulin was measured using electrochemiluminescence immunoassay (Cobas e602 Analyzer; Roche Diagnostics, Mannheim, Germany) (inter-assay coefficient of variation (CV) 0.9–1.5%, intra-assay CV 3.4–4.9%). Mid-region pro ANP was analyzed using a commercial fluoroimmunoassay (BRAHMS MR-pro ANP KRYPTOR; BRAHMS Thermo Fisher) (inter-assay CV ≤ 6.5%, intra-assay CV < 2.5%). Plasma VEGF was measured by commercial ELISA (R&D Systems, UK).
Tissue preparation and real-time quantitative polymerase chain reaction
Frozen tissue was homogenized and total RNA was isolated according to the manufacturer's instructions of SV Total RNA Isolation (Promega, Mannheim, Germany). RNA samples were stored at −80 °C until assayed.
Complementary DNA (cDNA) synthesis was done according to manufacturer's manual (High Capacity RNA-tocDNA Kit; Applied Biosystems, Foster City, CA). Samples were analyzed in triplicate with Power SYBR Green PCR Master Mix (Applied Biosystems). Real-time quantitative polymerase chain reaction was performed using an ABI PRISM 7300 System (using SDS 1.4 system software, Applied Biosystems). The expression level of cyclophyllin A was used as an internal control. Primer sequences of analyzed genes are presented in Table S1 of the supplemental data. Cycle threshold values were used to calculate the amount of amplified polymerase chain reaction product in comparison to the housekeeping gene cyclophyllin A. The relative amounts of each transcript were analyzed using the 2−ΔCt method.
Statistics
Statistical procedures were performed using SPSS version 22.0 (SPSS Inc., Chicago, IL, USA) and R statistics package (version 3.0.1). Skeletal muscle insulin sensitivity was analyzed as a predefined secondary endpoint. Data are presented as median and limits of the interquartile range (IQR: 25th–75th percentile) unless stated otherwise. Parameters were compared between normoxic and hypoxic patient groups using Mann–Whitney U test and within patient groups to compare levels before and after 6 weeks of intervention with Wilcoxon signed rank test. Correlations between metric variables were assessed by Spearman's rank correlation coefficient partially with adjustment for ΔFM as mentioned within the results. This is an exploratory analysis, all tests have been two-sided and no further adjustment for multiple comparisons has been done.
Results
Demographic and anthropometric data of our subjects are given in Table 1. The participants were middle-aged, obese, untrained men characterized by the typical findings of metabolic syndrome and an impaired whole-body and myocellular insulin sensitivity. The groups were well matched for age, BMI, lipid levels, ISIClamp, and maximal workload (WLmax) before the training period. Only systolic blood pressure was slightly higher in the hypoxic-training group. At baseline, we observed as expected a moderate correlation of myocellular insulin sensitivity with estimates of obesity (FM: r = −0.528, p = 0.014 and BMI: r = −0.541, p = 0.011). Even though we observed the known relationship between MR-proANP and age (r = 0.555, p = 0.009) and between MR-proANP and FM (r = 0.673, p = 0.001), the baseline ISIClamp was not significantly correlated with circulating MR-proANP level, which might be caused by limited sample size.
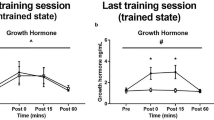
In accordance to our previous report of the entire patient group of this randomized controlled trial [14], we observed an improvement of several lipid parameters in both treatment groups, whereas relative FM was not changed by any intervention (Table S2). As expected, hypoxic training was associated with a stronger reduction of SpO2 before (−7.7 (IQR −8.7–(−6.5)) vs. −1.0 (IQR −3.1–0.5) %; p = 0.001) as well as after the 6-week training period (−7.3 (IQR −9.9–(−5.7)) vs. −1.0 (IQR −3.1–(−0.5)) %; p = 6.6 × 10−4). Training workload (WLT) of the subjects of the normoxic group was significantly increased after the training period, while this was not observed during hypoxic training (Table S2). Despite unchanged workload, 6 weeks of hypoxic training induced a substantial improvement of myocellular insulin sensitivity, whereas no effect could be observed under normoxic condition although workload did slightly increase within this group (Fig. 2). The between-group comparison did not reach level of significance (difference of means over time 0.009 mg *kg−1 *min−1/(mU *l−1), 95%CI [−0.006–0.023]; p = 0.422) and showed a small standardized effect size (Cohen's d = 0.26). In contrast, whole-body insulin sensitivity, assessed by HOMA-IR before and after 6 weeks of training, was similar for normoxic (4.6 (IQR 2.6–7.2) vs. 3.4 (IQR 1.9–5.7); p = 0.484) and hypoxic training (4.0 (IQR 2.7–9.3) vs. 3.9 (IQR 2.0–7.0); p = 0.859).
Circulating MR-proANP and VEGF levels, as well as adipose mRNA expression of NPR-A and NPR-C, did not significantly change with any type of training (Table 2). However, the balance between NPR-A and NPR-C receptor, which might reflect ANP efficacy, was increased during normoxic training (Fig. 3). In contrast, hypoxic training resulted in a reduction of adipose VEGF mRNA expression by trend (Table 2). Interestingly, training-induced individual changes of plasma VEGF were positively correlated with concomitant changes of adipose VEGF mRNA expression during hypoxia (r = 0.709; p = 0.015) (Fig. S1). This was not seen during normoxia.
Improvement of ISIClamp was associated with individual changes of circulating VEGF level during hypoxic training (Fig. 4), while this was not the case for subjects of the normoxic group. In contrast, changes in MR-proANP in normoxic (r = 0.700, p = 0.036) but not in hypoxic group (r = 0.343, p = 0.276) were significantly correlated with training induced effects on myocellular insulin sensitivity. Given the fact that circulating MR-proANP levels were strongly associated with FM at baseline, we adjusted this analysis to ΔFM during the training. Thereby, the moderate to strong correlation of MR-proANP and ISIClamp could be confirmed in subjects trained under normoxic condition (r = 0.820, p = 0.013), but was weak and not significant in the hypoxic group, also after adjustment for ΔFM (r = 0.451, p = 0.164).
Discussion
Despite the beneficial effect of increased physical activity on cardiovascular risk markers, the number of subjects participating in physical training is limited [27] and current strategies cannot sufficiently increase the amount of physical activity in subjects at metabolic and cardiovascular risk [7]. Thus, we aimed to introduce an alternative approach based on normobaric hypoxia training as an augmentation of exercise. We were encouraged by our findings in normal persons [12] and healthy obese subjects [13]. Although the overall effect of moderate-intensity training in normobaric hypoxia was less than we had hoped in our obese subjects with metabolic syndrome [14], the results reported here may suggest some utility for such a training in terms of improving myocellular insulin resistance. Activation of muscular function during physical activity plays a crucial role in exercise-induced changes of metabolism. Hypoxia seems to represent a potential strategy to ameliorate this effect, even though the training intensity is too low to affect glucose disposal in skeletal muscle by its own in normoxia. While we could detect a significant effect within the hypoxic group, the between-group comparison failed to achieve significance. This might be driven by the small effect size of 0.26 as well as the limited sample size for this secondary analysis. Interestingly a very recent trial also analyzed the effect of hypoxic training on myocellular insulin sensitivity in slightly older male and female subjects. Although these subjects were not necessarily characterized by metabolic syndrome and the training intensity was somewhat higher as used in our training protocol, this study revealed a comparable finding [28]. Given the estimated effects size, our observation reflects a notable physiologic improvement. Although this was smaller than the dramatic increase of myocellular insulin sensitivity reported after 3 months of substantial weight loss in obese subjects [29], we believe these data indicate a relevant effect and further studies including a higher sample size are clearly warranted. Moreover, our data indicate a tissue-specific effect, as fasting lipid parameters and HOMA-IR, both are strongly regulated by hepatic metabolism, were not further improved by changing the partial pressure of oxygen (PaO2) to conditions similar to ~2500 m above sea level as found in Denver, CO, USA, or the lower Alps in Europe.
The underlying mechanism might involve different pathways. Local hypoxia, induced by acute exercise, is known to enhance HIF-1α signaling [30]. However, hypoxic training conditions do not mandatory modify exercise-induced effect on muscular HIF-1a expression, neither after acute exercise [31] nor chronic training [32], which is in line with the findings in our cohort [14]. Activation of HIF-1α and its target genes seems to primarily represent an early adaption, only seen in untrained muscle [33] and disappearing after a period of regular training due to an activation of negative HIF-1α regulators [34]. Therefore, other mechanism might be responsible for the observed effect of hypoxic training on myocellular insulin sensitivity.
In addition to direct mechanism within the skeletal muscle, adipose tissue function is known to be crucial for the regulation of myocellular insulin sensitivity. Therefore, we explored the role of two interesting pathways within adipose tissue. VEGF is a well-known target of hypoxia in adipose tissue in mice [17] and has been demonstrated to be relevant in exercise-induced angiogenesis [18]. The growth factor is regulated by HIF-1 [35] and seems to be involved in regulation of insulin sensitivity during physical exercise [36]. This state-of-affairs is thought to be driven by an increase in capillary density, as the number of capillaries in muscle is positively correlated to peripheral insulin action [37]. The observed association of hypoxic training-mediated effects on myocellular insulin sensitivity and plasma VEGF might support such an underlying mechanism. Moreover, our data indicate that alteration of circulating VEGF levels might be driven by alterations in adipose VEGF production due to local hypoxia. Given the known effect of HIF-1α on VEGF and VEGF-induced angiogenesis [34], this idea is tempting. The subsequent increase of capillary density would result in increased adipose tissue perfusion and adipose oxygen level at rest. The higher adipose tissue perfusion already demonstrated in our cohort after hypoxia training [14] reflects such a chronic super-compensation and could also explain the rather reduced adipose HIF-1α expression during hypoxia.
Atrial ANP release is also induced by local hypoxia in an experimental setting via HIF-1α pathway [21]. Given the effects of acute [19] and chronic [20] exercise training on ANP release as well as the impact of ANP system on insulin sensitivity [19, 29], this mechanism represents another promising target involved in the regulation of insulin sensitivity during hypoxia and physical exercise. Especially we were interested in the balance of adipose NPR-A and NPR-C, as latter acts as an ANP clearing receptor and the receptor balance is therefore strongly involved in the regulation of circulating ANP levels and ANP efficacy. Actually, the previously described association of ΔMR-proANP and improvement of insulin sensitivity [29] could be detected during normoxic training. The concomitant augmentation of NPR-A/NPR-C balance in adipose tissue, which suggests an increase of circulating ANP level or efficacy [29, 38], indicates an involvement of ANP system on training effects at least under normoxic conditions. This is in line with the exercise-induced elevation of circulating ANP levels reported after 4 months of physical training [20]. In contrast, ANP system was not related to effects of hypoxia training on insulin sensitivity, which does not support a role of ANP during hypoxia. We can only speculate about the mechanism. The well-known downregulation of NPR-C expression during hypoxia, seen in lungs of animals exposed to hypoxic condition [39], might be counterbalanced by the chronic super-compensation with hyperperfusion in adipose tissue.
The missing effect on insulin sensitivity in normoxia was not surprising, even if an increased myocellular insulin sensitivity was described after 12 weeks of exercise training previously [5]. We have designed a training protocol characterized by a shorter duration, lower intensity (60% V̇O2max compared to up to 85% V̇O2max) and lower frequency (3 days per week compared to 5 days per week). The intended low efficacy was also reflected by unchanged V̇O2max after 6 weeks of training. Accordingly, Tjonna and colleagues reported unchanged insulin sensitivity after 16 weeks moderate-intensity training using an exercise protocol (three sessions per week at a 70% of maximal heart rate) and a study cohort almost comparable to our study [9].
Our study has obvious limitations. First, we could only assess the effect on hypoxia in the context of our training protocol. Further studies including different training intensities and longer duration of the training period are clearly required to generalize our findings. Second, we analyzed only the subgroup of the participants that underwent a hyperinsulinemic euglycemic clamp procedure. However, both randomization groups were still well matched for age, BMI, resting EE, lipid levels, ISIClamp, and maximal workload. Third, studies enrolling a larger sample size should be performed to confirm our findings as mentioned above. Of course, behavioral, social as well as environmental factors during the intervention, like the individual diet might have influenced our findings. Even if the participants were advised to continue their diet, food intake was not strictly controlled in this outpatient study. Therefore, we could not entirely exclude the possibility that different food patterns or individual changes during the trial may have affected our results. However, our study also has some strengths. Study participants were well characterized. Especially, phenotyping procedures like metabolic chamber and hyperinsulinemic, euglycemic clamps [40] are considered as gold standard phenotyping techniques. This enables the analysis of organ-specific effects, which might remain undiscovered by analyzing systemic parameter of the metabolic syndrome. In addition, analyses of VEGF and ANP system also included tissue-based data, which are urgently required to understand the regulation of these systems.
Conclusions
In summary, our data indicate that hypoxia may ameliorate effects of intermittent moderate physical exercise on insulin sensitivity in men with metabolic syndrome in a tissue-specific manner. Even though further studies are clearly required, we speculate that this effect could provide a useful approach to counteract the failure of public strategies to implement appropriate physical activity in subjects at metabolic risk. Modulation of the VEGF system, but not global or adipose ANP system, seems to be involved in the beneficial effect of hypoxia.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bonora E, Formentini G, Calcaterra F, Lombardi S, Marini F, Zenari L, et al. HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in type 2 diabetic subjects: prospective data from the Verona Diabetes Complications Study. Diabetes Care. 2002;25:1135–41.
Hanley AJ, Williams K, Stern MP, Haffner SM. Homeostasis model assessment of insulin resistance in relation to the incidence of cardiovascular disease: the San Antonio Heart Study. Diabetes Care. 2002;25:1177–84.
Lean ME, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet. 2018;391:541–51.
Gregg EW, Chen H, Wagenknecht LE, Clark JM, Delahanty LM, Bantle J, et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA. 2012;308:2489–96.
Yassine HN, Marchetti CM, Krishnan RK, Vrobel TR, Gonzalez F, Kirwan JP. Effects of exercise and caloric restriction on insulin resistance and cardiometabolic risk factors in older obese adults-a randomized clinical trial. J Gerontol A Biol Sci Med Sci. 2009;64:90–5.
VDB JD, VDV JHPM, DEW EAC, Bosma H, Savelberg H, Schaper NC, et al. Replacement effects of sedentary time on metabolic outcomes: The Maastricht Study. Med. Sci. Sports Exerc. 2017;49:1351–8.
Moreno-Franco B, Penalvo JL, Casasnovas Lenguas JA, Leon-Latre M. [Compliance with Physical Activity Recommendations and Associated Factors in a Cohort of Spanish Adult Workers]. Rev Esp Salud Publica. 2015;89:447–57.
Harrison RA, Roberts C, Elton PJ. Does primary care referral to an exercise programme increase physical activity one year later? A randomized controlled trial. J Public Health (Oxf). 2005;27:25–32.
Tjonna AE, Lee SJ, Rognmo O, Stolen TO, Bye A, Haram PM, et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: a pilot study. Circulation. 2008;118:346–54.
Hamlin MJ, Lizamore CA, Hopkins WG. The effect of natural or simulated altitude training on high-intensity intermittent running performance in team-sport athletes: a meta-analysis. Sports Med. 2018;48:431–46.
Czuba M, Wilk R, Karpinski J, Chalimoniuk M, Zajac A, Langfort J. Intermittent hypoxic training improves anaerobic performance in competitive swimmers when implemented into a direct competition mesocycle. PLoS ONE. 2017;12:e0180380.
Haufe S, Wiesner S, Engeli S, Luft FC, Jordan J. Influences of normobaric hypoxia training on metabolic risk markers in human subjects. Med. Sci. Sports Exerc. 2008;40:1939–44.
Wiesner S, Haufe S, Engeli S, Mutschler H, Haas U, Luft FC, et al. Influences of normobaric hypoxia training on physical fitness and metabolic risk markers in overweight to obese subjects. Obesity. 2010;18:116–20.
Klug L, Mahler A, Rakova N, Mai K, Schulz-Menger J, Rahn G, et al. Normobaric hypoxic conditioning in men with metabolic syndrome. Physiol Rep. 2018;6:e13949.
Semenza GL. Regulation of mammalian O2 homeostasis by hypoxia-inducible factor 1. Annu Rev Cell Dev Biol. 1999;15:551–78.
Ameln H, Gustafsson T, Sundberg CJ, Okamoto K, Jansson E, Poellinger L, et al. Physiological activation of hypoxia inducible factor-1 in human skeletal muscle. FASEB J. 2005;19:1009–11.
Lolmede K, Durand de Saint Front V, Galitzky J, Lafontan M, Bouloumie A. Effects of hypoxia on the expression of proangiogenic factors in differentiated 3T3-F442A adipocytes. Int J Obes Relat Metab Disord. 2003;27:1187–95.
Gustafsson T. Vascular remodelling in human skeletal muscle. Biochem Soc Trans. 2011;39:1628–32.
Mandroukas A, Metaxas TI, Heller J, Vamvakoudis E, Christoulas K, Riganas CS, et al. The effect of different exercise-testing protocols on atrial natriuretic peptide. Clin Physiol Funct Imaging. 2011;31:5–10.
da Silveira Campos RM, Damaso AR, Masquio DCL, Duarte FO, Sene-Fiorese M, Aquino AE Jr., et al. The effects of exercise training associated with low-level laser therapy on biomarkers of adipose tissue transdifferentiation in obese women. Lasers Med Sci. 2018;33:1245–54.
Zhang QL, Cui BR, Li HY, Li P, Hong L, Liu LP, et al. MAPK and PI3K pathways regulate hypoxia-induced atrial natriuretic peptide secretion by controlling HIF-1 alpha expression in beating rabbit atria. Biochem. Biophys. Res. Commun. 2013;438:507–12.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97.
Mai K, Andres J, Bobbert T, Maser-Gluth C, Mohlig M, Bahr V, et al. Rosiglitazone decreases 11beta-hydroxysteroid dehydrogenase type 1 in subcutaneous adipose tissue. Clin Endocrinol. 2007;67:419–25.
DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979;237:E214–23.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Toka O, Tank J, Schachterle C, Aydin A, Maass PG, Elitok S, et al. Clinical effects of phosphodiesterase 3A mutations in inherited hypertension with brachydactyly. Hypertension. 2015;66:800–8.
Haftenberger M, Schuit AJ, Tormo MJ, Boeing H, Wareham N, Bueno-de-Mesquita HB, et al. Physical activity of subjects aged 50-64 years involved in the European Prospective Investigation into Cancer and Nutrition (EPIC). Public Health Nutr. 2002;5:1163–76.
Chobanyan-Jurgens K, Scheibe RJ, Potthast AB, Hein M, Smith A, Freund R, et al. Influences of hypoxia exercise on whole body insulin sensitivity and oxidative metabolism in older individuals. J Clin Endocrinol Metab. 2019;104:5238–48.
Brachs M, Wiegand S, Leupelt V, Ernert A, Kintscher U, Jumpertz von Schwarzenberg R, et al. ANP system activity predicts variability of fat mass reduction and insulin sensitivity during weight loss. Metabolism. 2016;65:935–43.
Gorgens SW, Benninghoff T, Eckardt K, Springer C, Chadt A, Melior A, et al. Hypoxia in combination with muscle contraction improves insulin action and glucose metabolism in human skeletal muscle via the HIF-1alpha pathway. Diabetes. 2017;66:2800–7.
Slivka DR, Heesch MW, Dumke CL, Cuddy JS, Hailes WS, Ruby BC. Human skeletal muscle mRNAResponse to a single hypoxic exercise bout. Wilderness Environ Med. 2014;25:462–5.
De Smet S, D'Hulst G, Poffe C, Van Thienen R, Berardi E, Hespel P. High-intensity interval training in hypoxia does not affect muscle HIF responses to acute hypoxia in humans. Eur J Appl Physiol. 2018;118:847–62.
Lundby C, Gassmann M, Pilegaard H. Regular endurance training reduces the exercise induced HIF-1alpha and HIF-2alpha mRNA expression in human skeletal muscle in normoxic conditions. Eur J Appl Physiol. 2006;96:363–9.
Lindholm ME, Rundqvist H. Skeletal muscle hypoxia-inducible factor-1 and exercise. Exp Physiol. 2016;101:28–32.
Trayhurn P, Wang B, Wood IS. Hypoxia and the endocrine and signalling role of white adipose tissue. Arch Physiol Biochem. 2008;114:267–76.
Wagner H, Fischer H, Degerblad M, Alvarsson M, Gustafsson T. Improvement of insulin sensitivity in response to exercise training in type 2 diabetes mellitus is associated with vascular endothelial growth factor A expression. Diab Vasc Dis Res. 2016;13:361–6.
Solomon TP, Haus JM, Li Y, Kirwan JP. Progressive hyperglycemia across the glucose tolerance continuum in older obese adults is related to skeletal muscle capillarization and nitric oxide bioavailability. J Clin Endocrinol Metab. 2011;96:1377–84.
Schlueter N, de SA, Willmes DM, Spranger J, Jordan J, Birkenfeld AL. Metabolic actions of natriuretic peptides and therapeutic potential in the metabolic syndrome. Pharmacol Ther. 2014;144:12–27.
Sun JZ, Oparil S, Lucchesi P, Thompson JA, Chen YF. Tyrosine kinase receptor activation inhibits NPR-C in lung arterial smooth muscle cells. Am J Physiol Lung Cell Mol Physiol. 2001;281:L155–63.
Rudvik A, Mansson M. Evaluation of surrogate measures of insulin sensitivity - correlation with gold standard is not enough. BMC Med Res Methodol. 2018;18:64.
Acknowledgements
We thank Gabriele Rahn, N. Huckauf, and C. Kalischke for excellent technical assistance.
Funding
This research was supported by the Deutsche Forschungsgemeinschaft (LU 435/13-1). KM was supported by the German Diabetes Society (DDG) and the German Ministry for Education and Research (BMBF) by support of the Berlin Institute of Health (BIH).
Author information
Authors and Affiliations
Contributions
NR, MB, LK, AM, TB, and JSM researched data. KM researched data and was primarily responsible for writing the manuscript. TB, MB, SP, AM, LK, JS, and FCL contributed to the discussion and reviewed/edited the manuscript. FCL conceived the study and obtained funding.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
The study protocols were approved by the Institutional Review Board of the Charité Medical School (EA1/140/12) and all subjects gave written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mai, K., Klug, L., Rakova, N. et al. Hypoxia and exercise interactions on skeletal muscle insulin sensitivity in obese subjects with metabolic syndrome: results of a randomized controlled trial. Int J Obes 44, 1119–1128 (2020). https://doi.org/10.1038/s41366-019-0504-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0504-z
- Springer Nature Limited
This article is cited by
-
Anaerobic threshold using sweat lactate sensor under hypoxia
Scientific Reports (2023)
-
Post-exercise cardiac autonomic and cardiovascular responses to heart rate-matched and work rate-matched hypoxic exercise
European Journal of Applied Physiology (2021)